Maniobras para la reducción de la pronación dolorosa del codo en niños pequeños
Resumen
Antecedentes
La pronación dolorosa del codo (codo de niñera) es una lesión común en los niños pequeños. Esta lesión resulta a menudo de una tracción súbita en el brazo, habitualmente por una persona adulta o más alta, que impulsa el radio a través del ligamento anular, lo que produce la subluxación (luxación parcial) de la cabeza del radio. También puede ser causada por una caída o una torcedura. El niño experimenta dolor agudo súbito y pérdida de la función en el brazo afectado. La pronación dolorosa del codo se trata generalmente mediante la intervención manual de la cabeza radial subluxada. Pueden aplicarse diversas maniobras; más comúnmente, la supinación del antebrazo, a menudo combinada con la flexión y la (hiper‐)pronación. No está claro qué maniobra es más exitosa. Ésta es una actualización de una revisión Cochrane publicada por primera vez en 2009 y actualizada por última vez en 2011.
Objetivos
Comparar los efectos (beneficiosos y perjudiciales) de los diferentes métodos utilizados para manipular la pronación dolorosa del codo en niños pequeños.
Métodos de búsqueda
Se realizaron búsquedas en el registro especializado de Ensayos Controlados del Grupo Cochrane de Lesiones Óseas, Articulares y Musculares (Cochrane Bone, Joint and Muscle Trauma Group), en el Registro Cochrane Central de Ensayos Controlados (Cochrane Central Register of Controlled Trials), MEDLINE, Embase, CINAHL, LILACS, PEDro, registros de ensayos clínicos y listas de referencias de artículos. Fecha de la última búsqueda: septiembre de 2016.
Criterios de selección
Se incluyeron los ensayos clínicos controlados aleatorios o cuasialeatorios que evaluaban las maniobras para la pronación dolorosa del codo. La medida de resultado primaria fue el fracaso en el primer intento, lo que requería tratamiento adicional.
Obtención y análisis de los datos
Dos autores de la revisión consideraron de forma independiente los ensayos para la inclusión, evaluaron el riesgo de sesgo y extrajeron los datos. Los datos se agruparon mediante un modelo de efectos fijos.
Resultados principales
En términos generales, se incluyeron nueve ensayos con 906 niños (todos menores de siete años de edad y un 58% de pacientes femeninos) de los cuales cinco ensayos fueron identificados recién en esta actualización. Ocho ensayos se realizaron en departamentos de urgencias o centros de atención ambulatoria, y uno se realizó en una unidad de ortopedia pediátrica terciaria. Se realizaron cuatro ensayos en los Estados Unidos, tres en Turquía, uno en Irán y uno en España. Cinco ensayos estuvieron en riesgo alto de sesgo de selección debido a la falta de ocultación de la asignación y todos los ensayos estuvieron en riesgo alto de sesgo de detección debido a la falta de cegamiento del asesor.
Ocho ensayos compararon la hiperpronación con supinación‐flexión. Se encontró evidencia de baja calidad de que la hiperpronación dio lugar a menos fracaso en el primer intento que la supinación‐flexión (9,2% versus 26,4%, cociente de riesgos [CR] 0,35; intervalo de confianza del 95%(IC) 0,25 a 0,50; 811 participantes, ocho estudios). Basado en un riesgo ilustrativo de 268 fracasos en el primer intento por 1000 niños tratados con supinación‐flexión, el mismo ascendió a 174 fracasos menos por 1000 niños tratados mediante hiperpronación (IC del 95%: 134 a 201 menos). Basado en los datos de las diferencias de riesgos, también se calculó un número necesario a tratar de 6 (IC del 95%: 5 a 8); este hecho significa que seis niños necesitarían ser tratados con el método de pronación en lugar del de supinación‐flexión para evitar un fracaso adicional en el primer intento.
La evidencia de muy baja calidad (de cuatro estudios) sobre el dolor durante o después de la manipulación significa que no se conoce si hay una diferencia entre la pronación y la supinación‐flexión. Hubo evidencia de muy baja calidad de seis estudios de que la pronación repetida puede ser más efectiva que la supinación‐flexión repetida para el segundo intento después del fracaso inicial. Los resultados restantes no se informaron (efectos adversos, recurrencia) o no fueron apropiados para el agrupamiento (fracaso final). El fracaso final, informado para la población en general solo debido a las diferencias en los protocolos de estudio en lo que se refiere a qué hacer después del fracaso en el primer intento, varió de ningún fracaso máximo en dos estudios a seis fracasos (4,1% de 148 episodios) en un estudio.
Un ensayo comparó supinación‐extensión versus supinación‐flexión. Aportó evidencia de muy baja calidad (disminuida en tres niveles debido al riesgo muy grave de sesgo y a la imprecisión grave) de ninguna diferencia clara en el fracaso en el primer intento entre los dos métodos.
Conclusiones de los autores
Hubo evidencia de baja calidad de ocho ensayos pequeños de que el método de pronación puede ser más efectivo en el primer intento que el método de supinación para manipular la pronación dolorosa del codo en los niños pequeños. Para otros resultados, no es posible establecer ninguna conclusión debido a la evidencia de muy baja calidad o a los resultados que no se informaron. Se sugiere que se necesita un ensayo clínico aleatorio de alta calidad que compare la hiperpronación y la supinación‐flexión para aportar evidencia definitiva. Se recomienda que el mismo sea precedido por una encuesta entre los médicos para establecer el grado de consenso clínico y para optimizar el diseño del estudio y el reclutamiento.
PICOs
Resumen en términos sencillos
Diferentes métodos de manipulación para la reducción de la pronación dolorosa del codo en niños pequeños
¿Qué es la pronación dolorosa del codo?
La pronación dolorosa del codo es una luxación de la articulación del codo en un niño pequeño generalmente causada por un adulto, o una persona más alta, que tira de manera repentina del brazo del niño cuando está extendido o cuando un niño se aparta de un adulto de un modo impulsivo.También puede ser causada por una caída o una torcedura. El niño se queja de dolor inmediatamente y no puede usar el brazo.
¿Cómo se trata?
El tratamiento consta generalmente de la manipulación del brazo para lograr que los huesos del codo recuperen su posición correcta. Esta lesión se trata generalmente mediante la intervención manual. Hay dos maniobras típicas, supinación y pronación. En la supinación, se tuerce o gira hacia fuera el antebrazo (la palma de la mano del niño mira hacia arriba), a veces seguida de la flexión del codo. Aunque esta maniobra se utiliza a menudo, no siempre es exitosa. En la pronación, el antebrazo se tuerce o se rota hacia adentro (la palma de la mano del niño mira hacia abajo). Por lo general, ambos métodos son seguros, aunque puede presentarse equimosis, y pueden ser dolorosos.
Resultados de la búsqueda
Se realizaron búsquedas en bases de datos de literatura médica hasta septiembre de 2016. Se encontraron nueve estudios pequeños que incluían a un total de 906 niños, de los cuales todos eran menores de siete años de edad. Alrededor de seis de cada 10 niños eran niñas. Ocho estudios se realizaron en departamentos de urgencias o centros de atención ambulatoria. Un estudio se realizó en una unidad especializada en ortopedia pediátrica. Ocho ensayos compararon la pronación versus supinación. Uno comparó dos métodos de supinación.
Resultados clave
El método de pronación (con la mano hacia abajo) puede ser más exitoso para la reubicación en el primer intento para los niños con pronación dolorosa del codo. Se calculó que si seis niños fueran tratados con el método de pronación en lugar del método de supinación, este procedimiento evitaría un fracaso más en el primer intento. La evidencia fue insuficiente para extraer conclusiones en cuanto a cuál de los dos métodos, si hubiese alguno, fue más doloroso. Cuando se realiza un segundo intento con el mismo método, la pronación puede ser más exitosa como un segundo intento. En unos pocos casos, hasta cuatro en 100; ninguno de una serie de intentos tuvo éxito. Ninguno de los estudios informó sobre los efectos secundarios ni sobre cuántos niños tuvieron otra pronación dolorosa del codo de forma posterior (recurrencia).
El estudio que comparó dos métodos de supinación aportó evidencia de muy baja calidad de que el fracaso después del primer intento fue similar en ambos métodos.
Calidad de la evidencia
Los nueve estudios tuvieron limitaciones metodológicas que pueden afectar la confiabilidad de los hallazgos y dar lugar a un alto riesgo de sesgo. La calidad de la evidencia para el fracaso en el primer intento en la comparación de pronación versus supinación fue baja, lo cual significa que no existe seguridad en cuanto a los resultados. La calidad muy baja de la evidencia sobre los otros resultados para ambas comparaciones significa que no existe seguridad acerca de los resultados.
Conclusiones
La evidencia de baja calidad indica que el método de pronación es más exitoso que el método de supinación para reducir la pronación dolorosa del codo en los niños pequeños. No es posible establecer conclusiones sobre otros resultados, incluido el dolor y los efectos secundarios.
Authors' conclusions
Summary of findings
| Pronation compared with supination reduction techniques for pulled elbow in young children | ||||||
| Patient or population: Children with pulled elbow1 Settings: Emergency departments, ambulatory care centres or orthopaedic units Intervention: Pronation (all were hyperpronation) for first manipulation Comparison: Supination (all included flexion) for first manipulation | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Supination‐flexion | Hyperpronation | |||||
| Failure: second attempt required | 268 per 10002 | 94 per 1000 (67 to 134) | RR 0.35 (0.25 to 0.50) | 811 | ⊕⊕⊝⊝ | |
| Pain (preferably during the procedure) | see Comments | see Comments | see Comments | ⊕⊝⊝⊝ | Data for this outcome are incomplete and were measured in very different ways in four studies. | |
| Adverse effects (e.g. bruising) | see Comments | see Comments | None of the trials reported this outcome. | |||
| Failure: continued failure after second attempt using same procedure as before | 147 per 10002 | 24 per 1000 | RR 0.16 (0.09 to 0.32) | 624 | ⊕⊝⊝⊝ | This outcome represented the cumulative effect of two manipulations using hyperpronation versus cumulative effect of two manipulations using supination‐flexion. Reassuringly, both procedures when used again resulted in further successful reductions; these were proportionally greater with hyperpronation (64% versus 28%). However, the second attempt should not be considered independently of the first attempt and the characteristics of the children requiring a second attempt may have differed in important ways between the two groups. |
| Ultimate failure | see Comments | see Comments | Although potentially influenced by the initial (allocated) method of manipulation, this outcome reflected various manipulation protocols that stipulated the choice of method used for subsequent attempts. Overall failure at the end of the protocol ranged from 0 to 6 (4.1% of 148 episodes). | |||
| Recurrence (within one month) | see Comments | see Comments | None of the trials reported this outcome. | |||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1. Young children: typically aged under 7 years; mean age around 2 years. 2. Median control group (supination‐flexion) risk across studies 3. Evidence downgraded two levels for very serious risk of bias (selection and detection biases). 4. Evidence downgraded two levels for very serious risk of bias (selection, detection and incomplete outcome biases) and one level for inconsistency (two of the studies reported in favour of pronation, whereas two studies reported no difference between the procedures) 5. Evidence downgraded two levels for very serious risk of bias (and one level for imprecision (there were just 9 events in the hyperpronation group) | ||||||
Background
Description of the condition
Pulled elbow (see Table 1 for synonyms) is a painful condition of acute onset, resulting in sudden loss of function in the affected limb of a child (Hagroo 1995). It is often caused when an adult (or taller person) holds the child by the hand while walking and suddenly pulls the child away from, for example, a dangerous situation, or merely drags the child up a curb or a step (Salter 1971); or when a child pulls away from an adult impulsively. This sudden pull on the arm in young children pulls the head of the radius (one of the two forearm bones) through the ring‐shaped ligament at the elbow which may partially tear and become entrapped between the radial head (top part of the radius) and the capitellum (bottom end of the upper arm bone) (Matles 1967; Stone 1916). This results in subluxation (partial dislocation) of the radial head. Pulled elbow can also be caused by a fall or twist (Irie 2014).
| Radial head subluxation |
| Partial dislocation of the radial head peculiar to children |
| Dislocation of the head of the radius by elongation |
| Annular ligament displacement |
| Partial epiphyseal separation of the radial head |
| Anterior isolated subluxation of the radial head |
| Internal derangement of the elbow |
| Slipped elbow of young children |
| Painful elongation of young children |
| Painful paralysis in young children |
| Rotation syndrome |
| Painful pronation |
| Tamper tantrum elbow |
| Elbow sprain |
| Goyrands’s injury |
| Malaigne’s luxation |
| Gromeyer’s injury |
| Pronatio dolorosa infantum (Chassaignac) |
| Curbstone fracture |
| Supermarket elbow |
| Sunday (afternoon) arm |
| Housemaid’s elbow |
| Nursemaid’s elbow |
| Babysitter’s elbow |
This injury is easily diagnosed on the basis of history and physical examination. The typical presentation is a child who has suddenly cried out with pain and refused to use their arm after a pulling incident, when a snap or click might have been heard (Magill 1954). The arm is held slightly flexed and twisted inward (Asher 1976), with no swelling or bruising (Hardy 1978). Pain is usually felt at the elbow but pain may only be felt at the wrist or shoulder or both (Asher 1976; Griffin 1955). The elbow can usually be flexed and extended, but twisting of the forearm meets resistance and causes pain in the elbow (Hardy 1978).
Pulled elbow is a common injury in young children (Illingworth 1975;Teach 1996). Population‐based incidence rates are scarce but an incidence of 1.2% per year in children aged 0 to 5 years in the Aberdeen city area of Scotland has been described and extrapolated to an annual incidence of 50,000 cases per year in England, Wales and Scotland (Jongschaap 1990). In Dutch general practice, an incidence was reported of 2.4 per 1000 person‐years in children aged 0 to 5 years (Krul 2011). In the United States, the incidence of emergency care visits for pulled elbow was estimated at 2.7 per 1000 children aged 0 to 18 years (Brown 2009). The injury is most common in the left arm, and a median age at presentation between 2 and 2.5 years has been reported in several case series (Hagroo 1995; Illingworth 1975; Irie 2014; Rudloe 2012; Vitello 2014). Salter 1971 reported that the injury is most common in boys but a recent Japanese report of over 1300 cases found no sex difference (Irie 2014), and a review of over 1200 charts from the United States found 60% of cases were girls (Vitello 2014).
Description of the intervention
Pulled elbow is usually treated by manual intervention of the subluxed radial head. Various manoeuvres can be applied. Sometimes, these may be in conjunction with application of manual pressure over the radial head. Two manoeuvres are often recommended. One manoeuvre is supination (Nocton 2004; Thompson 2004), where the forearm is twisted or rotated outwards (palm of child’s hand facing upwards), sometimes followed by flexion of the elbow (Sponseller 2006). While this has become standard practice, it is not always successful. Another manoeuvre is pronation, where the forearm is twisted or rotated inwards (palm of child’s hand facing downwards). Both methods are generally safe, although bruising can occur and they can be painful. We found the terms 'pronation', 'forced pronation' and 'hyperpronation' are often not defined precisely; we have assumed that they are synonyms.
How the intervention might work
The purpose of all manipulative interventions is to reposition both the radial head and the annular ligament, thereby restoring the function of the arm and relieving the pain. In relation to the supination‐flexion manoeuvre, Salter 1971 suggested that "the dramatic relief of pain and restoration of function after reduction of a pulled elbow (...) is explained by the release of the annular ligament from its pinched position and its return to a completely normal position".
As discussed in Bek 2009, the supination‐flexion manoeuvre can be viewed as a reversal of the main mechanism of the injury. However, rotation of the radial head can be done either with supination or pronation and either may be sufficient to reposition the annular ligament to the radial head. Bek 2009 also considered that the supination manoeuvre acts against a greater mechanical block, thus putting the child at greater risk of pain during the procedure.
Why it is important to do this review
Pulled elbow is a common and very painful condition in young children. Although most textbooks recommend supination and flexion of the forearm (as opposed to pronation and other approaches), evidence for this advice is usually not presented. It is therefore important to identify and summarise the evidence in order to find the most effective and painless intervention. This is an update of a Cochrane review first published in 2009 (Krul 2009).
Objectives
To compare the effects (benefits and harms) of the different methods used to manipulate pulled elbow in young children. The primary comparison, as stated a priori, is the pronation method versus the supination method.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled clinical trials or quasi‐randomised (method of allocating participants to a treatment which is not strictly random: e.g. by date of birth, hospital record number, alternation) trials evaluating manipulative interventions for pulled elbow in young children.
Types of participants
We included trials involving young children aged from birth up to adolescence, of either sex, diagnosed with an acute pulled elbow, either primary or recurrent. We excluded trials specifically focusing on older children or adults with this condition, as well as trials of children undergoing interventions for complete dislocation of the proximal radial head.
Types of interventions
We included trials focusing on various manoeuvres, such as pronation or supination of the forearm, used for the manual reduction of subluxation of the proximal radial head in the pulled elbow. We included interventions that took place in any setting (e.g. hospital, general practice, etc).
Types of outcome measures
Primary outcomes
The primary outcome was failure at the first attempt, where success was defined as immediate restoration of a pain‐free, fully functioning arm. Failure was defined by the need for subsequent treatment, usually another attempt at reduction, and lack of spontaneous use of the arm by the child.
Secondary outcomes
When available, we also included results on the following outcomes:
-
pain and distress during the intervention;
-
bruising and other adverse effects;
-
continued failure after second attempt using the same manoeuvre (added as an outcome during 2017 update);
-
ultimate failure (e.g. in terms of the need for more intensive intervention);
-
recurrence (within one month).
Search methods for identification of studies
Electronic searches
We searched the Cochrane Bone, Joint and Muscle Trauma Group Specialised Register (6 September 2016), the Cochrane Central Register of Controlled Trials (CENTRAL) (2016, Issue 8), MEDLINE (including Epub Ahead of Print, In‐Process & Other Non‐Indexed Citations and Ovid MEDLINE Daily) (1946 to 6 September 2016), Embase (1980 to 2016 Week 36), CINAHL (1937 to 6 September 2016), LILACS (Latin American and Caribbean Literature on the Health Sciences) (1982 to 6 September 2016), and PEDro (Physiotherapy Evidence Database) (1929 to 8 September 2016). For this update, the searches were limited to 2011 onwards. Details of the search strategies used for previous versions of the review are given in Krul 2012 and Krul 2009. We did not place any restrictions on language or publication status.
In MEDLINE, the subject‐specific search was combined with the sensitivity‐maximizing version of the Cochrane Highly Sensitive Search Strategy for identifying randomised trials (Lefebvre 2011) (see Appendix 1). Search strategies are also shown for the Cochrane Central Register of Controlled Trials, Embase, CINAHL, LILACS and PEDro (see Appendix 1). Search strategies included all synonyms for pulled elbow.
We searched the ISRCTN registry, World Health Organisation International Clinical Trials Registry platform (WHO ICTRP) and ClinicalTrials.gov for ongoing trials (8 September 2016) (see Appendix 1). We additionally ran a search of the Internet using Google Search (October 2016).
Searching other resources
We screened reference lists of relevant articles. We also contacted all authors who had published a trial on the treatment of the pulled elbow in the last 10 years, asking for additional studies.
Data collection and analysis
Selection of studies
Two review authors (MK and JCW) independently screened the results of the searches to identify studies that appeared to meet the inclusion criteria of the review, based on title and abstract. These studies were obtained in full text and the above two authors independently applied the review inclusion criteria. We resolved disagreements by discussion.
Data extraction and management
Using a data extraction form, two review authors (MK and JCW) independently extracted data from the included trials. MK and JCW entered data into RevMan. We resolved disagreements by discussion. We extracted results from graphs in trial reports when data were not provided in the text or tables. We attempted to contact authors of trials not reported in full journal publications for additional information or data or both.
Assessment of risk of bias in included studies
Two review authors (MK and JCW) independently assessed the included trials using Cochrane's tool for assessing risk of bias (Higgins 2008). Disagreements were resolved by discussion. Titles of journals, names of authors, or supporting institutions were not masked at any stage. The 'Risk of bias' tool incorporates assessment of randomisation (sequence generation and allocation concealment), blinding (of participants, treatment providers and outcome assessors), completeness of outcome data, selection of outcomes reported, and other sources of bias. We considered parent‐rated and clinician‐rated outcomes separately in our assessment of blinding and completeness of outcome data. Our other sources of bias were selection bias, where we assessed the risk of bias from imbalances in key baseline characteristics (age, time from injury, primary, or recurrent injury); and performance bias, where we checked for comparability in the experience of care providers and subsequent provision of treatment interventions, such as slings and advice.
Measures of treatment effect
Quantitative data reported in individual trial reports for the outcomes listed in the inclusion criteria are presented in the text and in the analyses, using risk ratios (RR) with 95% confidence intervals (CI) for dichotomous outcomes. We planned to calculate mean differences (MD) for outcomes, such as pain, that were measured with a visual analogue scale. Where different instruments or measures were used, we planned to use the standardised mean difference (SMD).
Unit of analysis issues
Rarely, children may present with two pulled elbows, which are randomised to one procedure (e.g. Schunk 1990: out of 83 children, one child presented with two pulled elbows). There is no easy way to include this cluster effect in our analysis. When reported data allowed, we planned to perform sensitivity analyses, with and without these children. Children with recurrent pulled elbows within the same study population were treated the same way as children who presented with a pulled elbow for the first time.
Dealing with missing data
Where appropriate, we planned to perform intention‐to‐treat analyses to include all children randomised to the intervention groups. We planned to investigate the effects of dropouts and exclusions by conducting worst and best case scenario analyses. We were alert to the potential mislabelling or non‐identification of standard errors and standard deviations. Unless missing standard deviations could be derived from confidence interval data, we did not assume values in order to present these in the analyses.
Assessment of heterogeneity
We considered whether participant characteristics and the setting of the studies (e.g. emergency departments, general practice) were homogeneous enough from a clinical point of view to allow statistical pooling of the study results. Statistical heterogeneity was assessed by visual inspection of forest plots and calculation of the I² statistic and Chi² test for heterogeneity.
Assessment of reporting biases
If more than 10 studies become available in future, we plan to construct a funnel plot.
Data synthesis
We statistically pooled the results using a fixed‐effect model to estimate summary effect measures and 95% confidence intervals when studies were clinically (e.g. regarding the setting, or age of the children) homogeneous. Where there was significant heterogeneity, we planned to see the effect of using a random‐effects model.
Subgroup analysis and investigation of heterogeneity
We planned subgroup analyses by age (0 to two years; two to five years; six years and above), clinical setting, and whether it was a primary or recurrent subluxation. Should subgroup analysis be done in a future update, we will investigate whether the results of subgroups were significantly different by inspecting the overlap of confidence intervals, and performing the test for subgroup differences available in RevMan.
Sensitivity analysis
Where possible, we performed sensitivity analyses examining various aspects of trial and review methodology, including the inclusion of trials at high risk of bias (specifically, from lack of allocation concealment).
'Summary of findings' tables
We prepared a 'Summary of findings' table for the main comparison (pronation versus supination). We used the GRADE approach to assess the quality of evidence for each of the listed outcomes as high, moderate, low or very low (see section 12.2 of the Cochrane Handbook for Systematic Reviews of Interventions, Schunemann 2011). We presented the following outcomes: failure (second attempt required), pain (preferably during the procedure), adverse effects (e.g. bruising), failure (continued failure after second attempt using same procedure as before), ultimate failure, and recurrence (within one month).
Results
Description of studies
Results of the search
For this update (2011 to September 2016), we screened a total of 239 records from the following databases: Cochrane Bone, Joint and Muscle Trauma Group Specialised Register (5 records); CENTRAL (29), MEDLINE (24), Embase (30), CINAHL (91), PEDro (14), LILACS (0) the WHO ICTRP (9), ISRCTN registry (4) and ClinicalTrials.gov (33). We identified three additional records by checking references of included studies (Quan 1985; Schunk 1990) and a Google search (Asadi 2011).
The results from the previous searches (up to July 2011) are reported in Appendix 2.
The search update resulted in the identification of 11 potentially eligible studies, for which full reports were obtained. Upon study selection, we included five new trials (Asadi 2011 ; Garcia‐Mata 2014; Gunaydin 2013; Guzel 2014; Schunk 1990) and excluded three studies (Dixon 2014; Quan 1985; Ruffing 2014). Dixon 2014 was previously identified as ongoing but after publication in 2014 it has now been excluded. We found one ongoing study (NCT01562535).
Overall, there are now nine included trials (Asadi 2011; Bek 2009; Garcia‐Mata 2014; Green 2006; Gunaydin 2013; Guzel 2014; Macias 1998; McDonald 1999; Schunk 1990), four excluded studies (Dixon 2014; Quan 1985; Ruffing 2014; Taha 2000) and one ongoing trial (NCT01562535). One study, which was only reported as a conference abstract (Vidosavljevic 2006), awaits classification.
A flow diagram summarising the study selection process for this update is shown in Figure 1.

Study flow diagram
Included studies
Details of the individual trials are given in the Characteristics of included studies.
Design
Of the nine included trials, five were described as randomised trials (Garcia‐Mata 2014; Green 2006; Guzel 2014; Macias 1998; McDonald 1999) but Garcia‐Mata 2014 turned out to a quasi‐randomised trial, based on day of admission (Garcia‐Mata 2017). Four other studies were also quasi‐randomised, by either day of month at admission (Gunaydin 2013; Schunk 1990) or date of birth of the child (Asadi 2011; Bek 2009).
Setting
Eight trials were performed in emergency departments or ambulatory care centres. Garcia‐Mata 2014 was performed in a tertiary paediatric orthopaedic unit. One trial was conducted in Spain (Garcia‐Mata 2014), one in Iran (Asadi 2011); three in Turkey (Bek 2009; Gunaydin 2013; Guzel 2014) and four in the USA (Green 2006; Macias 1998; McDonald 1999; Schunk 1990). All were single‐centre trials except for Macias 1998, which was conducted in four centres.
Participants
In total, 906 participants were recruited into the nine trials. The number of children in individual trials ranged from 75 (Guzel 2014) to 150 (Gunaydin 2013). The age range of the participants was 4.5 months to 7 years. The mean age was around 2 years, and, of the 896 children for whom baseline data were available, 58% were girls.
Schunk 1990 recruited three children with two episodes during the study; the duration of the intervals between the episodes was unknown.
Interventions
Eight included trials assigned children to either pronation (all involved hyperpronation) or supination (all were followed by flexion), with the exact methods described in varying and sometimes incomplete detail. Where described or illustrated, the child's elbow was often held at 90 degrees while the manoeuvre was performed; however, the elbow was held in (flexo)extension in Guzel 2014. McDonald 1999 followed pronation with active flexion at the elbow. One study compared two supination methods (Schunk 1990).
Where reported, interventions were carried out by physicians, residents (trainees) or medical students. All trials had a prespecified protocol detailing what were the actions to be taken in the case of initial failure. Six studies (Asadi 2011; Bek 2009; Gunaydin 2013; Guzel 2014; Macias 1998; McDonald 1999) stipulated that the same procedure should be used for the second attempt and the other three studies (Garcia‐Mata 2014; Green 2006; Schunk 1990) stipulated that the alternate procedure should be used.
Studies differed in the waiting time to assess failure and make a second attempt: this was 10 minutes in Green 2006 and Guzel 2014, 15 minutes in Asadi 2011, Bek 2009, Macias 1998 and Schunk 1990, 20 minutes in Gunaydin 2013 and 30 minutes in McDonald 1999. Garcia‐Mata 2014 did not report on this aspect.
Outcomes
All trials reported on success of the procedure, and also of subsequent attempts if the first attempt failed. Five studies defined what success comprised: Asadi 2011 and Bek 2009: "child started to use injured arm" (translation for Asadi 2011); Gunaydin 2013: "technique was deemed successful if the child reached for a toy or candy using the injured arm"; Macias 1998: "return of baseline function"; McDonald 1999: "the subject used the injured arm to reach for a piece of candy or a favorite toy"; and Schunk 1990: "child regained use of the arm".
Five studies also measured pain (Bek 2009; Green 2006; Gunaydin 2013; Guzel 2014; McDonald 1999). However, no outcome data on pain were presented by Bek 2009. Different instruments were used in the other four trials. In Guzel 2014, children who were old enough to communicate rated their pain with a faces pain rating scale. However, pain was not assessed during the procedure. Green 2006 and Gunaydin 2013 only reported on pain when treatment was successful. McDonald 1999 used a four‐point ordinal scale.
No studies reported on adverse effects or recurrence.
Excluded studies
Three trials were excluded because they did not compare different methods of reducing pulled elbow (Dixon 2014; Ruffing 2014; Taha 2000). While the study design in Quan 1985 was unclear, we considered that it was not a randomised or quasi‐randomised trial. Further details are provided in Characteristics of excluded studies.
Ongoing studies
There is one ongoing trial (NCT01562535); see Characteristics of ongoing studies. NCT01562535 compared pronation versus supination, with a planned sample size of 90 participants. Contact with one of the authors (September 2014) revealed that recruitment had not yet started.
Risk of bias in included studies
Figure 2 and Figure 3 summarise our assessment of the risk of bias for the included trials. Comments on the specific items we assessed are given below.

Methodological quality summary: review authors' judgements about each methodological quality item for each included study.
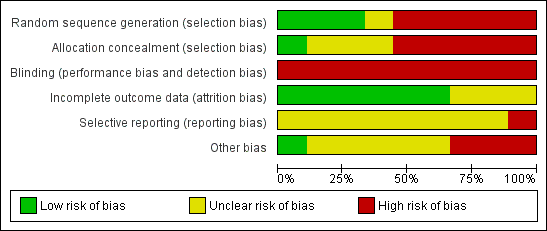
Methodological quality graph: review authors' judgements about each methodological quality item presented as percentages across all included studies.
Allocation
Three studies describing suitable methods of random sequence generation (use of a "randomizations table" or computer generated) were judged at 'low' risk for this item (Guzel 2014; Macias 1998; McDonald 1999). One study did not describe this and was judged to be at 'unclear' risk (Green 2006). Five studies were quasi‐randomised (Asadi 2011; Bek 2009; Garcia‐Mata 2014; Gunaydin 2013; Schunk 1990): treatment being assigned either according to the child's birthday (odd or even) or according to the day of admission. These studies were judged at 'high' risk of selection bias since no random sequence was generated and allocation was not concealed. Macias 1998 reported that allocation was concealed to the attending physician, and so risk of bias was considered low on this item. Allocation concealment was not mentioned in three studies (Green 2006; Guzel 2014; McDonald 1999). The associated risk of selection bias in these trials was judged as 'unclear'.
Blinding
Blinding of either the participants (hardly possible), the treatment providers (not possible) or the outcome assessors (which may be possible) was not done in any of the studies. However, the blinding of child and parents for the manipulation technique was probably not relevant, as they might not be aware of the different techniques nor have any preference. The lack of blinding, especially of treatment providers, was an important source of potential bias in all nine trials.
Incomplete outcome data
The six studies that analysed and reported on all randomised participants were judged at 'low' risk of attrition bias. The other three studies were judged at 'unclear' risk, reflecting concerns over missing data, data discrepancies or both (Green 2006; Guzel 2014; Schunk 1990).
Selective reporting
Trial registration and protocols were not available for any of the included studies. In Green 2006, pain was only recorded for successful attempts and not for the 9 (out of 72) participants with unsuccessful attempts. We considered this trial as having a 'high' risk of selective reporting bias.
Other potential sources of bias
Three trials were considered at 'high' risk of other bias. There was a considerable difference between the study groups in the time elapsed since the injury in Green 2006. Faults in the reporting of Guzel 2014 were of major concern. In Schunk 1990, treatment allocation was not according to protocol in an unknown number of participants, resulting in a considerable baseline imbalance between treatment arms (51:25). Additionally, 11 participants were not treated according to one of the treatment methods.
Lack of information to determine whether there was baseline comparability, discrepancies or small differences between key baseline characteristics were reasons for 'unclear' risk judgements in four trials (Asadi 2011; Bek 2009; Garcia‐Mata 2014; Macias 1998). There was no important imbalance in McDonald 1999.
Care providers and provision of care seemed comparable in the two groups in all trials and we found no differences between groups with respect to additional treatment they received. There was, however, no information on the experience of the attending physicians in reducing a pulled elbow. In some of the studies, at least a part of the interventions were performed by trainees (Bek 2009, Gunaydin 2013; McDonald 1999); training was specifically provided in two of these (Bek 2009; McDonald 1999). We found no differences between groups with respect to additional treatment they received.
Effects of interventions
See: Summary of findings for the main comparison
Comparison 1: Pronation versus supination
Eight studies compared hyperpronation (or forced pronation) with supination‐flexion.
Primary outcome: failure after first attempt
We considered the eight studies were sufficiently similar in terms of study populations and settings to warrant pooling data on failure rates. All eight trials reported fewer failures after hyperpronation (RR 0.35 favouring hyperpronation, 95% CI 0.25 to 0.50; 811 participants, 8 studies; I2 = 25%; low‐quality evidence downgraded two levels for very serious risk of bias; Figure 4, Analysis 1.1).

Forest plot of comparison: 1 Pronation versus supination, outcome: 1.1 Failure: second attempt required.
The failure rates of both methods varied between studies: for hyperpronation these ranged from 4.4% in Gunaydin 2013 to 20.9% in McDonald 1999; and for supination and flexion these ranged from 16.2% in Green 2006 to 34.2% in Guzel 2014. Based on the pooled data, with a mean failure rate of 26.4% when using the supination method (thus around one in four first attempts fail) and 9.2% when using the hyperpronation method, the number needed to treat (NNT) for the hyperpronation method was 6 (95% CI 5 to 9). This means that six children would need to be treated with the hyperpronation method rather than the supination‐flexion method to avoid one additional failure at the first attempt.
Subgroup and sensitivity analyses
Our planned subgroup analyses by age (0 to two years; two to five years; six years and above), clinical setting, and whether the subluxation was primary or recurrent were not possible due to lack of data.
For our primary outcome, we performed several sensitivity analyses, which tested the effects of excluding data from the four quasi‐randomised studies (Asadi 2011; Bek 2009; Garcia‐Mata 2014; Gunaydin 2013); excluding Green 2006, which was potentially confounded by the difference in mean time from injury between the two groups; and excluding data from the 17 children in Garcia‐Mata 2014 who had already undergone one or more manipulations, all using the supination‐flexion method before entering the main study. None of these analyses materially changed the findings, which continued to favour hyperpronation (Table 2).
| Sensitivity analysis | Results | NNT |
| Removal of quasi‐RCTs | RR 0.47, 95% CI 0.30 to 0.73; 370 participants; I2 = 13% | 8, 95% CI 5 to 17 |
| Removal of Green 2006 (baseline imbalance) | RR 0.34, 95% CI 0.24 to 0.49; 739 participants; I2 = 35% | 6, 95% CI 5 to 8 |
| Removal of 17 participants with prior manipulation in Garcia‐Mata 2014) | RR 0.35, 95% CI 0.24 to 0.50; 794 participants; I2 = 28% | 7, 95% CI 5 to 10 |
Secondary outcomes
Pain and distress
Pain was measured in five of the trials addressing this comparison (Bek 2009; Green 2006; Gunaydin 2013; Guzel 2014; McDonald 1999). However, they all used very different measures and Bek 2009, which did not state how pain had been measured, did not present separate pain data, instead combining it with clinician's perceived ease of the manoeuvre. Data for pain were not available for pooling. The pain results in the individual trials are summarised below.
In Green 2006, pain was only assessed for successful attempts. Green 2006 found that the difference in the visual analogue scores (10 cm scale) favoured pronation. The difference was 0.7 cm as perceived by physicians (reported P = 0.11); 1.0 cm by nurses (reported P = 0.03) and 1.7 cm by parents (reported P = 0.04). This last finding exceeded the minimal clinically significant difference of 1.3 cm stipulated by the trialists.
McDonald 1999 reported, using a four‐point ordinal score, that the treating physicians perceived the pronation method to be significantly less painful than supination (reported P = 0.013, with an estimated 1‐point difference), but that parental pain scores during reduction were similar for both procedures (reported P = 0.169).
Gunaydin 2013 used the Modified Children's Hospital of Eastern Ontario Pain Scale before, during, and after the procedure. Pain scale values during and after the procedure were not different between the two groups; reported P values were 0.801 (during) and 0.914 (after the procedure).
Guzel 2014 used the Wong‐Baker Faces Pain Rating Scale in children who were able to communicate, and the Face, Legs, Cry, Consolability Scale to be scored by research assistants if children were not able to communicate. Pain was assessed before and after the procedure, but not during the procedure. No differences were found after the procedure (reported P = 0.462).
Overall, two out of four studies found that pronation may be less painful, whereas two found no difference between the two procedures. The quality of the evidence for this outcome was judged to be very low due to very serious risk of bias (notably, selection bias, lack of assessor blinding and incomplete data) and serious inconsistency.
Bruising and other adverse effects
Bruising and other adverse effects were not reported in any of the studies.
Failure after second attempt using the same procedure
All studies reported failure after the second attempt, but the same procedure as in the first attempt was used only in six trials. The cumulative effect of two manipulations using hyperpronation again resulted in fewer reduction failures than two manipulations using supination‐flexion (RR 0.16, 95% CI 0.09 to 0.32; 624 participants; 6 studies; I2 = 0%; very low‐quality evidence downgraded two levels for very serious risk of bias and one level for serious imprecision; Analysis 1.2). Hyperpronation, when used for a second time, resulted in a greater percentage of successful reductions (70%: 21/30 primary failures) than did supination‐flexion (30%; 28/92 primary failures) in these six studies. Thus, while both procedures were successful on the second attempt, a second attempt using hyperpronation again appeared more effective than one using supination‐flexion.
Ultimate failure
Ultimate failure was reported in most studies. However, since the study protocols differed with respect to what to do after the first attempt failed and after any subsequent failure, it is inappropriate to attribute this outcome to the first‐used allocated manipulation method. This varied from no ultimate failures after the end of the manipulation protocol (Bek 2009; Gunaydin 2013) to six ultimate failures (4.1% of 148 participants) in McDonald 1999; we could not determine this outcome from Asadi 2011 and Guzel 2014. These data are summarised in Table 3.
| Study | Outcome definition | Overall no. of failures / no. episodes | Protocol |
| Failure after 4 attempts | Not reported | 4 attempts, cross‐over on 3rd attempt | |
| Failure after 3 attempts | 0 / 66 (0%) | 3 attempts, cross‐over on 3rd attempt | |
| Failure after 3 attempts | 3 / 115 (2.6%) | 3 attempts, cross‐over on 2rd attempt original method for 3rd attempt | |
| Failure after 2 attempts | 2 / 75 (2.7%) | 2 attempts, cross‐over on 2nd attempt | |
| Failure after 3 attempts | 0 / 150 (0%) | 3 attempts, cross‐over on 3rd attempt | |
| Failure after 3 attempts | Not reported | 3 attempts, cross‐over on 3rd attempt | |
| Failure after 4 attempts | 1 / 90 (1.1%) | 4 attempts, cross‐over on 3rd attempt order same for 4th attempt | |
| Failure after 3 attempts | 6 / 148 (4.1%) | 3 attempts, cross‐over on 3rd attempt |
Recurrence (within one month)
Recurrence was not reported as an outcome in all eight studies. Of note, however, is that five of the 85 children included by Macias 1998 were included twice, due to a recurrence. Only one of these recurred within one month (a few days).
Comparison 2: Supination‐extension versus supination‐flexion
This comparison was made only in Schunk 1990, a seriously flawed and inadequately‐reported quasi‐randomised trial reporting outcome data for 76 episodes (72 to 76 children). The manipulation protocol for Schunk 1990 involved cross‐over if the first attempt failed after 15 minutes.
Primary outcome: failure after first attempt
In the group treated with supination and extension, eight of 25 repositions failed. In the group treated with supination and flexion, ten of 51 repositions failed. An exploratory analysis showed no clear difference between the two reduction methods: RR 1.63, 95% CI 0.74 to 3.62; very low‐quality evidence reflecting downgrading for very serious risk of bias and serious imprecision; see Analysis 2.1).
Secondary outcomes
Schunk 1990 did not report on pain and distress, adverse effects or recurrence within one month. The second attempt, using the opposite manoeuvre, failed in 10 children. Ultimate failure occurred in three children (3.9% of 76 episodes); all three received a splint and left the emergency department without full use of their injured arm. All three children had normal use of their arm at subsequent orthopaedic follow‐up. Notably, Schunk 1990 included three children with two episodes during the study; there was no information on timing.
Discussion
Summary of main results
Eight of the nine trials included in this review compared hyperpronation with supination‐flexion for the primary reduction method for treating pulled elbow (subluxation of the radial head) in young children, all of whom were younger than seven years old. All seven trials were at high risk of bias. The results for this comparison are summarised in summary of findings Table for the main comparison. There was low‐quality evidence (downgraded two levels for very serious risk of bias) of a significantly lower risk of failure at first attempt (our primary outcome) after manipulation with hyperpronation than with supination‐flexion (RR 0.35; 95% CI 0.25 to 0.50; 811 participants, 8 trials). Based on an illustrative risk of 268 failures at first attempt per 1000 children treated using supination‐flexion, this amounted to 174 fewer failures per 1000 children treated using hyperpronation (95% CI 134 to 201 fewer). Based on risk difference data, we also estimated a number needed to treat of 6 (95% CI 5 to 8); this means that six children would need to be treated with the hyperpronation method rather than the supination‐flexion method to avoid one additional failure at the first attempt.
The very low‐quality evidence (from four studies; downgraded three levels for very serious risk of bias and serious inconsistency) for pain during or after manipulation means that it is uncertain whether there is or is not a difference between pronation and supination‐flexion. There was very low‐quality evidence from six studies that repeat pronation may be more effective than repeat supination‐flexion for the second attempt. The remaining outcomes were either not reported (adverse effects, recurrence) or unsuitable for pooling (ultimate failure). Ultimate failure, reported for overall population only, because of the differences in the study protocols with respect to what to do after the first attempt failed, ranged from no ultimate failures in two studies to six failures (4.1% of 148 episodes) in one study.
The single quasi‐randomised trial (data for 76 episodes) comparing two methods of supination (supination followed by extension versus supination followed by flexion) was at very serious risk of bias. It provided very low‐quality evidence (downgraded three levels for very serious risk of bias and serious imprecision) of no clear difference in failure at first attempt between the two methods.
Overall completeness and applicability of evidence
The objective of this review was to compare the effectiveness of, and pain associated with, different methods for manipulating the pulled elbow in young children. Eight of nine included studies addressed our stated primary comparison of pronation versus supination methods. We believe this review provided a relevant answer to the question of effectiveness of these basic procedures, but the evidence was still incomplete and susceptible to bias. In particular, there was insufficient or no evidence on pain, adverse effects or recurrence. Trial settings, care providers and the study populations were comparable in the seven trials. Also, the study protocols with respect to procedure and waiting times appeared to be realistic and applicable in clinical practice. Hence, the findings of these trials would apply more generally. However, our planned subgroup analyses by age (0 to two years; two to five years; six years and above) and by clinical setting were not possible.
The single trial comparing two methods of supination was of very low methodological quality.
Quality of the evidence
Overall, the quality of evidence for individual outcomes was either low ('further research is very likely to have an important impact on our confidence in the estimate of effect') or very low ('we are very uncertain about the estimate'). The main reason for downgrading the quality of the evidence by two levels for all outcomes was the very serious risk of bias due to selection bias (the majority of the trials were quasi‐randomised) and performance and detection biases reflecting the lack of blinding. We did not downgrade for publication bias because the number of included studies was too small to assess this.
As noted in summary of findings Table for the main comparison, we downgraded the evidence for pain one further level for serious inconsistency and the evidence for continued failure after second attempt using the same procedure as before by one further level for serious imprecision. For the study comparing two supination methods, we downgraded the evidence by one further level for serious imprecision.
Potential biases in the review process
Although our search was extensive, we cannot exclude the possibility that we have missed relevant evidence. We tried to contact the authors of the original studies but only two replied and in only one of these did it result in clarification of methods. Our search of grey literature, the pursuit of trials listed in clinical trial registers and the fact that we applied no restrictions based on language or publication status aimed to avoid publication bias, location bias, citation bias, language bias and outcome reporting bias. Given there were only eight studies available addressing the same comparison, we were unable to explore whether publication bias could have occurred by constructing a funnel plot.
Agreements and disagreements with other studies or reviews
We found four other reviews. Lewis 2003, which only included the studies by McDonald 1999 and Macias 1998, concluded that pronation with or without elbow flexion should be "the first line method of reduction for pulled elbows". Lewis 2003 pointed out that lack of blinding was a key weakness of these two trials. A later Dutch review (Knuistingh Neven 2008), which included the studies by Green 2006; Macias 1998; McDonald 1999 but also Taha 2000 (which we excluded), also concluded that the pronation method was more effective than the supination method. More recently, Curtis 2012 published a systematic review, discussing the limitations of the few randomised trials that have been performed. Bexkens 2017 included seven studies which were also included in this update but did not include Asadi 2011. The pooled results and conclusions of Bexkens 2017 are very much in line with those in our review update.
Several textbooks still suggest the supination method as the only or preferred method (e.g. Nocton 2004; Thompson 2004; Bachman 2010; Erickson 2016). This is not supported by the findings of this systematic review, which provided some evidence that pronation might be more effective and less painful than supination. Other textbooks also mentioned hyperpronation (Burg 2008; Joffe 2010). Lucas 2016 described hyperpronation (also labelled 'superpronation') as the preferred method. A recent instructional paper also mentioned both procedures (Aylor 2014). One excluded study (Dixon 2014) compared trained nurses (using hyperpronation at the first attempt) with physicians (who used either hyperpronation or supination‐flexion). It is notable that hyperpronation was selected as the method for the nurses in this study, perhaps indicating some perception of it being an easier method.

Methodological quality summary: review authors' judgements about each methodological quality item for each included study.
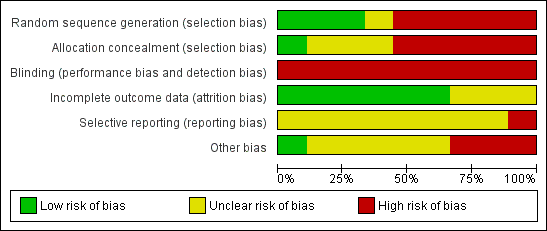
Methodological quality graph: review authors' judgements about each methodological quality item presented as percentages across all included studies.

Forest plot of comparison: 1 Pronation versus supination, outcome: 1.1 Failure: second attempt required.
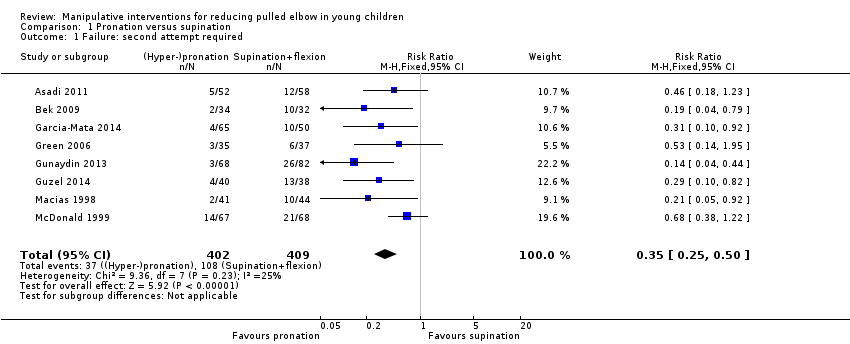
Comparison 1 Pronation versus supination, Outcome 1 Failure: second attempt required.

Comparison 1 Pronation versus supination, Outcome 2 Failure: continued failure after second attempt with same procedure.

Comparison 2 Supination and extension versus supination then flexion, Outcome 1 Failure: second attempt required.
| Pronation compared with supination reduction techniques for pulled elbow in young children | ||||||
| Patient or population: Children with pulled elbow1 Settings: Emergency departments, ambulatory care centres or orthopaedic units Intervention: Pronation (all were hyperpronation) for first manipulation Comparison: Supination (all included flexion) for first manipulation | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Supination‐flexion | Hyperpronation | |||||
| Failure: second attempt required | 268 per 10002 | 94 per 1000 (67 to 134) | RR 0.35 (0.25 to 0.50) | 811 | ⊕⊕⊝⊝ | |
| Pain (preferably during the procedure) | see Comments | see Comments | see Comments | ⊕⊝⊝⊝ | Data for this outcome are incomplete and were measured in very different ways in four studies. | |
| Adverse effects (e.g. bruising) | see Comments | see Comments | None of the trials reported this outcome. | |||
| Failure: continued failure after second attempt using same procedure as before | 147 per 10002 | 24 per 1000 | RR 0.16 (0.09 to 0.32) | 624 | ⊕⊝⊝⊝ | This outcome represented the cumulative effect of two manipulations using hyperpronation versus cumulative effect of two manipulations using supination‐flexion. Reassuringly, both procedures when used again resulted in further successful reductions; these were proportionally greater with hyperpronation (64% versus 28%). However, the second attempt should not be considered independently of the first attempt and the characteristics of the children requiring a second attempt may have differed in important ways between the two groups. |
| Ultimate failure | see Comments | see Comments | Although potentially influenced by the initial (allocated) method of manipulation, this outcome reflected various manipulation protocols that stipulated the choice of method used for subsequent attempts. Overall failure at the end of the protocol ranged from 0 to 6 (4.1% of 148 episodes). | |||
| Recurrence (within one month) | see Comments | see Comments | None of the trials reported this outcome. | |||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1. Young children: typically aged under 7 years; mean age around 2 years. 2. Median control group (supination‐flexion) risk across studies 3. Evidence downgraded two levels for very serious risk of bias (selection and detection biases). 4. Evidence downgraded two levels for very serious risk of bias (selection, detection and incomplete outcome biases) and one level for inconsistency (two of the studies reported in favour of pronation, whereas two studies reported no difference between the procedures) 5. Evidence downgraded two levels for very serious risk of bias (and one level for imprecision (there were just 9 events in the hyperpronation group) | ||||||
| Radial head subluxation |
| Partial dislocation of the radial head peculiar to children |
| Dislocation of the head of the radius by elongation |
| Annular ligament displacement |
| Partial epiphyseal separation of the radial head |
| Anterior isolated subluxation of the radial head |
| Internal derangement of the elbow |
| Slipped elbow of young children |
| Painful elongation of young children |
| Painful paralysis in young children |
| Rotation syndrome |
| Painful pronation |
| Tamper tantrum elbow |
| Elbow sprain |
| Goyrands’s injury |
| Malaigne’s luxation |
| Gromeyer’s injury |
| Pronatio dolorosa infantum (Chassaignac) |
| Curbstone fracture |
| Supermarket elbow |
| Sunday (afternoon) arm |
| Housemaid’s elbow |
| Nursemaid’s elbow |
| Babysitter’s elbow |
| Sensitivity analysis | Results | NNT |
| Removal of quasi‐RCTs | RR 0.47, 95% CI 0.30 to 0.73; 370 participants; I2 = 13% | 8, 95% CI 5 to 17 |
| Removal of Green 2006 (baseline imbalance) | RR 0.34, 95% CI 0.24 to 0.49; 739 participants; I2 = 35% | 6, 95% CI 5 to 8 |
| Removal of 17 participants with prior manipulation in Garcia‐Mata 2014) | RR 0.35, 95% CI 0.24 to 0.50; 794 participants; I2 = 28% | 7, 95% CI 5 to 10 |
| Study | Outcome definition | Overall no. of failures / no. episodes | Protocol |
| Failure after 4 attempts | Not reported | 4 attempts, cross‐over on 3rd attempt | |
| Failure after 3 attempts | 0 / 66 (0%) | 3 attempts, cross‐over on 3rd attempt | |
| Failure after 3 attempts | 3 / 115 (2.6%) | 3 attempts, cross‐over on 2rd attempt original method for 3rd attempt | |
| Failure after 2 attempts | 2 / 75 (2.7%) | 2 attempts, cross‐over on 2nd attempt | |
| Failure after 3 attempts | 0 / 150 (0%) | 3 attempts, cross‐over on 3rd attempt | |
| Failure after 3 attempts | Not reported | 3 attempts, cross‐over on 3rd attempt | |
| Failure after 4 attempts | 1 / 90 (1.1%) | 4 attempts, cross‐over on 3rd attempt order same for 4th attempt | |
| Failure after 3 attempts | 6 / 148 (4.1%) | 3 attempts, cross‐over on 3rd attempt |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Failure: second attempt required Show forest plot | 8 | 811 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.35 [0.25, 0.50] |
| 2 Failure: continued failure after second attempt with same procedure Show forest plot | 6 | 624 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.16 [0.09, 0.32] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Failure: second attempt required Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |

