Exposición quirúrgica abierta versus cerrada de dientes caninos desplazados hacia el techo de la boca
Resumen
Antecedentes
Los caninos desplazados hacia el paladar o CDP son los caninos superiores permanentes, comúnmente conocidos como “colmillos”, que se desplazan hacia el techo de la boca. Este trastorno puede dejar espacios desagradables, causar daño a las raíces circundantes (que puede ser tan severo como para causar la pérdida de los dientes vecinos o su extracción) y, ocasionalmente, dar lugar al desarrollo de quistes. Los CDP son una anomalía dental frecuente, presente en un 2% a un 3% de los jóvenes.
El tratamiento de este trastorno es costoso y requiere tiempo para su realización. Incluye la exposición quirúrgica (descubrimiento) seguida de ortodoncias fijas durante dos a tres años para alinear el canino dentro del arco dental. En el Reino Unido se utilizan habitualmente dos técnicas para exponer los caninos palatinos: la técnica cerrada y la técnica abierta. Mediante la técnica cerrada se deja el canino al descubierto, se acopla un ojalillo y una cadena de oro y luego se sutura la mucosa palatina nuevamente por encima del diente. Luego se coloca el diente en su posición cubierto por la mucosa palatina. En la técnica abierta se deja el diente canino al descubierto y se extrae el tejido palatino suprayacente para dejarlo descubierto. El ortodoncista luego puede ver la corona del canino para alinearlo.
Objetivos
Evaluar los efectos del uso del método quirúrgico abierto o cerrado para exponer los caninos que han sido desplazados hacia el techo de la boca, en cuanto al éxito y otros resultados clínicos e informados por los pacientes.
Métodos de búsqueda
El especialista en información del Grupo Cochrane de Salud Oral (Cochrane Oral Health's Information Specialist) buscó en las siguientes bases de datos: Registro de Ensayos del Grupo Cochrane de Salud Oral (Cochrane Oral Health Group) (hasta el 24 febrero 2017), Registro Cochrane Central de Ensayos Controlados (Cochrane Central Register of Controlled Trials) (CENTRAL) (en la Cochrane Library, 2017, número 1), MEDLINE Ovid (1946 hasta 24 febrero 2017), y en Embase Ovid (1980 hasta 24 febrero 2017). Se hicieron búsquedas de ensayos en curso en el US National Institutes of Health Ongoing Trials Register (ClinicalTrials.gov) y en la World Health Organization International Clinical Trials Registry Platform. No se impusieron restricciones de idiomani de fecha de publicación en la búsqueda en las bases de datos electrónicas.
Criterios de selección
Se incluyeron ensayos controlados aleatorios y cuasialeatorios que evaluaban a jóvenes sometidos al tratamiento quirúrgico para corregir los CDP superiores. No hubo limitación con respecto a la edad, la presencia de maloclusión ni el tipo de tratamiento ortodóntico activo realizado. Se incluyeron caninos desplazados de forma unilateral y bilateral.
Obtención y análisis de los datos
Dos autores de la revisión, de forma independiente, examinaron los resultados de las búsquedas electrónicas, extrajeron los datos y evaluaron el riesgo de sesgo de los estudios incluidos. Cuando fue posible, se intentó establecer contacto con los autores de los estudios para obtener los datos faltantes o aclaraciones. Para la síntesis de los datos, se siguieron las orientaciones del Manual Cochrane de Revisiones Sistemáticas de Intervenciones.
Resultados principales
Se incluyeron tres estudios con 146 participantes. Dos estudios fueron evaluados como de alto riesgo de sesgo.
El resultado principal de la revisión fue que las dos técnicas pueden ser igualmente exitosas para exponer los CDP (cociente de riesgos [CR] 0,99; intervalo de confianza [IC] del 95%: 0,93 a 1,06; tres estudios, 141 participantes analizados, evidencia de baja calidad).
Un fracaso quirúrgico se debió al desprendimiento de la cadena de oro (grupo de procedimiento cerrado). Un estudio informó las complicaciones posteriores a la intervención quirúrgica y encontró dos en el grupo de procedimiento cerrado: una infección postoperatoria que requirió antibióticos y dolor durante la alineación del canino a medida que la cadena de oro penetraba a través del tejido de la encía del paladar.
No fue posible agrupar los datos sobre la estética dental, el dolor y el malestar informados por el paciente, la salud periodóntica ni el periodo de tratamiento; sin embargo, los estudios individuales no encontraron diferencias entre las técnicas quirúrgicas (evidencia de calidad baja a muy baja).
Conclusiones de los autores
Actualmente, la evidencia indica que ni la técnica quirúrgica abierta ni la cerrada para exponer los dientes caninos maxilares desplazados hacia el paladar es superior para ninguno de los resultados incluidos en esta revisión; sin embargo, la evidencia se consideró de baja calidad debido a que dos de los tres estudios incluidos estuvieron en riesgo alto de sesgo. Esto sugiere la necesidad de más estudios de alta calidad. Se han identificado tres ensayos clínicos en curso y se espera que los mismos produzcan datos que puedan agruparse para aumentar el grado de certidumbre en estos hallazgos.
PICOs
Resumen en términos sencillos
Exposición quirúrgica abierta versus cerrada de dientes caninos desplazados hacia el techo de la boca
Pregunta de la revisión
¿Es mejor usar un método quirúrgico abierto o cerrado para exponer los caninos (“colmillos”) que se han desplazado hacia el techo de la boca?
Antecedentes
Los dientes caninos permanentes de la mandíbula superior erupcionan generalmente en la boca entre los 11 a 12 años de edad. En un 2% a un 3% de los jóvenes, los dientes caninos no logran erupcionar (crecen hacia abajo) y se desplazan hacia techo de la boca (paladar). Este trastorno puede dejar espacios desagradables, causar daño a las raíces circundantes (que pueden ser graves y causar la pérdida de los dientes vecinos o su extracción) y, ocasionalmente, dar lugar al desarrollo de quistes.
El tratamiento de este trastorno es costoso y requiere tiempo para su realización. Generalmente incluye la exposición quirúrgica (descubrimiento), seguida de aparatos ortodónticos fijos durante dos a tres años, para mover el canino a la posición correcta. En el Reino Unido se utilizan sistemáticamente dos técnicas quirúrgicas: la técnica cerrada implica el descubrimiento quirúrgico del diente, pegar un anexo en el diente expuesto y reubicar el colgajo palatino. Poco después de la cirugía, se utiliza un aparato ortodóntico para aplicar fuerzas suaves y traer al canino hacia su posición correcta dentro del arco dental. El canino se mueve hacia su posición por debajo de la encía. Un método alternativo es la técnica abierta, que incluye el descubrimiento quirúrgico del diente canino como se mencionó antes, aunque en vez de colocar un anexo sobre el diente expuesto, se extrae una ventana de la encía de alrededor del diente y se coloca un apósito (empaquetamiento) para cubrir el área expuesta. Cerca de diez días después, se extrae este empaquetamiento y se permite que el canino erupcione naturalmente. Una vez que el diente ha erupcionado lo suficiente para pegar un anexo ortodóntico sobre su superficie, se utilizan aparatos ortodónticos para alinear el diente con los otros dientes.
Características de los estudios
La evidencia en esta revisión está actualizada hasta febrero 2017. Los autores de Salud Bucodental Cochrane encontraron tres estudios relevantes, que incluían a 146 participantes con colmillos desplazados hacia el techo de la boca, en uno o ambos lados. La mayoría de los participantes eran mujeres y la edad promedio en los estudios varió de 14 a 17 años. Dos estudios estaban diseñados de una manera que probablemente les adjudicaba sesgo.
Resultados clave
Se combinaron los resultados de tres estudios y se encontró que una técnica no pareció tener una ventaja sobre la otra para asegurar el movimiento del diente a la posición correcta sin la necesidad de una intervención quirúrgica repetida.
Cinco de cada 141 participantes analizados fueron fracasos quirúrgicos, uno de los cuales se debió a la complicación del desprendimiento de la cadena de oro durante la intervención quirúrgica. Un estudio informó las complicaciones después de la intervención quirúrgica y encontró que un participante del grupo cerrado tuvo una infección postoperatoria que requirió antibióticos y que otro participante del grupo cerrado presentó dolor durante la alineación del canino a medida que la cadena de oro penetraba a través del tejido de la encía del paladar.
No fue posible combinar los resultados de los estudios para otros resultados, aunque los estudios individuales no mostraron evidencia de una diferencia entre las dos técnicas para el dolor, el malestar, la apariencia, la salud de las encías, la duración del periodo de tratamiento ni el costo (evidencia de calidad baja a muy baja).
Calidad de la evidencia
En términos generales, la calidad de la evidencia se evaluó como baja, que significa que no es posible tener seguridad en cuanto a los hallazgos.
Conclusiones de los autores
No parece que una técnica quirúrgica sea mejor que la otra para mover los colmillos desplazados a la posición correcta, ni para otros resultados, aunque este hallazgo es incierto debido a que la calidad de la evidencia es baja. Esto sugiere la necesidad de más estudios de alta calidad. Actualmente se están llevando a cabo tres estudios. Cuando estén completos, se incluirán en una actualización de esta revisión y se podrá llegar a conclusiones más firmes.
Authors' conclusions
Summary of findings
| Open surgical technique compared with closed surgical technique for palatally impacted canines | ||||||
| Patient or population: people with maxillary palatally impacted canines Settings: oral surgery departments Intervention: open surgical technique Comparison: closed surgical technique | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Closed surgery | Open surgery | |||||
| Success of surgery | 943 per 1000 | 934 per 1000 | RR 0.99 (0.93 to 1.06) | 141 | ⊕⊕⊝⊝ | The available evidence suggests that there is no difference in the success of surgery between the techniques and that both techniques have a high success rate. |
| Complications | One surgical failure was due to detachment of the gold chain (closed group). One study reported two complications following surgery, both in the closed group: a post‐operative infection requiring antibiotics and pain during alignment of the canine as the gold chain penetrated through the gum tissue of the palate. | |||||
| Aesthetics (reported in various manners at different time points) | This outcome was measured in a variety of ways in the studies that cannot be pooled. | ⊕⊝⊝⊝ | This outcome is subjective and can be measured and reported in many different ways. The current evidence suggests that there is no difference in aesthetic outcomes between the groups. | |||
| Patient response (pain and discomfort reported in different ways between 1 to 10 days postoperatively) | This outcome was measured in a variety of ways in the studies that cannot be pooled. | ⊕⊝⊝⊝ | This outcome is subjective and was measured and reported in different ways. The current evidence suggests that there is no difference in patient response outcomes between the groups. | |||
| Gum health (clinical attachment level (CAL); 3 months post‐debond) | Mean CAL in the closed group | Mean CAL in the intervention groups was 0.1 mm lower | 62 | ⊕⊕⊝⊝ | This outcome was measured and reported in different ways in different studies. The current evidence suggests that there is no difference in periodontal outcomes between the groups. | |
| Treatment time (length of time in operating theatre from first incision to final suture) | Mean of the closed group was 34.3 minutes in Parkin 2012; and 37.7 minutes in Gharaibeh 2008. | Mean of the open group was 3.18 minutes less (7.59 minutes less to 1.22 minutes more) | 89 (2 studies) | ⊕⊝⊝⊝ | The current evidence suggests that there is no difference in length of time in surgery between the groups. | |
| *The basis for the assumed risk is the Parkin 2012 closed group. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded one level due to high risk of bias in two studies. Downgraded one level as two studies had no failures. 2 Downgraded one level due to high risk of bias in one study. Downgraded one level as each outcome only reported by single studies. Downgraded one level as studies with few participants and large confidence intervals for some outcomes. 3 Downgraded two levels due to high risk of bias in two studies and subjective participant‐reported outcome with no blinding. Downgraded one level as each outcome only reported by single studies. 4 Downgraded two levels as single small study at high risk of bias. 5 Downgraded one level due to high risk of bias in one study. Downgraded one level as substantial heterogeneity between results. Downgraded one level as studies with few participants and large confidence intervals for some outcomes. | ||||||
Background
Description of the condition
Maxillary canine teeth are the third teeth along from the midline in the upper jaw, which erupt into the mouth around 11 to 12 years of age (Hagg 1986). Displaced teeth refers to those which have an abnormal position, whereas impacted teeth are those which cannot naturally erupt, usually because they are impeded by other teeth or bone. After mandibular (lower jaw) third molars or wisdom teeth, maxillary canines are the most common teeth to be displaced or impacted (Thilander 1973). Canine displacement usually occurs in the roof of the mouth (palate), whereas impaction usually occurs towards the cheek and lip (buccally) or in line with the arch (Counihan 2013). Canine teeth, which are displaced in the palate and cannot erupt naturally, are referred to as ‘palatally displaced canines’ or PDCs. Prevalence of PDCs has been reported as between 1% to 3% in different populations. It has been reported that in around 8% of these cases teeth on both sides of the mouth (bilateral) are affected (Bishara 1992; Peck 1994). The male to female ratio of maxillary canine displacement varies between studies conducted in different populations. In one study conducted in Italy, palatally displaced canines occurred three times more frequently in females than males (Sacerdoti 2004), whereas Bishara reports that displacements are twice as common in females than in males (Bishara 1992).
The aetiology of PDCs is not fully understood, but is considered multifactorial. Many studies have claimed that they are mainly inherited, with a polygenic mode of inheritance. Family studies have shown that positional abnormalities of canines are more common in relatives than the general population (Peck 1994; Peck 1996; Peck 1997). Local factors may also be a causative factor in displacement, such as missing or small incisor teeth, crowding or a lack of space in the jaw, delayed or early shedding of the primary tooth, presence of cleft in the jaw, fusion of the tooth to the bone (ankylosis) and trauma to other teeth in the area (Bishara 1992).
Displaced maxillary canines can result in several complications, such as root resorption of adjacent teeth (usually the maxillary lateral and sometimes central incisors (Strbac 2013)), and much more rarely, cystic change of the tissue around the displaced tooth (Manne 2012). Root resorption may become so severe that the neighbouring teeth have to be removed. Also, impaction of these teeth can lead to aesthetic problems (Shafer 1983), owing to a gap in the dental arch where the tooth has failed to erupt. This can lead to an abnormal position of the upper dental midline. Due to the potential severe sequelae, some displaced or impacted canines cannot be left alone and require surgical intervention.
Description of the intervention
With every patient, a careful discussion between the patient, parent/caregiver, orthodontist and oral surgeon is required. However, the preferred option for many PDCs is surgical exposure under general anaesthesia (or, in some countries, local anaesthetic) and orthodontic alignment. At present, two surgical techniques are routinely used to uncover palatally displaced canines: the open and closed techniques.
The closed technique involves surgically uncovering the tooth and gluing an attachment onto the exposed tooth, often in the form of a gold chain. The palatal flap is then repositioned and sutured, with the chain exiting through the mucosa. Historically, this could be seen as quite challenging in the surgical theatre setting; however, with the advent of new self‐etch adhesive bonding systems, the bonding technique could be simplified. Shortly after surgery, an orthodontic brace is used to apply gentle forces to bring the canine into its correct position, within the dental arch. The canine then erupts through the mucosa into its correct position (Clark 1971). See Figure 1.

Open technique
The open technique differs slightly. It involves surgically uncovering the canine tooth, as before, but instead of bonding an attachment on the exposed tooth at the time of the surgery, a window of tissue is removed from around the tooth leaving it exposed. A dressing or 'pack' is placed to cover the exposed area. The dressing is removed approximately 10 days later. The tooth is then either left to erupt naturally, or an orthodontic attachment is placed to enable the tooth to be moved, above the gum, into its correct position in line with the rest of the teeth (Lewis 1971). See Figure 2.

