Interventions chirurgicales pour la prise en charge précoce de la paralysie de Bell
Referencias
References to studies included in this review
References to studies excluded from this review
References to studies awaiting assessment
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Study characteristics | ||
| Methods | Quasi‐randomised controlled study Follow‐up 12 months, with additional assessments at 3‐ and 6‐month intervals Location: study conducted through the Peking Union Medical College Hospital, China Dates: treated at hospital between 2003 and 2013 | |
| Participants | 53 participants initially selected for 3 groups Inclusion criteria: adults aged > 16 years, total paralysis at onset, previous treatment with oral prednisolone 1 mg/kg within first 72 hours, duration > 2 months, worst score of facial paralysis was lower than HB V after 2 months, > 95% degeneration with reduced voluntary EMG activity after 2 months, no systemic disease Once allocated, 1 participant declined surgery and 11 participants declined the 'wait and see' control; therefore, all 12 were removed from the study, resulting in 41 participants for evaluation. Early surgery group (within 2–3 months from onset): n = 18; aged 21–53 years; male:female ratio 10:8 Late surgery group (> 3 months from onset): n = 8; aged 27–58 years; male:female ratio 4:4 Control/no treatment group: n = 15; aged 25–62; male:female ratio 8:7 No statistically significant baseline differences in the age and sex distributions between the 3 groups (P > 0.05) | |
| Interventions | Participants quasi‐randomised into surgical and non‐surgical groups via alternation Early surgery group: surgery performed within 2–3 months of denervation with decompression using a retro‐auricular transmastoid approach Late surgery group: surgery performed > 3 months after denervation with decompression using a retro‐auricular transmastoid approach Control group: no surgery All participants had received oral prednisolone 1 mg/kg within 72 hours of denervation onset to be included in the study. Any participants who declined their allocated interventions were removed from the study. | |
| Outcomes | HBGS used to measure physician‐based outcomes FaCE scales used to measure patient‐based outcomes Synkinesis and other clinical features assessed via the FaCE scale using patient‐reported data Outcomes measured at 3, 6 and 12 months Statistical methods included Fisher exact test for differences between proportions. Non‐parametric tests used due to non‐normal distribution of scores. All tests conducted at 5% level of significance. All analyses performed using SPSS 20. | |
| Funding | Supported by Key Projects in the National Science & Technology Pillar Program of China during the Twelfth Five‐Year Plan Period, the Natural Science Foundation of Shaanxi Province, and Xi'an Jioatong University basic scientific research operation expenses. | |
| Conflicts of interest | No declared conflicts of interest among the main researchers in study. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote: "all patients were allocated to the surgical treatment group or the follow‐up group by a quasi‐random method at the clinic (alternation) … total random distribution could not be performed because some patients refused surgical intervention." Comment: not true randomisation. Participants who declined their allocated interventions were removed from the study. There is also no mention as to how the order of alternation was determined, and we judged the risk of bias high. |
| Allocation concealment (selection bias) | Unclear risk | No comment on method of allocation concealment. This in combination with a high risk of bias from random sequence generation is likely to have caused baseline imbalances between treatment arms in the study. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not specified whether blinding of participants to either a surgical or non‐surgical intervention was possible. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Blinding of the investigator/outcome assessor was not reported and would have been difficult to perform in this study because of the surgical intervention involved. |
| Incomplete outcome data (attrition bias) | High risk | Quote: "one patient in the surgical group who declined surgery was removed from the study, and 11 patients in the follow‐up group who refused the wait‐and‐see approach and went to other hospitals for treatment were also removed from the study … One patient in the early surgery group and two patients in the no treatment group were lost to follow‐up … 11 patients in the early surgery group and 10 patients in the no treatment group completed the FaCE questionnaires at presentation and at the end of follow‐up." Comment: 12 participants were lost to allocation and commented on. However, 1/18 participants in the early surgical group and 2/13 participants in the no treatment group were lost to follow‐up after the 6‐month assessment with no reasons given. Only 21/41 participants completed the FaCE questionnaire with no reasons given. |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes were reported on; therefore, our judgement was low risk. |
| Other bias | Low risk | No other sources of bias identified. |
| Study characteristics | ||
| Methods | Randomised controlled trial After meeting inclusion criteria, participants were first allocated to a group with presumed 'bad prognosis' or to a group with presumed 'good prognosis.' For the 'bad prognosis' group, rate of recovery was followed for 1–3 years. Location: 2 centres participated simultaneously: University Hospital, Leiden and Municipal Hospital, The Hague, Netherlands Dates: 1965–1969 | |
| Participants | 25 participants were selected based on a 'bad prognosis', defined as complete facial palsy and EMG showing no voluntary control of motor unit or a minimal applied current evoking a motor response on the affected side 2.5 times that of the unaffected side. These responses needed to be confirmed on 2 occasions a few days apart. 1 participant refused surgery and was excluded from the study, resulting in 24 evaluable participants total. Surgery group: n = 11; mean age 45.3 years; male:female ratio 1:10; side of idiopathic facial palsy left:right = 7:4 Control group: n = 13; mean age 45 years; male:female ratio 8:5; side of idiopathic facial palsy left:right = 6:7 Study did not report if there were statistically significant differences between groups. | |
| Interventions | Surgery group: decompressed using a retro‐auricular approach 7–20 days after the onset of paralysis Control group: no treatment | |
| Outcomes | Recovery of facial nerve function at 12 months assessed using 0–5 scale (0 no function, 5 complete function). Study report did not state statistical methods used | |
| Funding | No sponsorship noted | |
| Conflicts of interest | No declared conflicts of interest among the main researchers in the study | |
| Notes | Study also included a population of 242 non‐randomised participants with 'presumed good prognosis' who did not meet the criteria for having a 'bad prognosis.' Quote: "They received no therapy... and were also followed clinically and electromyographically along with the patients of the controlled trial in order to validate our criteria." | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "in both hospitals these patients were entered on a list, previously prepared by the statistical department, University of Leiden (head, Mr H. De Jonge), which randomly allocated them to surgical treatment or to a control group." Comment: 25 participants were randomly allocated into surgical or control groups. 1 participant declined surgery and was removed from the study. |
| Allocation concealment (selection bias) | Unclear risk | No comment on any attempted allocation concealment. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not specified whether blinding of the participant to either a surgical or non‐surgical intervention was possible. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Report does not comment on blinding of the investigator/outcome assessor, which would have been difficult to perform in this study because of the surgical intervention involved. |
| Incomplete outcome data (attrition bias) | Low risk | Quote: "All patients were followed clinically and electromyographically for a least a year." Comment: complete follow‐up with no losses. |
| Selective reporting (reporting bias) | High risk | All prespecified outcomes were reported on indirectly via results "after the second week," inferring that results at each of our prespecified time points would be the same. |
| Other bias | Low risk | No other sources of bias identified. |
EMG: electromyography; FaCE: Facial Clinimetric Evaluation scale; HB: House‐Brackmann; HBGS: House‐Brackmann grading system; n: number of participants.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Participants who refused surgery were included and added to the control group. Therefore, allocation was not randomised. | |
| Included participants were not randomised into surgical or non‐surgical groups. | |
| Retrospective study. No control group included for comparison of outcomes. | |
| Retrospective audit. Study did not compare outcomes between groups or describe how surgery and no‐surgery groups were selected. | |
| Retrospective study. No description given as to how participants were allocated to the surgically treated or not surgically treated groups. No discussion of the non‐surgical group. Only 14 participants underwent surgery. | |
| No randomisation. Participants chose whether to have surgery. 11/30 participants offered surgery declined; therefore, only 19/169 evaluated had surgery. | |
| No randomisation. Participants chose whether to have surgery. Also, report did not describe the degree of baseline clinical palsy, merely that the nerve was degenerating. | |
| Upon initial abstract screening, the abstract suggested potential randomisation. However, on full‐text retrieval and translation, the study was non‐randomised. | |
| Literature review. Study did not include comparison groups. Primarily focused on efficacy of steroid and antiviral use as opposed to surgical interventions. | |
| Retrospective study. No randomisation. Participants chose whether to have surgery. 22/34 participants offered surgery declined, therefore, only 12 had surgery. | |
| Included participants were not randomised into surgical or non‐surgical groups. | |
| Included participants were diagnosed with hemi‐facial spasm. | |
| No control group included for comparison of outcomes. | |
| Prospective audit. No attempt at randomisation. Control group was self‐selected, considered poor surgical risk or had already received corticosteroids. 50 participants underwent surgery with a control group of 35. However, statistical comparison was performed on only the poorest prognostic groups of 25 surgical and 13 non‐surgical participants, which showed no statistically significant difference. | |
| Retrospective audit. Participants chose whether to have surgery. Control group either declined surgery or were considered poor surgical risk. | |
| Participants had trial of corticosteroids initially before being considered for surgery. No randomisation. Participants chose whether to have surgery. Report noted that younger participants opted for surgery and older participants refused surgery. | |
| Participants included those with 'hemifacial spasm' and outcomes were not reported separately by aetiology. In addition, timeframe from onset to procedure varied widely up to 180 days post onset, and was not reported separately for specific time periods. | |
| Retrospective study. No randomisation. Participants chose whether to have surgery. |
Characteristics of studies awaiting classification [ordered by study ID]
| Methods | Parallel, randomised, "placebo‐controlled" (sic) (assessor blinded) |
| Participants | Inclusion criteria: adults with severe Bell's palsy and Ramsay Hunt syndrome; aged > 15 years; with complete facial palsy (Yanagihara score ≤ 10); degree of denervation > 90% with ENOG and clinical follow‐up unavailable for more than 12 months Exclusion criteria: pregnancy; current neoplasms; chronic kidney disease; chronic liver disease; immune suppression; opt out decompression surgery |
| Interventions | Intervention group: facial nerve regenerating surgery with human recombinant bFGF Control group: transmastoid conventional facial nerve decompression surgery |
| Outcomes | Primary: non‐recovery rate 12 months after disease onset Secondary: non‐recovery rate 6 months after disease onset, incidence rate of sequelae 12 months after disease onset. Postoperative bleeding needing haemostasis in operating room and audiometric threshold elevation using air conduction pure tone audiometry at 250 Hz, 500 Hz, 1 kHz, 2 kHz and 4 kHz test frequencies |
| Funding | Quote: "Self‐funding." |
| Notes | Author contacted 22 June 2020 regarding likely publication date, clarification of intervention, outcomes and population, and whether study is ongoing or if statistical analysis is completed. |
bFGF: basic fibroblast growth factor; ENOG: electroneurography.
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1.1 Complete recovery at 12 months Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.1  Comparison 1: Early surgery versus no treatment, Outcome 1: Complete recovery at 12 months | ||||
| 1.2 Complete recovery at 3 months Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.2  Comparison 1: Early surgery versus no treatment, Outcome 2: Complete recovery at 3 months | ||||
| 1.3 Complete recovery at 6 months Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.3  Comparison 1: Early surgery versus no treatment, Outcome 3: Complete recovery at 6 months | ||||
| 1.4 Synkinesis Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 1.4  Comparison 1: Early surgery versus no treatment, Outcome 4: Synkinesis | ||||
| 1.5 Contractures Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 1.5  Comparison 1: Early surgery versus no treatment, Outcome 5: Contractures | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 2.1 Complete recovery at 12 months Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 2.1  Comparison 2: Early surgery versus late surgery, Outcome 1: Complete recovery at 12 months | ||||
| 2.2 Complete recovery at 3 months Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 2.2  Comparison 2: Early surgery versus late surgery, Outcome 2: Complete recovery at 3 months | ||||
| 2.3 Complete recovery at 6 months Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 2.3  Comparison 2: Early surgery versus late surgery, Outcome 3: Complete recovery at 6 months | ||||
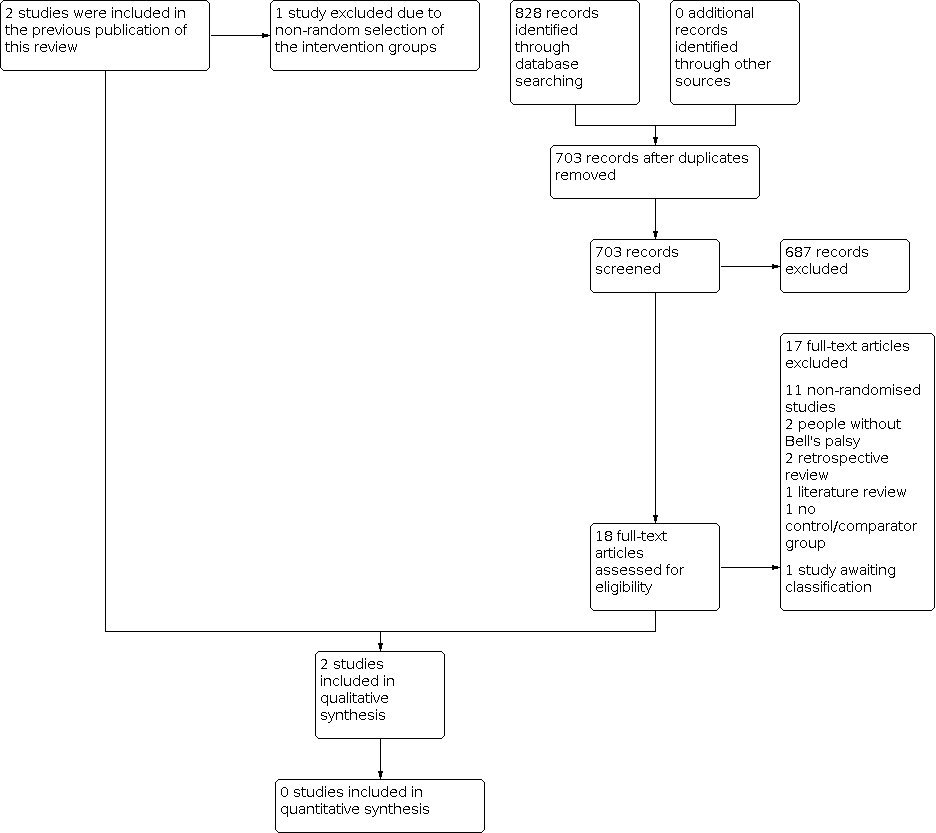
Study flow diagram.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study. Red = high risk of bias, yellow = unclear risk of bias and green = low risk of bias.

Comparison 1: Early surgery versus no treatment, Outcome 1: Complete recovery at 12 months

Comparison 1: Early surgery versus no treatment, Outcome 2: Complete recovery at 3 months

Comparison 1: Early surgery versus no treatment, Outcome 3: Complete recovery at 6 months

Comparison 1: Early surgery versus no treatment, Outcome 4: Synkinesis

Comparison 1: Early surgery versus no treatment, Outcome 5: Contractures

Comparison 2: Early surgery versus late surgery, Outcome 1: Complete recovery at 12 months

Comparison 2: Early surgery versus late surgery, Outcome 2: Complete recovery at 3 months

Comparison 2: Early surgery versus late surgery, Outcome 3: Complete recovery at 6 months
| Surgery compared with medical treatment for Bell's palsy | ||||||
| Patient or population: Bell's palsy Settings: hospital attendance with idiopathic facial paralysis Intervention: early surgery (within 3 months from denervation onset) Comparison: no surgical treatment | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | Number of participants | Certainty of the evidence | Comments | |
|---|---|---|---|---|---|---|
| Assumed risk | Corresponding risk | |||||
| No treatment | Early surgery | |||||
| Complete recovery of facial nerve function at 12 months Defined as: complete recovery HB grade I. Follow‐up: 12 months 1st study: scale 0–5 (0 = no function, 5 = complete function for 3 facial muscles) 2nd study: HBGS (complete = HB I, fair = HB II–III and poor recovery = HB IV–VI) | The 1st study (24 evaluable participants) compared surgery between the 2nd and 3rd week post onset to a no‐treatment control group. The 2nd study (33 evaluable participants) compared early surgery (within 2–3 months post paralysis onset) to no further treatment. Neither study reported a statistically significant difference in recovery of facial nerve function between the surgical and non‐surgical groups at 12 months (P > 0.05). We calculated the RR for complete recovery at 12 months for the 2nd study; 1/18 participants in the early surgery group achieved complete recovery at 12 months compared to 1/15 in the no‐treatment group (RR 0.76, 95% CI 0.05 to 11.11; P = 0.84). | 57 | ⊕⊝⊝⊝ | We are uncertain whether surgery affects recovery of facial nerve function at 1 year as the certainty of evidence was very low. 1 study did not perform statistical analysis, 1 did not state the method used. 1 study did not directly report 12‐month results. Different outcome measures in each study made combining results impractical. | ||
| Side effects and complications of treatment | The 1st study (24 evaluable participants) reported no complications of surgery. The 2nd study (41 evaluable participants) reported postoperative complications such as sensorineural hearing loss, tinnitus, vertigo and dizziness. There were no reported surgical complications such as wound dehiscence, infection, bleeding and numbness. 4 participants had sensorineural hearing loss at high frequencies, with bone conduction thresholds ranging from 35 dB to 50 dB at 4000 Hz. 3 participants reported tinnitus. There were no reported cases of postoperative vertigo or major labyrinthitis. | 57 | ⊕⊝⊝⊝ | The numbers involved in the included studies were small. Statistical analysis was not possible. | ||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; HB: House‐Brackmann; HBGS: House‐Brackmann grading system; RCT: randomised controlled trial; RR: risk ratio. | ||||||
| GRADE Working Group grades of evidence | ||||||
| aDowngraded twice because of very serious limitations in study design: 1 study did not report the method of randomisation. Both studies had unclear allocation concealment. Blinding of participants was not possible and neither study blinded outcome assessors. 1 study did not follow up large numbers of participants. We further downgraded the evidence for imprecision as there were small numbers of participants in both studies. 1 study also reported the primary and secondary facial nerve recovery outcomes of this review indirectly, which warranted further downgrading for indirectness. | ||||||
| Early surgery compared with late surgery for Bell's palsy | ||||||
| Patient or population: people with Bell's palsy Settings: hospital attendance with idiopathic facial paralysis Intervention: early surgery (within 3 months from denervation onset) Comparison: late surgery (later than 3 months from denervation onset) | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Certainty of the evidence | Comments | |
|---|---|---|---|---|---|---|
| Assumed risk | Corresponding risk | |||||
| Late surgery | Early surgery | |||||
| Complete recovery of facial nerve function at 12 months Defined as: complete recovery HB grade I. Follow‐up: 12 months 1st study: scale 0–5 (0 = no function, 5 = complete function for 3 facial muscles) 2nd study: HBGS (complete = HB I, fair = HB II–III, and poor recovery = HB IV–VI) | Within the 1 study (33 evaluable participants), 18 undergoing surgery within 2–3 months of denervation (early surgery) were compared with 8 participants undergoing surgery > 3 months from denervation onset (late surgery). There was no statistically significant difference in recovery of facial nerve function between the early surgical and late surgical groups at 12 months (P > 0.05). We calculated the RR for complete recovery at 12 months; 1/18 participants in the early surgery group achieved complete recovery at 12 months compared to 1/8 in the late surgery group. | RR 0.47 (0.03 to 6.60) | 26 (1 RCT) | ⊕⊝⊝⊝ | The evidence for recovery of facial nerve function with early vs late surgery was uncertain. | |
| Side effects and complications of treatment | The 1 study (41 evaluable participants) reported postoperative complications such as sensorineural hearing loss, tinnitus, vertigo and dizziness. There were no reported surgical complications such as wound dehiscence, infection, bleeding and numbness. 4 participants had sensorineural hearing loss at high frequencies, with bone conduction thresholds ranging from 35 dB to 50 dB at 4000 Hz. 3 participants reported tinnitus. There were no reported cases of postoperative vertigo or major labyrinthitis. | Not reported | 26 (1 RCT) | Unable to rate certainty of evidence | The trial that compared early and late surgery did not report adverse events separately by timing of surgery. | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; HB: House‐Brackmann; HBGS: House‐Brackmann grading system; RCT: randomised controlled trial; RR: risk ratio | ||||||
| GRADE Working Group grades of evidence | ||||||
| aDowngraded three times: twice because of very serious limitations in study design (high risk of bias in most domains) and once for imprecision from small‐study size (26 participants). | ||||||
| Risk of bias | Interpretation | Within study | Across studies |
|---|---|---|---|
| Low risk of bias | Plausible bias unlikely to seriously alter the results. | Low risk of bias for all key domains. | Most information is from studies at low risk of bias. |
| Unclear risk of bias | Plausible bias that raises some doubt about the results. | Unclear risk of bias for ≥ 1 key domains. | Most information is from studies at low or unclear risk of bias. |
| High risk of bias | Plausible bias that seriously weakens the confidence in the results. | High risk of bias for ≥ 1 key domains. | The proportion of information from studies at high risk of bias is sufficient to affect the interpretation of results. |
| Approach for summary assessments of the risk of bias for each important outcome (across domains) within and across studies (Higgins 2011). | |||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1.1 Complete recovery at 12 months Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.2 Complete recovery at 3 months Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.3 Complete recovery at 6 months Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.4 Synkinesis Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 1.5 Contractures Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 2.1 Complete recovery at 12 months Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.2 Complete recovery at 3 months Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.3 Complete recovery at 6 months Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |

