Music interventions for mechanically ventilated patients
Abstract
Background
Mechanical ventilation often causes major distress and anxiety in patients. The sensation of breathlessness, frequent suctioning, inability to talk, uncertainty regarding surroundings or condition, discomfort, isolation from others, and fear contribute to high levels of anxiety. Side effects of analgesia and sedation may lead to the prolongation of mechanical ventilation and, subsequently, to a longer length of hospitalization and increased cost. Therefore, non‐pharmacological interventions should be considered for anxiety and stress management. Music interventions have been used to reduce anxiety and distress and improve physiological functioning in medical patients; however, their efficacy for mechanically ventilated patients needs to be evaluated. This review was originally published in 2010 and was updated in 2014.
Objectives
To update the previously published review that examined the effects of music therapy or music medicine interventions (as defined by the authors) on anxiety and other outcomes in mechanically ventilated patients. Specifically, the following objectives are addressed in this review.
1. To conduct a meta‐analysis to compare the effects of participation in standard care combined with music therapy or music medicine interventions with standard care alone.
2. To compare the effects of patient‐selected music with researcher‐selected music.
3. To compare the effects of different types of music interventions (e.g., music therapy versus music medicine).
Search methods
We searched the Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library 2014, Issue 2), MEDLINE (1950 to March 2014), CINAHL (1980 to March 2014), EMBASE (1980 to March 2014), PsycINFO (1967 to March 2014), LILACS (1982 to March 2014), Science Citation Index (1980 to March 2014), www.musictherapyworld.net (1 March 2008) (database is no longer functional), CAIRSS for Music (to March 2014), Proquest Digital Dissertations (1980 to March 2014), ClinicalTrials.gov (2000 to March 2014), Current Controlled Trials (1998 to March 2014), the National Research Register (2000 to September 2007), and NIH CRISP (all to March 2014). We handsearched music therapy journals and reference lists, and contacted relevant experts to identify unpublished manuscripts. There was no language restriction. The original search was performed in January 2010.
Selection criteria
We included all randomized and quasi‐randomized controlled trials that compared music interventions and standard care with standard care alone for mechanically ventilated patients.
Data collection and analysis
Two review authors independently extracted the data and assessed the methodological quality of included studies. We contacted authors to obtain missing data where needed. Where possible, results for continuous outcomes were presented in meta‐analyses using mean differences and standardized mean differences. Post‐test scores were used. In cases of significant baseline difference, we used change scores. For dichotomous outcomes, we presented the results as risk ratios.
Main results
We identified six new trials for this update. In total, the evidence for this review rests on 14 trials (805 participants). Music listening was the main intervention used, and 13 of the studies did not include a trained music therapist. Results indicated that music listening may be beneficial for anxiety reduction in mechanically ventilated patients. Specifically, music listening resulted, on average, in an anxiety reduction that was 1.11 standard deviation units greater (95% CI ‐1.75 to ‐0.47, P = 0.0006) than in the standard care group. This is considered a large and clinically significant effect. Findings indicated that listening to music consistently reduced respiratory rate and systolic blood pressure, suggesting a relaxation response. Furthermore, one large‐scale study reported greater reductions in sedative and analgesic intake in the music listening group compared to the control group, and two other studies reported trends for reduction in sedative and analgesic intake for the music group. One study found significantly higher sedation scores in the music listening group compared to the control group.
No strong evidence was found for reduction in diastolic blood pressure and mean arterial pressure. Furthermore, inconsistent results were found for reduction in heart rate with seven studies reporting greater heart rate reductions in the music listening group and one study a slightly greater reduction in the control group. Music listening did not improve oxygen saturation levels.
Four studies examined the effects of music listening on hormone levels but the results were mixed and no conclusions could be drawn.
