Tratamiento activo versus tratamiento expectante en el periodo de alumbramiento del trabajo de parto
Resumen
Antecedentes
El tratamiento activo del periodo expulsivo del trabajo de parto incluye la administración de un uterotónico como profilaxis, pinzamiento inmediato del cordón y su tracción controlada para extraer la placenta. Con el tratamiento expectante se aguardan los signos de separación placentaria y la placenta se expulsa espontáneamente. El tratamiento activo se introdujo para tratar de reducir la hemorragia, un contribuyente principal a la mortalidad materna en los países de bajos ingresos. Ésta es una actualización de una revisión publicada por última vez en 2015.
Objetivos
Comparar los efectos del tratamiento activo versus el tratamiento expectante en el periodo expulsivo del trabajo de parto sobre la hemorragia posparto primaria grave, la pérdida sanguínea y otros resultados maternos e infantiles.
Comparar los efectos de las variaciones de los paquetes de tratamiento activo y expectante en el periodo de alumbramiento del trabajo de parto sobre la HPP primaria grave y otros resultados maternos e infantiles.
Métodos de búsqueda
Para esta actualización, se realizaron búsquedas en el Registro de Ensayos del Grupo Cochrane de Embarazo y Parto (Cochrane Pregnancy and Childbirth's Trials Register), ClinicalTrials.gov y en la World health Organization International Clinical Trials Registry Platform (ICTRP), el 22 de enero 2018, así como en las listas de referencias de los estudios recuperados.
Criterios de selección
Ensayos controlados aleatorizados y cuasialeatorizados que compararon el tratamiento activo versus el tratamiento expectante en el periodo expulsivo del trabajo de parto. Se consideraron elegibles para inclusión los ensayos aleatorizados grupales, pero no se identificaron.
Obtención y análisis de los datos
Dos autores de la revisión de forma independiente evaluaron los estudios para su inclusión, evaluaron el riesgo de sesgo, realizaron la extracción de datos y evaluaron la calidad de la evidencia mediante los criterios GRADE.
Resultados principales
Se incluyeron ocho estudios con 8892 mujeres en el análisis de los datos. Todos los estudios se realizaron en hospitales, siete en países de altos ingresos y uno en un país de bajos ingresos. Cuatro compararon el tratamiento activo versus el expectante y uno comparó el tratamiento activo versus una combinación de tratamientos. Para el análisis se utilizó un modelo de efectos aleatorios debido a la heterogeneidad clínica. De los ocho estudios incluidos, se consideró que tres tuvieron bajo riesgo de sesgo en los principales aspectos de la generación de la secuencia, la ocultación de la asignación y la exhaustividad de la recopilación de datos. Hubo falta de evidencia de calidad alta según las evaluaciones GRADE para los resultados primarios, lo que se refleja en el cauteloso lenguaje que se presenta a continuación.
La evidencia indicó que, para las mujeres con niveles mixtos de riesgo de hemorragia, no es seguro que el tratamiento activo reduzca el riesgo promedio de HPP primaria grave materna (más de 1000 ml) en el momento del parto (riesgo relativo [RR] promedio 0,34, intervalo de confianza [IC] del 95%: 0,14 a 0,87; tres estudios, 4636 mujeres; I2 = 60%; GRADE: calidad muy baja). Para la incidencia de hemoglobina (Hb) materna inferior a 9 g/dl después del parto, el tratamiento activo del periodo de alumbramiento puede reducir el número de mujeres con anemia después del parto (RR promedio 0,50; IC del 95%: 0,30 a 0,83; dos estudios, 1572 mujeres; GRADE: calidad baja). También se encontró que el tratamiento activo del periodo de alumbramiento puede hacer poca o ninguna diferencia en cuanto al número de recién nacidos ingresados en las unidades neonatales (RR promedio 0,81; IC del 95%: 0,60 a 1,11; dos estudios, 3207 recién nacidos; GRADE: calidad baja). No se conoce con certeza si el tratamiento activo del periodo de alumbramiento reduce el número de recién nacidos con ictericia que requieren tratamiento (RR 0,96; IC del 95%: 0,55 a 1,68; dos estudios, 3142 recién nacidos, I2 = 66%; GRADE: calidad muy baja). No hubo datos sobre los demás resultados primarios de HPP muy grave en el momento del parto (más de 2500 ml), mortalidad materna o policitemia neonatal que requirió tratamiento.
El tratamiento activo reduce la pérdida promedio de sangre materna al momento dl parto y probablemente reduce la tasa de pérdida de sangre primaria superior a 500 ml, así como la administración de uterotónicos terapéuticos. El tratamiento activo probablemente también reduce el peso promedio del recién nacido al parto, lo que refleja el menor volumen sanguíneo debido a la interferencia con la transfusión de placenta. Además, puede reducir la necesidad de una transfusión de sangre materna. Sin embargo, el tratamiento activo puede aumentar la presión arterial diastólica materna, los vómitos después del parto, los dolores posteriores al parto, la administración de analgésicos desde el parto hasta el alta de la sala de trabajo de parto y el número de mujeres que vuelven al hospital con hemorragia (resultado no especificado previamente).
En la comparación de las mujeres con bajo riesgo de hemorragia excesiva hubo hallazgos similares, excepto que no fue posible determinar con certeza si hubo diferencias entre los grupos para la HPP primaria grave (RR promedio 0,31; IC del 95%: 0,05 a 2,17; dos estudios, 2941 mujeres, I2 = 71%), Hb materna inferior a 9 g/dl a las 24 a 72 horas (RR promedio 0,17; IC del 95%: 0,02 a 1,47; un estudio, 193 mujeres) o la necesidad de ingreso neonatal (RR promedio 1,02; IC del 95%: 0,55 a 1,88; un estudio, 1512 mujeres). En este grupo, el tratamiento activo puede hacer poca diferencia en cuanto a la tasa de ictericia neonatal que requiere fototerapia (RR promedio 1,31; IC del 95%: 0,78 a 2,18; un estudio, 1447 mujeres).
La hipertensión y la interferencia en la transfusión placentaria se podrían evitar al utilizar modificaciones del paquete de tratamiento activo, por ejemplo, omitir los fármacos derivados del cornezuelo de centeno y diferir el pinzamiento del cordón, pero en esta revisión no hay evidencia directa al respecto.
Conclusiones de los autores
Aunque los datos parecieron mostrar que el tratamiento activo redujo el riesgo de una HPP primaria grave superior a 1000 ml en el momento del parto, no existe certeza en cuanto a este hallazgo debido a la calidad muy baja de la evidencia. El tratamiento activo puede reducir la incidencia de anemia materna (Hb inferior a 9 g/dl) después del parto, pero se identificaron daños como la hipertensión postnatal, el dolor y el regreso al hospital debido a hemorragia.
En las mujeres con bajo riesgo de hemorragia excesiva, no se conoce con certeza si hubo diferencias entre el tratamiento activo y el expectante para la HPP grave o la Hb materna de menos de 9 g/dl (a las 24 a 72 horas). Se podría dar a las mujeres información sobre los efectos beneficiosos y perjudiciales de ambos métodos para apoyar una elección informada. Debido a las inquietudes acerca del pinzamiento inmediato del cordón y los posibles efectos adversos de algunos uterotónicos, actualmente es fundamental examinar los componentes individuales de el tratamiento en el periodo expulsivo del trabajo de parto. También se necesitan datos de países de bajos ingresos.
Se debe señalar que esta revisión solo incluye un número reducido de estudios con un número relativamente pequeño de participantes, y la calidad de la evidencia de los resultados primarios es baja o muy baja.
PICO
Resumen en términos sencillos
Parto de la placenta en el periodo de alumbramiento del trabajo de parto
¿Cuál es el problema?
El objetivo de esta revisión Cochrane fue examinar las diferentes formas de alumbramiento de la placenta después del parto del recién nacido; tratamiento expectante, activo o mixto. La pregunta fue ¿cuáles son los efectos beneficiosos y los daños para todas las mujeres, pero específicamente para las mujeres con bajo riesgo de hemorragia grave? Se recopilaron y analizaron todos los estudios relevantes para responder esta pregunta (22 de enero 2018).
¿Por qué es esto importante?
Una vez que se produce el parto de un recién nacido, continúan las contracciones del útero, lo que hace que la placenta se separe de la pared del útero. La madre entonces expulsa la placenta, o "alumbra". A lo anterior se le llama tratamiento expectante del periodo de alumbramiento del trabajo de parto. El tratamiento activo del periodo de alumbramiento tiene tres componentes: 1) se administra un medicamento (un uterotónico) para ayudar a contraer el útero; 2) se pinza el cordón temprano (generalmente antes, junto o inmediatamente después de administrar el uterotónico); 3) se aplica tracción al cordón con contrapresión en el útero para expulsar la placenta (tracción controlada del cordón). El tratamiento mixto utiliza algunos, pero no todos, de los tres componentes. El tratamiento activo se introdujo para tratar de reducir la pérdida grave de sangre al momento del parto. Lo anterior es una de las principales causas de muerte de las mujeres en los países de bajos ingresos, donde las mujeres tienen más probabilidades de estar mal alimentadas, presentar anemia y padecer enfermedades infecciosas. En los países de ingresos altos la hemorragia ocurre con mucha menos frecuencia; no obstante, el tratamiento activo se ha convertido en una práctica estándar en muchos de ellos.
¿Qué evidencia se encontró?
Se encontraron ocho estudios que proporcionaron datos y en los que participaron 8892 mujeres y sus recién nacidos. Todos los estudios se realizaron en entornos hospitalarios, siete en países de altos ingresos y uno en un país de bajos ingresos. Cuatro estudios compararon el tratamiento activo con el tratamiento expectante y cuatro compararon el tratamiento activo con el tratamiento mixto.
En general, la calidad de la evidencia fue baja o muy baja y se necesitan más datos para tener confianza en los resultados. Para todas las mujeres, independientemente del riesgo de hemorragia grave, el tratamiento activo puede reducir la hemorragia grave y la anemia. Sin embargo, también puede reducir el peso del recién nacido y aumentar la presión arterial de la madre, los dolores posteriores, los vómitos y el número de mujeres que vuelven al hospital con hemorragia. Los resultados fueron similares para las mujeres con bajo riesgo de hemorragia, aunque no estuvo claro si hubo alguna diferencia en cuanto a la incidencia de hemorragia grave o anemia.
¿Qué significa esto?
Las mujeres deben recibir información antes de dar a luz para ayudarlas a tomar decisiones informadas. Algunos efectos adversos experimentados por las madres se pueden evitar posiblemente mediante el uso de fármacos específicos. Retrasar el pinzamiento del cordón umbilical puede beneficiar al recién nacido al evitar la reducción de peso al nacer por el pinzamiento temprano del cordón, pero se necesitan más estudios de investigación. También puede ser que el simple hecho de administrar un uterotónico pueda reducir la hemorragia grave, sin otros componentes del tratamiento activo. Se necesitan más estudios de investigación, en particular en los países de bajos ingresos.
Authors' conclusions
Summary of findings
| Active versus expectant management of the third stage of labour (all women) | ||||||
| Population: all women who expected a vaginal birth at 24 weeks' gestation or later and their babies Setting: UK and Ireland, hospital setting. The countries were classified as 'higher‐income' and 'lower‐income', with the border between lower‐middle‐income and upper‐middle‐income being the cut‐off. All studies included in this main analysis were undertaken in higher‐income countries (defined according to World Bank definitions 2018). Intervention: active management of the third stage of labour | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Expectant management of the third stage of labour | Active management of the third stage of labour | |||||
| Severe primary PPH (clinically estimated or measured blood loss ≥ 1000 mL at time of birth) | 24 per 1000 | 8 per 1000 | RR 0.34 | 4636 | ⊕⊝⊝⊝ | |
| Very severe primary PPH (clinically estimated or measured blood loss ≥ 2500 mL at time of birth) | See comment | See comment | Not estimable | 0 | See comment | No data |
| Maternal mortality | See comment | See comment | Not estimable | 0 | See comment | No data |
| Maternal Hb < 9 g/dL 24‐72 hours postpartum | 71 per 1000 | 36 per 1000 | RR 0.50 | 1572 | ⊕⊕⊝⊝ | |
| Admission to SCBU/NICU | 52 per 1000 | 42 per 1000 | RR 0.81 | 3207 | ⊕⊕⊝⊝ | |
| Neonatal jaundice requiring phototherapy or exchange transfusion | 49 per 1000 | 47 per 1000 | RR 0.96 | 3142 | ⊕⊝⊝⊝ | |
| Neonatal polycythaemia treated with dilutional exchange transfusion | See comment | See comment | Not estimable | 0 | See comment | No data |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| aRisk of bias: of the three studies providing data for this outcome, all are at low risk of bias for sequence generation (selection bias) and allocation concealment (selection bias). All are at high risk of bias for lack of blinding for clinicians and women and all are unclear for blinding of outcome assessment. Two studies are at low risk of bias for incomplete outcome data (attrition bias), and one is unclear. Two are at high risk of selective reporting (reporting bias) and one is unclear. One study is at high risk of other bias and two are unclear (see 'Risk of bias' tables and Figure 2). Downgraded 1. bRisk of bias: of the two studies providing data for this outcome, both are at low risk of bias for sequence generation (selection bias) and one is at low risk of bias for allocation concealment (selection bias) and the other is unclear. Both are at high risk of bias for lack of blinding of clinicians and women, both are unclear for blinding of outcome assessment (although unlikely to affect Hb measurements). One is at high risk of bias for incomplete outcome data (attrition bias) while the other is unclear. One is high risk of bias for selective reporting (reporting bias), the other is unclear. Both studies are at high risk of other bias (see 'Risk of bias' tables and Figure 2). Downgraded 1. cRisk of bias: of the two studies providing data for this outcome, both are at low risk of bias for sequence generation (selection bias) and allocation concealment (selection bias). Both are at high risk of bias for lack of blinding of clinicians and women, both are unclear for blinding of outcome assessment. One is at low risk of bias for incomplete outcome data (attrition bias), the other is unclear. Both are at high risk of bias for selective reporting (reporting bias) and both are at high risk for other biases (see 'Risk of bias' tables and Figure 2). Downgraded 1. dRisk of bias: of the two studies providing data for this outcome, both are at low risk of bias for sequence generation (selection bias) and allocation concealment (selection bias). Both are at high risk of bias for lack of blinding of clinicians and women, both are unclear for blinding of outcome assessment. One is low risk of bias for incomplete outcome data (attrition bias), the other is unclear. Both are at high risk of bias for selective reporting (reporting bias) and both are at high risk of other biases (see 'Risk of bias' tables and Figure 2). Downgraded 1. | ||||||
Background
Description of the condition
The third stage of labour is the time from the birth of the baby to the expulsion of the placenta and membranes. Once the baby is born, the uterus continues to contract and reduce in size. There is a lack of full understanding of the physiology of the third stage of labour, but recent work using ultrasonography has demonstrated that the process of placental separation has three distinct phases (Herman 2002). The first, or latent phase, consists of strong uterine contractions, which lead to thickening of the uterine muscle, thus causing a shearing force to occur between the elastic uterine wall and the more rigid placenta (Herman 2002). Continued contractions lead to gradual separation of the placenta, commencing at one of the poles (most commonly the lower) and spreading slowly during the contraction or detachment phase until full separation occurs. This is followed by delivery of the placenta in the expulsion phase (Herman 2002). Muscle fibres surrounding the maternal vessels contract to prevent excessive bleeding (Inch 1985), and the mother's coagulation system is activated temporarily (Bonnar 1970).
There is always some blood loss during the third stage of labour as the placenta separates and is delivered, but what might be considered a normal amount of loss is the subject of debate (Gyte 1992). Nevertheless, some women can suffer from considerable blood loss during or after the third stage of labour. This can be a primary haemorrhage (within the first 24 hours; Mousa 2014), or a secondary haemorrhage (between 24 hours and six weeks; McDonald 2003). Postpartum haemorrhage (PPH) is commonly defined as a blood loss in excess of 500 mL (WHO 2003), with severe haemorrhage being a loss of 1000 mL or more and very severe haemorrhage being a loss of 2500 mL or more (Bloomfield 1990; Greer 1998; Penney 2005). However, the impact of blood loss at birth on an individual woman can vary considerably and will depend not only on the volume of blood lost, but also on her general state of health, the speed of the loss, her haemoglobin (Hb) levels at the time and her coagulation system. It is well documented that blood loss is consistently under‐ or over‐estimated by clinicians (Razvi 2008), although many centres do try to measure and record blood loss accurately. In well‐nourished women, some consider that, in general, there is little impact from a blood loss of 500 mL (Bloomfield 1990), this being equivalent to a routine blood donation (Burnley 2006), but in women in low‐income countries who may be poorly nourished and anaemic, this loss can cause considerable morbidity or mortality. It has been estimated that at least 25% of maternal deaths in a number of countries are due to haemorrhage; most due to PPH (Abouzaher 1998; Khan 2006). The vast majority of these happen in the developing world, and PPH is the leading cause of maternal mortality in sub‐Saharan Africa (Lazarus 2005). However, a study in Mexico (Romero‐Gutierrez 2007), reported that while the leading cause of maternal death was haemorrhage, two‐thirds of bleeding‐related deaths resulted from placental abruption, placenta accreta, placenta praevia, and peripartum hysterectomy, rather than uterine atony (poor contraction of the muscles in the uterus). Significant morbidity does occur, though, from major bleeding due to uterine atony, which is far more common than the other causes of bleeding listed above. The seriousness with which PPH is viewed by professionals is evidenced in joint policy statements between the International Confederation of Midwives (ICM) and the International Federation of Gynaecology and Obstetrics (FIGO) (ICM‐FIGO 2003; ICM‐FIGO 2006), and the World Health Organization (WHO 2003), all of which have recommended active management of the third stage of labour. Debate continues among women and practitioners on the optimum method of management of the third stage of labour to balance the benefits and harms.
There are two distinct approaches to the clinical management of the third stage of labour: expectant and active management. However, a third approach is sometimes used that consists of a combination of components of both expectant and active management: this has been referred to as 'mixed management' or the 'piecemeal approach' (Prendiville 1989). Expectant, active and mixed management approaches, and comparisons of different types of active management, have been the subject of a number of critical reviews (Elbourne 1995; Gyte 1994; Maughan 2006; McDonald 2007a; Prendiville 1989; Prendiville 1996; Soltani 2008).
Description of the intervention
(a) Expectant management of the third stage of labour
Expectant management is also known as conservative or physiological management and is popular in some northern European countries (Nordstrom 1997), and in New Zealand (Dixon 2013). It is also practised on occasion in midwife‐led units and in home births in the UK and Ireland (Begley 2009; Blackburn 2008; Fry 2007; Kanikosmay 2007), and is the usual practice when birthing at home or in the community in some low‐income countries. The main principle of expectant management is a 'hands off' approach, where signs of placental separation are awaited and the placenta is birthed spontaneously or with the aid of gravity, maternal pushing (Begley 2012; Inch 1985) or, sometimes, nipple stimulation (Inch 1985) hence:
-
a prophylactic uterotonic agent is not administered;
-
ideally, the umbilical cord is neither clamped nor cut until the placenta has been delivered but, at a minimum, caregivers have waited until cord pulsation has ceased; and
-
the placenta is delivered spontaneously with the aid of gravity and sometimes by maternal effort (Begley 2012; Rogers 1998).
There can be variations within expectant management. For example, some caregivers will wait for the placenta to be delivered before clamping and cutting the cord whilst others, for convenience, just wait until pulsation has finished. Breastfeeding or other means of stimulating the physiological release of oxytocin, such as nipple stimulation, is sometimes also used (Bullough 1989), but is not an essential component of expectant management. Some 'expert' midwives will use gentle traction on the cord once the placenta is seen to be in the vagina (Begley 2012), with good results.
(b) Active management of the third stage of labour
In active management of the third stage of labour, the clinician intervenes by using the following package of interventions (Prendiville 1989):
-
the routine administration of a prophylactic uterotonic drug just before, with, or immediately after, the birth of the baby;
-
early cord clamping and cutting* (i.e. prior to, alongside, or immediately after administration of an oxytocic, which is before cord pulsation ceases); and
-
controlled cord traction to deliver the placenta.
*current WHO recommendations (WHO 2014), are to delay cord clamping, and the National Institute for Health and Clinical Excellence (NICE) now recommends "deferred" cord clamping (NICE 2014).
These interventions are implemented routinely and prophylactically in an attempt to reduce the blood loss associated with the third stage of labour and to reduce the risk of PPH. There are many possible variations with this package of interventions.
-
There are different uterotonic drugs that can be used, for example, oxytocin (intravenous (IV) or intramuscular (IM)); syntometrine (IM); ergometrine (IV or IM); misoprostol (IM; Liabsuetrakul 2018; McDonald 2007b; Su 2012; Tunçalp 2012; Westhoff 2013), carbetocin, or paired combinations of these drugs (Gallos 2018). There is also debate over the route of administration and dosage of the drugs used. Recent guidelines from WHO, FIGO, ICM and NICE all recommend the use of 10 IU (international units) of oxytocin IM ((ICM‐FIGO 2003; NICE 2014; WHO 2012). Misoprostol is potentially the most important uterotonic for use in some low‐income countries because it is stable at ambient temperatures and is inexpensive (Parsons 2007). However, it does have adverse side effects (Mousa 2014), such as shivering, nausea and headaches, and it has been shown to be less effective than other agents (Tunçalp 2012). A recent network analysis, however, suggests that the three most effective drugs for preventing PPH of 500 mL or more are ergometrine and oxytocin, carbetocin, and misoprostol combined with oxytocin (Gallos 2018).
-
There are differing timings for giving the prophylactic uterotonic drug, for example, with the crowning of the baby's head; with the birth of the anterior shoulder; immediately after the birth of the baby; after the birth of the baby but before the placenta is delivered (Harris 2004), and after the placenta is delivered (Winter 2007). The timing of administration of uterotonic drugs is the subject of another Cochrane Review (Soltani 2010).
-
There can be variation in the time when the cord is clamped and cut; this can be immediately the baby is born; within a set time after the birth, for example, within 30 seconds or a minute; or anytime before umbilical cord pulsation ceases (McDonald 2013; Rabe 2012; Van Rheenan 2007).
-
There are also different timings for the initiation of controlled cord traction, such as waiting for signs of placental separation or not (McDonald 2003).
-
There can also be a delay in using the whole package of active management until after cord pulsation ceases, which has been described as ‘delayed active management’ (Gyte 2006).
-
Some guidelines (e.g. ICM‐FIGO 2003), add uterine massage to the active management package although there is little evidence to support this (Abdel‐Aleem 2010).
Placental cord drainage is sometimes used with active management of the third stage. This involves releasing the clamp on the maternal end of the umbilical cord to allow the blood from the placental side to drain, thus reducing the size of the placenta and thereby hoping to help separation and reduce the chance of a retained placenta (Prendiville 1989; Soltani 2011).
Some of these variations in the components of active management of the third stage of labour may no longer be considered good practice (e.g. early cord clamping), but may, nonetheless, be used in included studies identified for this review.
(c) Mixed management of the third stage of labour
Mixed management of the third stage of labour, (or 'combined' or 'piecemeal' management), which consists of a mixture of some of the components of both active and expectant management of the third stage, but without exclusively containing all the components of either. Although active management of the third stage is usually recommended (ICM‐FIGO 2006; NICE 2014; WHO 2003), there are many variations, and in practice some women may actually receive mixed management (Harris 2006; Mercer 2000). Mixed management of the third stage might include, for example: (1) early uterotonic administration, cord clamping after pulsation ceases and controlled cord traction; or (2) delayed uterotonic administration until cord pulsation ceases, then cord clamping and controlled cord traction. These forms of mixed management of the third stage are of interest because of the evidence of benefits from delayed cord clamping for the baby (McDonald 2013; Mercer 2008; Rabe 2012).
How the intervention might work
Expectant management
Expectant management of the third stage relies on the natural contractions of the uterus, stimulated by a surge of physiological oxytocin at birth, and anything that interferes with this oxytocin release may reduce the effectiveness of the physiological process in the third stage (Inch 1985). Release of oxytocin can, for example, be inhibited by anxiety through the excess release of adrenaline (Buckley 2004).
Hence, expectant management of the third stage of labour is commonly only considered appropriate following a labour where there has been no interference with the natural release of oxytocin, for example, where oxytocin augmentation, induction, epidural or narcotic analgesia, or both, have not been used (Buckley 2004; Fry 2007); but some will consider that these aspects still need to be assessed in well‐designed studies. This type of labour is more likely when the woman has positive psychological support from her midwife, or other trained supporter, who encourages her to listen to her body's messages about movement, positioning, hydration and nutrition (Bohren 2017; Buckley 2004; Sandall 2016).
Active management
In active management of the third stage of labour, it is suggested that the prophylactic administration of a uterotonic will reduce bleeding and the risk of severe haemorrhage (Greer 1998; Prendiville 1989). The role of early cord clamping and controlled cord traction in the reduction of bleeding is less clear, but it is thought that once the uterotonic drug has been administered, it is important to deliver the placenta quickly to prevent it being retained. Applying a clamp to the cord thus gives the caregiver something to grasp in order to deliver the placenta quickly by applying controlled cord traction. Active management of the third stage has been standard practice in many parts of the world for many years (Prendiville 1989). Recently, however, arguments have been put forward for a delay in cord clamping, pointing out that it is not an evidence‐based part of the package of active management (Weeks 2007). A Cochrane Review found that neither early nor late cord clamping showed any significant difference in PPH rates (McDonald 2013).
A number of Cochrane Reviews have been conducted examining different aspects of active management of the third stage of labour. These include reviews on prophylactic oxytocin in the third stage of labour (Westhoff 2013); prophylactic ergometrine‐oxytocin versus oxytocin for the third stage of labour (McDonald 2007b); prophylactic use of ergot alkaloids in the third stage of labour (Liabsuetrakul 2018); prostaglandins for preventing PPH (Tunçalp 2012); oxytocin agonists for preventing PPH (Su 2012); timing of cord clamping in term infants (McDonald 2013) and timing of cord clamping in preterm infants (Rabe 2012).
Potential adverse effects
Interventions used in active management of the third stage have some adverse effects, due mainly to the uterotonic drugs used and to the common practice of early clamping of the cord.
Uterotonic drugs can increase the risk of hypertension, nausea and vomiting for women (Maughan 2006), and which appear to be related to the use of ergometrine‐based drugs. Active management in many countries has moved away from ergometrine‐based uterotonics, for this reason, and possibly also due to clinicians' fear of retained placenta, although a review of ergometrine‐based drugs compared with other uterotonics showed no difference in rates of manual removal of placentae (McDonald 2007b).