Closed technique
Regardless of which surgical technique is used, orthodontic treatment will be required following surgical exposure, in order to bring the canine tooth into its correct position. On average, this will take between two and three years.
How the intervention might work
Surgical exposure involves removing the bone or fibrous gum tissue (or both) that is impeding the movement of the canine. Without doing this, the tooth is unlikely to erupt. Exposing the canine tooth surgically allows access to the tooth to either allow natural eruption or orthodontic movement. Once sufficiently erupted, then the tooth can be brought into alignment with the rest of the teeth, using orthodontics.
Why it is important to do this review
Palatally impacted canines are a commonly encountered clinical problem that primarily affects children and adolescents. Up till now, there has been a lack of high‐quality research to assess the advantages of one technique over the other. Whilst considering patient factors, the choice of technique is currently determined by the orthodontists’ and surgeons’ preference. A survey to investigate the preference of orthodontists in the UK was equally divided between the two techniques (Clark 1994).
Several studies have evaluated treatment length, periodontal health, root length and aesthetics, while few have looked at the patient’s perception of recovery and other outcomes most important to the patient. As treatment is long and is being received at a young age, it is important to find out whether one surgical technique will result in better outcomes for the patient in terms of success and treatment burden.
Objectives
To assess the effects of using either an open or closed surgical method to expose canines that have become displaced in the roof of the mouth, in terms of success and other clinical and patient‐reported outcomes.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised or quasi‐randomised controlled clinical trials in which palatally impacted canines are surgically exposed and subsequently aligned using orthodontic treatment.
Types of participants
People receiving surgical treatment to correct maxillary palatally impacted canines. There is no restriction for age, presenting malocclusion or the type of active orthodontic treatment undertaken. We included unilaterally and bilaterally displaced canines.
We excluded trials including participants with craniofacial deformity/syndrome.
Types of interventions
-
Surgical exposure of palatally impacted canines with an open surgical technique.
-
Surgical exposure of palatally impacted canines with a closed surgical technique.
Types of outcome measures
Our main focus of the outcomes for this review was to look at outcomes most important to the patient. We looked at differences between the 'open' and 'closed' groups.
Primary outcomes
-
Success of surgery, defined as eruption of the canine crown, sufficient to allow for orthodontic alignment, without the need for repeated surgery.
-
Complications or adverse effects.
-
Aesthetics of the treated canine compared to the untreated contra‐lateral canine.
Secondary outcomes
-
Patient‐reported outcomes, including pain/discomfort reported soon after surgery and also patient satisfaction after orthodontic treatment.
-
Gum health recorded at a minimum of three months after fixed appliance removal, as measured by: loss of attachment of the gum from around the tooth, bleeding on probing, recession of the gum margin and crestal bone height.
-
Treatment time measured by, for example, length of time in theatre, duration of orthodontic treatment and number of orthodontic appointments. This will have a cost implication and differences in cost can also be measured.
Search methods for identification of studies
Electronic searches
Cochrane Oral Health’s Information Specialist conducted systematic searches in the following databases for randomised controlled trials and controlled clinical trials. There were no language, publication year or publication status restrictions.
-
Cochrane Oral Health’s Trials Register (searched 24 February 2017) (Appendix 1);
-
Cochrane Central Register of Controlled Trials (CENTRAL; 2017, Issue 1) in the Cochrane Library (searched 24 February 2017) (Appendix 2);
-
MEDLINE Ovid (1946 to 24 February 2017) (Appendix 3);
-
Embase Ovid (1980 to 24 February 2017) (Appendix 4).
Subject strategies were modelled on the search strategy designed for MEDLINE Ovid.
Searching other resources
We searched the following trial registries for ongoing studies.
-
US National Institutes of Health Ongoing Trials Register ClinicalTrials.gov (clinicaltrials.gov; searched 24 February 2017) (Appendix 5);
-
World Health Organization International Clinical Trials Registry Platform (apps.who.int/trialsearch; searched 24 February 2017) (Appendix 6).
We searched the reference lists of included studies and relevant systematic reviews for further studies.
We did not perform a separate search for adverse effects of interventions. We considered adverse effects described in included studies only.
Data collection and analysis
Selection of studies
For this updated review, two review authors (IK and SG), independently screened the titles and abstracts (when available) of all reports identified through the electronic search update. The title, keywords and abstract were examined for the following criteria.
-
Is it a randomised or quasi‐randomised trial?
-
Does it involve the surgical exposure of palatally impacted canine(s)?
-
Does it directly compare the closed versus the open surgical technique?
We obtained the full report for all studies that appeared to meet the inclusion criteria, or for which there were insufficient data in the title and abstract to make a clear decision. Two review authors independently assessed the full reports to establish whether or not the studies met the inclusion criteria. If in the opinion of both authors an article clearly did not fulfil the defined inclusion criteria, it was considered ineligible. We resolved disagreements by discussion. Where resolution was not possible, we consulted a member of the Cochrane Oral Health editorial team. We recorded studies rejected at this or subsequent stages in the Characteristics of excluded studies table, with the reasons for exclusion.
Data extraction and management
For this update, two review authors (IK and SG) independently performed data extraction. All studies meeting the inclusion criteria underwent data extraction and a risk of bias assessment, using a pre‐standardised data extraction form. We resolved any disagreements through discussion. If it was not possible to come to a resolution, we consulted an experienced member of the Cochrane Oral Health editorial team to achieve consensus.
We recorded the following data for each included study, which was tabulated in the Characteristics of included studies table.
-
Year of publication, country of origin, study design, number of centres, study duration.
-
Details of the participants, including the inclusion/exclusion criteria, age at baseline, other prognostic factors, gender ratios, numbers randomised to each treatment group and numbers analysed.
-
Details of how the surgical technique was performed for each group and any additional measures which were carried out.
-
Details of outcomes reported, including method of assessment and time intervals.
-
Any additional features to note, such as any sample size calculation, adverse effects, source of study funding or other declarations/conflicts of interest reported.
We contacted authors to provide missing details where possible.
Assessment of risk of bias in included studies
For this update, two review authors (IK and SG) independently assessed the risk of bias of each included study using the Cochrane domain‐based, two‐part tool, as described in Chapter 8 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We contacted study authors for clarification of missing information where necessary and feasible. We resolved any disagreements through discussion. If we were unable to come to a resolution, we consulted an experienced member of the Cochrane Oral Health editorial team to achieve consensus.
We completed a 'Risk of bias' table for each included study. For each domain, we first described what was reported to have happened in the study. This provided the rationale for our judgement of whether that domain was at low, high, or unclear risk of bias.
We assessed each included study to the following domains.
-
Sequence generation (selection bias).
-
Allocation concealment (selection bias).
-
Blinding of participants and personnel (performance bias).
-
Blinding of outcome assessment (detection bias).
-
Incomplete outcome data (attrition bias).
-
Selective outcome reporting (reporting bias).
-
Other bias.
We categorised the overall risk of bias of individual studies as being at low, high, or unclear risk of bias according to the following criteria.
-
Low risk of bias (plausible bias unlikely to seriously alter the results) if all domains were at low risk of bias.
-
High risk of bias (plausible bias that seriously weakens confidence in the results) if one or more domains were at high risk of bias.
-
Unclear risk of bias (plausible bias that raises some doubt about the results) if one or more domains were at unclear risk of bias.
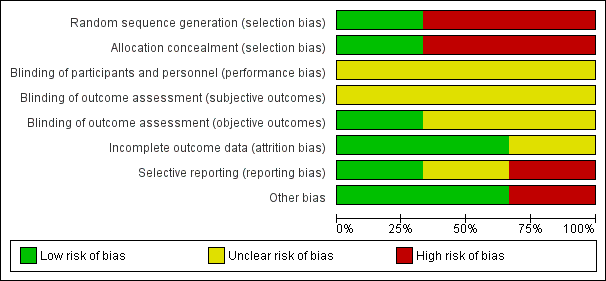
The 'Risk of bias' summary was presented graphically (Figure 3; Figure 4).

Risk of bias summary: review authors' judgements about each risk of bias item for each included study
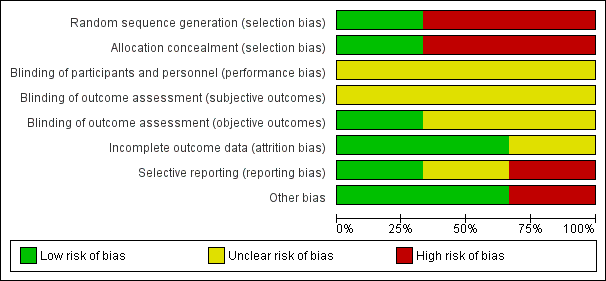
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies
Measures of treatment effect
For continuous outcomes (e.g. pain on a visual analogue scale) where studies used the same scale, we used the mean values and standard deviations (SDs) reported in the studies in order to express the estimate of effect as mean difference (MD) with 95% confidence interval (CI). Where different scales were used, we would have considered expressing the treatment effect as a standardised mean difference (SMD) with 95% CI. For dichotomous outcomes (e.g. success of surgery), we expressed the estimate of the intervention effect as a risk ratio (RR) with 95% CI.
Where possible, we pooled data from studies to give an overall estimate of the intervention effect. This was only undertaken if there were sufficient similarities between the studies. If it was not possible to carry out a meta‐analysis, then a narrative description was provided for that outcome.
Unit of analysis issues
The participant was the unit of analysis. If two teeth within one individual participant were treated differently, then this was taken into account in the analysis. The analysis of intra‐individual trials followed the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011).
Dealing with missing data
Where outcome data were missing from the published report, or could not be calculated from the information presented in the report, we attempted, where feasible, to contact the author(s) of studies to obtain the missing data or for clarification. The analyses generally included only the available data (ignoring missing data). If the number of participants was not reported, we did not include outcome data in the analyses.
Where standard deviations were missing, we used methods described in the Cochrane Handbook for Systematic Reviews of Interventions to calculate them.
Assessment of heterogeneity
If meta‐analyses were performed, we assessed the possible presence of heterogeneity by visually inspecting the point estimates and CIs on the forest plots; if the CIs had poor overlap then heterogeneity was considered to be present. We also assessed heterogeneity statistically using a Chi² test, with a P value of less than 0.1 indicating statistically significant heterogeneity. Furthermore, we quantified heterogeneity using the I² statistic. A guide to interpretation of the I² statistic is given in Section 9.5.2 of the Cochrane Handbook for Systematic Reviews of Interventions as follows (Higgins 2011).
-
0% to 40%: might not be important.
-
30% to 60%: may represent moderate heterogeneity.
-
50% to 90%: may represent substantial heterogeneity.
-
75% to 100%: considerable heterogeneity.
Assessment of reporting biases
Publication bias arises when the nature and direction of the findings influences whether the research is published or not. For example, statistically significant 'positive' results which show an intervention works are more likely to be published, are published more rapidly in English, are published more than once and in higher‐impact journals.
If at least 10 studies were included in a meta‐analysis, we planned to assess publication bias according to the recommendations on testing for funnel plot asymmetry (Egger 1997), as described in Section 10.4 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). Asymmetries of funnel plots may indicate publication bias and other biases related to sample size. If asymmetries were identified, we would examine possible causes.
Data synthesis
We performed data synthesis in the latest version of Review Manager 5 (RevMan 5) (Review Manager 2014). We only carried out a meta‐analysis where studies of similar comparisons reported the same outcomes. We combined mean differences (MDs) for continuous outcomes and risk ratios (RRs) for dichotomous outcomes, using a random‐effects model.
Subgroup analysis and investigation of heterogeneity
We did not intend to undertake any subgroup analysis.
Sensitivity analysis
If there were sufficient studies in the meta‐analysis, we planned to undertake a sensitivity analysis for the 'low risk of bias' studies, to ensure the conclusions were robust. There were insufficient studies to do this.
Results
Description of studies
Results of the search
The previous published version of this review had no included and six excluded studies. The electronic search for this version of the review update produced a total of 329 records. After duplicates were removed, the number was reduced to 228. After screening by two authors (IK, SG), we found three ongoing trials (Characteristics of ongoing studies) and six articles (reporting three trials) appeared to meet the inclusion criteria. After obtaining and examining the full texts, we included three trials (six publications) that reported results from a total 146 participants (Gharaibeh 2008; Parkin 2012; Smailienė 2013). Figure 5 presents a summary of the study selection process as a flow chart.
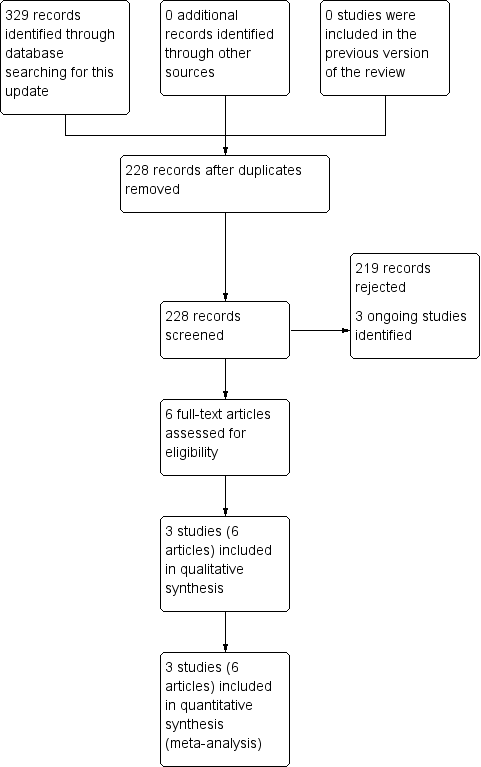
Study flow diagram of searches conducted for this update (2008 to 2017)
Included studies
See Characteristics of included studies.
Characteristics of the trials and settings
All studies were either randomised (Parkin 2012) or quasi‐randomised (Gharaibeh 2008; Smailienė 2013) trials, using a two‐arm parallel group design to detect superiority of one technique over the alternative technique. One study was conducted in the United Kingdom (Parkin 2012), one in Jordan (Gharaibeh 2008) and one in Lithuania (Smailienė 2013). One study was multi‐centred (Parkin 2012).
Characteristics of participants
A total of 146 participants were analysed across all three studies: 32 (Gharaibeh 2008), 71 (Parkin 2012) and 43 (Smailienė 2013). All included participants had palatally displaced canines, either unilaterally or bilaterally. All studies included children, but with different mean ages: 17.5 years (Gharaibeh 2008), 14.2 years (Parkin 2012) and 15.8 years (Smailienė 2013). The majority of participants were female.
Characteristics of interventions
All the included studies directly compared the open surgical exposure versus the closed surgical exposure techniques, for palatally displaced maxillary canine teeth.
Characteristics of outcomes
Two studies did not report all the outcomes of interest for this review (Gharaibeh 2008; Smailienė 2013). We wrote to these authors to see if data from unreported outcomes were collected.
Primary outcomes
Success of surgery
Only Parkin 2012 published data for this outcome. Data were obtained from correspondence with the authors of the other two studies.
Complications or adverse effects
Only Parkin 2012 published data for complications. Gharaibeh 2008 measured intraoperative bleeding but the information presented in a conference abstract did not match participant numbers reported in the published paper. The trial author stated in an email that additional participants had been added to the study. As there was a lack of clarity around this, we did not use these data. Smailienė 2013 did not assess complications.
Aesthetics of the treated canine
Only two studies reported outcome data on aesthetics (Parkin 2012; Smailienė 2013). We were unable to pool the data as the outcome measures were too different.
Secondary outcomes
Patient response (pain/discomfort)
Two studies reported patient‐based outcome responses (Gharaibeh 2008; Parkin 2012). We were unable to pool the data as the outcome measures were too different.
Gum health
Two studies reported data related to periodontal condition of the treated tooth (Parkin 2012; Smailienė 2013). We were unable to pool the data as the outcome measures were too different. Gharaibeh 2008 stated in an email that periodontal health had been assessed but data were not yet available for this outcome.
Treatment time
All studies reported data concerning various stages of treatment.
-
Two studies reported data on the length of the surgical procedure (Gharaibeh 2008; Parkin 2012).
-
One study reported the average time taken for eruption of the canine (Smailienė 2013).
-
One study reported the average time of the fixed appliance phase (Smailienė 2013).
Parkin 2012 measured time taken for canine to be aligned and overall duration of treatment, but these data are not yet available for inclusion in the review.
Excluded studies
Details of the six studies excluded from the previous version can be found in the Characteristics of excluded studies table. No additional studies were excluded in this version of the review. Most of the studies were excluded as they were not randomised controlled trials.
Risk of bias in included studies
Figure 3 and Figure 4 show a summary of our 'Risk of bias' assessments for the included studies.
Allocation
Only one study was at low risk of bias as it described an adequate method of random sequence generation (Parkin 2012). We sought clarification from the authors of Gharaibeh 2008 as they did not provide details of randomisation in the paper. Neither Gharaibeh 2008 nor Smailienė 2013 used an adequate method of randomisation. Both studies were quasi‐randomised, with participants allocated to interventions by alternation, which we assessed as being at high risk of bias.
Blinding
Blinding of participants and personnel (performance bias)
It is not possible to blind participants or personnel as to the surgical procedure being carried out. Although we thought it unlikely this would introduce any performance bias that could affect the outcomes, assuming that the surgeon was equally experienced at using both techniques, we judged all studies to be at unclear risk of bias for this domain.
Blinding of outcome assessment ‐ subjective outcomes (detection bias)
It is not possible to blind participants. Although we think this is unlikely to introduce bias in the patient‐reported outcomes as the participants had no experience of the alternative technique, we assessed this domain as at unclear risk of bias.
Blinding of outcome assessment ‐ objective outcomes (detection bias)
One study provided details on blinding of outcome assessment and was assigned 'low risk' (Parkin 2012). Gharaibeh 2008 did not make any comments on blinding of outcome assessment and Smailienė 2013 did not provide details on methods of blinding for all outcome measures; thus we judged both studies to be at unclear risk of detection bias.
Incomplete outcome data
Gharaibeh 2008 and Parkin 2012 were judged to be at low risk of bias, as they reported all outcome data, and accounted for withdrawals and dropouts, with few participants being excluded. We judged Smailienė 2013 as 'unclear risk of bias', as during correspondence with the author we found out that one participant had been excluded from the study, but this was not reported in the paper. Attrition was less than 20% for all studies.
Selective reporting
One study was judged to be at low risk of bias for this domain (Parkin 2012). Gharaibeh 2008 indicated in personal correspondence that periodontal health data had been recorded but this was not reported in the published paper and we do not know if it was in the protocol, so we assessed the risk of reporting bias as unclear. We assessed Smailienė 2013 as high risk because there was no clear statement about primary or secondary outcomes.
Other potential sources of bias
All studies were assigned 'low risk' for this domain.
Effects of interventions
See: Summary of findings for the main comparison
Open versus closed surgical technique
Success of treatment
One trial reported on success and failure rates of treatment for each surgical technique at 10 days (Parkin 2012). Out of 66 participants, there were 28 successful treatments and three failures in the open group (n = 31) and 33 successful treatments and two failures in the closed group (n = 35). Gharaibeh 2008 and Smailienė 2013 reported in email correspondence with the review authors that they had a 100 per cent success rate for both techniques. Overall, therefore, there were three failures out of 69 in participants having the open treatment and two failures out of 72 participants having the closed treatment. There was no evidence of a difference in success rates between the the open and closed groups (RR 0.99, 95% CI 0.93 to 1.06, P = 0.79). There was no heterogeneity between the results of the studies (Analysis 1.1).
Complications
One of the surgical failures was due to detachment of the gold chain (closed group). Parkin 2012 reported complications following surgery, which both occurred in the closed group: one participant developed a postoperative infection requiring antibiotic treatment, and one participant experienced pain during traction and the chain fenestrated the palatal mucosa.
Aesthetics
Two trials reported on aesthetics using different outcomes (Parkin 2012; Smailienė 2013).
One study showed photographs of the treated canine and untreated contralateral canine to two panels made up of orthodontists and laypeople, who were asked if they could identify the operated canine from the unoperated canine and whether the operated canine or unoperated canine looked best (Parkin 2012). Orthodontists correctly identified the operated side 60.7% of the time (95% CI 53.7 to 67.8), which was significantly different from the null percentage of 50% (P = 0.003). The lay judges correctly identified the operated side 49.7% of the time (95% CI 45.3 to 54.0), which was not significantly different to the null value (P = 0.880). The were no differences in the proportion of correctly identified sides between those treated with an open or closed surgical procedure for either panel.
The other study assessed aesthetics by looking at tooth colour, tooth position in the dental arch and tooth inclination and reported the number of participants that did not have 'normal' outcomes (Smailienė 2013). There was no evidence of a difference between the groups for: colour (RR 1.91, 95% CI 0.19 to 19.52, P = 0.59), position in the dental arch (RR 2.39, 95% CI 0.52 to 10.99, P = 0.26) or tooth inclination (RR 1.91, 95% CI 0.78 to 4.66, P = 0.16) (Analysis 1.3).
Patient response
One trial measured the worst pain experienced every day for one week postoperatively (Gharaibeh 2008). There was no evidence of a difference in moderate or severe pain experienced between the two groups at one day postoperatively (RR 0.86, 95% CI 0.61 to 1.20, P = 0.37). No participant experienced moderate or severe pain at one week postoperatively in either group (Analysis 1.5).
One trial used a visual analogue scale from 1 to 10 cm (with 10 being the worst) to measure response to treatment with regards to pain or soreness, difficulty eating, discomfort following the operation, bad taste in the mouth and difficulty speaking (Parkin 2012). Duration of pain or soreness was also recorded and dichotomous data on pain‐killer use were collected. There was no evidence of a difference in the pain scores between the open and closed groups (MD 0.00, 95% CI −1.09 to 1.09, P = 1.00). Total discomfort score was calculated using scores for pain, difficulty eating, difficulty brushing, difficulty speaking and bad taste in the mouth . There was no evidence of a difference between the groups (MD 0.10, 95% CI −4.17 to 4.37, P = 0.96) (Analysis 1.4).
One trial recorded participant satisfaction with the treatment as either satisfactory or unsatisfactory (Smailienė 2013). All participants in both groups were satisfied with the treatment (RR 1.00, 95% CI 0.92 to 1.09, P = 1.00) (Analysis 1.9).
Gum health
Probing depth
One study reported periodontal probing depths by using six‐point probing (Smailienė 2013). There was no evidence of a difference in probing depths between the two groups (MD −0.14 mm, 95% CI −0.48 to 0.20, P = 0.41) (Analysis 1.6).
Bleeding on probing
One study measured bleeding on probing using the Papilla Bleeding Index (Smailienė 2013). There was no evidence of a difference between the two groups (MD 0.21, 95% CI −0.14 to 0.56, P = 0.24) (Analysis 1.6).
Clinical attachment level
One study reported clinical attachment level in millimetres by measuring the periodontal probing depth and adding this to the gingival recession value (Parkin 2012) . There was no evidence of a difference between the open and closed surgical groups (MD −0.10 mm, 95% CI −0.45 to 0.25, P = 0.57) (Analysis 1.6).
Crestal bone levels
One study reported radiographic crestal bone levels as a percentage at the mesial point and distal point of the canine tooth (Smailienė 2013). There was no overall evidence of a difference between the open and closed surgical groups at either point: mesial (MD 3.21 mm, 95% CI −0.33 to 6.75, P = 0.08); distal (MD −0.18 mm, 95% CI −3.09 to 2.73, P = 0.90) (Analysis 1.6).
The other study that assessed radiographic bone levels reported "no significant difference was found between the open and closed groups (independent t test, P = 0.936)" (Parkin 2012). Bone levels were assessed between the canine and lateral incisor (mesial bone levels). However, there were few radiographs available and some were of low quality, where "it was not always possible to see bone levels clearly for assessment" (Analysis 1.6).
Gingival recession
One study reported gingival recession using six‐point probing (Smailienė 2013). There was no evidence of a difference between the open and closed surgical groups (RR 0.19, 95% 0.01 to 3.76, P = 0.28) (Analysis 1.6).
Midbuccal recession
Two studies reported midbuccal recession in millimetres (Parkin 2012; Smailienė 2013). In Parkin 2012, standard deviations were calculated from the raw data available. There was no evidence of a difference between the open and closed groups (MD −0.02 mm, 95% CI −0.21 to 0.16, P = 0.81). There was no statistical heterogeneity between the results of the studies (Analysis 1.6).
Midpalatal recession
One study measured midpalatal recession in millimetres (Smailienė 2013). As the mean values reported were very small, a difference was not estimable; thus there was no evidence of a difference between the two groups (Analysis 1.6).
One study measured midpalatal gingival recession using an index (1 ‒ cementoenamel junction not visible; 2 ‒ cementoenamel junction and less than 2 mm of root surface visible; 3 ‒ cementoenamel junction and 2 mm or more of root surface visible) (Parkin 2012). No participants scored a 3 on the index. There was no evidence of a difference between the open and closed groups (RR 1.32, 95% CI 0.63 to 2.77, P = 0.47) (Analysis 1.7).
Treatment time
Length of time in surgery
Two studies reported length of time in surgery from the initial incision to the final suture (Gharaibeh 2008; Parkin 2012). There was no evidence of a difference between the open and closed groups: mean difference (MD −3.30 minutes, 95% CI −9.97 to 3.36, P = 0.33). There was substantial statistical heterogeneity between the studies. Parkin 2012 discusses that this may be due to additional procedures, such as extractions, being carried out at the same time as the surgery and reports that if "other procedures performed at the same time as the surgical exposure had been excluded from the analysis, then the mean operating times would be similar to those of Gharaibeh and Al‐Numri" (Analysis 1.8).
Time taken for the canine to erupt/extrude
One study reported a difference in the mean time 'from surgical exposure to bonding a bracket on the middle of the labial surface' (MD −3.81 months, 95% CI −5.80 to −1.82, P = 0.0002) (Analysis 1.8) (Smailienė 2013); but as the aim of the closed exposure is not to allow the tooth to erupt naturally, but to align it under the mucosa, the clinical significance of this difference is not clear.
Duration of orthodontic treatment
One study reported the duration of orthodontic treatment from time of placement to removal of the fixed appliances (Smailienė 2013). There was no evidence of a difference in the overall treatment time between the open and closed surgery groups (MD −3.77 months, 95% CI −9.20 to 1.66, P = 0.17) (Analysis 1.8). There were large differences between the standard deviation of the treatment times between the two groups (open SD 5.0 months; closed 11.7 months); however, whereas participants undergoing an open exposure had their surgery before the placement of fixed appliances (mean 1.6 months, SD 4.4), those having a closed exposure had their surgery after placement of fixed appliances (3.7 months, SD 3.6).
Discussion
Summary of main results
From the three included trials, it appears that there may be no advantage in performing an exposure using an open rather than a closed technique for the outcomes documented; however, we cannot be certain of this finding as the quality of the evidence is low. Only one trial was randomised; the other two were quasi‐randomised and had a high risk of bias in several domains.
Exposure of PDCs appears to be a successful intervention: only three failures (out of 69) occurred in the open groups and two (out of 71) in the closed groups.
Aesthetic analysis is probably one of the most important outcomes to the patient and it appears that there was little or no difference between operated and unoperated canines at the end of treatment. It is therefore hardly surprising that there was no difference in aesthetic outcome when PDCs exposed with an open versus closed procedure are compared. This is also the case when periodontal health was examined: although a statistically significant difference was detected between unoperated and operated canines, this difference was small (0.5 mm) and unlikely to be clinically relevant. When open versus closed techniques were compared, there was no difference.
Other patient‐centred outcomes included pain/discomfort in the post‐operative period, and duration of treatment. Again, from the data collected, we could not detect a significant difference.
It should be borne in mind that we cannot be certain about any of our findings because the quality of the evidence is low to very low.
Overall completeness and applicability of evidence
More data are required from high‐quality RCTs to investigate these outcomes further, particularly for patient‐centred outcomes, such as treatment duration and aesthetics. As there are only three small RCTs, with two of them at high risk of bias, it is not possible to draw any firm conclusions.
There was no attempt to investigate the influence of tooth location: is there a difference in outcome if the PDC is mildly impacted, as opposed to severely impacted, according to the technique used? The research question asked in the review is non‐specific and it might be more applicable to practice if we ask which technique is superior for mildly displaced canines, moderately displaced canines and severely displaced canines. This may be something we explore in future updates of our review.
Quality of the evidence
The available evidence is limited to three small studies, two of which are at high risk of bias. As the evidence found for the review is of overall low quality, further research is likely to have an important impact on our confidence in the estimate that no difference exists between the two techniques.
Potential biases in the review process
Some authors of this review (NP, PB) are also investigators involved with one of the included clinical trials; however the screening of abstracts, determination of the included studies and data extraction for this update were undertaken independently of these two authors.
Agreements and disagreements with other studies or reviews
The previous review published in 2009 had no studies included so no conclusions could be drawn. There is now some evidence that there is no difference in outcome whether PDCs are exposed using an open or a closed technique.
Evidence from excluded studies
There has been one review (not systematic) by Burden 1999, which concluded that there was no evidence to support either technique. It included only one study that directly compared closed and open techniques (Wisth 1976a). Thirty‐four participants received an open exposure and 22 participants received a closed exposure. It was found that the mean duration of treatment was four months longer in the closed group and it was reported that this was likely due to lack of direct vision of the canine from when it was exposed to when it was brought into the line of the arch. The closed group appeared to have less periodontal damage in terms of loss or attachment and bone levels. The study, however, was retrospective and pretreatment equivalence was not established (in terms of participants' age or severity of canine displacement), therefore the risk of selection and detection bias was high.
Schmidt 2007 conducted a study that evaluated differences in periodontal health, root length and aesthetics in 16 participants with unilaterally palatally displaced canines and six participants with bilaterally displaced canines. All were exposed using an open technique and the canines were allowed to erupt autonomously before being brought into their correct position with braces. Outcomes were compared to the contralateral untreated canine (control teeth) and also to data obtained from an earlier study (Woloshyn 1994). In the Woloshyn study, all palatally displaced canines received a closed exposure. Both studies found that the roots of the impacted canine and adjacent lateral incisor were slightly shorter than those of the contralateral canine and that the treated canine could be visually identified from the untreated canine in 70% to 80% of cases. Woloshyn also found significant differences in probing depths and crestal bone height when comparing treated with untreated canines, which was not found in the Schmidt study. It was concluded that the overall consequences to the impacted canine with this technique seem better than with a closed technique; however, consequences to the lateral incisor were similar with both techniques. This is in contrast to findings of other authors (Becker 1983; Crescini 2007; Kohavi 1984; Quirynen 2000). The authors reported excellent periodontal health following alignment of canines using a closed technique. Importantly, all these mentioned studies (including that by Schmidt) are retrospective and findings therefore score low in terms of evidence.
A prospective study investigating "patients' perception of recovery after exposure of impacted teeth" made a direct comparison between open and closed techniques (Chaushu 2005). Sixty participants were enrolled: 25 received a closed exposure and 32 received an open exposure. There was no random allocation. Questionnaires were given to the participants following surgery to assess their perception of recovery in four main areas: pain; oral function; ability to participate in routine daily activities; and 'other symptoms' such as bad taste, bleeding or swelling. The comparison revealed that participants receiving an open exposure had a longer recovery time in all areas, except 'ability to participate in routine activities'. However, since the participants were not randomly allocated, the risk of selection bias is high. If one group had more severely impacted canines, this would have a bearing on the results.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies
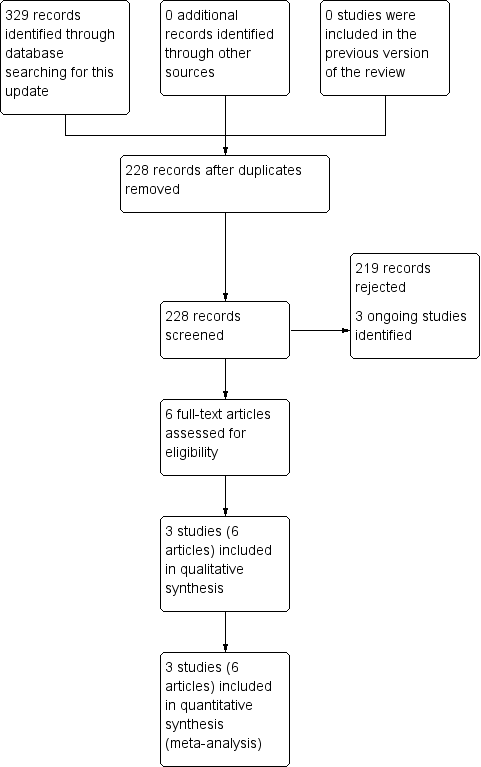
Study flow diagram of searches conducted for this update (2008 to 2017)

Comparison 1 Open surgical technique versus closed surgical technique, Outcome 1 Success of surgery.
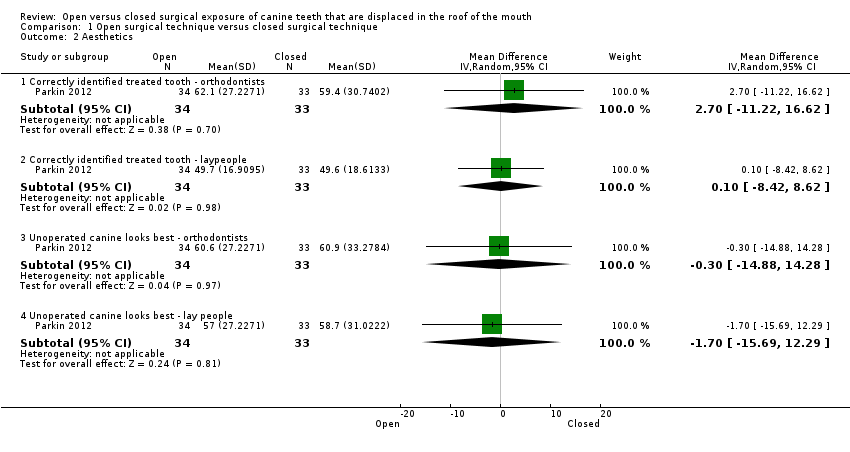
Comparison 1 Open surgical technique versus closed surgical technique, Outcome 2 Aesthetics.
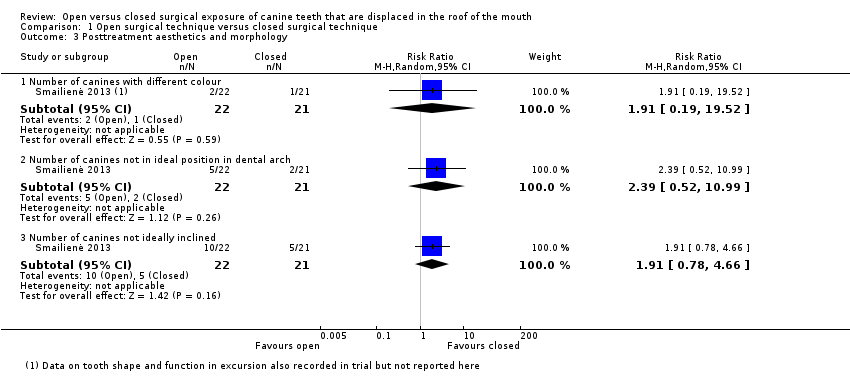
Comparison 1 Open surgical technique versus closed surgical technique, Outcome 3 Posttreatment aesthetics and morphology.
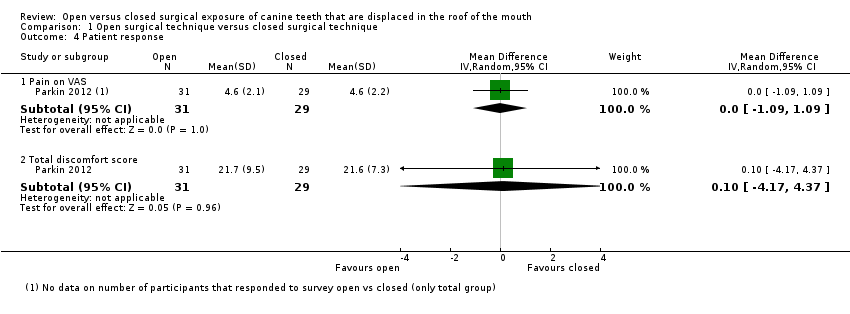
Comparison 1 Open surgical technique versus closed surgical technique, Outcome 4 Patient response.
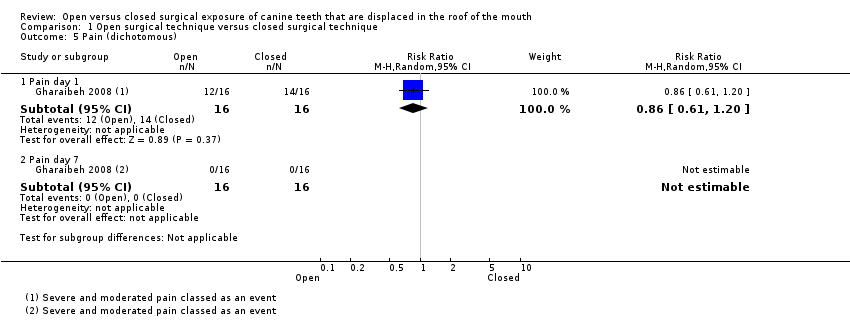
Comparison 1 Open surgical technique versus closed surgical technique, Outcome 5 Pain (dichotomous).
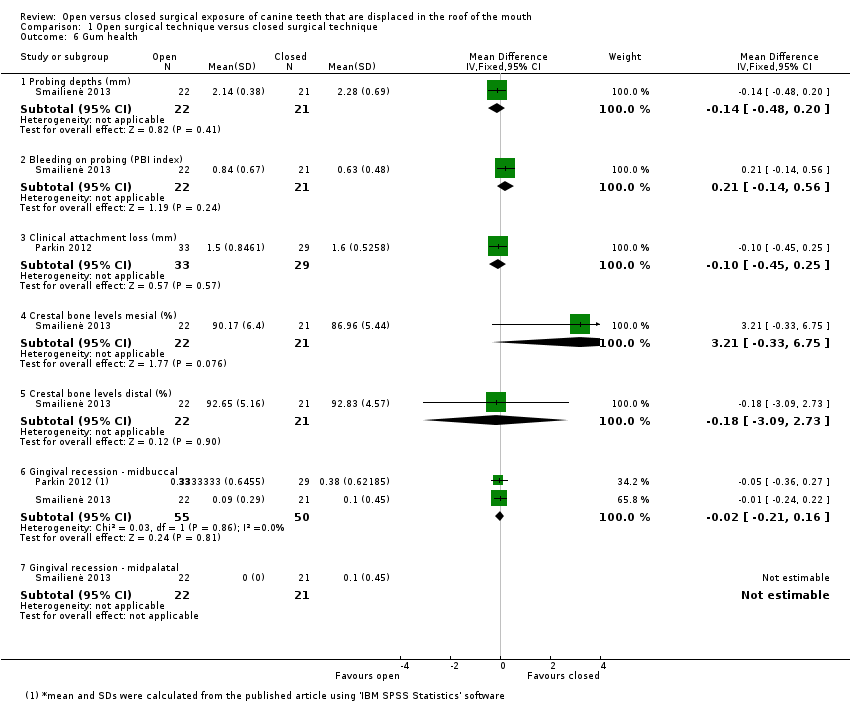
Comparison 1 Open surgical technique versus closed surgical technique, Outcome 6 Gum health.

Comparison 1 Open surgical technique versus closed surgical technique, Outcome 7 Gingival recession (dichotomous).

Comparison 1 Open surgical technique versus closed surgical technique, Outcome 8 Treatment time.
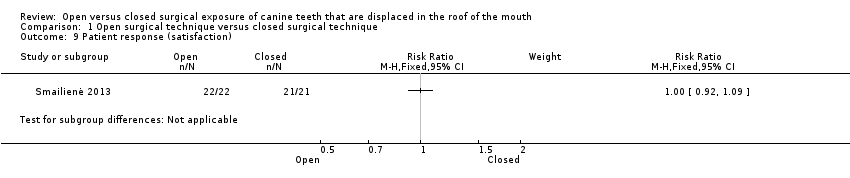
Comparison 1 Open surgical technique versus closed surgical technique, Outcome 9 Patient response (satisfaction).
| Open surgical technique compared with closed surgical technique for palatally impacted canines | ||||||
| Patient or population: people with maxillary palatally impacted canines Settings: oral surgery departments Intervention: open surgical technique Comparison: closed surgical technique | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Closed surgery | Open surgery | |||||
| Success of surgery | 943 per 1000 | 934 per 1000 | RR 0.99 (0.93 to 1.06) | 141 | ⊕⊕⊝⊝ | The available evidence suggests that there is no difference in the success of surgery between the techniques and that both techniques have a high success rate. |
| Complications | One surgical failure was due to detachment of the gold chain (closed group). One study reported two complications following surgery, both in the closed group: a post‐operative infection requiring antibiotics and pain during alignment of the canine as the gold chain penetrated through the gum tissue of the palate. | |||||
| Aesthetics (reported in various manners at different time points) | This outcome was measured in a variety of ways in the studies that cannot be pooled. | ⊕⊝⊝⊝ | This outcome is subjective and can be measured and reported in many different ways. The current evidence suggests that there is no difference in aesthetic outcomes between the groups. | |||
| Patient response (pain and discomfort reported in different ways between 1 to 10 days postoperatively) | This outcome was measured in a variety of ways in the studies that cannot be pooled. | ⊕⊝⊝⊝ | This outcome is subjective and was measured and reported in different ways. The current evidence suggests that there is no difference in patient response outcomes between the groups. | |||
| Gum health (clinical attachment level (CAL); 3 months post‐debond) | Mean CAL in the closed group | Mean CAL in the intervention groups was 0.1 mm lower | 62 | ⊕⊕⊝⊝ | This outcome was measured and reported in different ways in different studies. The current evidence suggests that there is no difference in periodontal outcomes between the groups. | |
| Treatment time (length of time in operating theatre from first incision to final suture) | Mean of the closed group was 34.3 minutes in Parkin 2012; and 37.7 minutes in Gharaibeh 2008. | Mean of the open group was 3.18 minutes less (7.59 minutes less to 1.22 minutes more) | 89 (2 studies) | ⊕⊝⊝⊝ | The current evidence suggests that there is no difference in length of time in surgery between the groups. | |
| *The basis for the assumed risk is the Parkin 2012 closed group. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded one level due to high risk of bias in two studies. Downgraded one level as two studies had no failures. 2 Downgraded one level due to high risk of bias in one study. Downgraded one level as each outcome only reported by single studies. Downgraded one level as studies with few participants and large confidence intervals for some outcomes. 3 Downgraded two levels due to high risk of bias in two studies and subjective participant‐reported outcome with no blinding. Downgraded one level as each outcome only reported by single studies. 4 Downgraded two levels as single small study at high risk of bias. 5 Downgraded one level due to high risk of bias in one study. Downgraded one level as substantial heterogeneity between results. Downgraded one level as studies with few participants and large confidence intervals for some outcomes. | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Success of surgery Show forest plot | 3 | 141 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.93, 1.06] |
| 2 Aesthetics Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 Correctly identified treated tooth ‐ orthodontists | 1 | 67 | Mean Difference (IV, Random, 95% CI) | 2.70 [‐11.22, 16.62] |
| 2.2 Correctly identified treated tooth ‐ laypeople | 1 | 67 | Mean Difference (IV, Random, 95% CI) | 0.10 [‐8.42, 8.62] |
| 2.3 Unoperated canine looks best ‐ orthodontists | 1 | 67 | Mean Difference (IV, Random, 95% CI) | ‐0.30 [‐14.88, 14.28] |
| 2.4 Unoperated canine looks best ‐ lay people | 1 | 67 | Mean Difference (IV, Random, 95% CI) | ‐1.70 [‐15.69, 12.29] |
| 3 Posttreatment aesthetics and morphology Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 3.1 Number of canines with different colour | 1 | 43 | Risk Ratio (M‐H, Random, 95% CI) | 1.91 [0.19, 19.52] |
| 3.2 Number of canines not in ideal position in dental arch | 1 | 43 | Risk Ratio (M‐H, Random, 95% CI) | 2.39 [0.52, 10.99] |
| 3.3 Number of canines not ideally inclined | 1 | 43 | Risk Ratio (M‐H, Random, 95% CI) | 1.91 [0.78, 4.66] |
| 4 Patient response Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 4.1 Pain on VAS | 1 | 60 | Mean Difference (IV, Random, 95% CI) | 0.0 [‐1.09, 1.09] |
| 4.2 Total discomfort score | 1 | 60 | Mean Difference (IV, Random, 95% CI) | 0.10 [‐4.17, 4.37] |
| 5 Pain (dichotomous) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 5.1 Pain day 1 | 1 | 32 | Risk Ratio (M‐H, Random, 95% CI) | 0.86 [0.61, 1.20] |
| 5.2 Pain day 7 | 1 | 32 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Gum health Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 6.1 Probing depths (mm) | 1 | 43 | Mean Difference (IV, Fixed, 95% CI) | ‐0.14 [‐0.48, 0.20] |
| 6.2 Bleeding on probing (PBI index) | 1 | 43 | Mean Difference (IV, Fixed, 95% CI) | 0.21 [‐0.14, 0.56] |
| 6.3 Clinical attachment loss (mm) | 1 | 62 | Mean Difference (IV, Fixed, 95% CI) | ‐0.10 [‐0.45, 0.25] |
| 6.4 Crestal bone levels mesial (%) | 1 | 43 | Mean Difference (IV, Fixed, 95% CI) | 3.21 [‐0.33, 6.75] |
| 6.5 Crestal bone levels distal (%) | 1 | 43 | Mean Difference (IV, Fixed, 95% CI) | ‐0.18 [‐3.09, 2.73] |
| 6.6 Gingival recession ‐ midbuccal | 2 | 105 | Mean Difference (IV, Fixed, 95% CI) | ‐0.02 [‐0.21, 0.16] |
| 6.7 Gingival recession ‐ midpalatal | 1 | 43 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Gingival recession (dichotomous) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 7.1 Midpalatal recession | 1 | 62 | Risk Ratio (M‐H, Random, 95% CI) | 1.32 [0.63, 2.77] |
| 8 Treatment time Show forest plot | 3 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 8.1 Length of time in surgery | 2 | 89 | Mean Difference (IV, Random, 95% CI) | ‐3.30 [‐9.97, 3.36] |
| 8.2 Time taken for eruption | 1 | 43 | Mean Difference (IV, Random, 95% CI) | ‐3.81 [‐5.80, ‐1.82] |
| 8.3 Length of fixed appliance phase | 1 | 43 | Mean Difference (IV, Random, 95% CI) | ‐3.77 [‐9.20, 1.66] |
| 9 Patient response (satisfaction) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |

