Radioterapia coadyuvante posterior a la prostatectomía radical para el cáncer de próstata
Información
- DOI:
- https://doi.org/10.1002/14651858.CD007234.pub2Copiar DOI
- Base de datos:
-
- Cochrane Database of Systematic Reviews
- Versión publicada:
-
- 07 diciembre 2011see what's new
- Tipo:
-
- Intervention
- Etapa:
-
- Review
- Grupo Editorial Cochrane:
-
Grupo Cochrane de Urología
- Copyright:
-
- Copyright © 2011 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Cifras del artículo
Altmetric:
Citado por:
Autores
Contributions of authors
TD wrote the protocol, reviewed results of search and abstracts, extracted and checked data and 'Risk of bias' tables, co‐wrote the discussion and edited review.
BH edited protocol, reviewed results of search and abstracts, extracted and checked data, constructed Risk of bias tables, entered data into RevMan, analysed data, co‐wrote and edited discussion.
ML edited protocol, reviewed results of search and abstracts, edited review.
Sources of support
Internal sources
-
Princess Alexandra Cancer Collaborative Group, Australia.
External sources
-
No sources of support supplied
Declarations of interest
None.
Acknowledgements
Princess Alexandra Cancer Collaborative Group
Version history
| Published | Title | Stage | Authors | Version |
| 2011 Dec 07 | Adjuvant radiotherapy following radical prostatectomy for prostate cancer | Review | Tiffany Daly, Brigid E Hickey, Margot Lehman, Daniel P Francis, Adrienne M See | |
| 2008 Jul 16 | Adjuvant radiotherapy following radical prostatectomy for prostate cancer | Protocol | Tiffany Daly, Brigid E Hickey, Margot Lehman, Daniel P Francis | |
Differences between protocol and review
We reported risk difference not odds ratio as we proposed to do in the protocol (based on peer reviewer's recommendation).
Keywords
MeSH
Medical Subject Headings (MeSH) Keywords
Medical Subject Headings Check Words
Humans; Male;

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Comparison 1 Adjuvant RT versus nil postprostatectomy, Outcome 1 Overall survival.
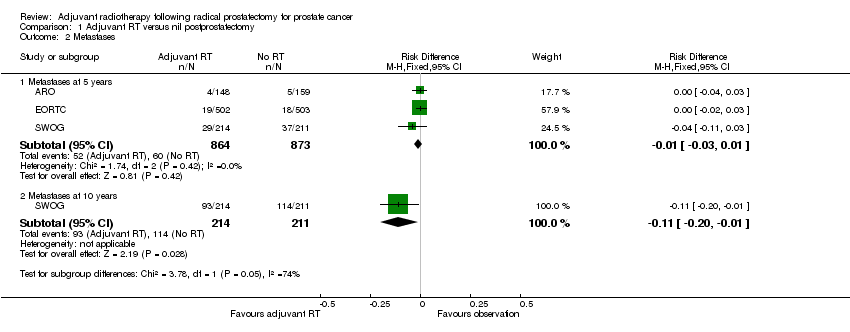
Comparison 1 Adjuvant RT versus nil postprostatectomy, Outcome 2 Metastases.
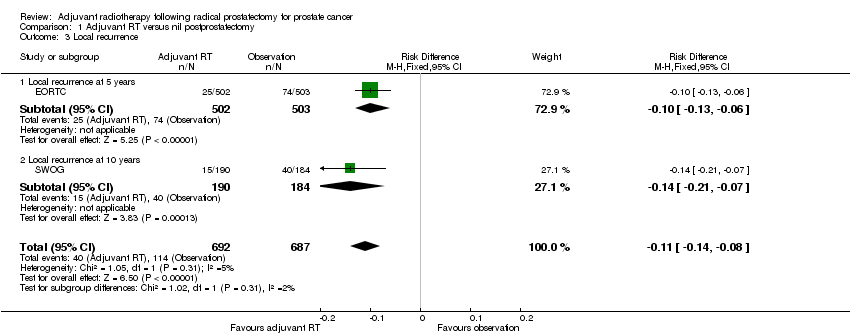
Comparison 1 Adjuvant RT versus nil postprostatectomy, Outcome 3 Local recurrence.
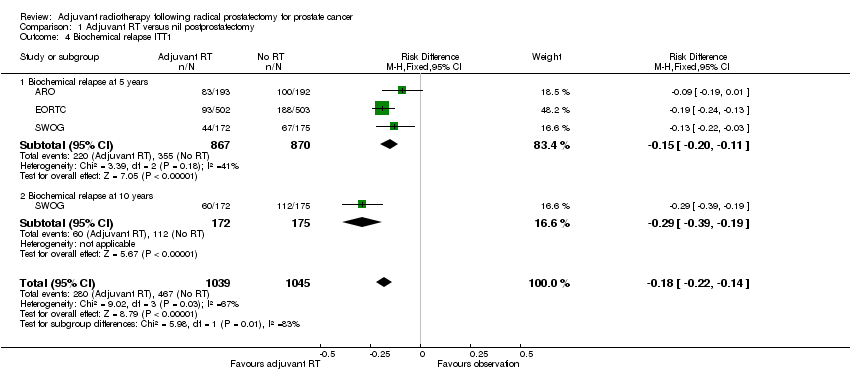
Comparison 1 Adjuvant RT versus nil postprostatectomy, Outcome 4 Biochemical relapse ITT1.

Comparison 1 Adjuvant RT versus nil postprostatectomy, Outcome 5 Urethral stricture.
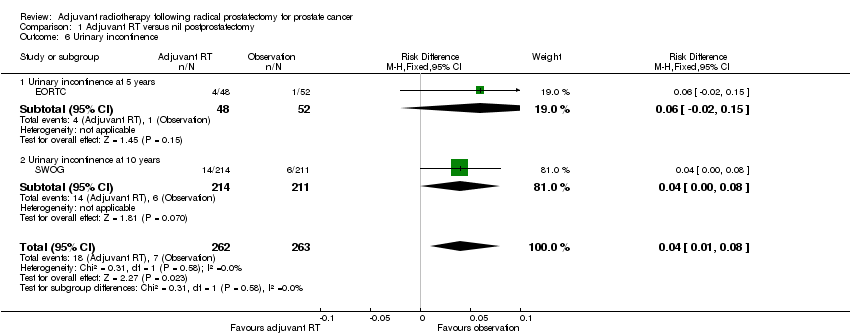
Comparison 1 Adjuvant RT versus nil postprostatectomy, Outcome 6 Urinary incontinence.

Comparison 1 Adjuvant RT versus nil postprostatectomy, Outcome 7 Prostate cancer specific survival.
| Grade | Definition |
| 0 | dry < 1 gm (gram) no pads |
| 1 | minimal 1 to 9 gm 1 to 4 pads (humid) |
| 2 | moderate 10 to 50 gm 1 to 4 pads (soaked) |
| 3 | severe > 50 gm with > 4 pads |
| 0 | 1 | 2 | 3 | 4 | |
| Symptom | None | Slight | Moderate | Severe frequency and dysuria; | Necrosis/Contracted |
| Symptom | Scale |
| Tenderness and urgency with bowel movements |
|
| Urinary frequency |
|
| Erectile dysfunction |
|
| Global HQRL: rating of how life is affected by the state of your health |
|
| Study | Definition of nadir |
| ARO | postoperative PSA < 0.1ng/dL |
| EORTC | PSA < 0.2 ng/dL |
| SWOG | PSA ≤ 0.4 ng/dL |
| Study | Number of men who did not nadir |
| ARO | 78/388 (20%) |
| EORTC | 108/1005 (10%) |
| SWOG | 127/376 (33%) did not achieve PSA ≤ 0.2 ng/dL 29/376 (7%) of men did not achieve PSA ≤ 0.4ng/dL (which is the definition they used for nadir) NB: only had PSA information for 376/425 men postoperatively |
| Grade | Symptoms |
| 0 | No change from baseline |
| 1 | urinary frequency and nocturia 2 times pretreatment habit, urgency, no medications |
| 2 | frequency, urgency and nocturia, medications required |
| 3 | frequency urgency and nocturia with spasms and frequent medications required |
| 4 | Haematuria requiring transfusion, acute bladder obstruction ulceration/necrosis |
| 5 | Death secondary to radiation side effects |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Overall survival Show forest plot | 3 | Risk Difference (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 Overall survival at 5 years | 3 | 1737 | Risk Difference (M‐H, Fixed, 95% CI) | ‐0.00 [‐0.03, 0.02] |
| 1.2 Overall survival at 10 years | 1 | 425 | Risk Difference (M‐H, Fixed, 95% CI) | ‐0.11 [‐0.20, ‐0.02] |
| 2 Metastases Show forest plot | 3 | Risk Difference (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 Metastases at 5 years | 3 | 1737 | Risk Difference (M‐H, Fixed, 95% CI) | ‐0.01 [‐0.03, 0.01] |
| 2.2 Metastases at 10 years | 1 | 425 | Risk Difference (M‐H, Fixed, 95% CI) | ‐0.11 [‐0.20, ‐0.01] |
| 3 Local recurrence Show forest plot | 2 | 1379 | Risk Difference (M‐H, Fixed, 95% CI) | ‐0.11 [‐0.14, ‐0.08] |
| 3.1 Local recurrence at 5 years | 1 | 1005 | Risk Difference (M‐H, Fixed, 95% CI) | ‐0.10 [‐0.13, ‐0.06] |
| 3.2 Local recurrence at 10 years | 1 | 374 | Risk Difference (M‐H, Fixed, 95% CI) | ‐0.14 [‐0.21, ‐0.07] |
| 4 Biochemical relapse ITT1 Show forest plot | 3 | 2084 | Risk Difference (M‐H, Fixed, 95% CI) | ‐0.18 [‐0.22, ‐0.14] |
| 4.1 Biochemical relapse at 5 years | 3 | 1737 | Risk Difference (M‐H, Fixed, 95% CI) | ‐0.15 [‐0.20, ‐0.11] |
| 4.2 Biochemical relapse at 10 years | 1 | 347 | Risk Difference (M‐H, Fixed, 95% CI) | ‐0.29 [‐0.39, ‐0.19] |
| 5 Urethral stricture Show forest plot | 2 | Risk Difference (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5.1 Urethral stricture at 5 years | 1 | 307 | Risk Difference (M‐H, Fixed, 95% CI) | 0.01 [‐0.02, 0.03] |
| 5.2 Urethral stricture at 10 years | 1 | 425 | Risk Difference (M‐H, Fixed, 95% CI) | 0.08 [0.02, 0.15] |
| 6 Urinary incontinence Show forest plot | 2 | 525 | Risk Difference (M‐H, Fixed, 95% CI) | 0.04 [0.01, 0.08] |
| 6.1 Urinary incontinence at 5 years | 1 | 100 | Risk Difference (M‐H, Fixed, 95% CI) | 0.06 [‐0.02, 0.15] |
| 6.2 Urinary incontinence at 10 years | 1 | 425 | Risk Difference (M‐H, Fixed, 95% CI) | 0.04 [‐0.00, 0.08] |
| 7 Prostate cancer specific survival Show forest plot | 1 | 1005 | Risk Difference (M‐H, Fixed, 95% CI) | ‐0.01 [‐0.03, 0.00] |