The potential consequences for the newborn infant of active management of the third stage of labour relate mainly to the timing of cord clamping. The effects on the neonate of early versus deferred cord clamping have been explored in Cochrane and other systematic reviews (Hutton 2007; McDonald 2013; Rabe 2012). Early cord clamping reduces the volume of placental blood transfusion and thus reduces the baby's blood volume at birth by about 20% for term infants (RCOG 2009; Werner 2005). This results in lower blood haematocrit (HCT) levels and Hb concentrations after birth in term infants but the long‐term importance of this effect is unknown (Hutton 2007; McDonald 2013; Prendiville 1989; Van Rheenan 2007). Potentially, placental transfusion may be more important for infants born in low‐ and middle‐income settings where iron‐deficiency anaemia exacerbated by nutritional and infectious insults may have substantial and long‐term adverse effects on growth and development (Van Rheenan 2007). For preterm infants, another specific concern is the effect of postnatal placental transfusion on neonatal haemodynamic transition processes. The Cochrane Review of early versus delayed cord clamping for preterm infants found some evidence that infants who had early cord clamping had a higher risk of hypotension treated with volume‐transfusion and of intraventricular haemorrhage (Rabe 2012).
In contrast, early cord clamping also results in lower postnatal levels of plasma bilirubin and a lower incidence of neonatal jaundice that requires phototherapy (McDonald 2013; Rabe 2012). Treatment of neonatal jaundice may result in mother‐infant separation that delays the initiation and establishment of breastfeeding and disrupts early neonatal metabolic adaptation (Mercer 2001). For infants born in low‐ or middle‐income settings, or in rural or remote settings distant from healthcare facilities, the need for phototherapy (or its lack of availability) may be of greater clinical importance.
If uterotonic drugs are administered before delivery of the infant, for example, inadvertently prior to the birth of an undiagnosed twin, then disruption of the placental‐uterine wall interface and interruption of placental‐umbilical blood flow may cause acute perinatal asphyxia compromising neonatal cardio‐respiratory transition. Newborn infants compromised at birth are more likely to need transition support (cardio‐respiratory resuscitation). If an asphyxial insult has been severe or prolonged (for example, if exacerbated by obstructed labour such as shoulder dystocia) then other potential consequences may include neonatal encephalopathy, with its associated risk of mortality and long‐term neurodevelopmental morbidity.
Why it is important to do this review
We undertook this review because of the need to determine if active, expectant management, or a mixed management package, was most likely to be of overall benefit. It is important to assess the impact of all these forms of care on both the mother and baby. We believe that this review is highly relevant to families and clinicians, as women frequently enquire about the differences in third‐stage management during the antenatal period. This is an update of review last published in 2015 (Begley 2015).
Objectives
-
To compare the effects of active versus expectant management of the third stage of labour on severe primary postpartum haemorrhage (PPH) and other maternal and infant outcomes.
-
To compare the effects of variations in the packages of active and expectant management of the third stage of labour on severe primary PPH and other maternal and infant outcomes.
Methods
Criteria for considering studies for this review
Types of studies
We included all randomised, and quasi‐randomised, controlled trials of active versus expectant management of the third stage of labour. Cluster‐randomised trials were eligible for inclusion, but none were identified.
Types of participants
All women who expected a vaginal birth at 24 weeks' gestation or later. We looked at women in higher‐income settings separately from women in lower‐income settings.
Types of interventions
(a) Active management of the third stage of labour, which is here defined as the package of interventions comprising:
-
the administration of a prophylactic uterotonic just before, with, or immediately after the birth of the baby;
-
early cord clamping and cutting (from immediately after the birth of the baby's head in the case of a nuchal cord, or immediately after the birth of the baby to, usually, within a minute of birth);
-
controlled cord traction to aid the delivery of the placenta.
(b) Expectant management of the third stage of labour, which is here defined as:
-
no prophylactic administration of a uterotonic;
-
the umbilical cord is neither clamped nor cut until the placenta has been delivered or until cord pulsation has ceased; and
-
the placenta is delivered spontaneously with the aid of gravity and sometimes by maternal effort.
-
None of the components of active management, described above, are employed routinely.
(c) Mixed management of the third stage of labour consists of a mixture of some of the components of both active and expectant management of the third stage, but without exclusively containing all the components of either (Table 1).
| Terms | Definitions used in this review |
| Expectant management of third stage of labour |
|
| Active management of third stage of labour |
|
| Mixed management of third stage of labour | A mixture of some of the components of both active and expectant management of third stage of labour, but without exclusively containing all the components of either. There can be a number of different mixed third stage managements, for example:
|
| Early prophylactic uterotonic | Prophylactic uterotonic drug administered just before, with, or immediately after, the birth of the infant |
| Delayed prophylactic uterotonic | Prophylactic uterotonic drug administered after the cord pulsation has ceased |
| Early cord clamping | The application of a clamp to the umbilical cord within 60 seconds of the birth of the infant (McDonald 2013) |
| Delayed cord clamping | The application of a clamp to the umbilical cord more than 1 minute after birth or when cord pulsation has ceased (McDonald 2013) |
| Sarnat staging for hypoxic ischaemic encephalopathy (Sarnat 1976) |
|
Comparisons
-
Active versus expectant management of the third stage of labour: all women
-
Active versus expectant management of the third stage of labour: women at low risk of bleeding
-
Active versus mixed management of the third stage of labour, with early prophylactic uterotonic administration, delayed cord clamping and controlled cord traction
-
Active versus mixed management of the third stage of labour, with delayed prophylactic uterotonic administration, delayed cord clamping and controlled cord traction
-
Active versus mixed management of the third stage of labour, with delayed prophylactic uterotonic administration, delayed cord clamping, no controlled cord traction
-
Expectant versus mixed management of the third stage of labour, with early prophylactic uterotonic administration, delayed cord clamping and controlled cord traction
-
Expectant versus mixed management of the third stage of labour, with delayed prophylactic uterotonic administration, delayed cord clamping and controlled cord traction
-
Expectant versus mixed management of the third stage of labour, with delayed prophylactic uterotonic administration, delayed cord clamping, no controlled cord traction
-
Active versus mixed management of the third stage of labour with uterotonic after placental delivery, immediate cord clamping, no controlled cord traction
-
Active versus mixed management of the third stage of labour with no routine uterotonic, early cord clamping, no controlled cord traction
-
Active versus mixed management of the third stage of labour with no routine uterotonic, early cord clamping, and controlled cord traction
We included comparisons three to eight because of the review team's awareness of these different forms of clinical management of the third stage of labour and following the results of two reviews that indicated the benefits of delaying cord clamping for the baby (McDonald 2013; Rabe 2012). There are other variations of mixed management that could also be considered, for example, variations in controlled cord traction (Hofmeyr 2015), but we considered the above to be the most commonly used and thus important to review. We included comparisons nine to 11 because we added studies that had used these comparisons to this review update.
Types of outcome measures
We selected outcome measures in order of importance with due recognition of the core data set of outcome measures identified by Devane 2007.
Primary outcomes
Maternal
-
*Severe primary postpartum haemorrhage (PPH) at time of birth (clinically estimated or measured blood loss greater than or equal to 1000 mL)
-
*Very severe primary PPH at time of birth (clinically estimated or measured blood loss greater than or equal to 2500 mL)
-
Maternal mortality
-
Maternal Hb concentration less than 9 g/dL 24 to 72 hours postpartum
Infant
-
Admission to neonatal special care or intensive care unit
-
Neonatal jaundice requiring phototherapy or exchange transfusion
-
Neonatal polycythaemia treated with dilutional exchange transfusion
Secondary outcomes
Maternal
-
*Severe primary PPH after delivery of placenta and up to 24 hours (clinically estimated or measured blood loss greater than or equal to 1000 mL)
-
*Severe primary PPH at time of birth and up to 24 hours (clinically estimated or measured blood loss greater than or equal to 1000 mL)
-
*Primary blood loss equal to or greater than 500 mL at time of birth (clinically estimated or measured)
-
*Primary blood loss equal to or greater than 500 mL after delivery of placenta and up to 24 hours (clinically estimated or measured)
-
*Primary blood loss equal to or greater than 500 mL at time of birth and up to 24 hours (clinically estimated or measured)
-
*Mean blood loss (mL) at time of birth (clinically estimated or measured)
-
*Mean blood loss (mL) after delivery of placenta and up to 24 hours (clinically estimated or measured).
-
*Mean blood loss (mL) at time of birth and up to 24 hours (clinically estimated or measured)
-
Maternal blood transfusion
-
Clinical signs of severe blood loss at the time of birth, for example, woman feeling breathless, weak, faint, pale, exhausted
-
Therapeutic uterotonics during the third stage or within the first 24 hours, or both
-
Mean length of the third stage (minutes)
-
Manual removal of the placenta as defined by study authors
-
Diastolic blood pressure greater than 90 mmHg between birth of baby and discharge from the labour ward
-
Vomiting between birth of baby and discharge from the labour ward
-
Any analgesia between birth of the baby and discharge from the labour ward
-
Women's assessment of pain during the third stage as reported by study authors
-
Secondary blood loss/any vaginal bleeding needing treatment (after 24 hours and before six weeks)
-
Amount of lochia either estimated or measured after 24 hours and up to discharge from hospital
-
Surgical evacuation of retained products of conception
-
Afterpains ‐ abdominal pain associated with the contracting uterus in the postpartum period
Infant
-
Apgar score less than 7 at five minutes
-
Birthweight
-
Neonatal encephalopathy assessed using Sarnat staging (Sarnat 1976; Table 1)
-
Neonatal mortality (not pre‐specified)
-
Intraventricular haemorrhage ‐ papillae grade III/IV (for infants born before 34 weeks' gestation only)
-
Number of infants who received a red blood cell transfusion
-
Infant Hb level at 24 to 72 hours
-
Infant Hb level at three to six months
-
Infant iron indices (ferritin) at three to six months
-
Exclusive breastfeeding at discharge
-
Neurodevelopmental, cognitive or developmental outcomes assessed after age 18 months
*All PPH amounts and mean blood losses are now expressed at three time periods, 'at the time of the birth', 'after delivery of the placenta and up to 24 hours', and 'at the time of birth and up to 24 hours'.
Search methods for identification of studies
The following search methods section of this review is based on a standard template used by Cochrane Pregnancy and Childbirth.
Electronic searches
For this update, we searched Cochrane Pregnancy and Childbirth’s Trials Register by contacting their Information Specialist (22 January 2018).
The Register is a database containing over 24,000 reports of controlled trials in the field of pregnancy and childbirth. It represents over 30 years of searching. For full current search methods used to populate Pregnancy and Childbirth’s Trials Register including the detailed search strategies for CENTRAL, MEDLINE, Embase and CINAHL; the list of handsearched journals and conference proceedings, and the list of journals reviewed via the current awareness service, please follow this link to the editorial information about the Cochrane Pregnancy and Childbirth.
Briefly, Cochrane Pregnancy and Childbirth’s Trials Register is maintained by their Information Specialist and contains studies identified from:
-
monthly searches of the Cochrane Central Register of Controlled Trials (CENTRAL);
-
weekly searches of MEDLINE (Ovid);
-
weekly searches of Embase (Ovid);
-
monthly searches of CINAHL (EBSCO);
-
handsearches of 30 journals and the proceedings of major conferences;
-
weekly current awareness alerts for a further 44 journals plus monthly BioMed Central email alerts.
Two people screen search results and review the full text of all relevant study reports identified through the searching activities described above. Based on the intervention described, the Information Specialist assigns each study report a number that corresponds to a specific Pregnancy and Childbirth review topic (or topics), and then adds it to the Register. The Information Specialist searches the Register for each review using this topic number rather than keywords. This results in a more specific search set that has been fully accounted for in the relevant review sections (Included studies; Excluded studies; Studies awaiting classification).
In addition, we searched ClinicalTrials.gov and the WHO International Clinical Trials Registry Platform (ICTRP) for unpublished, planned and ongoing study reports (22 January 2018) using the search methods described in Appendix 1.
Searching other resources
We retrieved additional relevant references cited in papers identified through the above search strategy and assessed their suitability for inclusion in the review.
We did not apply any language or date restrictions.
Data collection and analysis
For methods used in the previous version of this review, see Begley 2015.
For this update, we used the following methods for assessing the five reports that we identified as a result of the updated search.
The following methods section of this review is based on a standard template used by Cochrane Pregnancy and Childbirth.
Selection of studies
We obtained all potentially eligible studies identified by the search strategy as full‐text papers and two review authors assessed each study for potential inclusion. We resolved any disagreements through discussion with at least one additional review author. None of the potentially eligible studies required translation. We sought and received additional information from Yildirim 2016.
Data extraction and management
We used the data extraction form designed for the previous version of this review (Begley 2015), to extract data. Two review authors extracted the data independently from the included study using the form. We resolved discrepancies through discussion with at least one additional review author. In the previous version of this review, two review authors (Gillian Gyte (GG), Declan Devane (DD)), and a member of the Cochrane Pregnancy and Childbirth Group's staff independently reviewed Begley's paper (Begley 1990), and the lead author of this review was not involved in any discussions of the paper's inclusion, or assessment of its risk of bias status. We used the Review Manager software (Review Manager 2014), to enter all data, which were checked independently.
Assessment of risk of bias in included studies
Two review authors (GG and LB) independently assessed risk of bias as a measure of methodological quality of included studies using the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2017). We resolved discrepancies through discussion with at least one additional review author. When information regarding any of the criteria was unclear, we contacted the authors of the original reports to provide further details. Where these data were unobtainable, and the missing data were thought to introduce serious bias, we explored the impact of including such studies in the overall assessment of results by sensitivity analysis. We used the following criteria in the assessment of bias.
(1) Random sequence generation (checking for possible selection bias)
We described for each included study the method used to generate the allocation sequence in sufficient detail to allow an assessment of whether it should produce comparable groups.
We assessed the method as:
-
low risk of bias (any truly random process, e.g. random number table; computer random number generator);
-
high risk of bias (any non‐random process, e.g. odd or even date of birth; hospital or clinic record number);
-
unclear risk of bias.
(2) Allocation concealment (checking for possible selection bias)
We described for each included study the method used to conceal allocation to interventions prior to assignment and assessed whether intervention allocation could have been foreseen in advance of, or during recruitment, or changed after assignment.
We assessed the methods as:
-
low risk of bias (e.g. telephone or central randomisation; consecutively numbered sealed opaque envelopes);
-
high risk of bias (open random allocation; unsealed or non‐opaque envelopes, alternation; date of birth);
-
unclear risk of bias.
(3.1) Blinding of participants and personnel (checking for possible performance bias)
It is not possible to blind participants or personnel in these trials, as the fact that a uterotonic has been given (rather than a placebo, or nothing) is usually apparent to both women (who feel a strong contraction or pain) and clinicians (who can see or feel a strongly contracted uterus) following injection of a uterotonic. In addition, it is clear, in many cases, to both women and clinicians if early versus late cord clamping is practised or if cord traction versus maternal effort is used. It is usually possible to blind technicians who conduct laboratory tests, but this does not always happen so cannot be presumed to be so.
We assessed the methods as:
-
high risk of bias for participants;
-
high risk of bias for personnel.
(3.2) Blinding of outcome assessment (checking for possible detection bias)
We described for each included study the methods used, if any, to blind outcome assessors from knowledge of which intervention a participant received. We assessed blinding separately for different outcomes or classes of outcomes. It is usually possible to blind technicians who conduct laboratory tests, but this does not always happen so cannot be presumed to be so.
We assessed methods used to blind outcome assessment as:
-
low, high or unclear risk of bias.
(4) Incomplete data collection (checking for possible attrition bias due to the amount, nature and handling of incomplete outcome data)
We describe for each included study and for each outcome the completeness of data, including attrition and exclusions from the analysis. We state whether attrition and exclusions were reported, the numbers included in the analysis at each stage (compared with the total randomised participants), reasons for attrition or exclusion where reported, and whether missing data were balanced across groups or were related to outcomes. Where sufficient information was reported or was sought and supplied by the trial authors, we re‐included missing data in the analyses. No studies required re‐analysis with the original allocated treatment groups being restored to their correct groups. Following these steps, studies were assessed as:
-
low risk of bias ‐ less than 10% attrition at any stage, or 10% to 15% attrition in small sections of data, equal in both groups and due to natural fall‐out of long‐term follow‐up;
-
high risk of bias ‐ more than 20% attrition, or more than 15% exclusion at any stage when the reason for missing data was likely to be related to true outcomes;
-
unclear risk of bias.
Acknowledging that with long‐term follow‐up, complete data are difficult to attain, we discussed whether missing data greater than 20% might (a) be reasonably expected, and (b) impact on outcomes; if the latter, we excluded such studies. We subjected studies where attrition levels were unclear, or missing data greater than 15% occurred, to sensitivity analysis.
(5) Selective reporting bias
We describe for each included study how we examined the possibility of selective outcome reporting bias and we assessed reporting methods as:
-
low risk of bias (where it is clear that all of the study’s pre‐specified outcomes and all expected outcomes of interest to the review have been reported);
-
high risk of bias (where not all the study’s pre‐specified outcomes have been reported; one or more reported primary outcomes were not pre‐specified; outcomes of interest were reported incompletely and so could not be used; study failed to include results of a key outcome that would be expected to have been reported);
-
unclear risk of bias.
(6) Other sources of bias
We also assessed and describe for each included study any important concerns we had about other possible sources of bias (e.g. specific study design, trial stopped early; extreme baseline imbalances). We thus assessed studies as being:
-
low risk of bias;
-
high risk of bias (problems detailed);
-
unclear risk of bias.
(7) Overall risk of bias
We made explicit judgements about whether or not studies were, overall, at high risk of bias, according to the criteria given in the Cochrane Handbook for Systematic Reviews of Interventions with reference to (1) to (6) above (Higgins 2017). As necessary, we explored the impact of the level of bias through undertaking sensitivity analyses.
Assessment of the quality of the evidence using GRADE
We assessed the quality of the evidence using the GRADE approach as outlined in the GRADE Handbook in order to assess the quality of the body of evidence relating to the following outcomes for the main comparison (GRADE 2013).
-
Maternal *severe primary PPH at time of birth (clinically estimated or measured blood loss greater than or equal to 1000 mL)
-
*Very severe primary PPH at time of birth (clinically estimated or measured blood loss greater than or equal to 2500 mL)
-
Maternal mortality
-
Maternal Hb concentration less than 9 g/dL 24 to 72 hours postpartum
-
Infant admission to neonatal special care or intensive care unit
-
Neonatal jaundice requiring phototherapy or exchange transfusion
-
Neonatal polycythaemia treated with dilutional exchange transfusion
We used the GRADEpro Guideline Development Tool (GRADEpro GDT 2015), to import data from Review Manager 5 (Review Manager 2014), in order to create ’Summary of findings’ tables. We produced a summary of the intervention effect and a measure of quality for each of the above outcomes using the GRADE approach. The GRADE approach uses five considerations (study limitations, consistency of effect, imprecision, indirectness and publication bias) to assess the quality of the body of evidence for each outcome. The evidence can be downgraded from 'high quality' by one level for serious (or by two levels for very serious) limitations, depending on assessments for risk of bias, indirectness of evidence, serious inconsistency, imprecision of effect estimates or potential publication bias.
Measures of treatment effect
Dichotomous data
For dichotomous data, we presented results as summary risk ratio (RR) with 95% confidence intervals (CIs).
Continuous data
For continuous data, we used the mean difference (MD) as outcomes were measured in the same way between studies. We planned to use the standardised mean difference (SMD) to combine studies that measured the same outcome, but used different scales, but this was not required.
Unit of analysis issues
Cluster‐randomised trials
We identified no cluster‐randomised trials in this review.
In future updates, we will include cluster‐randomised trials in the analyses along with individually‐randomised studies. We will adjust their sample sizes using the methods described in the Cochrane Handbook for Systematic Reviews of Interventions (section 16.3.4 or 16.3.6), using an estimate of the intracluster correlation co‐efficient (ICC) derived from the study (if possible), from a similar study or from a study of a similar population (Higgins 2011). If we use ICCs from other sources, we will report this and conduct sensitivity analyses to investigate the effect of variation in the ICC. If we identify both cluster‐randomised trials and individually‐randomised studys, we plan to synthesise the relevant information. We will consider it reasonable to combine the results from both if there is little heterogeneity between the study designs and the interaction between the effect of intervention and the choice of randomisation unit is considered to be unlikely.
We will also acknowledge heterogeneity in the randomisation unit and perform a sensitivity analysis to investigate the effects of the randomisation unit.
Cross‐over trials
This is not an eligible study design for this review.
Dealing with missing data
We analysed data on all participants with available data in the group to which they were allocated, regardless of whether or not they received the allocated intervention. If, in the original reports, participants were not analysed in the group to which they were randomised, and there was sufficient information in the study report or in information obtained from the study authors, we planned to restore them to the correct group and analyse accordingly (i.e. intention‐to‐treat (ITT) analysis). No studies required re‐analysis with the original allocated treatment groups being restored to their correct groups. We used the number of women randomised minus the number of participants known to have missing data as the denominators. Where loss to follow‐up was greater than 20%, or where study authors had excluded participants at a level greater than 15% and for reasons that were deemed to impact on outcomes, we excluded that study.
Assessment of heterogeneity
We assessed statistical heterogeneity in each meta‐analysis using the Tau², I² (Higgins 2003), and Chi² statistics. We regarded heterogeneity as substantial if the Tau² was greater than zero and either an I² statistic was greater than 30% or there was a low P value (< 0.10) in the Chi² test for heterogeneity (Deeks 2017).
Assessment of reporting biases
If there had been 10 or more studies in the meta‐analysis, we would have investigated reporting biases (such as publication bias) using funnel plots. We would have assessed funnel plot asymmetry visually. If asymmetry was suggested by a visual assessment, we would have performed exploratory analyses to investigate it (Sterne 2017).
Where we suspected reporting bias (see 'Selective reporting bias' above), we contacted study authors asking them to provide missing outcome data. If this had not been possible, and the missing data were thought to introduce serious bias, we would have explored the impact of including such studies in the overall assessment of results by conducting a sensitivity analysis.
Data synthesis
We carried out statistical analysis using the Review Manager 5 software (Review Manager 2014). We used random‐effects meta‐analyses for combining data because we considered that there was clinical heterogeneity sufficient to expect that the underlying treatment effects would differ between studies. We treated the random‐effects summary as the average of the range of possible treatment effects and we have discussed the clinical implications of treatment effects differing between studies. If we had considered that the average treatment effect was not clinically meaningful, we would not have combined studies. We have presented the results as the average treatment effect with its 95% CI, and the estimates of Tau², P value for the Chi² test and I² statistic (Deeks 2017). We found significant clinical and methodological heterogeneity between studies sufficient to suggest that treatment effects might differ between studies, which supported our choice of random‐effects meta‐analysis.
Subgroup analysis and investigation of heterogeneity
We did not undertake any interaction tests (Deeks 2001), as we were unable to conduct subgroup analyses as planned, due to lack of usable data. We had planned the following subgroup analyses:
-
spontaneous versus operative vaginal birth;
-
nulliparous versus multiparous women;
-
lower‐income versus higher‐income setting;
-
full‐term versus preterm birth (including outcomes specific to preterm babies).
For this update, we deleted the fifth subgroup analysis, ‘low risk of PPH versus high risk of PPH’, as we realised that the analysis we had undertaken of the low‐risk group was in fact a separate comparison rather than a subgroup analysis. We decided to split the countries into 'higher‐income' and 'lower‐income', based on the World Bank definitions, with the border between lower‐middle‐income and upper‐middle‐income being the cut‐off. All the included studies in the main analysis were undertaken in higher‐income countries (defined according to World Bank definitions 2018).
Sensitivity analysis
We performed sensitivity analysis based on study quality, separating high‐quality studies from studies of lower quality. 'High quality' was, for the purposes of this sensitivity analysis, defined as a study having adequate sequence generation, allocation concealment and an attrition rate of less than 20%, given the stated importance of attrition as a quality measure (Tierney 2005).
Results
Description of studies
Results of the search
See: Figure 1.

Study flow diagram
The updated 2018 search retrieved five records to assess and we also re‐assessed one report awaiting classification in the previous section of the review (Rosario 1973). We included one new study (Yildirim 2016), excluded one study (Neri‐Mejia 2016) and linked three clinical trials registry reports to studies already assessed (Hoffman 2006; Jangsten 2011; Rogers 1998). We are still unable to source the full‐text of Rosario 1973.
Included studies
We included eight studies involving 8892 women (analysed) (Begley 1990; Jangsten 2011; Jerbi 2007; Khan 1997; Prendiville 1988; Rogers 1998; Thilaganathan 1993; Yildirim 2016). Included studies were conducted in the UK (Prendiville 1988; Rogers 1998; Thilaganathan 1993), Abu Dhabi (Khan 1997), Ireland (Begley 1990), Sweden (Jangsten 2011), Tunisia (Jerbi 2007), and Turkey (Yildirim 2016) . All studies took place in hospital settings. (See Characteristics of included studies.)
Four studies (4829 women) compared active versus expectant management (Begley 1990; Prendiville 1988; Rogers 1998; Thilaganathan 1993), and four studies (4063 women) compared active versus mixed management (Jangsten 2011; Jerbi 2007; Khan 1997; Yildirim 2016). In all studies, participants were healthy pregnant women expected to give birth vaginally. Four studies included only women classified as being at low risk of bleeding or its effects (Begley 1990; Rogers 1998; Thilaganathan 1993; Yildirim 2016), and four (Jangsten 2011; Jerbi 2007; Khan 1997; Prendiville 1988) included women irrespective of their risk of bleeding.
Studies were conducted from January 1986 to January 1987 (Prendiville 1988); from October 1987 to October 1988 (Begley 1990); from January 1988 to February 1990 (Thilaganathan 1993); June 1993 to December 1995 (Rogers 1998); January to June 1995 (Khan 1997); February to March 2005 (Jerbi 2007); November 2006 to April 2008 (Jangsten 2011); and “in 2010” (Yildirim 2016). Funding sources were; the Maternity and Child Division at the World Health Organization, Geneva, and support for the National Perinatal Epidemiology Unit from the DHSS (Prendiville 1988); the Research and Development Trust of the Coombe Hospital (Begley 1990); the Public Health and Operational Research Committee of the Anglia and Oxford Regional Health Authority, and support for the National Perinatal Epidemiology Unit from the DHSS (Rogers 1998); Research and Development Board in Göteborg and Bohuslän Baby Bag and the SU foundation (Jangsten 2011); and Kanuni Sultan Suleyman Education and Research Hospital (Yildirim 2016). Three studies gave no information on funding (Jerbi 2007; Khan 1997; Thilaganathan 1993). Only two studies gave any declarations of interest (Jangsten 2011; Yildirim 2016), both stating that there were none. We noted considerable differences in the protocols for both active and expectant management in the various studies (Table 2).
| Study | Active management protocol | Expectant management protocol | Active management used | Expectant management used |
|
|
|
|
| |
|
|
|
|
| |
|
|
|
|
| |
|
|
| No information | No information | |
| BP: blood pressure; CCT: controlled cord traction; IM: intramuscular; IV: intravenous | ||||
Interventions in the ‘active’ management groups
The studies used various uterotonic regimens. These were intravenous (IV) ergometrine 0.5 mg (Begley 1990), intramuscular (IM) syntometrine (5 units oxytocin + 0.5 mg ergometrine; Thilaganathan 1993), IM syntometrine (5 units oxytocin + 0.5 mg ergometrine) or IM 10 units oxytocin if the woman had raised blood pressure (Prendiville 1988; Rogers 1998), IM 10 units oxytocin for all women (Khan 1997; Yildirim 2016), IV oxytocin 5 units (Jerbi 2007) and IV oxytocin 10 units (Jangsten 2011). The descriptions of the timing of administration of uterotonic agent also varied and included, “at the delivery of the anterior shoulder”, “as soon as possible after birth of anterior shoulder”, “immediately after the birth of the anterior shoulder” (which in practice probably equates to the same time), “immediately following birth”, “as soon as baby is born” (which is, in practice, very similar in timing to the preceding descriptions, perhaps 10 to 20 seconds later), "within the first minute after delivery" and "within 2 minutes of birth".
All studies stated that the cord was clamped and cut either within 30 seconds or “immediately” or "early", which in practice is likely to be approximately similar timing. All studies attempted controlled cord traction once the uterus was contracted. Two studies included maternal effort as an option (Jangsten 2011; Rogers 1998), and one included fundal pressure (Jerbi 2007).
Protocols in the ‘expectant’ management groups
In all studies, no uterotonic was to be given routinely prior to delivery of the placenta. However, in one study, an IV infusion of oxytocin 10 units in 500 mL normal saline was given slowly to all women following delivery of the placenta (Khan 1997). One study administered 2 mL of placebo (saline solution) intravenously within two minutes (Jangsten 2011). Practice varied widely as to how many women did, in fact, receive a uterotonic, either prophylactically: 0% (Begley 1990), 2.5% (Rogers 1998), and 20% (Jangsten 2011; Prendiville 1988), and/or as a treatment 9% (Yildirim 2016), 14% (Begley 1990), 21% (Rogers 1998), 30% (Prendiville 1988), and 38% (Jangsten 2011), with no information given in the other three studies.
In four studies, clinicians were asked to try not to cut or clamp the cord until after pulsation ceased (Begley 1990; Prendiville 1988; Rogers 1998; Thilaganathan 1993), although this was achieved in only 42% to 70% of participants. In one study the cord was clamped after "cord pulsation had slowed down " (Yildirim 2016). In three studies, the cord was to be clamped and cut after birth of the baby (Jangsten 2011; Jerbi 2007; Khan 1997). Maternal effort was to be used in six studies (Begley 1990; Jangsten 2011; Prendiville 1988; Rogers 1998; Thilaganathan 1993, Yildirim 2016), with the option in some of gentle controlled cord traction once the placenta had separated (Begley 1990), or assisting the placenta out once it was felt in the vagina (Thilaganathan 1993). Maternal effort was used by 32% to 88% of participants, across the six studies. One study used controlled cord traction with gentle fundal pressure (Jerbi 2007), and another used uterine massage after placental delivery (Jangsten 2011).
Given the differences in uterotonics used in the active groups and the wide variation in the proportion of women in expectant management groups who actually received a uterotonic, it was decided to use a random‐effects model due to the degree of clinical heterogeneity.
Excluded studies
We excluded 10 studies (Abdel‐Aleem 2010; Deneux‐Tharaux 2013; Gulmezoglu 2012; Hoffman 2006; Kashanian 2010; Magann 2006; Muller 1996; Ramirez 2001; Vasegh 2005Neri‐Mejia 2016 (see Characteristics of excluded studies)). One study was only available as a conference abstract with no information on the number of women randomised to each group, and the authors of the previous version of the review had been unable to obtain further information from the study authors (Muller 1996). Although we were able to contact one of the authors, we obtained no further useful information. One study assessed the timing for manual removal of the placenta, so did not fit the criteria for inclusion (Magann 2006). We excluded the third study because of the high number of women excluded after randomisation (48%) (Kashanian 2010). We excluded the fourth study (Hoffman 2006), due to concerns regarding the number of women withdrawn, after randomisation, due to caesarean section. Only a conference abstract was available, but we obtained further information on methodology from the authors. We excluded the fifth study due to insufficient information on the numbers included in each of the three arms, and the method of management for the expectant arm (Ramirez 2001). We excluded Vasegh 2005 due to insufficient information in the published study and inability to elicit a response from the authors. One study (Neri‐Mejia 2016), evaluated three different types of oxytocin administration (IM, IV and infusion) and two studies that looked at active management with or without controlled cord traction (Deneux‐Tharaux 2013; Gulmezoglu 2012), were excluded as we deemed them more appropriate for inclusion in the Cochrane Review on controlled cord traction (Hofmeyr 2015).
Risk of bias in included studies
Other than for the medication, it is not possible to blind personnel and participants to active or expectant management of the third stage. None of the studies used a placebo, and so we assessed all studies as high risk of bias for blinding. Of the eight studies included, we considered three studies as having low risk of bias in the main aspects of sequence generation, allocation concealment and completeness of data collection (Begley 1990; Jangsten 2011; Rogers 1998), these being our criteria for overall quality for sensitivity analyses. We assessed one study as having low risk of bias in sequence generation and allocation concealment, and high risk of bias for lack of blinding and other biases (Prendiville 1988). We considered one study at high risk of bias for completeness of data collection, lack of blinding and other biases and 'unclear' for allocation concealment and selective reporting (Thilaganathan 1993), and assessed one study as unclear on five of the assessment criteria (Khan 1997). We assessed one study as unclear for sequence generation and blinding of outcome assessment, at high risk of bias for allocation concealment, blinding of participants, selective reporting and other biases, but acceptable for completeness of data (Jerbi 2007), and the final study was unclear on four of the assessment criteria, at high risk of bias for blinding of participants but had a low risk of bias for sequence generation and completeness of data collection (Yildirim 2016). See Figure 2 and Figure 3 for a summary of risk of bias assessments.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Six studies used adequate sequence generation using random‐number tables or computer random‐number generators (Begley 1990; Jangsten 2011; Prendiville 1988; Rogers 1998; Thilaganathan 1993; Yildirim 2016) and in two the method was unclear (Jerbi 2007; Khan 1997). We judged allocation concealment as low risk of bias in four studies (Begley 1990; Jangsten 2011; Prendiville 1988; Rogers 1998), and as unclear risk in three (Khan 1997; Thilaganathan 1993; Yildirim 2016). One study did not conceal allocation and so we assessed it as high risk of bias (Jerbi 2007).
Blinding
Blinding was not possible when assessing the management of third stage of labour, for either women or clinicians (Characteristics of included studies). The assessment of many outcomes, particularly blood loss, could, therefore, have been unconsciously affected by people's beliefs. Having chosen maternal Hb less than 9 g/dL as a hard outcome relating to blood loss at the protocol stage, we have now also included the mean postnatal Hb values to help in understanding the blood loss estimations. Haemoglobin assessment would usually be performed by a technician who would be blinded to the study allocation.
Begley 1990 and Jangsten 2011, the Dublin and Swedish studies respectively, measured blood loss, but all the other studies estimated it, and are therefore open to subjective inaccuracies, which should, however, have been the same across both groups; in addition, both blood loss estimation and measurement were open to bias. For certain outcomes such as Hb concentration, which could be measured by a blinded outcome assessor, we attempted to assess how such blinding had occurred. In practice, we found that almost all studies did not mention how they blinded such assessors.
Incomplete outcome data
Five studies presented complete outcome data (Begley 1990; Jangsten 2011; Jerbi 2007; Rogers 1998; Yildirim 2016), with acceptable levels of attrition except for some follow‐up measures, such as postnatal Hb levels. However, one of these studies excluded women post randomisation (2.2%) who had a postpartum haemorrhage (PPH) due to deep vaginal lacerations and so we assessed it as being at unclear risk of bias (Yildirim 2016). We considered one study at high risk of bias for complete data in that it was not clear how many women were randomised, and an unknown number of women were withdrawn following randomisation, due to caesarean section, operative delivery and cervical tears (Thilaganathan 1993). One study had high levels of missing data for some outcomes, for example, 19% of Hb results missing in the active arm and 18% in the expectant, but for other outcomes data were more complete and so we assessed this study as being at unclear risk of bias (Prendiville 1988). In the remaining study, it was also unclear how many data were missing (Khan 1997). In all three of these studies (Khan 1997; Prendiville 1988; Thilaganathan 1993), and in the study that excluded women with deep vaginal lacerations (Yildirim 2016), the denominator used was the number given by study authors as taking part in the study after withdrawals had been made.
Selective reporting
We did not assess any studies as free of selective reporting bias. We categorised five as 'unclear' (Begley 1990; Jangsten 2011; Khan 1997; Thilaganathan 1993; Yildirim 2016), as it was not apparent from the published papers that they had reported all outcomes, and we were unable to check study protocols. We judged three studies as high risk of reporting bias due to some outcomes being reported which were not listed in the methods section (Jerbi 2007; Prendiville 1988; Rogers 1998).
Other potential sources of bias
We judged one study as free of other apparent sources of bias (Begley 1990). One of the remaining studies (Prendiville 1988), included women at increased risk of PPH (high parity, all age groups, previous PPH, epidural, long labour, operative delivery). This was also a problem with another study (Khan 1997). Women at increased risk of PPH will have a higher blood loss, by definition, using expectant management; clinicians experiencing this may respond by anxiety in subsequent births, even of low‐risk women, which may result in higher intervention (mixed management) rates. In Prendiville 1988, 50% of the expectant management group received an oxytocic, a proportion of intervention incompatible with the philosophy of expectant management. In one study, although 11,000 women were available, of whom at least half would usually be considered potentially eligible, only 1802 were entered into the study (Jangsten 2011). The majority were excluded due to "excessive workload". This has the potential to have biased the study, as midwives would have had the choice of not asking the women to participate and may unconsciously have not offered participation to some women who they felt were not suitable for expectant management. Jerbi 2007 reported that women were allocated to the two groups after placental delivery, yet they described the active management group as having had oxytocin with the anterior shoulder. One other study had no power calculation, did not use a null hypothesis, and the study groups were quite different sizes (103 and 90). In addition, they described the variables age, birthweight and parity as equal between the groups but did not give any details (Thilaganathan 1993).
Midwives in all studies, (except Yildirim 2016), were more used to using active than expectant management, which is likely to have had an influence on results in the expectant arm. This influence may have been that they a) reverted to a type of active management, potentially reducing blood loss and narrowing the difference between study arms in terms of blood loss outcomes or b) used mixed management, which, from the data, was more likely to increase blood loss or c) would have conducted a type of expectant management that was not ideal and resulted in increased blood loss in the expectant arm. Rogers 1998 administered a questionnaire to 92 of the 153 midwives prior to the study commencement, which showed that 84% felt "very confident" of active management, whilst only 41% were "very confident" of expectant management. Similarly, Prendiville 1988 states that, before the study commenced, the midwives were trained in the use of expectant management. Only six (13%), however, said that they were very confident in using expectant management before the study started and 22 (46%) afterwards. In addition, of 49 midwives responding to a questionnaire regarding this study, 30 (61%) had never managed a third stage expectantly. Among the remaining 19, only one had practised expectant management as defined in the report (Harding 1989). In Begley 1990, the PPH rate in the expectant arm fell during the study from 21% in the pilot study and 12% over the first four months, to 7% in the last six months, as midwives developed their skill (Begley 1990). In contrast to training in the use of expectant management, additional information provided by the lead author of one study (Yildirim 2016), noted that they had to train practitioners for "the active management protocol (especially for controlled cord traction)". The other studies did not provide any information on skill levels, nor on whether practitioners had training in both expectant and active management of third stage of labour.
Finally, Prendiville 1988 changed the protocol after 425 births, but included all births in the results, which may have affected the findings.
Effects of interventions
The review includes eight studies involving 8892 women. We used a random‐effects model for pooling data because of clinical heterogeneity seen in the included studies. In the forest plots, for six of the outcomes the "Favours expectant" label is on the left rather than the right. This was dictated by whether we are reporting negative (e.g. PPH) or positive (e.g. breastfeeding) outcomes.
1. Active versus expectant management of third stage of labour: all women (four studies, 4829 women)
This comparison included four studies (Begley 1990; Prendiville 1988; Rogers 1998; Thilaganathan 1993). Three studies included only women at low risk of bleeding (Begley 1990; Rogers 1998; Thilaganathan 1993) and one study included women irrespective of risk of bleeding (Prendiville 1988). We assessed two studies as being of high quality (Begley 1990; Rogers 1998); one raised concerns regarding high risk of bias in terms of midwives' comfort with expectant management, and other possible biases (Prendiville 1988); and we considered one study to have high risk of bias in terms of incomplete outcome data and selective reporting bias (Thilaganathan 1993). We used random‐effects meta‐analyses due to the clinical heterogeneity involved. The random‐effects summary gives an average for 'active' methods versus 'expectant' methods, and it is important to note that the treatment effect found by comparing any two specific techniques may differ from this. For a number of outcomes, there was very little statistical heterogeneity found (Tau² = 0 and I² = 0%), so there appears to be a single common treatment effect for these outcomes. We have assessed the overall quality of the evidence using GRADE (GRADE 2013; summary of findings Table for the main comparison).
Primary outcomes
For women
Compared with expectant management, it is uncertain whether active management reduces the incidence of severe PPH:
-
severe primary PPH, 1000 mL or more at time of birth (average risk ratio (RR) 0.34, 95% confidence interval (CI) 0.14 to 0.87, 3 studies, 4636 women, random‐effects (Tau² = 0.38, Chi² P = 0.08, I² = 60%) very low‐quality evidence; Analysis 1.1).
However, active management may reduce the number of women who are anaemic after birth:
-
maternal Hb less than 9 g/dL at 24 to 72 hours (average RR 0.50, 95% CI 0.30 to 0.83, 2 studies, 1572 women, random‐effects (Tau² = 0.02, Chi² P = 0.31, I² = 3%) low‐quality evidence; Analysis 1.4).
None of the studies reported on the other primary maternal outcomes of very severe primary PPH (≥ 2500 mL), except Begley 1990, who found no instances of such extreme blood loss in either group, or maternal mortality.
For babies
Compared with expectant management, active management may make little or no difference to:
-
admission to neonatal special care or intensive care unit (average RR 0.81, 95% CI 0.60 to 1.11, 2 studies, 3207 infants, random‐effects (Tau² = 0.00, Chi² P = 0.40, I² = 0%) low‐quality evidence; Analysis 1.5);
and it is uncertain whether active management reduces or increases the number of babies with jaundice requiring treatment:
-
neonatal jaundice requiring phototherapy or exchange transfusion (average RR 0.96, 95% CI 0.55 to 1.68, 2 studies, 3142 infants, random‐effects (Tau² = 0.11, Chi² P = 0.09, I² = 66%) very low‐quality evidence; Analysis 1.6).
None of the studies reported on the other primary neonatal outcome of neonatal polycythaemia treated with dilutional exchange transfusion.
It should be noted that the evidence presented on the primary outcomes selected is based on results of a small number of studies with relatively small numbers of participants. The lack of consistent quality of evidence for these outcomes should be borne in mind when considering the overall results (see summary of findings Table for the main comparison).
Secondary outcomes
Compared with expectant management, active management (with high‐quality evidence) reduces:
-
mean maternal blood loss (mean difference (MD) in mL −78.80, 95% CI −95.96 to −61.64, 2 studies, 2941 women, random‐effects (Tau² = 34.93, Chi² P = 0.26, I² = 22%) Analysis 1.13).
Also, active management (with moderate‐quality evidence) probably reduces:
-
primary blood loss 500 mL or more, clinically estimated or measured at birth (average RR 0.34, 95% CI 0.27 to 0.44, 3 studies, 4636 women, random‐effects (Tau² = 0.02, Chi² P = 0.23, I² = 32%) Analysis 1.10);
-
therapeutic uterotonics during the third stage and/or within the first 24 hours (average RR 0.19, 95% CI 0.15 to 0.23, 4 studies, 4829 women, random‐effects (Tau² = 0.00, Chi² P = 0.47, I² = 0%) Analysis 1.18);
-
mean birthweight (MD in g −76.90, 95% CI −108.51 to −45.30, 2 studies, 3207 infants, random‐effects (Tau² = 0.00, Chi² P = 0.58, I² = 0%) Analysis 1.30).
In addition, active management (with low‐quality evidence) may reduce:
-
maternal blood transfusion (average RR 0.35, 95% CI 0.22 to 0.55, 4 studies, 4829 women, random‐effects (Tau² = 0.00, Chi² P = 0.46, I² = 0%) Analysis 1.16).
Compared with expectant management, active management (with low‐quality evidence) may increase:
-
postnatal diastolic blood pressure more than 90 mmHg up to discharge from labour ward (average RR 4.10, 95% CI 1.63 to 10.30, 3 studies, 4636 women, random‐effects (Tau² = 0.32, Chi² P = 0.14, I² = 49%) Analysis 1.21);
-
vomiting from birth of baby to discharge from labour ward (average RR 2.47, 95% CI 1.36 to 4.48, 3 studies, 4636 women, random‐effects (Tau² = 0.14, Chi² P = 0.09, I² = 59%) Analysis 1.22);
-
administration of any analgesia from birth up to discharge from labour ward (RR 2.53, 95% CI 1.34 to 4.78, 1 study, 1429 women; Analysis 1.23);
-
afterpains (RR 2.53, 95% CI 1.34 to 4.78, 1 study, 1429 women; Analysis 1.28);
-
return to hospital as an in‐ or outpatient because of bleeding (outcome not pre‐specified) (average RR 2.21, 95% CI 1.29 to 3.79, 2 studies, 2941 women, random‐effects (Tau² = 0.00, Chi² P = 0.82, I² = 0%) Analysis 1.40);
-
postnatal maternal Hb (outcome not pre‐specified) (MD 0.52, 95% CI 0.44 to 0.60, 3 studies, 4062 women, random‐effects (Tau² = 0.00, Chi² P = 0.66, I² = 0%) Analysis 1.41).
Compared with expectant management, active management (with moderate‐quality evidence) probably makes little or no difference to:
-
exclusive breastfeeding at discharge (RR 1.01, 95% CI 0.96 to 1.07, 1 study, 1695 women; Analysis 1.38).
Also, active management (with low‐quality evidence) may make little or no difference to:
-
mean length of the third stage in minutes (MD −0.30, 95% CI −1.87 to 1.27, 1 study, 1429 women; Analysis 1.19);
-
secondary blood loss/any vaginal bleeding needing treatment after 24 hours and before six weeks (average RR 1.10, 95% CI 0.40 to 2.99, 3 studies, 4636 women, random‐effects (Tau² = 0.67, Chi² P = 0.0005, I² = 87%) Analysis 1.25);
-
surgical evacuation of retained products of conception (average RR 0.74, 95% CI 0.32 to 1.71, 3 studies, 4636 women, random‐effects (Tau² = 0.26, Chi² P = 0.15, I² = 47%) Analysis 1.27).
In addition, we are uncertain if active management (with very low‐quality evidence) improves the incidence of:
-
manual removal of placenta (average RR 1.78, 95% CI 0.57 to 5.56, 4 studies, 4829 women, random‐effects (Tau² = 0.82, Chi² P = 0.01, I² = 73%) Analysis 1.20);
-
Apgar scores less than 7 at five minutes (RR 1.00, 95% CI 0.38 to 2.66, 1 study, 1695 infants; Analysis 1.29).
Authors of the included studies did not assess any of the review's other secondary outcomes.
2. Active versus expectant management of third stage of labour: women at low risk of bleeding (three studies, 3134 women)
This comparison included three studies (Begley 1990; Rogers 1998; Thilaganathan 1993). We considered two studies to be of high methodological quality (Begley 1990; Rogers 1998) and one study to have high risk of bias in terms of incomplete outcome data and selective reporting bias (Thilaganathan 1993). All meta‐analyses used random‐effects meta‐analyses due to the clinical heterogeneity involved. For a number of outcomes, there was very little heterogeneity found (Tau² = 0 and I² = 0%), so there appears to be a single common treatment effect for these outcomes.
Primary outcomes
For women at low risk of PPH: compared with expectant management, it is uncertain whether active management (with very low‐quality evidence) reduces:
-
severe primary PPH, 1000 mL or more at time of birth (average RR 0.31, 95% CI 0.05 to 2.17, 2 studies, 2941 women, random‐effects (Tau² = 1.46, Chi² P = 0.06, I² = 71%) Analysis 2.1);
-
maternal Hb less than 9 g/dL at 24 to 72 hours (RR 0.17, 95% CI 0.02 to 1.47, 1 study, 193 women; Analysis 2.4).
None of the studies reported the other primary outcomes of: very severe primary PPH (≥ 2500 mL) except Begley 1990, who found no instances of such extreme blood loss in either group, or maternal mortality.
Also, active management (with low‐quality evidence) may make little or no difference to:
-
neonatal jaundice requiring phototherapy or exchange transfusion (RR 1.31, 95% CI 0.78 to 2.18, 1 study, 1447 infants; Analysis 2.6).
In addition, it is uncertain if active management (with very low‐quality evidence) makes any difference to:
-
admission to neonatal special care or intensive care unit (RR 1.02, 95% CI 0.55 to 1.88, 1 study, 1512 infants; Analysis 2.5).
None of the studies reported the other primary outcome of neonatal polycythaemia.
Secondary outcomes
For women at low risk of PPH: compared with expectant management, active management (with moderate‐quality evidence) probably reduces:
-
therapeutic uterotonics during the third stage and/or within the first 24 hours (average RR 0.15, 95% CI 0.11 to 0.21, 3 studies, 3134 women, random‐effects (Tau² = 0.00, Chi² P = 0.98, I² = 0%) Analysis 2.18).
Also, active management (with low‐quality evidence) may reduce:
-
primary blood loss 500 mL or more, clinically estimated or measured at time of birth (average RR 0.33, 95% CI 0.20 to 0.56, 2 studies, 2941 women, random‐effects (Tau² = 0.10, Chi² P = 0.10, I² = 63%) Analysis 2.10);
-
mean maternal blood loss (mL) (MD −78.80, 95% CI −95.96 to −61.64, 2 studies, 2941 women, random‐effects (Tau² = 34.93, Chi² P = 0.26, I² = 22%) Analysis 2.13);
-
maternal blood transfusions (average RR 0.30, 95% CI 0.10 to 0.88, 3 studies, 3134 women, random‐effects (Tau² = 0.14, Chi² P = 0.32, I² = 11%) Analysis 2.16);
-
mean birthweight in g (MD −67.00, 95% CI −114.13 to −19.87, 1 study, 1512 infants; Analysis 2.30).
Compared with expectant management, active management (with moderate‐quality evidence) probably increases:
-
postnatal maternal mean Hb (outcome not pre‐specified) (MD in g/dL 0.50, 95% CI 0.41 to 0.59, 2 studies, 2683 women, random‐effects (Tau² = 0.00, Chi² P = 1.00, I² = 0%) Analysis 2.41).
Also, active management (with low‐quality evidence) may increase:
-
postnatal diastolic blood pressure more than 90 mm Hg (average RR 7.00, 95% CI 2.99 to 16.43, 2 studies, 2941 women, random‐effects (Tau² = 0.00, Chi² P = 0.89, I² = 0%) Analysis 2.21);
-
administration of any analgesia between birth of the baby and discharge from labour ward (RR 2.53, 95% CI 1.34 to 4.78, 1 study, 1429 women; Analysis 2.23);
-
afterpains (RR 2.53, 95% CI 1.34 to 4.78, 1 study, 1429 women; Analysis 2.28);
-
return to hospital as an in‐ or outpatient because of bleeding (outcome not pre‐specified) (average RR 2.21, 95% CI 1.29 to 3.79, 2 studies, 2941 women, random‐effects (Tau² = 0.00, Chi² P = 0.82, I² = 0%) Analysis 2.40).
In addition, active management (with moderate‐quality evidence) probably slightly increases:
-
secondary blood loss/any vaginal bleeding needing treatment after 24 hours and before six weeks (average RR 1.78, 95% CI 0.69 to 4.60, 2 studies, 2941 women, random‐effects (Tau² = 0.39, Chi² P = 0.01, I² = 84%) Analysis 2.25).
However, active management (with low‐quality evidence) may make little or no difference to:
-
length of the third stage in minutes (MD −0.30, 95% CI −1.87 to 1.27, 1 study, 1429 women; Analysis 2.19);
-
manual removal of placenta (average RR 3.58, 95% CI 0.42 to 30.61, 3 studies, 3134 women, random‐effects (Tau² = 2.58, Chi² P = 0.02, I² = 75%) Analysis 2.20);
-
postnatal vomiting (average RR 5.63, 95% CI 0.69 to 46.08, 2 studies, 2941 women, random‐effects (Tau² = 1.60, Chi² P = 0.12, I² = 60%) Analysis 2.22);
-
surgical evacuation of retained products of conception (average RR 0.69, 95% CI 0.12 to 3.98, 2 studies, 2941 women, random‐effects (Tau² = 1.17, Chi² P = 0.06, I² = 72%) Analysis 2.27).
Authors of the included studies did not assess any of the review's other secondary outcomes.
3. Active versus mixed management of third stage: all women, early uterotonic, delayed cord clamping, controlled cord traction (no studies)
There were no studies that assessed this comparison.
4. Active versus mixed management of third stage of labour: all women, delayed uterotonic, delayed cord clamping, controlled cord traction (no studies)
There were no studies that assessed this comparison.
5. Active versus mixed management of third stage of labour: all women, delayed uterotonic, delayed cord clamping, no controlled cord traction (one study, 654 women)
This comparison included one study (Yildirim 2016).
Primary outcomes
The study did not report any of the review's primary outcomes: severe primary PPH (≥ 1000 mL time of birth); very severe primary PPH (≥ 2500 mL); maternal mortality; maternal Hb less than 9 g/dL at 24 to 72 hours; admission to neonatal special care or intensive care unit; neonatal jaundice requiring phototherapy or exchange transfusion; neonatal polycythaemia treated with dilutional exchange transfusion. The study authors' own primary outcome was one of this review's secondary outcomes.
Secondary outcomes
Compared with mixed management, active management (with low‐quality evidence) may slightly reduce:
-
mean length of the third stage in minutes (MD −5.15, 95% CI −5.71 to −4.59, 1 study, 654 women; Analysis 5.10);
-
postnatal maternal mean Hb (MD in g/dL 0.69, 95% CI 0.58 to 0.80, 1 study, 654 women; Analysis 5.14).
Also, active management (with low‐quality evidence) ‐ may slightly increase:
-
birthweight in g (MD 68, 95% CI 23.87 to 112.13, 1 study, 654 infants; Analysis 5.13).
Compared with mixed management, it is uncertain if active management (with very low‐quality evidence) makes any difference, improves, or reduces:
-
maternal blood transfusions (RR 0.75, 95% CI 0.17, 3.32, 1 study, 654 women; Analysis 5.8);
-
therapeutic uterotonics during the third stage and/or within the first 24 hours (RR 0.90, 95% CI 0.55 to 1.48, 1 study, 654 women; Analysis 5.9);
-
manual removal of placenta (RR 0.67, 95% CI 0.11 to 3.96, 1 study, 654 women; Analysis 5.11);
-
surgical evacuation of retained products of conception (RR 7.00, 95% CI 0.36 to 134.98, 1 study, 654 women; Analysis 5.12).
The authors of this study did not assess any of the review's other secondary outcomes.
6. Expectant versus mixed management of third stage of labour: all women, early uterotonic, delayed cord clamping, controlled cord traction (no studies)
There were no studies that assessed this comparison.
7. Expectant versus mixed management of third stage of labour: all women, delayed uterotonic, delayed cord clamping, controlled cord traction (no studies)
There were no studies that assessed this comparison.
8. Expectant versus mixed management of third stage of labour: all women, delayed uterotonic, delayed cord clamping, no controlled cord traction (no studies)
There were no studies that assessed this comparison.
9. Active versus mixed management of third stage of labour: all women, immediate cord clamping, no controlled cord traction, uterotonic after placental delivery (one study, 1648 women; comparison not pre‐specified)
This comparison included one study with 1648 women (Khan 1997). We had not pre‐specified this comparison.
Primary outcomes
Compared with mixed management, it is uncertain whether active management (with very low‐quality evidence) reduces:
-
severe primary PPH, blood loss1000 mL or more at time of birth (RR 0.23, 95% CI 0.09 to 0.55, 1 study, 1648 women; Analysis 9.1).
The study did not report the other primary outcomes of: very severe primary PPH (≥ 2500 mL); maternal Hb less than 9 g/dL at 24 to 72 hours; maternal mortality, neonatal jaundice requiring phototherapy or exchange transfusion; or neonatal polycythaemia treated with dilutional exchange transfusion.
Secondary outcomes
Compared with mixed management, it is uncertain whether active management (wit−h very low‐quality evidence) reduces:
-
primary blood loss of 500 mL or more, clinically estimated or measured at time of birth (RR 0.53, 95% CI 0.38 to 0.74, 1 study, 1648 women; Analysis 9.10);
-
therapeutic uterotonics during the third stage and/or within the first 24 hours (RR 0.45, 95% CI 0.26 to 0.77, 1 study, 1648 women; Analysis 9.18);
-
length of the third stage in minutes (MD −10.00, 95% CI −10.24 to −9.76, 1 study, 1648 women; Analysis 9.19).
Also, it is uncertain if active management (with very low‐quality evidence) reduces or improves:
-
maternal blood transfusions (RR 0.25, 95% CI 0.03 to 2.22, 1 study, 1648 women; Analysis 9.16);
-
clinical signs of severe blood loss (RR 0.25, 95% CI 0.05 to 1.17, 1 study, 1648 women; Analysis 9.17).
Authors of the included study did not assess any of the review's other secondary outcomes.
10. Active versus mixed management of third stage of labour: all women, no routine uterotonic, immediate cord clamping, no controlled cord traction (one study, 1631 women, comparison not pre‐specified)
This comparison included one study (Jangsten 2011). We judged this study to be at low risk of bias for sequence generation, allocation concealment and incomplete outcome data, unclear for selective reporting bias, but high risk of bias for other biases (see Characteristics of included studies).
Primary outcomes
Compared with mixed management, it is uncertain if active management (with very low‐quality evidence) reduces:
-
severe primary PPH at time of birth of 1000 mL or more (RR 0.78, 95% CI 0.48 to 1.24, 1 study, 1621 women; Analysis 10.1).
Also, active management (with very low‐quality evidence) may slightly improve:
-
maternal Hb less than 9 g/dL at 24 to 72 hours (RR 1.23, 95% CI 0.75 to 2.01, 1 study, 1631 women; Analysis 10.4).
The study did not report the other primary outcomes of: very severe primary PPH (≥ 2500 mL); maternal mortality; neonatal jaundice requiring phototherapy or exchange transfusion; neonatal polycythaemia treated with dilutional exchange transfusion.
Secondary outcomes
Compared with mixed management, active management (with moderate‐quality evidence) probably reduces:
-
therapeutic uterotonics during the third stage and/or within the first 24 hours (RR 0.39, 95% CI 0.33 to 0.48, 1 study, 1631 women; Analysis 10.18);
-
severe primary PPH at time of birth and up to two hours after, clinically estimated or measured blood loss of 1000 mL or more (RR 0.60, 95% CI 0.47 to 0.78, 1 study, 1621 women, Analysis 10.44); we had not pre‐specified this outcome);
-
mean maternal blood loss after delivery of the placenta and up to two hours (outcome not pre‐specified) (MD in mL −49.00, 95% CI −75.52 to −22.48, 1 study, 1621 women; Analysis 10.45).
Also, active management (with low‐quality evidence) may reduce:
-
primary blood loss of 500 mL or more at time of birth, clinically estimated or measured at birth (RR 0.51, 95% CI 0.40 to 0.66, 1 study, 1621 women; Analysis 10.10);
-
mean maternal blood loss at time of birth (MD in mL −94.00, 95% CI −126.57 to −61.43, 1 study, 1621 women; Analysis 10.13);
-
mean length of third stage in minutes (MD −1.60, 95% CI −3.08 to −0.12; Analysis 10.19);
-
severe primary PPH after delivery of placenta and up to two hours, clinically estimated or measured blood loss of 1000 mL or more (RR 0.54, 95% CI 0.39 to 0.74, 1 study, 1621 women; Analysis 10.43); we had not pre‐specified this outcome.
Compared with mixed management, active management (with low‐quality evidence) may increase:
-
postnatal maternal mean Hb (MD in g/dL 0.28, 95% CI 0.14 to 0.42, 1 study, 1631 women; Analysis 10.42); we had not pre‐specified this outcome.
Compared with mixed management, active management (with low‐quality evidence) may make little or no difference to:
-
mean birthweight (MD in g 15.00, 95% CI ‐28.88 to 58.88; Analysis 10.31).
Also, it is uncertain whether active management (with very low‐quality evidence) improves or reduces:
-
maternal blood transfusion (RR 0.79, 95% CI 0.43 to 1.46; Analysis 10.16);
-
manual removal of placenta (RR 1.25, 95% CI 0.71 to 2.21; Analysis 10.20).
The study did not assess any of the review's other secondary outcomes, including, afterpains ‐ abdominal pain associated with the contracting uterus in the postpartum period. However, we assessed two similar, non‐prespecified outcomes (Jangsten 2011), and active management (with low‐quality evidence) may reduce:
-
afterpains at two hours after birth (RR −2.80, 95% CI −4.62 to −0.98, 1 study, 1425 women; Analysis 10.28);
-
afterpains the day after birth (RR −3.00, 95% CI −5.33 to −0.67, 1 study, 1336 women; Analysis 10.29).
11. Active versus mixed management of third stage of labour: all women, no routine uterotonic, immediate cord clamping, controlled cord traction (one study, 130 women, comparison not pre‐specified)
This comparison included one study (Jerbi 2007).
Primary outcomes
Compared with mixed management, it is uncertain whether active management (with very low‐quality evidence) reduces:
-
maternal Hb less than 9 g/dL at 24 to 72 hours (RR 0.80, 95% CI 0.34 to 1.90; Analysis 11.4).
The study did not report on the other primary outcomes of: severe primary PPH (≥ 1000 mL time of birth); very severe primary PPH (≥ 2500 mL); maternal mortality; neonatal jaundice requiring phototherapy or exchange transfusion; neonatal polycythaemia treated with dilutional exchange transfusion.
Secondary outcomes
Compared with mixed management, it is uncertain if active management (with very low‐quality evidence) reduces:
-
mean length of the third stage in minutes (MD −8.12 95% CI −9.72 to −6.52; Analysis 11.19).
Also, it is uncertain if active management (with very low quality evidence) makes any difference to the incidence of:
-
manual removal of placenta (RR 1.00, 95% CI 0.06 to 15.65; Analysis 11.20).
The study did not assess any of the review's other secondary outcomes.
Sensitivity analysis
We undertook sensitivity analyses including only the four studies with adequate sequence generation, allocation concealment and complete outcome reporting (Begley 1990; Jangsten 2011; Prendiville 1988; Rogers 1998). Removing the studies at high risk of bias did not change the overall findings.
Discussion
This review includes eight studies conducted in hospital settings in five countries involving 8892 women. None of the included studies reported any maternal deaths, nor any very severe (greater than 2500 mL) postpartum haemorrhages (PPH), and also no neonatal mortality. It should be noted that the random‐effects summaries presented are the average effects found for 'active' versus 'expectant' management. Thus, it may not necessarily be true that all methods of active management will have the reported size of advantage in terms of PPH, or other outcomes, over all methods of expectant management.
Summary of main results
Active versus expectant management of the third stage of labour in women, irrespective of their risk of bleeding
It is uncertain whether active management in hospitals in higher‐income settings leads to a reduction in severe primary PPH of 1000 mL or more, and it may reduce the number of women with maternal Hb less than 9 g/dL at 24 to 72 hours postnatal. Indices of maternal blood loss may be improved; for example, mean Hb may be higher by 0.5 g/dL in the active group. However, the average difference may not be clinically important, as routine blood donation reduces Hb levels by approximately 0.6 g/dL (Burnley 2006), without ill effects, and postnatal women undergo a diuresis postnatally that reverses the haemodilution of pregnancy, thus increasing their Hb levels within a few days after birth (Hytten 2001; Taylor 1981). The more clinically important effects are the possible reduction in severe PPH rate, need for transfusion and uterotonic therapy, which suggests (with very low‐quality) its effectiveness in lessening the severe bleeding that can prove life‐threatening if left untreated.
However, active management (with moderate‐quality evidence) probably reduces average birthweight for the baby (possibly due to decreased placental transfusion at birth arising from the early cord clamping component, Farrar 2009a), and (with low‐quality evidence) may increase the incidence of maternal postpartum diastolic blood pressure greater than 90 mmHg (possibly due to the use of ergometrine‐based uterotonics), afterpains, need for postpartum analgesia in the labour ward, and women having to return to hospital because of bleeding. Using data from only the high‐quality studies showed similar results.
The main findings may also be presented using the 'number needed to treat for an additional harmful outcome'. There would be one fewer severe PPH for every 66 women who had active management (95% CI 44 to 127) and one woman fewer with a postnatal Hb under 9 g/dL for every 28 women who had active management (95% CI 17 to 73). Conversely, there would be one more woman with a diastolic blood pressure greater than 90 mmHg for every 52 women who had active management (95% CI 38 to 83) and one more woman who had to return to hospital because of bleeding for every 65 women who had active management (95% CI 39 to 192).
Although this analysis considers women irrespective of risk of bleeding, the studies mainly included women at low risk of bleeding, with just one out of the four studies specifically including women of any risk. There were no specific data on women considered to be at high risk of bleeding.
Overall, active management may reduce the risk of severe bleeding, and it would be important to investigate if this benefit arose from the uterotonic component of the active management alone. The negative effects of active management appear, in the main, to be due either to 1) the administration of a specific uterotonic (e.g. hypertension due to ergometrine‐containing preparations and hypotension due to intravenous oxytocin boluses (Lewis 2007)), or 2) possibly to controlled cord traction leading to retained shreds of membrane or placenta, thus causing the increased incidence of return to hospital due to bleeding, or 3) early cord clamping leading to a 20% reduction in the baby's blood volume. Different uterotonics will have differing effects, and clinicians will need to assess the optimum one to use according to the circumstances. Recent international guidelines have turned to intramuscular oxytocin as a uterotonic that provides effective prophylaxis but without the associated side effects (ICM‐FIGO 2003; NICE 2014; WHO 2012) and a recent network meta‐analysis has suggested that the most effective drugs for preventing PPH of 500 mL of more could be ergometrine and oxytocin, carbetocin, or misoprostol combined with oxytocin (Gallos 2018). However, most of these studies group together intramuscular and intravenous oxytocin, and a recent randomised study suggests that the intravenous route may be more effective (Adnan 2018). In this Cochrane Review, of the eight studies, three administered the drug intravenously and five intramuscularly. Thus some of the oxytocics may have been less effective and so reduced the overall efficacy of the prophylaxis. The possible increased incidence of women in the active management group having to return to hospital due to bleeding is of concern, as such bleeding takes place away from immediate access to medical assistance. This would, again, be of greater significance for women in low‐income countries.
The probable reduction in the average birthweight of babies following active management is possibly due to a reduction in placental transfusion following early cord clamping (McDonald 2013; Rabe 2012; RCOG 2009). The evidence from the studies we identified is that the average volume of transfused blood was 77 mL (45 to 108 mL) based on differences in the birthweight between the groups. This estimate is consistent with historical data (Yao 1974), and also with more recent data (Farrar 2009a). Farrar’s small study (n = 26) weighing babies at birth on accurate scales to calculate placental transfusion showed that 79 mL (interquartile range 50 to 163 mL) of extra blood was transfused to babies following vaginal births and 84 mL (interquartile range 59 to 165 mL) following caesarean births. Placental transfusion for most of these babies was completed by about three minutes after birth, but transfusion continued for up to five minutes for some babies (Farrar 2009a). As all babies in this study breathed normally at birth, further studies are necessary to ascertain whether or not the cord remains pulsating for longer if the baby has not commenced respiration.
With expectant management, term infants receive about 80 mL more blood from placental transfusion than with active management, with its early cord clamping ‐ thus adding about 20% more to the infant's blood volume (Werner 2005). This may be associated with a lower incidence of anaemia in infancy (Cernadas 2006; Chaparro 2006; McDonald 2013; Van Rheenan 2007). It is possible that anaemia in early infancy may have adverse effects for the infant's longer‐term growth and development, particularly for infants born in low‐income countries. Although it is also plausible that placental transfusion with expectant management may increase the risk of neonatal jaundice requiring phototherapy (McDonald 2013), there was no evidence for this in the two studies that assessed this outcome. Finally, it needs to be considered that in the context of the administration of a powerful uterotonic, early cord clamping may protect the baby by preventing a sudden increase of blood volume into the transitional circulation, that might disrupt physiological processes such as duct closure, lung fluid reabsorption and cerebral haemodynamic autoregulation. This may be particularly important to infants who are slow to breathe (Mercer 2008). This problem can be avoided by giving the uterotonic drug immediately following the deferred cord clamping. The included studies did not report on these specific neonatal adverse outcomes, but this review did not find evidence that admission rates to special care baby units (SCBU) or neonatal intensive care units (NICU) were affected by the types of third‐stage management included (average RR 0.81, 95% CI 0.60 to 1.11, 2 studies, 3207 babies).
In the three studies that documented both severe PPH (≥ 1000 mL) and number of blood transfusions (Begley 1990; Prendiville 1988; Rogers 1998), it is noted that a total of 78 out of the 4636 women had a severe PPH, whereas 94 received a blood transfusion, perhaps indicating an over‐use of this treatment in a healthy population, under‐estimation of blood loss, or undetected low antenatal haemoglobins in some women. Given that a woman’s body is well prepared for normal blood loss at birth by the haemodilution of pregnancy (Mims 2005), and that 600 mL to 750 mL of diluted blood is equivalent to a routine blood donation, it is possible that the impact of blood losses less than 750 mL are not severe in normal, healthy women, but this needs investigation. In addition, the decrease in plasma volume in the early days after birth increases postnatal Hb concentration in a reversal of haemodilution (Hytten 2001; Mims 2005; Taylor 1981).
Active versus expectant management of the third stage of labour in women at low risk of bleeding
In hospitals in higher‐income settings, we found that it was uncertain whether active management (with very low‐quality evidence) reduced maternal primary PPH greater than 1000 mL, although the number of women was insufficient to assess this outcome with confidence (two studies, 2941 women) and further studies would be needed to study this association.
One small study (n = 193) compared the number of women with Hb levels less than 9 g/dL postnatally (Thilaganathan 1993) but the high risk of bias identified means that we cannot rely on the findings. None of the studies assessed Apgar scores less than 7 at five minutes. Other indices of maternal blood loss (with low‐quality evidence) may be reduced with the use of active management in this population. Active management again resulted (with moderate‐quality evidence) in a probable lower birthweight (possibly due to reduced placental transfusion), and (with low‐quality evidence) might result in an increase in the incidence of postpartum diastolic blood pressure greater than 90 mmHg, afterpains, need for postpartum analgesia in the labour ward, and having to return to hospital as an in‐ or outpatient because of bleeding.
Mixed managements around the timing of cord clamping in combination with the timing of uterotonic drug
Active versus mixed management of third stage of labour: all women, delayed prophylactic uterotonic administration, delayed cord clamping, no controlled cord traction (one study, 654 women)
The one study included (Yildirim 2016), was of low quality (unclear on four of the assessment criteria, and at high risk of bias for lack of blinding). The women were all at low risk of bleeding. The results indicated that, compared with mixed management, active management (with low‐quality evidence) may slightly reduce mean length of the third stage, and slightly increase birthweight. It is uncertain if active management (with very low‐quality evidence) makes any difference, improves, or reduces rates of maternal blood transfusions, therapeutic uterotonics during the third stage or within the first 24 hours, manual removal of placenta, or surgical evacuation of retained products of conception.
Active versus mixed management of the third stage of labour: all women, immediate cord clamping, no controlled cord traction and uterotonic after placental delivery (one study, 1648 women, comparison not pre‐specified)
The one study (Khan 1997), assessing this comparison was of uncertain quality (sequence generation was unclear). The results indicated that it is uncertain whether active management (with very low‐quality evidence) showed a reduction in severe primary PPH. It is also uncertain whether active management (with very low‐quality evidence) showed a reduction in the rate of blood loss greater than 500 mL, use of therapeutic uterotonics postpartum and length of the third stage, and it is uncertain if active management (with very low‐quality evidence) reduces or improves the number of blood transfusions (Figure 2).
Active versus mixed management of third stage of labour: all women, no routine uterotonic, immediate cord clamping, no controlled cord traction (one study, 1631 women, comparison not pre‐specified)
The one study included was of high quality (Jangsten 2011). Compared with mixed management, it is uncertain if active management (with very low‐quality evidence) reduces severe primary PPH or rates of maternal Hb less than 9 g/dL at 24 to 72 hours. Active management (with low‐quality evidence) may reduce the rate of blood loss greater than 500 mL and mean length of the third stage, may make little or no difference to mean birthweight, and (with moderate‐quality evidence) probably reduces the use of therapeutic uterotonics during the third stage. It is uncertain whether active management (with very low‐quality evidence) improves or reduces the number of maternal blood transfusions or rate of manual removal of placenta.
Active versus mixed management of third stage of labour: all women, no routine uterotonic, immediate cord clamping, controlled cord traction (one study, 130 women, comparison not pre‐specified)
The one study included was of moderate quality (Jerbi 2007). The results indicated that it is uncertain whether active management (with very low‐quality evidence) reduces maternal Hb less than 9 g/dL at 24 to 72 hours, compared to mixed management. It is uncertain if active management (with very low‐quality evidence) showed a reduction in mean length of the third stage, or makes any difference to the incidence of rates of manual removal of placenta.
Overall completeness and applicability of evidence
Four studies compared active versus expectant management of the third stage of labour and four compared active versus mixed management. All were conducted in hospitals, seven in higher‐income settings, and one in a lower‐income setting (n = 130). Four studies involved women at low risk of bleeding and four included women irrespective of their risk of bleeding. Given these factors, the results of the meta‐analysis can only be applied to care given in higher‐income settings. As only four studies (two of uncertain quality), compared active versus mixed management, and all mixed managements differed, we are unable to draw firm conclusions on any apparent differences between these two managements. Also, for many of the outcomes there is heterogeneity in the treatment effects, so there is no information as to the specific factors that might affect the difference between active and expectant management.
Quality of the evidence
The evidence presented on the primary outcomes selected is based on results of a small number of studies with relatively small numbers of participants. The lack of consistent high‐quality evidence for these outcomes should be borne in mind when considering the overall results (see summary of findings Table for the main comparison).
We assessed the methodological quality of the included studies as ‘high quality’ in terms of sequence generation, allocation concealment and complete outcome data for three studies (Begley 1990; Jangsten 2011; Rogers 1998). We undertook sensitivity analysis by study quality to assess for any substantial difference in the main results. This made little difference to the overall findings except to indicate that there was no high‐quality evidence for the results of comparisons between active management and mixed management of the third stage of labour.
In all studies, there is the problem of assessment of blood loss by clinicians where no blinding is possible. However, studies used other indices of blood loss, such as postnatal Hb, which may have been assessed by technicians blinded to treatment allocation. For this reason, we included an outcome that had not been pre‐specified, mean postnatal Hb, in addition to comparing the number of women with Hb levels less than 9 g/dL at 24 to 72 hours, which not all studies had measured.
Adherence to intervention protocols and, in particular, to the management proposed for the two study arms was mixed (Table 2). In the three high‐quality studies (Begley 1990; Jangsten 2011; Rogers 1998), the majority of women in the active management arm (93% to 100%) received a uterotonic as directed. In the expectant management arm, however, practice varied widely, with 86% receiving "no uterotonic" in one study (Begley 1990), 76.5% in another (Rogers 1998), and 62% in the third (Jangsten 2011). Only 50% of women in the expectant management arm in one study (Prendiville 1988), received "no uterotonic", with no information given in the other three studies. The intervention protocol for the expectant arm of Prendiville 1988 did allow for administration of a uterotonic if necessary, as it stated, “Try not to give a uterotonic”; however, the actual proportion that received the drug appears incompatible with a philosophy of expectant management. In addition, the fact that the administration of the same uterotonic that constituted the main treatment in active management to half of the 'expectant' management group as well, does raise questions as to the usefulness of the findings. The resulting 'mixed' management may also increase levels of blood loss and other complications, as changing the study protocol after the first 425 births to exclude participants when mixed management had to be used (due to cutting the cord early because of nuchal cord, concerns about meconium or baby needing resuscitation) resulted in a decrease in PPH rate.
In addition, Prendiville 1988 included women at increased risk of bleeding. The total numbers involved are not clear, but 84 (5%) had previous third‐stage problems, 212 (13%) had an epidural in labour, and 230 (14%) had assisted births. As these women are likely to have a higher blood loss when expectant management is used, clinicians experiencing this may respond by anxiety in subsequent births using expectant management, even for women at low risk of bleeding, and be more likely to give a uterotonic early; this may have increased the intervention or 'mixed management' rates in women allocated to expectant management in this study (30% received uterotonic for treatment, and 20% prophylactically), and would also have decreased the opportunity for those midwives to keep up their skill level in expectant management.
A second study, comparing active with mixed management, also included women at increased risk of bleeding (Jangsten 2011), with similar possible results as above: 7% (n = 131) had a caesarean section, 714 (40%) had an epidural in labour, and 148 (8%) had a ventouse birth.
The skill of the midwives in both forms of care in all studies is of interest. The midwives in Rogers 1998 were said to be “similarly confident” in active and expectant management. However, the questionnaire administered to 92 of the 153 midwives prior to the study commencement showed that, whereas 84% felt “very confident” of active management, only 41% were “very confident” of expectant management. Similarly, Prendiville 1988 states that, before the study commenced, the researchers sought the advice of midwives in the UK who were “known to practise physiological management” and then used this advice to train the midwives. Only six (13%) of the midwives in this study, however, said that they were very confident of physiological management before the study started and 22 (46%) afterwards. Harding 1989 found that, of 49 midwives responding to a questionnaire regarding this study, 30 (61%) had never managed a third stage physiologically. Among the remaining 19, only one had practised physiological management as defined in the study. Those in Begley 1990 were also more used to active management and the PPH rate in the expectant arm fell during the study from 21% in the pilot study to 7% in the last six months, as they developed their skills. Yildirim 2016 was unique in that the authors had to train clinicians for the active management protocol, particularly in how to perform controlled cord traction, as it was not common practice in the hospital at the time.
Midwives’ skill and the accurate measurement of blood loss obviously has an impact on documented blood loss in the third stage of labour. For example, the mean (estimated) blood loss in the active arm of Rogers 1998 (269 mL, standard deviation (SD) 246), was actually greater than the mean (measured) blood loss in the expectant arm of Begley 1990 (235 mL, SD 224). This indicates that results of all these studies need to be examined in conjunction with local practice, to ascertain whether or not similar results will be found in different settings.
Finally, Prendiville 1988 changed the protocol after 425 births, but included all births in the results, which may have affected the findings.
We examined the quality of the body of evidence for our four primary outcomes for which we found data (severe primary PPH (≥ to 1000 mL at time of birth), maternal Hb < 9 g/dL 24 to 72 hours postpartum, admission to SCBU or NICU, neonatal jaundice requiring phototherapy or exchange transfusion) using GRADE. The GRADE assessments were of either low or very low quality. Downgrading decisions were based on inconsistency in two of the outcomes, and risk of bias and imprecision in all four ‐ see summary of findings Table for the main comparison.
Potential biases in the review process
All the authors of this review have an interest in third‐stage management, and each brings different views on the methods that might be used. C Begley conducted one of the studies included in the review, and is a member of a team who conducted a systematic review for the International Confederation of Midwives (ICM) on expectant management of the third stage of labour. G Gyte has written on the third stage and is a involved in a study on timing of cord clamping in preterm birth, and other members have written on third‐stage management. W McGuire is also involved in further studies on timing of cord clamping. A Weeks is involved in running clinical studies of the timing of cord clamping and misoprostol for third‐stage prophylaxis in low‐resource settings. However, the review authors’ views differed and, during the review process, discussion and consensus was necessary to reach a final conclusion acceptable to all. Although all humans bring potential biases to any endeavour, we did try to ensure that our eventual conclusion arose solely from the data. Feedback from an international audience will serve to improve the next review update.
Agreements and disagreements with other studies or reviews
Previous version of this review
Our assessment of the evidence differs from the first published version of this review (Prendiville 2000), which concluded that active management was "superior" to expectant management. For the main comparison, we have no additional studies but we analysed four studies (Jangsten 2011; Jerbi 2007; Yildirim 2016; Khan 1997), in different categories of 'active compared with mixed management', which were not included in the main analysis. We have, however, used the recent methodology introduced for Cochrane Reviews, which assesses risk of bias in the individual studies more carefully than in the past (Higgins 2017). We also chose to use a random‐effects model for analysis due to the clear variations in the specific forms of both active and expectant management used in the included studies (clinical heterogeneity). Our findings, therefore, differ for some outcomes because of this decision (particularly for the group of women at low risk of bleeding) but we have reported Tau² and I² statistic, regardless of level of heterogeneity. We believe the evidence shows both benefits and harms for active management, and believe it is now critical to look at the advantages and disadvantages of the individual components of third‐stage management to see if the benefits can be achieved with fewer harms.
The previous authors of this review recommended active management of the third stage due to the benefit identified in terms of reduced incidence of severe bleeding. We agree that bleeding is a very important component when balancing the benefits and harms of active compared to expectant management of the third stage of labour. However, we consider that the number of harms caused by active management also deserve consideration. In particular, the increased rate of hypertension, increased numbers of mothers returning to hospital due to bleeding, and the possible decrease in average blood volume of newborns reflected in the lower birthweight for babies where the mother has received active management of the third stage, are of concern. In the population of women at low risk of bleeding, such harms are of more concern, as there was no statistical evidence that severe bleeding was reduced by active management. Further studies would be needed to confirm if there is a difference or not. Our analysis of women at low risk of bleeding differs from the previous version of the review in that we excluded the Prendiville data (Prendiville 1988), as we considered there to be a high risk of bias because the randomisation was not stratified by high and low risk of bleeding and there were no specific data in the published study to enable us to use the data had we chosen to do so.
Other systematic reviews on active versus expectant management of the third stage of labour
Active management in the included studies involved, in general, clamping and cutting the cord soon after the baby’s birth. A number of women in the expectant management groups also had their baby’s cord clamped and cut before pulsation had ceased. Another Cochrane Review has recommended that, in future, the umbilical cord should not be clamped and cut until after pulsation has ceased, regardless of the type of management used (McDonald 2013); if this change in practice is implemented it may negate the harms of active management due to early cord clamping. However, the optimum timing of the administration of the uterotonic still needs to be determined clearly. Despite the evidence from the Cochrane Review regarding timing of cord clamping (McDonald 2013), a survey of 1176 members of the Royal College of Obstetricians and Gynaecologists (RCOG) and 1445 members of the Royal College of Midwives (RCM) in the UK found that the majority (94% and 71%, respectively) 'always' or 'usually' use active management, and 73% and 40% clamp the cord within 20 seconds (Farrar 2009b). It would thus appear that there is considerable variation in practice and not all practitioners use the complete package of ‘active’ or ‘expectant’ management as described in these studies.
Drawing on evidence from the Cochrane Review on 'Prophylactic ergometrine‐oxytocin versus oxytocin for the third stage of labour' (McDonald 2007b), and other research on ergot compounds (Maughan 2006), we would expect that omitting the ergot component of the prophylactic uterotonic drug used as part of active management of the third stage should reduce the adverse effects of hypertension identified for active management.
Guidelines issued by various policy‐making bodies promote different aspects of third‐stage management. The RCM provides information on the benefits and harms of both methods, drawing on the published literature, including the previous version of the Cochrane Review. They recommend providing information for women and state that expectant/physiological management of the third stage can be seen as the logical ending to a normal labour (RCM 2008). The National Institute for Health and Clinical Excellence (NICE) contains recommendations on the management of the third stage of labour in their guideline on intrapartum care (NICE 2014). Using the previous Cochrane Review and other published research evidence, NICE conclude that active management of the third stage is to be recommended, including the use of oxytocin (10 international units by intramuscular injection), deferred clamping and cutting of the cord and controlled cord traction. They recommend that women should be told the benefits and harms of both active and expectant management. It is recommended that women who request expectant management and are at low risk of PPH "should be supported in their choice" (NICE 2014 p 183), but the guideline does not acknowledge the findings of the previous Cochrane Review, in women at low risk of PPH, that show no difference in severe PPH or rates of maternal Hb less than 9 g/dL at 24 to 72 hours postnatal between those receiving expectant or active management. The World Health Organization (WHO) also bases its recommendations on the previous Cochrane Review, promoting the offering of active management to all women, provided they are cared for by skilled attendants (WHO 2012). The International Confederation of Midwives states that, "Every midwife is required to attend the birth of the placenta without the aid of uterotonics" and that knowledge of expectant/physiological management of the third stage is "a basic midwifery competency". It further recommends that "when a woman makes an active choice to experience a non‐interventionist placental birth, the midwife will ensure the woman and her family have all the information necessary on which to make the decision" (ICM 2008).
Two issues bear further discussion in relation to published work: the experience of midwives in using expectant management and the use of expectant management of the third stage when the first and second stages of labour have not been normal. The RCM defines a normal birth as one where a woman commences, continues and completes labour physiologically at term (RCM 2004 Part 4e). Anecdotally, midwives experienced in expectant management say that only women who have had a normal, physiological labour and birth should have expectant management of the third stage. It has also been suggested in the literature that women who require induction or augmentation of labour with oxytocin (Sheiner 2005), or misoprostol (Phillip 2004), are prone to higher blood loss postpartum. In three of the four studies included in this review, high percentages of women had received a uterotonic for induction or acceleration of labour, and in all of them expectant management was not the norm for the midwives involved. It was recommended at the time of the first Cochrane Review on this topic that studies be conducted in areas where midwives were skilled at using expectant or physiological management. The Netherlands and New Zealand are two such places, and observational studies emanating from these countries are worth examining as their results indicate no increase in blood loss in conjunction with the use of expectant management.
In Holland, a descriptive study was conducted to determine the incidence and risk factors for PPH in 3464 nulliparous women giving birth vaginally. The women were stratified for high and low risk factors for PPH, with 1416 stratified as low risk (41%) (Bais 2004). Approximately 50% of these women received prophylactic oxytocin and 50% did not, with no significant difference found in blood loss (Bais 2004). The New Zealand College of Midwives conducted a population‐based, retrospective cohort study, which reported on the management provided by midwives during the third stage of labour (NZCM 2009). The study included 33,752 women who experienced a expectant/physiologically normal labour and birth. Almost half of the women (48.1%) had expectant management in the third stage while 51.9% had an actively managed third stage. Women who had expectant management were more likely to have a blood loss of less than 500 mL (96.3%) than those who had active management (93.1%). Mean blood loss was 213.6 mL (95% CI 211.6 mL to 215.5 mL) for the expectant management group and 241.6 mL (95% CI 239.4 mL to 243.8 mL) for active management. Similar findings were seen in an Irish study comparing midwife‐led with consultant‐led care (Begley 2009; Begley 2011a). Thirty per cent (n = 136) of the 446 women who received midwife‐led care throughout their pregnancy and birth, and received no epidurals or oxytocin in labour, had expectant management. None of these 136 women had a PPH, whereas the PPH rate for the women having active management was 1% (Begley 2009). A more recent study in the same Irish midwife‐led unit (MLU), over a six‐year period, showed that, of 1878 women birthing in the MLU, 50% had physiological management of the third stage compared with 5% of 900 similarly low‐risk women who were transferred to the hospital labour ward and had a spontaneous vaginal birth. The PPH rates were 2.9% and 7.2%, respectively (Dencker 2017).
Although these are observational data, there is an interesting link here between normal blood loss and expectant management of the third stage, when such management follows a physiologically normal first and second stage, and care is given by midwives skilled in the technique. This is an area that would benefit from further research.

Study flow diagram

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Comparison 1 Active versus expectant management of 3rd stage of labour (all women), Outcome 1 Severe primary postpartum haemorrhage (PPH) at time of birth (clinically estimated or measured blood loss ≥ 1000 mL).

Comparison 1 Active versus expectant management of 3rd stage of labour (all women), Outcome 4 Maternal Hb < 9 g/dL 24‐72 hours postpartum.

Comparison 1 Active versus expectant management of 3rd stage of labour (all women), Outcome 5 Admission to neonatal special/intensive care.

Comparison 1 Active versus expectant management of 3rd stage of labour (all women), Outcome 6 Neonatal jaundice requiring phototherapy or exchange transfusion.

Comparison 1 Active versus expectant management of 3rd stage of labour (all women), Outcome 10 Primary blood loss ≥ 500 mL at time of birth (clinically estimated or measured).

Comparison 1 Active versus expectant management of 3rd stage of labour (all women), Outcome 13 Mean maternal blood loss (mL) at time of birth (clinically estimated or measured).

Comparison 1 Active versus expectant management of 3rd stage of labour (all women), Outcome 16 Maternal blood transfusion.

Comparison 1 Active versus expectant management of 3rd stage of labour (all women), Outcome 18 Therapeutic uterotonics during third stage and/or within 24 hours.

Comparison 1 Active versus expectant management of 3rd stage of labour (all women), Outcome 19 Mean length of third stage.

Comparison 1 Active versus expectant management of 3rd stage of labour (all women), Outcome 20 Manual removal of placenta as defined by study authors.

Comparison 1 Active versus expectant management of 3rd stage of labour (all women), Outcome 21 Postnatal diastolic blood pressure > 90 mmHg between birth of baby and discharge from the labour ward.
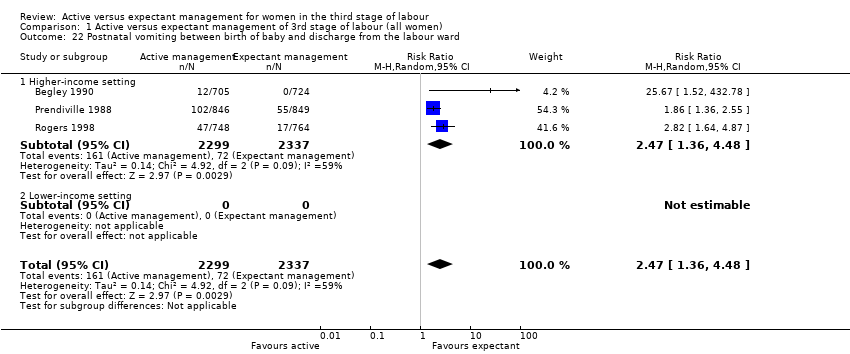
Comparison 1 Active versus expectant management of 3rd stage of labour (all women), Outcome 22 Postnatal vomiting between birth of baby and discharge from the labour ward.

Comparison 1 Active versus expectant management of 3rd stage of labour (all women), Outcome 23 Any analgesia between birth of the baby and discharge from labour ward.

Comparison 1 Active versus expectant management of 3rd stage of labour (all women), Outcome 25 Secondary blood loss/any vaginal bleeding needing treatment (after 24 hours and up to 6 weeks).

Comparison 1 Active versus expectant management of 3rd stage of labour (all women), Outcome 27 Surgical evacuation of retained products of conception.

Comparison 1 Active versus expectant management of 3rd stage of labour (all women), Outcome 28 Afterpains ‐ abdominal pain associated with the contracting uterus in the postpartum period.

Comparison 1 Active versus expectant management of 3rd stage of labour (all women), Outcome 29 Apgar score < 7 at 5 minutes.

Comparison 1 Active versus expectant management of 3rd stage of labour (all women), Outcome 30 Birthweight.

Comparison 1 Active versus expectant management of 3rd stage of labour (all women), Outcome 38 Exclusive breastfeeding at discharge from hospital.

Comparison 1 Active versus expectant management of 3rd stage of labour (all women), Outcome 40 Return to hospital as in‐ or outpatient because of bleeding (not pre‐specified).

Comparison 1 Active versus expectant management of 3rd stage of labour (all women), Outcome 41 Postnatal maternal mean Hb (outcome not pre‐specified).

Comparison 2 Active versus expectant management of 3rd stage of labour (women at low risk), Outcome 1 Severe primary PPH at time of birth (clinically estimated or measured blood loss ≥ 1000 mL).

Comparison 2 Active versus expectant management of 3rd stage of labour (women at low risk), Outcome 4 Maternal Hb < 9 g/dL at 24‐72 hr.

Comparison 2 Active versus expectant management of 3rd stage of labour (women at low risk), Outcome 5 Admission to neonatal special/intensive care.

Comparison 2 Active versus expectant management of 3rd stage of labour (women at low risk), Outcome 6 Neonatal jaundice requiring phototherapy or exchange transfusion.

Comparison 2 Active versus expectant management of 3rd stage of labour (women at low risk), Outcome 10 Primary blood loss ≥ 500 mL at time of birth (clinically estimated or measured).
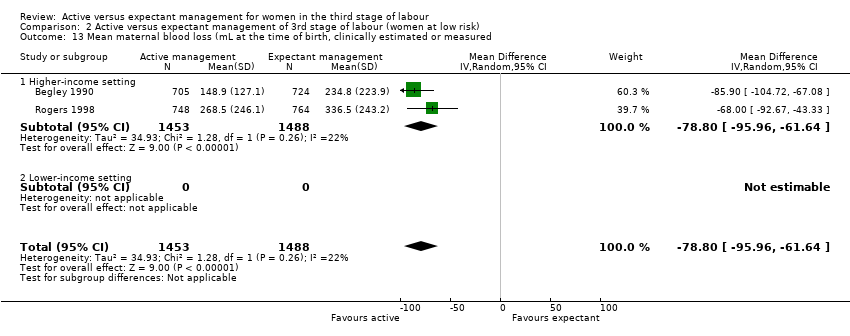
Comparison 2 Active versus expectant management of 3rd stage of labour (women at low risk), Outcome 13 Mean maternal blood loss (mL at the time of birth, clinically estimated or measured.

Comparison 2 Active versus expectant management of 3rd stage of labour (women at low risk), Outcome 16 Maternal blood transfusion.

Comparison 2 Active versus expectant management of 3rd stage of labour (women at low risk), Outcome 18 Therapeutic uterotonics during third stage and/or within 24 hours.
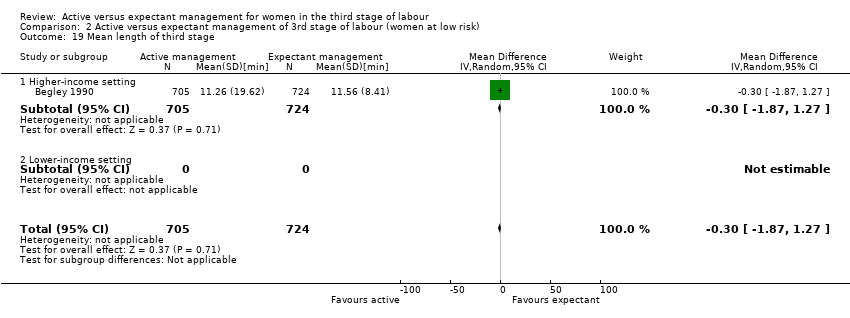
Comparison 2 Active versus expectant management of 3rd stage of labour (women at low risk), Outcome 19 Mean length of third stage.

Comparison 2 Active versus expectant management of 3rd stage of labour (women at low risk), Outcome 20 Manual removal of placenta as defined by study authors.

Comparison 2 Active versus expectant management of 3rd stage of labour (women at low risk), Outcome 21 Postnatal diastolic blood pressure > 90 mmHg between birth of baby and discharge from the labour ward.

Comparison 2 Active versus expectant management of 3rd stage of labour (women at low risk), Outcome 22 Postnatal vomiting between birth of baby and discharge from the labour ward..

Comparison 2 Active versus expectant management of 3rd stage of labour (women at low risk), Outcome 23 Any analgesia between birth of the baby and up to discharge from labour ward.

Comparison 2 Active versus expectant management of 3rd stage of labour (women at low risk), Outcome 25 Secondary blood loss/any vaginal bleeding needing treatment (after 24 hours and up to 6 weeks).

Comparison 2 Active versus expectant management of 3rd stage of labour (women at low risk), Outcome 27 Surgical evacuation of retained products of conception.

Comparison 2 Active versus expectant management of 3rd stage of labour (women at low risk), Outcome 28 Afterpains ‐ abdominal pain associated with the contracting uterus in the postpartum period.

Comparison 2 Active versus expectant management of 3rd stage of labour (women at low risk), Outcome 30 Birthweight.

Comparison 2 Active versus expectant management of 3rd stage of labour (women at low risk), Outcome 40 Return to hospital as in‐ or outpatient because of bleeding (not pre‐specified).

Comparison 2 Active versus expectant management of 3rd stage of labour (women at low risk), Outcome 41 Postnatal maternal mean Hb (outcome not pre‐specified).

Comparison 5 Active versus mixed management of 3rd stage (delayed uterotonic, delayed cord clamping, no controlled cord traction), Outcome 8 Maternal blood transfusion.

Comparison 5 Active versus mixed management of 3rd stage (delayed uterotonic, delayed cord clamping, no controlled cord traction), Outcome 9 Therapeutic uterotonics during third stage and/or within 24 hours.

Comparison 5 Active versus mixed management of 3rd stage (delayed uterotonic, delayed cord clamping, no controlled cord traction), Outcome 10 Mean length of third stage.

Comparison 5 Active versus mixed management of 3rd stage (delayed uterotonic, delayed cord clamping, no controlled cord traction), Outcome 11 Manual removal of placenta as defined by study authors.

Comparison 5 Active versus mixed management of 3rd stage (delayed uterotonic, delayed cord clamping, no controlled cord traction), Outcome 12 Surgical evacuation of retained products of conception.

Comparison 5 Active versus mixed management of 3rd stage (delayed uterotonic, delayed cord clamping, no controlled cord traction), Outcome 13 Birthweight.

Comparison 5 Active versus mixed management of 3rd stage (delayed uterotonic, delayed cord clamping, no controlled cord traction), Outcome 14 Postnatal maternal mean Hb.

Comparison 9 Active versus mixed management (uterotonic after placental delivery, immediate cord clamping and no controlled cord traction) , Outcome 1 Severe primary PPH at time of birth (clinically estimated or measured blood loss ≥ 1000 mL).

Comparison 9 Active versus mixed management (uterotonic after placental delivery, immediate cord clamping and no controlled cord traction) , Outcome 10 Primary blood loss ≥ 500 mL at time of birth (clinically estimated or measured).
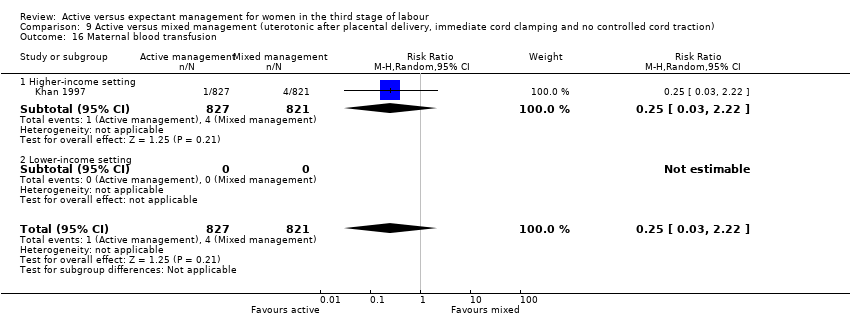
Comparison 9 Active versus mixed management (uterotonic after placental delivery, immediate cord clamping and no controlled cord traction) , Outcome 16 Maternal blood transfusion.

Comparison 9 Active versus mixed management (uterotonic after placental delivery, immediate cord clamping and no controlled cord traction) , Outcome 17 Clinical signs of severe blood loss.
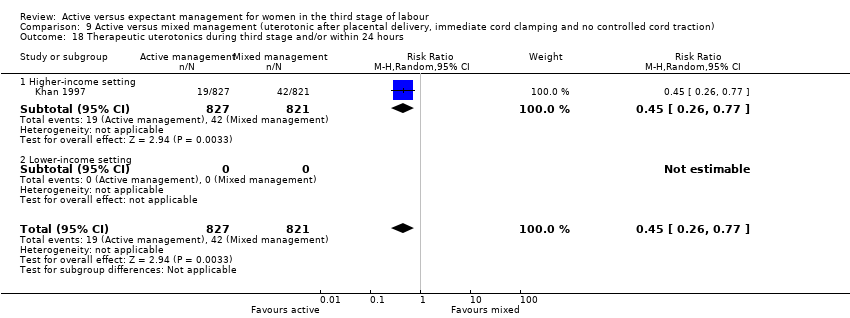
Comparison 9 Active versus mixed management (uterotonic after placental delivery, immediate cord clamping and no controlled cord traction) , Outcome 18 Therapeutic uterotonics during third stage and/or within 24 hours.

Comparison 9 Active versus mixed management (uterotonic after placental delivery, immediate cord clamping and no controlled cord traction) , Outcome 19 Mean length of third stage.

Comparison 10 Active versus mixed management (no routine uterotonic, early cord clamping, no controlled cord traction), Outcome 1 Severe primary PPH at time of birth (clinically estimated or measured blood loss ≥ 1000 mL).

Comparison 10 Active versus mixed management (no routine uterotonic, early cord clamping, no controlled cord traction), Outcome 4 Maternal Hb < 9 g/dL at 24‐72 hr.

Comparison 10 Active versus mixed management (no routine uterotonic, early cord clamping, no controlled cord traction), Outcome 10 Primary blood loss ≥ 500 mL at time of birth (clinically estimated or measured).

Comparison 10 Active versus mixed management (no routine uterotonic, early cord clamping, no controlled cord traction), Outcome 13 Mean maternal blood loss (mL) at time of birth (clinically estimated or measured).

Comparison 10 Active versus mixed management (no routine uterotonic, early cord clamping, no controlled cord traction), Outcome 16 Maternal blood transfusion.

Comparison 10 Active versus mixed management (no routine uterotonic, early cord clamping, no controlled cord traction), Outcome 18 Therapeutic uterotonics during third stage and/or within 24 hours.
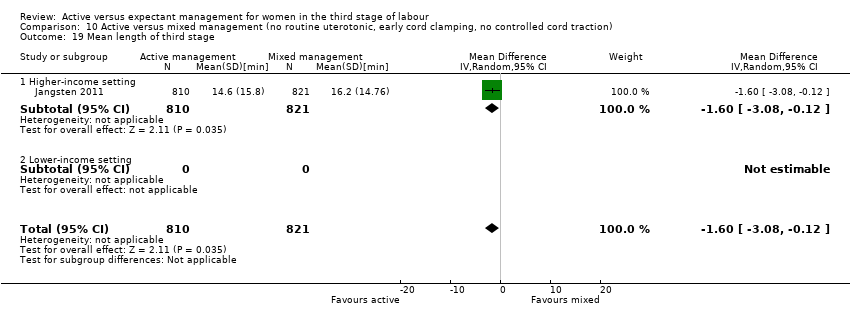
Comparison 10 Active versus mixed management (no routine uterotonic, early cord clamping, no controlled cord traction), Outcome 19 Mean length of third stage.

Comparison 10 Active versus mixed management (no routine uterotonic, early cord clamping, no controlled cord traction), Outcome 20 Manual removal of placenta as defined by study authors.

Comparison 10 Active versus mixed management (no routine uterotonic, early cord clamping, no controlled cord traction), Outcome 28 Not prespecified: afterpains at 2 hours after birth (id 20458).

Comparison 10 Active versus mixed management (no routine uterotonic, early cord clamping, no controlled cord traction), Outcome 29 Not pre‐specified: afterpains the day after birth (id 20458).

Comparison 10 Active versus mixed management (no routine uterotonic, early cord clamping, no controlled cord traction), Outcome 31 Birthweight.

Comparison 10 Active versus mixed management (no routine uterotonic, early cord clamping, no controlled cord traction), Outcome 42 Postnatal maternal mean Hb (outcome not pre‐specified).

Comparison 10 Active versus mixed management (no routine uterotonic, early cord clamping, no controlled cord traction), Outcome 43 Severe primary PPH after placental delivery and up to 2 hours (clinically estimated or measured blood loss ≥ 1000 mL) ‐ not pre‐specified.

Comparison 10 Active versus mixed management (no routine uterotonic, early cord clamping, no controlled cord traction), Outcome 44 Severe primary PPH at time of birth and up to 2 hours (clinically estimated or measured blood loss ≥1000 mL) ‐ not pre‐specified.

Comparison 10 Active versus mixed management (no routine uterotonic, early cord clamping, no controlled cord traction), Outcome 45 Mean blood loss (mL) (clinically estimated or measured at birth and up to 2 hours (not pre‐specified).

Comparison 11 Active versus mixed management (no routine uterotonic, early cord clamping, controlled cord traction), Outcome 4 Maternal Hb < 9 g/dL at 24‐72 hr.

Comparison 11 Active versus mixed management (no routine uterotonic, early cord clamping, controlled cord traction), Outcome 19 Mean length of third stage.
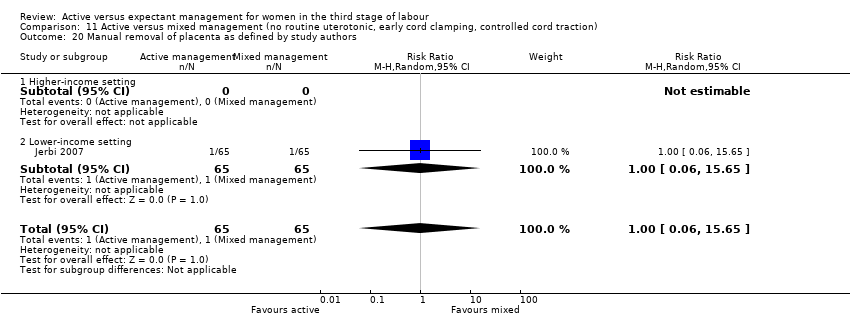
Comparison 11 Active versus mixed management (no routine uterotonic, early cord clamping, controlled cord traction), Outcome 20 Manual removal of placenta as defined by study authors.
| Active versus expectant management of the third stage of labour (all women) | ||||||
| Population: all women who expected a vaginal birth at 24 weeks' gestation or later and their babies Setting: UK and Ireland, hospital setting. The countries were classified as 'higher‐income' and 'lower‐income', with the border between lower‐middle‐income and upper‐middle‐income being the cut‐off. All studies included in this main analysis were undertaken in higher‐income countries (defined according to World Bank definitions 2018). Intervention: active management of the third stage of labour | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Expectant management of the third stage of labour | Active management of the third stage of labour | |||||
| Severe primary PPH (clinically estimated or measured blood loss ≥ 1000 mL at time of birth) | 24 per 1000 | 8 per 1000 | RR 0.34 | 4636 | ⊕⊝⊝⊝ | |
| Very severe primary PPH (clinically estimated or measured blood loss ≥ 2500 mL at time of birth) | See comment | See comment | Not estimable | 0 | See comment | No data |
| Maternal mortality | See comment | See comment | Not estimable | 0 | See comment | No data |
| Maternal Hb < 9 g/dL 24‐72 hours postpartum | 71 per 1000 | 36 per 1000 | RR 0.50 | 1572 | ⊕⊕⊝⊝ | |
| Admission to SCBU/NICU | 52 per 1000 | 42 per 1000 | RR 0.81 | 3207 | ⊕⊕⊝⊝ | |
| Neonatal jaundice requiring phototherapy or exchange transfusion | 49 per 1000 | 47 per 1000 | RR 0.96 | 3142 | ⊕⊝⊝⊝ | |
| Neonatal polycythaemia treated with dilutional exchange transfusion | See comment | See comment | Not estimable | 0 | See comment | No data |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| aRisk of bias: of the three studies providing data for this outcome, all are at low risk of bias for sequence generation (selection bias) and allocation concealment (selection bias). All are at high risk of bias for lack of blinding for clinicians and women and all are unclear for blinding of outcome assessment. Two studies are at low risk of bias for incomplete outcome data (attrition bias), and one is unclear. Two are at high risk of selective reporting (reporting bias) and one is unclear. One study is at high risk of other bias and two are unclear (see 'Risk of bias' tables and Figure 2). Downgraded 1. bRisk of bias: of the two studies providing data for this outcome, both are at low risk of bias for sequence generation (selection bias) and one is at low risk of bias for allocation concealment (selection bias) and the other is unclear. Both are at high risk of bias for lack of blinding of clinicians and women, both are unclear for blinding of outcome assessment (although unlikely to affect Hb measurements). One is at high risk of bias for incomplete outcome data (attrition bias) while the other is unclear. One is high risk of bias for selective reporting (reporting bias), the other is unclear. Both studies are at high risk of other bias (see 'Risk of bias' tables and Figure 2). Downgraded 1. cRisk of bias: of the two studies providing data for this outcome, both are at low risk of bias for sequence generation (selection bias) and allocation concealment (selection bias). Both are at high risk of bias for lack of blinding of clinicians and women, both are unclear for blinding of outcome assessment. One is at low risk of bias for incomplete outcome data (attrition bias), the other is unclear. Both are at high risk of bias for selective reporting (reporting bias) and both are at high risk for other biases (see 'Risk of bias' tables and Figure 2). Downgraded 1. dRisk of bias: of the two studies providing data for this outcome, both are at low risk of bias for sequence generation (selection bias) and allocation concealment (selection bias). Both are at high risk of bias for lack of blinding of clinicians and women, both are unclear for blinding of outcome assessment. One is low risk of bias for incomplete outcome data (attrition bias), the other is unclear. Both are at high risk of bias for selective reporting (reporting bias) and both are at high risk of other biases (see 'Risk of bias' tables and Figure 2). Downgraded 1. | ||||||
| Terms | Definitions used in this review |
| Expectant management of third stage of labour |
|
| Active management of third stage of labour |
|
| Mixed management of third stage of labour | A mixture of some of the components of both active and expectant management of third stage of labour, but without exclusively containing all the components of either. There can be a number of different mixed third stage managements, for example:
|
| Early prophylactic uterotonic | Prophylactic uterotonic drug administered just before, with, or immediately after, the birth of the infant |
| Delayed prophylactic uterotonic | Prophylactic uterotonic drug administered after the cord pulsation has ceased |
| Early cord clamping | The application of a clamp to the umbilical cord within 60 seconds of the birth of the infant (McDonald 2013) |
| Delayed cord clamping | The application of a clamp to the umbilical cord more than 1 minute after birth or when cord pulsation has ceased (McDonald 2013) |
| Sarnat staging for hypoxic ischaemic encephalopathy (Sarnat 1976) |
|
| Study | Active management protocol | Expectant management protocol | Active management used | Expectant management used |
|
|
|
|
| |
|
|
|
|
| |
|
|
|
|
| |
|
|
| No information | No information | |
| BP: blood pressure; CCT: controlled cord traction; IM: intramuscular; IV: intravenous | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Severe primary postpartum haemorrhage (PPH) at time of birth (clinically estimated or measured blood loss ≥ 1000 mL) Show forest plot | 3 | 4636 | Risk Ratio (M‐H, Random, 95% CI) | 0.34 [0.14, 0.87] |
| 1.1 Higher‐income setting | 3 | 4636 | Risk Ratio (M‐H, Random, 95% CI) | 0.34 [0.14, 0.87] |
| 1.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Very severe primary PPH at time of birth (clinically estimated or measured blood loss ≥ 2500 mL) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 3 Maternal mortality | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 3.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 3.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Maternal Hb < 9 g/dL 24‐72 hours postpartum Show forest plot | 2 | 1572 | Risk Ratio (M‐H, Random, 95% CI) | 0.50 [0.30, 0.83] |
| 4.1 Higher‐income setting | 2 | 1572 | Risk Ratio (M‐H, Random, 95% CI) | 0.50 [0.30, 0.83] |
| 4.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Admission to neonatal special/intensive care Show forest plot | 2 | 3207 | Risk Ratio (M‐H, Random, 95% CI) | 0.81 [0.60, 1.11] |
| 5.1 Higher‐income setting | 2 | 3207 | Risk Ratio (M‐H, Random, 95% CI) | 0.81 [0.60, 1.11] |
| 5.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Neonatal jaundice requiring phototherapy or exchange transfusion Show forest plot | 2 | 3142 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.55, 1.68] |
| 6.1 Higher‐income setting | 2 | 3142 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.55, 1.68] |
| 6.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Neonatal polycythaemia treated with dilutional exchange transfusion | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 7.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 7.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 8 Severe primary PPH after placental delivery and up to 24 hours (clinically estimated or measured blood loss ≥ 1000 mL) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 8.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 8.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 9 Severe primary PPH at time of birth and up to 24 hours (clinically estimated or measured blood loss ≥ 1000 mL) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 9.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 9.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 10 Primary blood loss ≥ 500 mL at time of birth (clinically estimated or measured) Show forest plot | 3 | 4636 | Risk Ratio (M‐H, Random, 95% CI) | 0.34 [0.27, 0.44] |
| 10.1 Higher‐income setting | 3 | 4636 | Risk Ratio (M‐H, Random, 95% CI) | 0.34 [0.27, 0.44] |
| 10.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 11 Primary blood loss ≥ 500 mL after delivery of placenta and up to 24 hours (clinically estimated or measured) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 11.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 11.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 12 Primary blood loss ≥ 500 mL at time of birth and up to 24 hours (clinically estimated or measured) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 12.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 12.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 13 Mean maternal blood loss (mL) at time of birth (clinically estimated or measured) Show forest plot | 2 | 2941 | Mean Difference (IV, Random, 95% CI) | ‐78.80 [‐95.96, ‐61.64] |
| 13.1 Higher‐income setting | 2 | 2941 | Mean Difference (IV, Random, 95% CI) | ‐78.80 [‐95.96, ‐61.64] |
| 13.2 Lower‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 14 Mean maternal blood loss (mL) after delivery of placenta and up to 24 hours (clinically estimated or measured) | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 14.1 Higher‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 14.2 Lower‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 15 Mean maternal blood loss (mL at time of birth and up to 24 hours (clinically estimated or measured) | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 15.1 Higher‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 15.2 Lower‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 16 Maternal blood transfusion Show forest plot | 4 | 4829 | Risk Ratio (M‐H, Random, 95% CI) | 0.35 [0.22, 0.55] |
| 16.1 Higher‐income setting | 4 | 4829 | Risk Ratio (M‐H, Random, 95% CI) | 0.35 [0.22, 0.55] |
| 16.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 17 Clinical signs of severe blood loss | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 17.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 17.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 18 Therapeutic uterotonics during third stage and/or within 24 hours Show forest plot | 4 | 4829 | Risk Ratio (M‐H, Random, 95% CI) | 0.19 [0.15, 0.23] |
| 18.1 Higher‐income setting | 4 | 4829 | Risk Ratio (M‐H, Random, 95% CI) | 0.19 [0.15, 0.23] |
| 18.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 19 Mean length of third stage Show forest plot | 1 | 1429 | Mean Difference (IV, Random, 95% CI) | ‐0.30 [‐1.87, 1.27] |
| 19.1 Higher‐income setting | 1 | 1429 | Mean Difference (IV, Random, 95% CI) | ‐0.30 [‐1.87, 1.27] |
| 19.2 Lower‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 20 Manual removal of placenta as defined by study authors Show forest plot | 4 | 4829 | Risk Ratio (M‐H, Random, 95% CI) | 1.78 [0.57, 5.56] |
| 20.1 Higher‐income setting | 4 | 4829 | Risk Ratio (M‐H, Random, 95% CI) | 1.78 [0.57, 5.56] |
| 20.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 21 Postnatal diastolic blood pressure > 90 mmHg between birth of baby and discharge from the labour ward Show forest plot | 3 | 4636 | Risk Ratio (M‐H, Random, 95% CI) | 4.10 [1.63, 10.30] |
| 21.1 Higher‐income setting | 3 | 4636 | Risk Ratio (M‐H, Random, 95% CI) | 4.10 [1.63, 10.30] |
| 21.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 22 Postnatal vomiting between birth of baby and discharge from the labour ward Show forest plot | 3 | 4636 | Risk Ratio (M‐H, Random, 95% CI) | 2.47 [1.36, 4.48] |
| 22.1 Higher‐income setting | 3 | 4636 | Risk Ratio (M‐H, Random, 95% CI) | 2.47 [1.36, 4.48] |
| 22.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 23 Any analgesia between birth of the baby and discharge from labour ward Show forest plot | 1 | 1429 | Risk Ratio (M‐H, Random, 95% CI) | 2.53 [1.34, 4.78] |
| 23.1 Higher‐income setting | 1 | 1429 | Risk Ratio (M‐H, Random, 95% CI) | 2.53 [1.34, 4.78] |
| 23.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 24 Women's assessment of pain during third stage as reported by study authors | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 24.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 24.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 25 Secondary blood loss/any vaginal bleeding needing treatment (after 24 hours and up to 6 weeks) Show forest plot | 3 | 4636 | Risk Ratio (M‐H, Random, 95% CI) | 1.10 [0.40, 2.99] |
| 25.1 Higher‐income setting | 3 | 4636 | Risk Ratio (M‐H, Random, 95% CI) | 1.10 [0.40, 2.99] |
| 25.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 26 Amount of lochia either estimated or measured after 24 hours and up to discharge from hospital | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 26.1 Higher‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 26.2 Lower‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 27 Surgical evacuation of retained products of conception Show forest plot | 3 | 4636 | Risk Ratio (M‐H, Random, 95% CI) | 0.74 [0.32, 1.71] |
| 27.1 Higher‐income setting | 3 | 4636 | Risk Ratio (M‐H, Random, 95% CI) | 0.74 [0.32, 1.71] |
| 27.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 28 Afterpains ‐ abdominal pain associated with the contracting uterus in the postpartum period Show forest plot | 1 | 1429 | Risk Ratio (M‐H, Random, 95% CI) | 2.53 [1.34, 4.78] |
| 28.1 Higher‐income setting | 1 | 1429 | Risk Ratio (M‐H, Random, 95% CI) | 2.53 [1.34, 4.78] |
| 28.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 29 Apgar score < 7 at 5 minutes Show forest plot | 1 | 1695 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.38, 2.66] |
| 29.1 Higher‐income setting | 1 | 1695 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.38, 2.66] |
| 29.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 30 Birthweight Show forest plot | 2 | 3207 | Mean Difference (IV, Random, 95% CI) | ‐76.90 [‐108.51, ‐45.30] |
| 30.1 Higher‐income setting | 2 | 3207 | Mean Difference (IV, Random, 95% CI) | ‐76.90 [‐108.51, ‐45.30] |
| 30.2 Lower‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 31 Neonatal encephalopathy assessed using Sarnat staging (Sarnat 1976; Table 1) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 31.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 31.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 32 Neonatal mortality | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 32.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 32.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 33 Intraventricular haemorrhage ‐ Papille grade III/IV ‐ (for infants born before 34 weeks' gestation only) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 33.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 33.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 34 Number of infants who received a red blood cell transfusion | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 34.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 34.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 35 Infant Hb level at 24 to 72 hours | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 35.1 Higher‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 35.2 Lower‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 36 Infant Hb level at 3‐6 months | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 36.1 Higher‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 36.2 Lower‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 37 Infant iron indices (ferritin) at 3 to 6 months. | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 37.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 37.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 38 Exclusive breastfeeding at discharge from hospital Show forest plot | 1 | 1695 | Risk Ratio (M‐H, Random, 95% CI) | 1.01 [0.96, 1.07] |
| 38.1 Higher‐income setting | 1 | 1695 | Risk Ratio (M‐H, Random, 95% CI) | 1.01 [0.96, 1.07] |
| 38.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 39 Neurodevelopmental, cognitive or developmental outcomes assessed after age 18 months | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 39.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 39.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 40 Return to hospital as in‐ or outpatient because of bleeding (not pre‐specified) Show forest plot | 2 | 2941 | Risk Ratio (M‐H, Random, 95% CI) | 2.21 [1.29, 3.79] |
| 40.1 Higher‐income setting | 2 | 2941 | Risk Ratio (M‐H, Random, 95% CI) | 2.21 [1.29, 3.79] |
| 40.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 41 Postnatal maternal mean Hb (outcome not pre‐specified) Show forest plot | 3 | 4062 | Mean Difference (IV, Random, 95% CI) | 0.52 [0.44, 0.60] |
| 41.1 Higher‐income setting | 3 | 4062 | Mean Difference (IV, Random, 95% CI) | 0.52 [0.44, 0.60] |
| 41.2 Lower‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Severe primary PPH at time of birth (clinically estimated or measured blood loss ≥ 1000 mL) Show forest plot | 2 | 2941 | Risk Ratio (M‐H, Random, 95% CI) | 0.31 [0.05, 2.17] |
| 1.1 Higher‐income setting | 2 | 2941 | Risk Ratio (M‐H, Random, 95% CI) | 0.31 [0.05, 2.17] |
| 1.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Very severe primary PPH at time of birth (clinically estimated or measured blood loss ≥ 2500 mL) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 3 Maternal mortality | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 3.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 3.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Maternal Hb < 9 g/dL at 24‐72 hr Show forest plot | 1 | 193 | Risk Ratio (M‐H, Random, 95% CI) | 0.17 [0.02, 1.47] |
| 4.1 Higher‐income setting | 1 | 193 | Risk Ratio (M‐H, Random, 95% CI) | 0.17 [0.02, 1.47] |
| 4.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Admission to neonatal special/intensive care Show forest plot | 1 | 1512 | Risk Ratio (M‐H, Random, 95% CI) | 1.02 [0.55, 1.88] |
| 5.1 Higher‐income setting | 1 | 1512 | Risk Ratio (M‐H, Random, 95% CI) | 1.02 [0.55, 1.88] |
| 5.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Neonatal jaundice requiring phototherapy or exchange transfusion Show forest plot | 1 | 1447 | Risk Ratio (M‐H, Random, 95% CI) | 1.31 [0.78, 2.18] |
| 6.1 Higher‐income setting | 1 | 1447 | Risk Ratio (M‐H, Random, 95% CI) | 1.31 [0.78, 2.18] |
| 6.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Neonatal polycythaemia treated with dilutional exchange transfusion | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 7.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 7.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 8 Severe primary PPH after placental delivery and up to 24 hours (clinically estimated or measured blood loss ≥ 1000 mL) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 8.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 8.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 9 Severe primary PPH at time of birth and up to 24 hours (clinically estimated or measured blood loss ≥ 1000 mL) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 9.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 9.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 10 Primary blood loss ≥ 500 mL at time of birth (clinically estimated or measured) Show forest plot | 2 | 2941 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.20, 0.56] |
| 10.1 Higher‐income setting | 2 | 2941 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.20, 0.56] |
| 10.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 11 Primary blood loss ≥ 500 mL after delivery of placenta and up to 24 hours (clinically estimated or measured) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 11.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 11.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 12 Primary blood loss ≥ 500 mL at time of birth and up to 24 hours (clinically estimated or measured) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 12.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 12.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 13 Mean maternal blood loss (mL at the time of birth, clinically estimated or measured Show forest plot | 2 | 2941 | Mean Difference (IV, Random, 95% CI) | ‐78.80 [‐95.96, ‐61.64] |
| 13.1 Higher‐income setting | 2 | 2941 | Mean Difference (IV, Random, 95% CI) | ‐78.80 [‐95.96, ‐61.64] |
| 13.2 Lower‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 14 Mean maternal blood loss (mL) after delivery of placenta and up to 24 hours (clinically estimated or measured) | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 14.1 Higher‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 14.2 Lower‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 15 Mean maternal blood loss (mL) at time of birth and up to 24 hours (clinically estimated or measured) | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 15.1 Higher‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 15.2 Lower‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 16 Maternal blood transfusion Show forest plot | 3 | 3134 | Risk Ratio (M‐H, Random, 95% CI) | 0.30 [0.10, 0.88] |
| 16.1 Higher‐income setting | 3 | 3134 | Risk Ratio (M‐H, Random, 95% CI) | 0.30 [0.10, 0.88] |
| 16.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 17 Clinical signs of severe blood loss | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 17.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 17.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 18 Therapeutic uterotonics during third stage and/or within 24 hours Show forest plot | 3 | 3134 | Risk Ratio (M‐H, Random, 95% CI) | 0.15 [0.11, 0.21] |
| 18.1 Higher‐income setting | 3 | 3134 | Risk Ratio (M‐H, Random, 95% CI) | 0.15 [0.11, 0.21] |
| 18.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 19 Mean length of third stage Show forest plot | 1 | 1429 | Mean Difference (IV, Random, 95% CI) | ‐0.30 [‐1.87, 1.27] |
| 19.1 Higher‐income setting | 1 | 1429 | Mean Difference (IV, Random, 95% CI) | ‐0.30 [‐1.87, 1.27] |
| 19.2 Lower‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 20 Manual removal of placenta as defined by study authors Show forest plot | 3 | 3134 | Risk Ratio (M‐H, Random, 95% CI) | 3.58 [0.42, 30.61] |
| 20.1 Higher‐income setting | 3 | 3134 | Risk Ratio (M‐H, Random, 95% CI) | 3.58 [0.42, 30.61] |
| 20.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 21 Postnatal diastolic blood pressure > 90 mmHg between birth of baby and discharge from the labour ward Show forest plot | 2 | 2941 | Risk Ratio (M‐H, Random, 95% CI) | 7.00 [2.99, 16.43] |
| 21.1 Higher‐income setting | 2 | 2941 | Risk Ratio (M‐H, Random, 95% CI) | 7.00 [2.99, 16.43] |
| 21.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 22 Postnatal vomiting between birth of baby and discharge from the labour ward. Show forest plot | 2 | 2941 | Risk Ratio (M‐H, Random, 95% CI) | 5.63 [0.69, 46.08] |
| 22.1 Higher‐income setting | 2 | 2941 | Risk Ratio (M‐H, Random, 95% CI) | 5.63 [0.69, 46.08] |
| 22.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 23 Any analgesia between birth of the baby and up to discharge from labour ward Show forest plot | 1 | 1429 | Risk Ratio (M‐H, Random, 95% CI) | 2.53 [1.34, 4.78] |
| 23.1 Higher‐income setting | 1 | 1429 | Risk Ratio (M‐H, Random, 95% CI) | 2.53 [1.34, 4.78] |
| 23.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 24 Women's assessment of pain during third stage as reported by study authors | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 24.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 24.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 25 Secondary blood loss/any vaginal bleeding needing treatment (after 24 hours and up to 6 weeks) Show forest plot | 2 | 2941 | Risk Ratio (M‐H, Random, 95% CI) | 1.78 [0.69, 4.60] |
| 25.1 Higher‐income setting | 2 | 2941 | Risk Ratio (M‐H, Random, 95% CI) | 1.78 [0.69, 4.60] |
| 25.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 26 Amount of lochia either estimated or measured after 24 hours and up to discharge from hospital | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 26.1 Higher‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 26.2 Lower‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 27 Surgical evacuation of retained products of conception Show forest plot | 2 | 2941 | Risk Ratio (M‐H, Random, 95% CI) | 0.69 [0.12, 3.98] |
| 27.1 Higher‐income setting | 2 | 2941 | Risk Ratio (M‐H, Random, 95% CI) | 0.69 [0.12, 3.98] |
| 27.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 28 Afterpains ‐ abdominal pain associated with the contracting uterus in the postpartum period Show forest plot | 1 | 1429 | Risk Ratio (M‐H, Random, 95% CI) | 2.53 [1.34, 4.78] |
| 28.1 Higher‐income setting | 1 | 1429 | Risk Ratio (M‐H, Random, 95% CI) | 2.53 [1.34, 4.78] |
| 28.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 29 Apgar score < 7 at 5 minutes | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 29.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 29.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 30 Birthweight Show forest plot | 1 | 1512 | Mean Difference (IV, Random, 95% CI) | ‐67.0 [‐114.13, ‐19.87] |
| 30.1 Higher‐income setting | 1 | 1512 | Mean Difference (IV, Random, 95% CI) | ‐67.0 [‐114.13, ‐19.87] |
| 30.2 Lower‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 31 Neonatal encephalopathy assessed using Sarnat staging (Sarnat 1976; Table 1) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 31.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 31.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 32 Neonatal mortality | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 32.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 32.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 33 Intraventricular haemorrhage ‐ Papille grade III/IV ‐ (for infants born before 34 weeks' gestation only) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 33.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 33.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 34 Number of infants exposed to one or more red blood cell transfusions | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 34.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 34.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 35 Infant Hb level at 24 to 72 hours | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 35.1 Higher‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 35.2 Lower‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 36 Infant Hb level at 3‐6 months | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 36.1 Higher‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 36.2 Lower‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 37 Infant iron indices (ferritin) at 3 to 6 months. | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 37.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 37.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 38 Exclusive breastfeeding at discharge from hospital | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 38.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 38.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 39 Neurodevelopmental, cognitive or developmental outcomes assessed after age 18 months | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 39.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 39.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 40 Return to hospital as in‐ or outpatient because of bleeding (not pre‐specified) Show forest plot | 2 | 2941 | Risk Ratio (M‐H, Random, 95% CI) | 2.21 [1.29, 3.79] |
| 40.1 Higher‐income setting | 2 | 2941 | Risk Ratio (M‐H, Random, 95% CI) | 2.21 [1.29, 3.79] |
| 40.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 41 Postnatal maternal mean Hb (outcome not pre‐specified) Show forest plot | 2 | 2683 | Mean Difference (IV, Random, 95% CI) | 0.5 [0.41, 0.59] |
| 41.1 Higher‐income setting | 2 | 2683 | Mean Difference (IV, Random, 95% CI) | 0.5 [0.41, 0.59] |
| 41.2 Lower‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Severe primary PPH at time of birth (clinically estimated or measured blood loss ≥ 1000 mL) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 1.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 1.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Very severe primary PPH at time of birth (clinically estimated or measured blood loss ≥ 2500 mL) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 3 Maternal mortality | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 3.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 3.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Maternal Hb < 9 g/dL at 24‐72 hr | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 4.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 4.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Admission to neonatal special/intensive care | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 5.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 5.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Neonatal jaundice requiring phototherapy or exchange transfusion | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 6.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 6.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Neonatal polycythaemia treated with dilutional exchange transfusion | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 7.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 7.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Severe primary PPH at time of birth (clinically estimated or measured blood loss ≥ 1000 mL) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 1.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 1.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Very severe primary PPH at time of birth (clinically estimated or measured blood loss ≥ 2500 mL) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 3 Maternal mortality | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 3.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 3.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Maternal Hb < 9 g/dL at 24‐72 hr | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 4.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 4.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Admission to neonatal special/intensive care | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 5.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 5.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Neonatal jaundice requiring phototherapy or exchange transfusion | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 6.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 6.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Neonatal polycythaemia treated with dilutional exchange transfusion | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 7.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 7.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Severe primary PPH at time of birth (clinically estimated or measured blood loss ≥ 1000 mL) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 1.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 1.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Very severe primary PPH at time of birth (clinically estimated or measured blood loss ≥ 2500 mL) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 3 Maternal mortality | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 3.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 3.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Maternal Hb < 9 g/dL at 24‐72 hr | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 4.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 4.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Admission to neonatal special/intensive care | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 5.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 5.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Neonatal jaundice requiring phototherapy or exchange transfusion | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 6.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 6.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Neonatal polycythaemia treated with dilutional exchange transfusion | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 7.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 7.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 8 Maternal blood transfusion Show forest plot | 1 | 654 | Risk Ratio (M‐H, Random, 95% CI) | 0.75 [0.17, 3.32] |
| 8.1 Higher‐income setting | 1 | 654 | Risk Ratio (M‐H, Random, 95% CI) | 0.75 [0.17, 3.32] |
| 8.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 9 Therapeutic uterotonics during third stage and/or within 24 hours Show forest plot | 1 | 654 | Risk Ratio (M‐H, Random, 95% CI) | 0.9 [0.55, 1.48] |
| 9.1 Higher‐income setting | 1 | 654 | Risk Ratio (M‐H, Random, 95% CI) | 0.9 [0.55, 1.48] |
| 9.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 10 Mean length of third stage Show forest plot | 1 | 654 | Mean Difference (IV, Random, 95% CI) | ‐5.15 [‐5.71, ‐4.59] |
| 10.1 Higher‐income setting | 1 | 654 | Mean Difference (IV, Random, 95% CI) | ‐5.15 [‐5.71, ‐4.59] |
| 10.2 Lower‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 11 Manual removal of placenta as defined by study authors Show forest plot | 1 | 654 | Risk Ratio (M‐H, Random, 95% CI) | 0.67 [0.11, 3.96] |
| 11.1 Higher‐income setting | 1 | 654 | Risk Ratio (M‐H, Random, 95% CI) | 0.67 [0.11, 3.96] |
| 11.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 12 Surgical evacuation of retained products of conception Show forest plot | 1 | 654 | Risk Ratio (M‐H, Random, 95% CI) | 7.0 [0.36, 134.98] |
| 12.1 Higher‐income setting | 1 | 654 | Risk Ratio (M‐H, Random, 95% CI) | 7.0 [0.36, 134.98] |
| 12.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 13 Birthweight Show forest plot | 1 | 654 | Mean Difference (IV, Random, 95% CI) | 68.0 [23.87, 112.13] |
| 13.1 Higher‐income setting | 1 | 654 | Mean Difference (IV, Random, 95% CI) | 68.0 [23.87, 112.13] |
| 13.2 Lower‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 14 Postnatal maternal mean Hb Show forest plot | 1 | 654 | Mean Difference (IV, Random, 95% CI) | 0.69 [0.58, 0.80] |
| 14.1 Higher‐income setting | 1 | 654 | Mean Difference (IV, Random, 95% CI) | 0.69 [0.58, 0.80] |
| 14.2 Lower‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Severe primary PPH at time of birth (clinically estimated or measured blood loss ≥ 1000 mL) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 1.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 1.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Very severe primary PPH at time of birth (clinically estimated or measured blood loss ≥ 2500 mL) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 3 Maternal mortality | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 3.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 3.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Maternal Hb < 9 g/dL at 24‐72 hr | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 4.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 4.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Admission to neonatal special/intensive care | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 5.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 5.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Neonatal jaundice requiring phototherapy or exchange transfusion | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 6.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 6.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Neonatal polycythaemia treated with dilutional exchange transfusion | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 7.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 7.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Severe primary PPH at time of birth (clinically estimated or measured blood loss ≥ 1000 mL) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 1.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 1.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Very severe primary PPH at time of birth (clinically estimated or measured blood loss ≥ 2500 mL) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 3 Maternal mortality | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 3.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 3.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Maternal Hb < 9 g/dL at 24‐72 hr | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 4.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 4.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Admission to neonatal special/intensive care | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 5.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 5.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Neonatal jaundice requiring phototherapy or exchange transfusion | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 6.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 6.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Neonatal polycythaemia treated with dilutional exchange transfusion | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 7.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 7.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Severe primary PPH at time of birth (clinically estimated or measured blood loss ≥ 1000 mL) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 1.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 1.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Very severe primary PPH at time of birth (clinically estimated or measured blood loss ≥ 2500 mL) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 3 Maternal mortality | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 3.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 3.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Maternal Hb < 9 g/dL at 24‐72 hr | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 4.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 4.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Admission to neonatal special/intensive care | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 5.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 5.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Neonatal jaundice requiring phototherapy or exchange transfusion | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 6.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 6.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Neonatal polycythaemia treated with dilutional exchange transfusion | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 7.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 7.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Severe primary PPH at time of birth (clinically estimated or measured blood loss ≥ 1000 mL) Show forest plot | 1 | 1648 | Risk Ratio (M‐H, Random, 95% CI) | 0.23 [0.09, 0.55] |
| 1.1 Higher‐income setting | 1 | 1648 | Risk Ratio (M‐H, Random, 95% CI) | 0.23 [0.09, 0.55] |
| 1.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Very severe primary PPH at time of birth (clinically estimated or measured blood loss ≥ 2500 mL) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 3 Maternal mortality | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 3.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 3.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Maternal Hb < 9 g/dL at 24‐72 hr | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 4.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 4.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Admission to neonatal special/intensive care | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 5.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 5.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Neonatal jaundice requiring phototherapy or exchange transfusion | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 6.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 6.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Neonatal polycythaemia treated with dilutional exchange transfusion | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 7.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 7.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 8 Severe primary PPH after placental delivery and up to 24 hours (clinically estimated or measured blood loss ≥ 1000 mL) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 8.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 8.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 9 Severe primary PPH at time of birth and up to 24 hours (clinically estimated or measured blood loss ≥1000 mL) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 9.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 9.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 10 Primary blood loss ≥ 500 mL at time of birth (clinically estimated or measured) Show forest plot | 1 | 1648 | Risk Ratio (M‐H, Random, 95% CI) | 0.53 [0.38, 0.74] |
| 10.1 Higher‐income setting | 1 | 1648 | Risk Ratio (M‐H, Random, 95% CI) | 0.53 [0.38, 0.74] |
| 10.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 11 Primary blood loss ≥ 500 mL after delivery of placenta and up to 24 hours (clinically estimated or measured) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 11.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 11.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 12 Primary blood loss ≥ 500 mL at time of birth and up to 24 hours (clinically estimated or measured) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 12.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 12.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 13 Mean maternal blood loss (mL) at time of birth (clinically estimated or measured) | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 13.1 Higher‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 13.2 Lower‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 14 Mean maternal blood loss (mL) after delivery of placenta and up to 24 hours (clinically estimated or measured) | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 14.1 Higher‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 14.2 Lower‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 15 Mean maternal blood loss (mL) at time of birth and up to 24 hours (clinically estimated or measured) | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 15.1 Higher‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 15.2 Lower‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 16 Maternal blood transfusion Show forest plot | 1 | 1648 | Risk Ratio (M‐H, Random, 95% CI) | 0.25 [0.03, 2.22] |
| 16.1 Higher‐income setting | 1 | 1648 | Risk Ratio (M‐H, Random, 95% CI) | 0.25 [0.03, 2.22] |
| 16.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 17 Clinical signs of severe blood loss Show forest plot | 1 | 1648 | Risk Ratio (M‐H, Random, 95% CI) | 0.25 [0.05, 1.17] |
| 17.1 Higher‐income setting | 1 | 1648 | Risk Ratio (M‐H, Random, 95% CI) | 0.25 [0.05, 1.17] |
| 17.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 18 Therapeutic uterotonics during third stage and/or within 24 hours Show forest plot | 1 | 1648 | Risk Ratio (M‐H, Random, 95% CI) | 0.45 [0.26, 0.77] |
| 18.1 Higher‐income setting | 1 | 1648 | Risk Ratio (M‐H, Random, 95% CI) | 0.45 [0.26, 0.77] |
| 18.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 19 Mean length of third stage Show forest plot | 1 | 1648 | Mean Difference (IV, Random, 95% CI) | ‐10.0 [‐10.24, ‐9.76] |
| 19.1 Higher‐income setting | 1 | 1648 | Mean Difference (IV, Random, 95% CI) | ‐10.0 [‐10.24, ‐9.76] |
| 19.2 Lower‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 20 Manual removal of placenta as defined by study authors | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 20.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 20.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 21 Postnatal diastolic blood pressure > 90 mmHg between birth of baby and discharge from the labour ward | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 21.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 21.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 22 Postnatal vomiting between birth of baby and discharge from the labour ward | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 22.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 22.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 23 Any analgesia between birth of the baby and discharge from labour ward | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 23.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 23.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 24 Women's assessment of pain during third stage as reported by study authors | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 24.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 24.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 25 Secondary blood loss/any vaginal bleeding needing treatment (after 24 hours and up to 6 weeks) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 25.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 25.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 26 Amount of lochia either estimated or measured after 24 hours and up to discharge from hospital | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 26.1 Higher‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 26.2 Lower‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 27 Surgical evacuation of retained products of conception | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 27.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 27.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 28 Afterpains ‐ abdominal pain associated with the contracting uterus in the postpartum period | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 28.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 28.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 29 Apgar score < 7 at 5 minutes | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 29.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 29.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 30 Birthweight | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 30.1 Higher‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 30.2 Lower‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 31 Neonatal encephalopathy assessed using Sarnat staging (Sarnat 1976; Table 1) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 31.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 31.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 32 Neonatal mortality | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 32.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 32.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 33 Intraventricular haemorrhage ‐ Papille grade III/IV ‐ (for infants born before 34 weeks' gestation only) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 33.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 33.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 34 Number of infants who received a red blood cell transfusion | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 34.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 34.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 35 Infant Hb level at 24 to 72 hours | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 35.1 Higher‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 35.2 Lower‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 36 Infant Hb level at 3‐6 months | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 36.1 Higher‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 36.2 Lower‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 37 Infant iron indices (ferritin) at 3 to 6 months | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 37.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 37.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 38 Exclusive breastfeeding at discharge from hospital | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 38.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 38.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 39 Neurodevelopmental, cognitive or developmental outcomes assessed after age 18 months | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 39.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 39.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 40 Return to hospital as in‐ or outpatient because of bleeding (not pre‐specified) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 40.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 40.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 41 Postnatal maternal mean Hb (outcome not pre‐specified) | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 41.1 Higher‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 41.2 Lower‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Severe primary PPH at time of birth (clinically estimated or measured blood loss ≥ 1000 mL) Show forest plot | 1 | 1621 | Risk Ratio (M‐H, Random, 95% CI) | 0.78 [0.48, 1.24] |
| 1.1 Higher‐income setting | 1 | 1621 | Risk Ratio (M‐H, Random, 95% CI) | 0.78 [0.48, 1.24] |
| 1.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Very severe primary PPH at time of birth (clinically estimated or measured blood loss ≥ 2500 mL) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 3 Maternal mortality | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 3.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 3.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Maternal Hb < 9 g/dL at 24‐72 hr Show forest plot | 1 | 1631 | Risk Ratio (M‐H, Random, 95% CI) | 1.23 [0.75, 2.01] |
| 4.1 Higher‐income setting | 1 | 1631 | Risk Ratio (M‐H, Random, 95% CI) | 1.23 [0.75, 2.01] |
| 4.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Admission to neonatal special/intensive care | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 5.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 5.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Neonatal jaundice requiring phototherapy or exchange transfusion | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 6.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 6.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Neonatal polycythaemia treated with dilutional exchange transfusion | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 7.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 7.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 8 Severe primary PPH after placental delivery and up to 24 hours (clinically estimated or measured blood loss ≥ 1000 mL) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 8.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 8.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 9 Severe primary PPH at time of birth and up to 24 hours (clinically estimated or measured blood loss ≥1000 mL) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 9.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 9.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 10 Primary blood loss ≥ 500 mL at time of birth (clinically estimated or measured) Show forest plot | 1 | 1621 | Risk Ratio (M‐H, Random, 95% CI) | 0.51 [0.40, 0.66] |
| 10.1 Higher‐income setting | 1 | 1621 | Risk Ratio (M‐H, Random, 95% CI) | 0.51 [0.40, 0.66] |
| 10.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 11 Primary blood loss ≥ 500 mL after delivery of placenta and up to 24 hours (clinically estimated or measured) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 11.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 11.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 12 Primary blood loss ≥ 500 mL at time of birth and up to 24 hours (clinically estimated or measured) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 12.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 12.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 13 Mean maternal blood loss (mL) at time of birth (clinically estimated or measured) Show forest plot | 1 | 1621 | Mean Difference (IV, Random, 95% CI) | ‐94.0 [‐126.57, ‐61.43] |
| 13.1 Higher‐income setting | 1 | 1621 | Mean Difference (IV, Random, 95% CI) | ‐94.0 [‐126.57, ‐61.43] |
| 13.2 Lower‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 14 Mean maternal blood loss (mL) after delivery of placenta and up to 24 hours (clinically estimated or measured) | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 14.1 Higher‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 14.2 Lower‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 15 Mean maternal blood loss (mL) at time of birth and up to 24 hours (clinically estimated or measured) | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 15.1 Higher‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 15.2 Lower‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 16 Maternal blood transfusion Show forest plot | 1 | 1631 | Risk Ratio (M‐H, Random, 95% CI) | 0.79 [0.43, 1.46] |
| 16.1 Higher‐income setting | 1 | 1631 | Risk Ratio (M‐H, Random, 95% CI) | 0.79 [0.43, 1.46] |
| 16.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 17 Clinical signs of severe blood loss | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 17.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 17.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 18 Therapeutic uterotonics during third stage and/or within 24 hours Show forest plot | 1 | 1631 | Risk Ratio (M‐H, Random, 95% CI) | 0.39 [0.33, 0.48] |
| 18.1 Higher‐income setting | 1 | 1631 | Risk Ratio (M‐H, Random, 95% CI) | 0.39 [0.33, 0.48] |
| 18.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 19 Mean length of third stage Show forest plot | 1 | 1631 | Mean Difference (IV, Random, 95% CI) | ‐1.60 [‐3.08, ‐0.12] |
| 19.1 Higher‐income setting | 1 | 1631 | Mean Difference (IV, Random, 95% CI) | ‐1.60 [‐3.08, ‐0.12] |
| 19.2 Lower‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 20 Manual removal of placenta as defined by study authors Show forest plot | 1 | 1631 | Risk Ratio (M‐H, Random, 95% CI) | 1.25 [0.71, 2.21] |
| 20.1 Higher‐income setting | 1 | 1631 | Risk Ratio (M‐H, Random, 95% CI) | 1.25 [0.71, 2.21] |
| 20.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 21 Postnatal diastolic blood pressure > 90 mmHg between birth of baby and discharge from the labour ward | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 21.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 21.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 22 Postnatal vomiting between birth of baby and discharge from the labour ward | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 22.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 22.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 23 Any analgesia between birth of the baby and discharge from labour ward | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 23.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 23.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 24 Women's assessment of pain during third stage as reported by study authors | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 24.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 24.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 25 Secondary blood loss/any vaginal bleeding needing treatment (after 24 hours and up to 6 weeks) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 25.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 25.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 26 Amount of lochia either estimated or measured after 24 hours and up to discharge from hospital | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 26.1 Higher‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 26.2 Lower‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 27 Surgical evacuation of retained products of conception | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 27.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 27.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 28 Not prespecified: afterpains at 2 hours after birth (id 20458) Show forest plot | 1 | 1425 | Mean Difference (IV, Random, 95% CI) | ‐2.80 [‐4.62, ‐0.98] |
| 28.1 Higher‐income setting | 1 | 1425 | Mean Difference (IV, Random, 95% CI) | ‐2.80 [‐4.62, ‐0.98] |
| 28.2 Lower‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 29 Not pre‐specified: afterpains the day after birth (id 20458) Show forest plot | 1 | 1336 | Mean Difference (IV, Random, 95% CI) | ‐3.0 [‐5.33, ‐0.67] |
| 29.1 Higher‐income setting | 1 | 1336 | Mean Difference (IV, Random, 95% CI) | ‐3.0 [‐5.33, ‐0.67] |
| 29.2 Lower‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 30 Apgar score < 7 at 5 minutes | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 30.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 30.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 31 Birthweight Show forest plot | 1 | 1631 | Mean Difference (IV, Random, 95% CI) | 15.0 [‐28.88, 58.88] |
| 31.1 Higher‐income setting | 1 | 1631 | Mean Difference (IV, Random, 95% CI) | 15.0 [‐28.88, 58.88] |
| 31.2 Lower‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 32 Neonatal encephalopathy assessed using Sarnat staging (Sarnat 1976; Table 1) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 32.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 32.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 33 Neonatal mortality | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 33.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 33.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 34 Intraventricular haemorrhage ‐ Papille grade III/IV ‐ (for infants born before 34 weeks' gestation only) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 34.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 34.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 35 Number of infants who received a red blood cell transfusion. | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 35.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 35.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 36 Infant Hb level at 24 to 72 hours | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 36.1 Higher‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 36.2 Lower‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 37 Infant Hb level at 3‐6 months | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 37.1 Higher‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 37.2 Lower‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 38 Infant iron indices (ferritin) at 3 to 6 months. | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 38.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 38.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 39 Exclusive breastfeeding at discharge from hospital | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 39.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 39.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 40 Neurodevelopmental, cognitive or developmental outcomes assessed after age 18 months | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 40.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 40.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 41 Return to hospital as in‐ or outpatient because of bleeding (not pre‐specified) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 42 Postnatal maternal mean Hb (outcome not pre‐specified) Show forest plot | 1 | 1631 | Mean Difference (IV, Random, 95% CI) | 0.28 [0.14, 0.42] |
| 42.1 Higher‐income setting | 1 | 1631 | Mean Difference (IV, Random, 95% CI) | 0.28 [0.14, 0.42] |
| 42.2 Lower‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 43 Severe primary PPH after placental delivery and up to 2 hours (clinically estimated or measured blood loss ≥ 1000 mL) ‐ not pre‐specified Show forest plot | 1 | 1621 | Risk Ratio (M‐H, Random, 95% CI) | 0.54 [0.39, 0.74] |
| 43.1 Higher‐income setting | 1 | 1621 | Risk Ratio (M‐H, Random, 95% CI) | 0.54 [0.39, 0.74] |
| 43.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 44 Severe primary PPH at time of birth and up to 2 hours (clinically estimated or measured blood loss ≥1000 mL) ‐ not pre‐specified Show forest plot | 1 | 1621 | Risk Ratio (M‐H, Random, 95% CI) | 0.60 [0.47, 0.78] |
| 44.1 Higher‐income setting | 1 | 1621 | Risk Ratio (M‐H, Random, 95% CI) | 0.60 [0.47, 0.78] |
| 44.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 45 Mean blood loss (mL) (clinically estimated or measured at birth and up to 2 hours (not pre‐specified) Show forest plot | 1 | 1621 | Mean Difference (IV, Random, 95% CI) | ‐49.0 [‐75.52, ‐22.48] |
| 45.1 Higher‐income setting | 1 | 1621 | Mean Difference (IV, Random, 95% CI) | ‐49.0 [‐75.52, ‐22.48] |
| 45.2 Lower‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Severe primary PPH at time of birth (clinically estimated or measured blood loss ≥ 1000 mL) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 1.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 1.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Very severe primary PPH at time of birth (clinically estimated or measured blood loss ≥ 2500 mL) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 3 Maternal mortality | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 3.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 3.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Maternal Hb < 9 g/dL at 24‐72 hr Show forest plot | 1 | 130 | Risk Ratio (M‐H, Random, 95% CI) | 0.8 [0.34, 1.90] |
| 4.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 4.2 Lower‐income setting | 1 | 130 | Risk Ratio (M‐H, Random, 95% CI) | 0.8 [0.34, 1.90] |
| 5 Admission to neonatal special/intensive care | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 5.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 5.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Neonatal jaundice requiring phototherapy or exchange transfusion | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 6.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 6.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Neonatal polycythaemia treated with dilutional exchange transfusion | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 7.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 7.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 8 Severe primary PPH after placental delivery and up to 24 hours (clinically estimated or measured blood loss ≥ 1000 mL) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 8.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 8.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 9 Severe primary PPH at time of birth and up to 24 hours (clinically estimated or measured blood loss ≥1000 mL) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 9.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 9.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 10 Primary blood loss ≥ 500 mL at time of birth (clinically estimated or measured) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 10.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 10.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 11 Primary blood loss ≥ 500 mL after delivery of placenta and up to 24 hours (clinically estimated or measured) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 11.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 11.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 12 Primary blood loss ≥ 500 mL at time of birth and up to 24 hours (clinically estimated or measured) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 12.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 12.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 13 Mean maternal blood loss (mL) at time of birth (clinically estimated or measured) | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 13.1 Higher‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 13.2 Lower‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 14 Mean maternal blood loss (mL) after delivery of placenta and up to 24 hours (clinically estimated or measured) | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 14.1 Higher‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 14.2 Lower‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 15 Mean maternal blood loss (mL) at time of birth and up to 24 hours (clinically estimated or measured) | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 15.1 Higher‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 15.2 Lower‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 16 Maternal blood transfusion | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 16.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 16.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 17 Clinical signs of severe blood loss | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 17.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 17.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 18 Therapeutic uterotonics during third stage and/or within 24 hours | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 18.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 18.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 19 Mean length of third stage Show forest plot | 1 | 130 | Mean Difference (IV, Random, 95% CI) | ‐8.12 [‐9.72, ‐6.52] |
| 19.1 Higher‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 19.2 Lower‐income setting | 1 | 130 | Mean Difference (IV, Random, 95% CI) | ‐8.12 [‐9.72, ‐6.52] |
| 20 Manual removal of placenta as defined by study authors Show forest plot | 1 | 130 | Risk Ratio (M‐H, Random, 95% CI) | 1.0 [0.06, 15.65] |
| 20.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 20.2 Lower‐income setting | 1 | 130 | Risk Ratio (M‐H, Random, 95% CI) | 1.0 [0.06, 15.65] |
| 21 Postnatal diastolic blood pressure > 90 mmHg between birth of baby and discharge from the labour ward | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 21.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 21.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 22 Postnatal vomiting between birth of baby and discharge from the labour ward | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 22.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 22.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 23 Any analgesia between birth of the baby and discharge from labour ward | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 23.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 23.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 24 Women's assessment of pain during third stage as reported by study authors | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 24.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 24.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 25 Secondary blood loss/any vaginal bleeding needing treatment (after 24 hours and up to 6 weeks) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 25.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 25.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 26 Amount of lochia either estimated or measured after 24 hours and up to discharge from hospital | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 26.1 Higher‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 26.2 Lower‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 27 Surgical evacuation of retained products of conception | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 27.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 27.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 28 Afterpains ‐ abdominal pain associated with the contracting uterus in the postpartum period | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 28.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 28.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 29 Apgar score < 7 at 5 minutes | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 29.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 29.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 30 Birthweight | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 30.1 Higher‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 30.2 Lower‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 31 Neonatal encephalopathy assessed using Sarnat staging (Sarnat 1976; Table 1) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 31.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 31.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 32 Neonatal mortality | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 32.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 32.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 33 Intraventricular haemorrhage ‐ Papille grade III/IV ‐ (for infants born before 34 weeks' gestation only) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 33.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 33.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 34 Number of infants who received a red blood cell transfusion | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 34.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 34.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 35 Infant Hb level at 24 to 72 hours | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 35.1 Higher‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 35.2 Lower‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 36 Infant Hb level at 3‐6 months | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 36.1 Higher‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 36.2 Lower‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 37 Infant iron indices (ferritin) at 3 to 6 months. | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 37.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 37.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 38 Exclusive breastfeeding at discharge from hospital | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 38.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 38.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 39 Neurodevelopmental, cognitive or developmental outcomes assessed after age 18 months | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 39.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 39.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 40 Return to hospital as in‐ or outpatient because of bleeding (not pre‐specified) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 40.1 Higher‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 40.2 Lower‐income setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 41 Postnatal maternal mean Hb (outcome not pre‐specified) | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 41.1 Higher‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 41.2 Lower‐income setting | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |

