Restauraciones con amalgama unidas con adhesivos versus sin adhesivos para la caries dental
Resumen
Antecedentes
La caries dental es una de las enfermedades más frecuentes que aqueja a la humanidad, y se ha calculado que afecta hasta un 80% de personas en países de ingresos altos. La caries perjudica y destruye progresivamente los tejidos del diente, incluida la pulpa dental (nervio), y como consecuencia los dientes se debilitan, presentan un aspecto antiestético y su función se deteriora. El tratamiento de las lesiones de la caries dental, que progresan a través de la dentina y han causado la formación de una cavidad, incluye la provisión de restauraciones dentales (rellenos). Esta revisión actualiza la versión anterior publicada en 2009.
Objetivos
Evaluar los efectos de la unión con adhesivos en el rendimiento clínico y la longevidad de las restauraciones con amalgamas dentales.
Métodos de búsqueda
Se realizaron búsquedas en el Registro Especializado de Ensayos Controlados del Grupo Cochrane de Salud Oral (Cochrane Oral Health Group) (hasta el 21 de enero de 2016), el Registro Cochrane Central de Ensayos Controlados (Cochrane Central Register of Controlled Trials, CENTRAL) ( The Cochrane Library2015, número 12), MEDLINE vía OVID (1946 hasta el 21 de enero de 2016) y EMBASE vía OVID (1980 hasta el 21 de enero de 2016). También se realizaron búsquedas en el registro de ensayos de los Institutos Nacionales de Salud de los Estados Unidos (http://clinicaltrials.gov) y en la Plataforma de Registro de Ensayos Clínicos Internacionales de la OMS (www.who.int/ictrp/search/en) (ambas hasta el 21 de enero de 2016) para encontrar ensayos en curso. No se impusieron restricciones de idioma ni de fecha de publicación en la búsqueda en las bases de datos electrónicas.
Criterios de selección
Ensayos controlados aleatorizados que comparaban restauraciones con amalgama unidas con adhesivos versus restauraciones tradicionales sin adhesivos en preparaciones convencionales que utilizan la retención deliberada, en adultos con molares y premolares permanentes adecuados para restauraciones con amalgama de Clase I y II solamente.
Obtención y análisis de los datos
Dos revisores de forma independiente examinaron los documentos, extrajeron la información y evaluaron el riesgo de sesgo en el estudio incluido.
Resultados principales
Se incluyó un ensayo con 31 pacientes que recibieron 113 restauraciones. A los dos años, 50 de las 53 restauraciones del grupo no vinculado sobrevivieron, y 55 de las 60 restauraciones vinculadas sobrevivieron con cinco no contabilizadas en el seguimiento. La sensibilidad posterior a la inserción no fue significativamente diferente (P > 0,05) en la línea de base o en el seguimiento de dos años. No se informaron fracturas del tejido dental y no hubo diferencias significativas entre los grupos o pares de restauraciones en cuanto a su adaptación marginal (p > 0,05).
Conclusiones de los autores
No hay evidencia para afirmar o refutar una diferencia en la supervivencia entre las restauraciones con amalgama unidas o no unidas con adhesivos. Esta revisión sólo encontró un ensayo no informado. Este ensayo no halló diferencias significativas en el rendimiento clínico de las restauraciones con amalgama unidas con adhesivos, de tamaño moderado, en cuanto a su tasa de supervivencia y su integridad marginal, en comparación con las amalgamas no unidas con adhesivos, durante un período de dos años. En vista de la ausencia de evidencia sobre un beneficio adicional de la amalgama unida con adhesivo, en comparación con la amalgama sin adhesivo, es importante que los odontólogos tengan presente los costes extra que puede tener.
PICO
Resumen en términos sencillos
Restauraciones con amalgama unidas con adhesivos o sin adhesivos para la caries dental
Pregunta de la revisión
¿Añadir adhesivo diseñado para unir los empastes de amalgama dental a los dientes hace que los empastes funcionen mejor y duren más que los empastes sin él?
Antecedentes
La caries dental es un problema frecuente que afecta tanto a niños como adultos. Las caries se forman en los dientes por la acción del ácido producido por las bacterias presentes en la placa dental o el biofilm.
Pueden utilizarse varias técnicas y diversos materiales para restaurar u obturar los dientes afectados por la caries. Uno de los materiales de relleno más utilizados y comparativamente más baratos es la amalgama dental (una mezcla de partículas de mercurio y aleaciones metálicas). Los autores de la revisión procuraron evaluar el beneficio adicional de utilizar un adhesivo para adherir la amalgama a la estructura dental para ver si los empastes adheridos durarían más tiempo y funcionarían mejor.
Características de los estudios
La evidencia de esta revisión, realizada por los autores de la Grupo Cochrane de Salud Oral, están actualizadas al 21 de enero de 2016. Se incluyó un ensayo con 31 participantes (21 hombres, 10 mujeres) que recibieron 113 restauraciones. El estudio tuvo lugar en el Reino Unido en un ambiente de hospital dental universitario. Se eligieron participantes que eran aptos para un tratamiento dental de rutina. La comparación realizada fue entre dientes de la misma persona en lados opuestos de la boca, uno tratado con la técnica de unión, el otro sin ella. A los dos años no se encontró ninguna diferencia.
Resultados clave
Sólo un estudio, que proporcionó información limitada, demostró que en el caso de los empastes de tamaño mediano no había diferencia de sensibilidad entre los empastes adheridos y los no adheridos después de su colocación y que la adhesión de la amalgama al diente no tenía ningún efecto en la supervivencia del empaste en un período de dos años. En vista de la ausencia de evidencia sobre un beneficio adicional de la amalgama unida con adhesivo, en comparación con la amalgama sin adhesivo, es importante que los odontólogos tengan presente los costes extra que puede tener.
Existe una amplia gama de agentes adhesivos desarrollados a lo largo de varios años que están disponibles para su uso por parte de los dentistas. Por lo tanto, es muy decepcionante que haya tanta falta de ensayos adecuados de su efectividad.
Calidad de la evidencia
Sólo se incluyó un estudio que no aporta evidencia suficiente de que las restauraciones de amalgama unidas con adhesivos tengan un mejor rendimiento que las restauraciones de amalgama no unidas con adhesivos cuando se les hace un seguimiento durante dos años.
La calidad de la evidencia es baja. Además, el entorno de la clínica dental universitaria puede significar que los participantes no son representativos de la población general y que el tratamiento ofrecido no es típico de eso en la práctica dental general, por lo que los resultados pueden no ser generalizables.
Authors' conclusions
Summary of findings
| Adhesive bonding for restorations of dental amalgam | ||||||
| Patient or population: Patients with restorations of dental amalgam | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | Number of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Adhesive bonding | |||||
| Survival of the restoration | See comment | See comment | Not estimable | 31 | ⊕⊕⊝⊝ | Of the adhesively bonded 55/60 were a success, 5 were unavailable at 24‐month follow‐up Of the non‐bonded 50/53 were a success, and the remaining 3 a failure |
| Post‐insertion sensitivity or pain assessed by a validated pain scale ‐ not measured | See comment | See comment | Not estimable | ‐ | See comment | No study addressed this outcome |
| Secondary caries, as diagnosed clinically ‐ not measured | See comment | See comment | Not estimable | ‐ | See comment | No study addressed this outcome |
| Marginal deterioration of the restoration and fracture of the remaining tooth tissue | Study population | Not estimable | 31 | ⊕⊕⊝⊝ | Marginal adaptation USPHS Alpha ratings: Occlusal; adhesively bonded from 97 at baseline to 96, non‐bonded from 94 at baseline to 88 Proximal; adhesively bonded from 88 at baseline to 91, non‐bonded from 87 at baseline to 82 | |
| See comment | See comment | |||||
| Economic data: direct costs of materials and any reported associated indirect costs ‐ not measured | See comment | See comment | Not estimable | ‐ | See comment | No study addressed this outcome |
| Adverse effects: any event for which the causal relationship between the event and the amalgam restoration is at least a reasonable possibility ‐ not measured | See comment | See comment | Not estimable | ‐ | See comment | No study addressed this outcome |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Attrition bias | ||||||
Background
Dental caries (tooth decay) is one of the commonest diseases which afflicts mankind, and has been estimated to affect up to 80% of people in high‐income countries (Chadwick 2001).
Description of the condition
Caries is a term used to denote both lesions of caries and the carious process, the demineralisation of enamel, dentine and cementum caused by organic acids produced by acidogenic bacteria in dental plaque. Across the world the incidence and severity of caries is strongly associated with social deprivation, with a focus in children and, increasingly, older people who have retained a number of their natural teeth (WHO 2005). Despite caries being preventable through, in particular, effective oral hygiene, dietary control and the use of anticariogenic agents, notably fluoride in toothpastes and when administered systemically, it is anticipated to remain a common disease for the foreseeable future, with the prevalence being greatest in many of the low‐ and middle‐income countries (Yee 2002).
Consequences of caries
Caries adversely affects and progressively destroys the tissues of the tooth, including the dental pulp (nerve), leaving teeth unsightly, weakened and with impaired function, subsequent to the disease process causing parts of the teeth to cavitate and fracture under loading. Carious teeth can become painful when advancing lesions of caries cause pulpal inflammation. If untreated pulpal inflammation becomes irreversible and the pulp dies, with the possibility of infection passing out of the tooth to cause a dental abscess.
Caries is an opportunistic, infectious disease responsible for a great deal of human suffering. Where dental healthcare systems exist, caries is responsible for a substantial financial burden which increases with recurrence of the disease process (Burke 2001; Yee 2002).
Description of the intervention
Treatment
The treatment of lesions of dental caries, which are progressing through dentine and have caused the formation of a cavity, involves the provision of dental restorations (fillings). Restorations can be of many different forms and various materials, with variations in technique sensitivity and durability.
Dental amalgam
Despite many important developments in dental materials and minimally interventive techniques, in many parts of the world most restorations tend to continue to be of a traditional form and of the material most widely used in dentistry over at least the last 100 years i.e. dental amalgam (Berry 1998). This material, a combination of mercury and alloy particles of different compositions and form is cost effective in the management of dental caries, but lacking many of the features of an ideal dental filling material (Downer 1999; Mackert 2004).
A major limitation of dental amalgam, other than its poor appearance, is its inability to bond to remaining tooth tissues, and thereby form a seal between restoration and tooth. This limitation is to a variable extent countered by dental amalgam corrosion products building up in the restoration/tooth interface, and thereby helping to limit the negative effects of the interfacial percolation of oral fluids, including cariogenic bacteria and their food substrate of fermentable carbohydrates (Ben‐Amar 1995).
How the intervention might work
Bonding
With the development of systems to bond tooth‐coloured dental filling materials to calcified tooth tissues (enamel and dentine), there were investigations to determine if bonding systems could be applied to dental amalgams, and thereby address certain limitations in the use of such metallic materials (Turner 1995). These investigations, which included a small number of short duration clinical studies were considered, at the turn of the century, to indicate that there was evidence accruing clinically that the bonding of dental amalgams could be used, despite its technique sensitivity and technical difficulties, to extend the range of usage of dental amalgam to non‐retentive conservative preparations and, toward the other extreme, as an adjunct to other forms of retention in large compound (complex) restorations (Setcos 2000) thereby offering opportunity to conserve sound tooth structure.
Why it is important to do this review
Given the above and the recognition that dental amalgams will, for the foreseeable future, remain the material of choice for certain restorations in posterior teeth, including the replacement therapy for existing amalgam fillings (SCENIHR 2007), it is considered important to undertake a systematic review of recent clinical findings on adhesively bonded versus non‐bonded amalgam restorations in the management of dental caries. This review builds on earlier non‐Cochrane reviews which assessed the longevity of routine dental restorations (Chadwick 2001; Downer 1999), and whilst there are differing views over the point at which restorations may require replacement there is a consensus that the survival time for amalgam fillings is within a range of 10 to 20 years. This review updates the previous version published in 2009 (Fedorowicz 2009).
Objectives
To assess the effects of adhesive bonding on the in‐service performance and longevity of dental amalgam restorations.
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials (RCTs) to include paired tooth and split‐mouth study designs, with a minimum length of follow‐up of two years. The unit of randomisation considered was either at the level of the tooth or the individual patient.
Only studies that assessed the in‐service performance and longevity of restorations using clearly defined criteria e.g. United States Public Health Service (USPHS) or any recognised modifications to these criteria were included in the review (Hickel 2007).
Types of participants
Adults and adolescents with permanent posterior molar and premolar teeth suitable for Class I and II, but excluding Class V, amalgam restorations.
Types of interventions
Adhesively bonded versus traditional non‐bonded amalgam restorations in conventional preparations utilising deliberate retention. All types of bonding agents were considered.
Types of outcome measures
The main outcome of interest was the longevity/survival of the restorations as assessed by clinical examination and defined by the USPHS criteria, Ryge criteria or modifications of these scales (Ryge 1981). Longevity represents the survival rate of the restorations at specified time points or at completion of the study. Failure is defined as the total mechanical failure of the restoration i.e. mobility, fracture, missing in part or in total or the death of the pulp and/or catastrophic failure leading to the extraction of the tooth.
Although we intended categorising outcome data at defined time points, in order that we capture data on early failures there was no minimum follow‐up.
Primary outcomes
The nature of the primary outcome data (survival/failure) sought in this review was principally dichotomous.
-
Survival of the restoration: longevity/survival to defined time points yearly up to a maximum of 10 years and if available: time‐to‐first‐event and failure‐free survival presented as the proportion of restorations placed that survived after a designated period of time of 1, 2, 5 and 10 years.
Secondary outcomes
-
Post‐insertion sensitivity or pain assessed by a validated pain scale.
-
Secondary caries, as diagnosed clinically.
-
Marginal deterioration of the restoration and fracture of the remaining tooth tissue.
-
Economic data: direct costs of materials and any reported associated indirect costs.
-
Adverse effects: any event for which the causal relationship between the event and the amalgam restoration is at least a reasonable possibility.
Search methods for identification of studies
Electronic searches
For the identification of studies included or considered for this review, we developed detailed search strategies for each database searched. These were based on the search strategy developed for MEDLINE (Ovid) but revised appropriately for each database. The search strategy used a combination of controlled vocabulary and free text terms and was linked with the Cochrane Highly Sensitive Search Strategy (CHSSS) for identifying randomised trials (RCTs) in MEDLINE: sensitivity maximising version (2008 revision) as referenced in Chapter 6.4.11.1 and detailed in box 6.4.c of the Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011) (Higgins 2011). Details of the MEDLINE search are provided in Appendix 3. The search of EMBASE was linked to the Cochrane Oral Health Group filter for identifying RCTs.
-
The Cochrane Oral Health Group Trials Register (to 21 January 2016) (Appendix 1).
-
The Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library 2015, Issue 12) (Appendix 2).
-
MEDLINE via Ovid (1946 to 21 January 2016) (Appendix 3).
-
EMBASE via Ovid (1980 to 21 January 2016) (Appendix 4).
No restrictions were placed on the language or date of publication when searching the electronic databases.
Searching other resources
We searched the following databases for ongoing trials (Appendix 5):
-
US National Institutes of Health Trials Register (http://clinicaltrials.gov) (to 21 January 2016);
-
the WHO International Clinical Trials Registry Platform (http://apps.who.int/trialsearch/default.aspx) (to 21 January 2016).
We examined the reference lists of relevant articles and contacted the investigators of the included study by electronic mail to ask for details of additional published and unpublished trials. We did not handsearch any journals.
Data collection and analysis
Selection of studies
Two review authors (Anirudha Agnihotry (AA) and Zbys Fedorowicz (ZF)) independently assessed the abstracts of studies resulting from the searches. We obtained full copies of all relevant and potentially relevant studies, those appearing to meet the inclusion criteria, and for which there were insufficient data in the title and abstract to make a clear decision. The full text papers were assessed independently by the two review authors and any disagreement on the eligibility of included studies was resolved through discussion and consensus or if necessary through a third party (Mona Nasser (MN)). We excluded all irrelevant records and noted details of the studies and the reasons for their exclusion in the Characteristics of excluded studies table in RevMan 5 (RevMan 2014).
Data extraction and management
We entered study details into the Characteristics of included studies table in RevMan 5 and collected outcome data using a pre‐determined form designed for this purpose.
Data were extracted independently and in duplicate by two review authors (ZF and MN) and only included if there was a consensus.
The following details were extracted.
-
Trial methods: (a) method of allocation; (b) masking of participants, trialists and outcome assessors; (c) exclusion of participants after randomisation and proportion and reasons for losses at follow‐up.
-
Participants: (a) country of origin and location: private clinic or academic institute; (b) sample size; (c) age; (d) sex; (e) inclusion and exclusion criteria; (f) location and type of cavity (Class I or II); (g) cavity size.
-
Intervention: (a) type, amalgam alloy and bonding material and method of cure; (b) length of time in follow‐up; (c) failure and reasons for failure if reported.
-
Control: (a) type of amalgam alloy; (b) length of time in follow‐up; (c) failure and reasons for failure if reported.
-
Outcomes: (a) primary and secondary outcomes mentioned in the Types of outcome measures section of this review.
If stated, the sources of funding of any of the included studies were recorded.
The review authors used this information to help them assess heterogeneity and the external validity of any included trials.
Assessment of risk of bias in included studies
Each review author graded the selected trial using a simple contingency form and followed the domain‐based evaluation described in Chapter 8 of theCochrane Handbook for Systematic Reviews of Interventions 5.1.0 (Higgins 2011). The evaluations were compared and any inconsistencies between the review authors were discussed and resolved.
The following domains were assessed as low risk of bias, unclear (i.e. uncertain risk of bias) or high risk of bias:
-
sequence generation;
-
allocation concealment;
-
blinding (of participants, personnel and outcome assessors);
-
incomplete outcome data;
-
selective outcome reporting;
-
free of other bias.
Risk of bias in any included studies was categorised according to the following:
-
low risk of bias (plausible bias unlikely to seriously alter the results) if all criteria were met;
-
unclear risk of bias (plausible bias that raises some doubt about the results) if one or more criteria were assessed as unclear; or
-
high risk of bias (plausible bias that seriously weakens confidence in the results) if one or more criteria were not met.
These assessments are reported in the Risk of bias in included studies table.
Measures of treatment effect
We had planned to transform longevity/survival data to dichotomous outcomes (failure/not). Risk ratios and their 95% confidence intervals would be calculated for all dichotomous data. The mean difference and 95% confidence intervals would be calculated for continuous data.
Unit of analysis issues
These may arise in within‐patient studies. In future updates, if studies present paired data for this intervention and comparison these will be entered into tables and summarised.
Dealing with missing data
Attempts were made to contact trialists to obtain missing data but these were unavailable to us.
In future updates if data are missing from trials, reasonable attempts will be made to contact the investigators or sponsors of these studies. We will re‐analyse data according to the intention‐to‐treat (ITT) principle whenever possible. For dichotomous outcomes, if authors had conducted a per‐protocol analysis we will carry out an ITT analysis with imputation setting the missing data to their baseline values, after checking the degree of imbalance in the drop‐outs between the arms to determine the potential impact of bias (section 16.2.2 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011)). For continuous outcomes a per‐protocol analysis will be carried out in place of an ITT analysis.
Assessment of heterogeneity
A lack of included studies precluded any assessment of heterogeneity but if further trials are identified the following methods will be used.
We will assess clinical heterogeneity by examining the characteristics of the studies, the similarity between the types of participants, the interventions and the outcomes as specified in the criteria for included studies. Statistical heterogeneity will be assessed using a Chi2 test and the I2 statistic where I2 values over 50% indicate moderate to high heterogeneity. We will consider heterogeneity to be significant when the P value is less than 0.10 (Higgins 2003).
Assessment of reporting biases
If further trials are identified for inclusion in this review, publication bias will be assessed according to the recommendations on testing for funnel plot asymmetry (Egger 1997) as described in section 10.4.3.1 of the Cochrane Handbook for Systematic Reviews of Interventions 5.1.0 (Higgins 2011), and if asymmetry is identified, we will try to assess other possible causes and these will be explored in the discussion if appropriate.
Data synthesis
As only one study was included in this review, data synthesis was not feasible but if further studies are identified for inclusion in this review, the following methods will be used.
Two review authors (ZF and MN) will analyse the data and report them as specified in Chapter 9 of the Cochrane Handbook for Systematic Reviews of Interventions 5.1.0 (Higgins 2011). Analysis will be conducted at the same level as the allocation.
Subgroup analysis and investigation of heterogeneity
Subgroup analyses will be conducted for any of the following: different bonding agents, the type of cavity (Class I or II) and its location (premolar or molar tooth), only if there are sufficient numbers of included trials with appropriate data.
Sensitivity analysis
If sufficient studies are included in future updates we plan to conduct sensitivity analyses to assess the robustness of our review results by repeating the analysis with the following adjustments: exclusion of studies with unclear or inadequate allocation concealment, unclear or inadequate blinding of outcomes assessment and completeness of follow‐up.
Presentation of main results
We established a summary of findings Table for the main comparison using the following outcomes listed according to priority.
-
Survival of the restoration.
-
Post‐insertion sensitivity or pain assessed by a validated pain scale.
-
Secondary caries, as diagnosed clinically.
-
Marginal deterioration of the restoration and fracture of the remaining tooth tissue.
-
Economic data: direct costs of materials and any reported associated indirect costs.
-
Adverse effects: any event for which the causal relationship between the event and the amalgam restoration is at least a reasonable possibility.
Results
Description of studies
Results of the search
De‐duplication of the initial search results carried out in July 2009 produced 437 references to potentially eligible studies. After examination of the titles and abstracts of these references, all but seven (Browning 2000; Mach 2002; McEvoy 1992; McEvoy 1993; Mahler 1996; Setcos 1999; Xia 2002) were eliminated and excluded from further review. Full text copies of these remaining studies were obtained and then subjected to further evaluation which included an examination of their bibliographical references which provided no additional citations to potentially eligible trials.
We arranged to translate (Xia 2002) from the Chinese to the English language. From the translated version of this study we noted that neither the inclusion criteria nor the interventions used were explicitly described and that the outcome data were incompletely reported. Poor methodological rigour and the possibility of high risk of bias coupled with our lack of success in contacting the investigators resulted in its exclusion.
The review authors discussed the eligibility of the potentially eligible studies, resolved any uncertainties by consensus and finally excluded all the studies, seeCharacteristics of excluded studies, with the exception of Setcos 1999 which met our inclusion criteria and was included in this review.
Updated searches
We updated the electronic searches in January 2016 and found 206 new records, but no new trials were identified for inclusion (Figure 1).
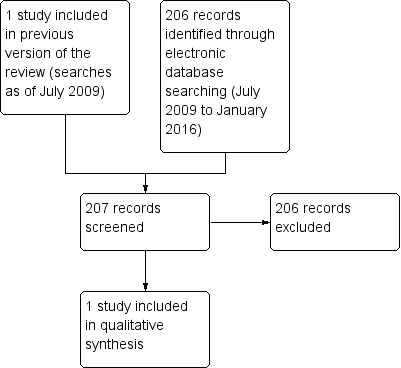
Study flow diagram.
Included studies
Characteristics of the trial setting and investigators
Setcos 1999 was a single centre prospective randomised controlled trial which was conducted in the UK but the report provided no further details about the setting. The providers and assessors of treatment were university research staff.
Although the investigators indicated that the study was supported by Kuraray Co Ltd, Osaka, Japan they did not specify the level of support nor did they declare any potential conflicts of interest.
Characteristics of the participants
Very limited demographic details were presented in the report other than that the participants were "drawn from a healthy population with no contraindications to routine dental treatment", and required Class II (two or three surface) restorations in vital posterior teeth. The investigators stated that they sought to utilise contralateral pairs of teeth such that in‐mouth comparisons could be made and thus the study attempted to match contralateral pais of teeth in the same patient (split‐mouth) in addition to single restorations. Participants received appropriate oral hygiene instruction and support prior to treatment and were "seen more regularly for dental examinations and tooth cleaning" during the course of the study.
Characteristics of the interventions
The majority of these were replacements for defective restorations in which some of the preparations had pre‐existing retention and undercuts. Cavity preparation consisted of conservative excavation of caries with minimal removal of sound tooth tissue and the investigators indicated that no attempt was made to provide additional deliberate retention through either grooves or undercuts. In a subsequent communication with one of the trialists it was confirmed that, to reduce interoperator variability, all the restorations were placed by the same dentist.
In the adhesive group (60 teeth), ED primer was applied to the preparation with a sponge pellet for 60 seconds and dried with an air syringe. Panavia 21TC was applied with a brush and left for 60 seconds, the cavity was filled incrementally with amalgam and then carved and burnished. The margins were covered with Oxyguard II gel to allow setting of the adhesive cement. The materials were handled according to manufacturers instructions, and standard clinical procedures were used for finishing and polishing of the set amalgam.
The restorative procedures used in the non‐adhesive group (53 teeth) were identical but excluded the use of adhesive, varnish or any similar material.
Characteristics of outcome measures
Outcome assessments were made by two dentists, who were experienced in rating restorations, within the first month post‐intervention (baseline) and at a two‐year follow‐up. The assessments were made independently by both evaluators at each recall visit and any discrepancies in the ratings were discussed and agreed by consensus. The number of failed restorations was recorded, where failure referred to a restoration which had been dislodged and lost. Participants were also questioned at these time points about thermally sensitivity, which was rated according to the modified USPHS criteria: A (Alpha): tooth not temperature sensitive, or momentary slight sensitivity; B (Bravo): tooth moderately temperature sensitive, but does not linger; C (Charlie): tooth severely temperature sensitive.
Further details of this trial can be found in the Characteristics of included studies table.
Excluded studies
Six studies were excluded: two were surveys (McEvoy 1992; McEvoy 1993); Mahler 1996 was a non‐randomised study and Xia 2002 lacked methodological rigour. The decision to exclude Browning 2000 was based on our categorisation of this study at high risk of (selection) bias for the outcomes of interest in addition to the incompleteness of its data as a result of the large number of withdrawals. We eliminated the Mach 2002 study from this review because it included teeth with lesions other than Class II, as well as the lack of clarity and consistency in the reporting of the interventions participants received as well as in the presentation of the outcome data. SeeCharacteristics of excluded studies table.
Risk of bias in included studies
We were successful in contacting another one of the study investigators by email who was able to clarify some missing trial details which enabled a change in both the assessment of concealed randomisation and blinded assessment of outcomes from unclear risk to low risk to be made for this study.
As not all of the criteria used in the assessment of risk of bias were met, this trial was assessed as at unclear risk of bias (plausible bias that raises some doubt about the results). Further details of these assessments are available in the Risk of bias in included studies table.
Effects of interventions
See: Summary of findings for the main comparison Adhesive bonding for restorations of dental amalgam
The single included trial provided a limited amount of data relevant to some of the primary and secondary outcomes of this review and therefore we have not entered these into the RevMan analysis but present these data in the Additional tables section of this review together with a descriptive summary. In addition, we note that although the data analysis in this trial failed to take into account the clustering of matched pairs of teeth it was considered that this would have a limited impact on the overall results.
Primary outcomes
(1) Survival of the restoration: longevity/survival to defined time points yearly up to a maximum of 10 years
Only three restorations (non‐bonded) were reported as lost at 4, 7 and 24 months, and in all three the loss of proximal boxes was attributed to a lack of retention (Additional Table 1). It was unclear how many, if any, of the five bonded restorations which were unavailable at the 24‐month recall could be classified as failures.
Due to the unclear number of participants and effect of clustering, these data were not further analysed.
| Adhesively bonded | Non‐bonded | ||
| Success | Failure | Success | Failure |
| 55/60 | 5 restorations unavailable at 24‐month follow‐up | 50/53 | 3 (5.7%) |
Fisher's Exact test P = 0.115
Secondary outcomes
(1) Post‐insertion sensitivity or pain assessed by a validated pain scale
Only the modified USPHS criteria were used to rate post‐insertion temperature sensitivity at both baseline and at the 24‐month assessment. Although the investigators indicated that there was no significant difference in sensitivity between the two groups (P > 0.05), this conclusion appeared to be based on the assessments made solely at these two time points. However, because such ordinal ratings of severity are unlikely to be sufficiently sensitive in providing a discriminative assessment of post‐operative sensitivity when compared with a validated visual analogue scale (VAS), we have not reported these data.
(2) Secondary caries, as diagnosed clinically
The report provided no data for this outcome.
(3) Marginal deterioration of the restoration and fracture of the remaining tooth tissue
No fractures of remaining tooth tissue were reported in either of the intervention groups. The marginal deterioration of restorations was assessed at the occlusal and proximal surfaces, and the investigators reported that there was no significant difference between the groups or the matched pairs of restorations in their marginal adaptation (P > 0.05), and that these provided comparable Alpha rating scores at both baseline and 24 months (Additional Table 2).
| Occlusal | Proximal | |||
| Adhesively bonded | Non‐bonded | Adhesively bonded | Non‐bonded | |
| Baseline | 97 | 94 | 88 | 87 |
| 24 months | 96 | 88 | 91 | 82 |
All data are expressed as Alpha percentages, remaining ratings were Bravo.
Although not discussed by the investigators, the apparent improvement in Alpha scores (88% to 91%) in the proximal assessment in the bonded group at 24 months may reflect the subsequent replacement of the three failed non‐bonded restorations with adhesively bonded restorations and is consistent with their survival at the 24‐month recall.
(4) Economic data: direct costs of materials and any reported associated indirect costs
No data were reported.
(5) Adverse effects
The investigators did not report any adverse effects.
For further details of this trial see the Characteristics of included studies table.
Discussion
Summary of main results
The single randomised controlled trial, albeit only of short duration, which was included in this review would appear to confirm some of the findings of several other studies in that moderately sized adhesively bonded amalgam restorations have a similar survival profile and clinical performance to non‐bonded restorations. However, whilst attempts were made in this study to ensure that the preparations for bonded restorations had limited retentive form compared to conventional preparations utilising deliberate retention, such that assessment could be made of the added value of bonding, there can be no certainty that this is reflected by the similarity of survival data in both treatment groups chiefly because of the difficulties of eliminating all potential sources of retention. Although these similarities may suggest that there is reliable evidence for the effectiveness of bonding agents, they also indicate that adhesive bonding of dental amalgam restorations has neither beneficial nor detrimental effects on clinical performance, as assessed by modified USPHS over periods of up to two years after placement, and therefore calls into question the additional cost of materials and time expended on bonding. The results are summarised in the summary of findings Table for the main comparison.
Overall completeness and applicability of evidence
There was only one included study and it provides insufficient evidence that adhesively bonded amalgam restorations perform any better than non‐adhesively bonded amalgam restoration when followed up for two years. The results of this single study provided very limited evidence which can be applied to the clinical setting and there appears to be no continuing research covering this clinical topic.
Quality of the evidence
The paucity of high quality trials evaluating the effects of adhesive bonding on the in‐service performance and longevity of restorations of dental amalgam proved to be somewhat disappointing more especially because of the availability and usage, by clinicians, of a wide range of bonding agents that have been developed over a number of years.
Limitations in study design
Whilst recognising some of the complexities of assessing post‐operative sensitivity for these interventions, the apparent lack of temperature sensitivity in the two groups may be potentially misleading. The absence of temperature sensitivity at the 24‐month recall could in any event be indicative of post‐operative loss of vitality and in particular if there was immediate post‐insertion hypersensitivity. This lack of detailed information about any immediate post‐insertion sensitivity or pain and in particular its duration and intensity due to any stimulus as assessed with a VAS was a further, small but not insignificant, limitation of this study.
Indirectness of the evidence
Even though the clinical trial that was included in this systematic review satisfied our inclusion criteria, the generalisability of its results are likely to be compromised by several factors: the selection of patients from a university dental hospital environment, which could be considered unrepresentative of the population at large, as well as the comparative freedom from some of the constraints, e.g. time and cost of materials, which might apply in general dental practice.
Imprecision of the results
Imprecision in the results was reflected by the small sample size in the single included study.
Inconsistency of the results
The single included study did not allow any assessment of inconsistency of results.
Potential biases in the review process
Every attempt was made to limit bias in the review process by ensuring a comprehensive search for potentially eligible studies. The authors' independent assessments of eligibility of studies for inclusion in this review minimised the potential for selection bias. The effects of language bias on the identification and selection of studies for inclusion in a systematic review is widely recognised; therefore, we ensured that language of publication was not used as an exclusion criterion.
Agreements and disagreements with other studies or reviews
Our searches did not identify any other potential systematic reviews to compare with.

Study flow diagram.
| Adhesive bonding for restorations of dental amalgam | ||||||
| Patient or population: Patients with restorations of dental amalgam | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | Number of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Adhesive bonding | |||||
| Survival of the restoration | See comment | See comment | Not estimable | 31 | ⊕⊕⊝⊝ | Of the adhesively bonded 55/60 were a success, 5 were unavailable at 24‐month follow‐up Of the non‐bonded 50/53 were a success, and the remaining 3 a failure |
| Post‐insertion sensitivity or pain assessed by a validated pain scale ‐ not measured | See comment | See comment | Not estimable | ‐ | See comment | No study addressed this outcome |
| Secondary caries, as diagnosed clinically ‐ not measured | See comment | See comment | Not estimable | ‐ | See comment | No study addressed this outcome |
| Marginal deterioration of the restoration and fracture of the remaining tooth tissue | Study population | Not estimable | 31 | ⊕⊕⊝⊝ | Marginal adaptation USPHS Alpha ratings: Occlusal; adhesively bonded from 97 at baseline to 96, non‐bonded from 94 at baseline to 88 Proximal; adhesively bonded from 88 at baseline to 91, non‐bonded from 87 at baseline to 82 | |
| See comment | See comment | |||||
| Economic data: direct costs of materials and any reported associated indirect costs ‐ not measured | See comment | See comment | Not estimable | ‐ | See comment | No study addressed this outcome |
| Adverse effects: any event for which the causal relationship between the event and the amalgam restoration is at least a reasonable possibility ‐ not measured | See comment | See comment | Not estimable | ‐ | See comment | No study addressed this outcome |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Attrition bias | ||||||
| Adhesively bonded | Non‐bonded | ||
| Success | Failure | Success | Failure |
| 55/60 | 5 restorations unavailable at 24‐month follow‐up | 50/53 | 3 (5.7%) |
| Fisher's Exact test P = 0.115 | |||
| Occlusal | Proximal | |||
| Adhesively bonded | Non‐bonded | Adhesively bonded | Non‐bonded | |
| Baseline | 97 | 94 | 88 | 87 |
| 24 months | 96 | 88 | 91 | 82 |
| All data are expressed as Alpha percentages, remaining ratings were Bravo. | ||||