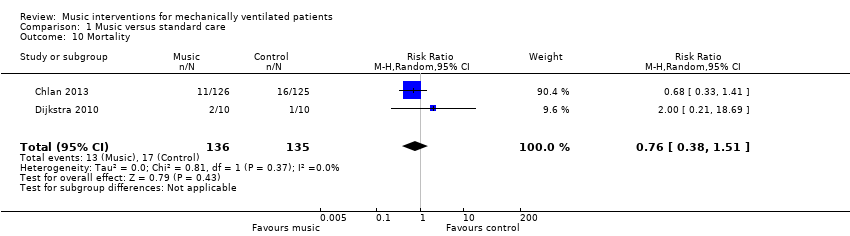
No strong evidence was found for an effect of music listening on mortality rate but this evidence rested on only two trials.
Most trials were assessed to be at high risk of bias because of lack of blinding. Blinding of outcome assessors is often impossible in music therapy and music medicine studies that use subjective outcomes, unless the music intervention is compared to another treatment intervention. Because of the high risk of bias, these results need to be interpreted with caution.
No studies could be found that examined the effects of music interventions on quality of life, patient satisfaction, post‐discharge outcomes, or cost‐effectiveness. No adverse events were identified.
Authors' conclusions
This updated systematic review indicates that music listening may have a beneficial effect on anxiety in mechanically ventilated patients. These findings are consistent with the findings of three other Cochrane systematic reviews on the use of music interventions for anxiety reduction in medical patients. The review furthermore suggests that music listening consistently reduces respiratory rate and systolic blood pressure. Finally, results indicate a possible beneficial impact on the consumption of sedatives and analgesics. Therefore, we conclude that music interventions may provide a viable anxiety management option to mechanically ventilated patients.
PICOs
Plain language summary
Music interventions for mechanically ventilated patients
Review question
We reviewed the evidence on the effect of music interventions compared to standard care on anxiety and other outcomes in mechanically ventilated patients.
Background
Mechanical ventilation often causes major distress and anxiety in patients, putting them at greater risk for complications. Side effects of analgesia and sedation may lead to the prolongation of mechanical ventilation and, subsequently, to a longer length of hospitalization and increased cost. Therefore, non‐pharmacological interventions should be considered for anxiety and stress management. Several studies have examined the impact of music interventions on anxiety and physiological responses in mechanically ventilated patients. Music interventions are categorized as 'music medicine' when passive listening to pre‐recorded music is offered by medical personnel. In contrast, music therapy requires the implementation of a music intervention by a trained music therapist, the presence of a therapeutic process, and the use of personally tailored music experiences. A systematic review was needed to gauge the efficacy of both music therapy and music medicine interventions.
Search date
The evidence is current to March 2014.
Study characteristics
We included 14 controlled trials involving 805 critically ill participants on mechanical ventilation. All participants were alert. Slightly more patients (58%) included in these studies were male and their average age was 58 years.
The majority of the studies examined the effects of patients listening to pre‐recorded music. Most studies offered one 20 to 30‐minute music session to the participants.
Key results
The findings suggest that music listening may have a large anxiety‐reducing effect on mechanically ventilated patients. The results furthermore suggest that music listening consistently reduces respiratory rate and systolic blood pressure, suggesting a relaxation response. No evidence of effect was found for diastolic blood pressure, mean arterial pressure, or oxygen saturation level and inconsistent results were found for heart rate and hormone levels. One large‐scale study reported greater reductions in the intake of sedative and analgesic medications in the music listening group compared to the control group, and two other studies reported similar trends.
Music listening did not result in any harm.
Quality of the evidence
Most trials presented some methodological weakness. Therefore, these results need to be interpreted with caution. However, the results are consistent with the findings of three other Cochrane systematic reviews on the use of music interventions for anxiety reduction in medical patients. Therefore, we conclude that music interventions may provide a viable anxiety management option to mechanically ventilated patients.
Authors' conclusions
Summary of findings
| Music compared to standard care for mechanically ventilated patients | |||
| Patient or population: mechanically ventilated patients | |||
| Outcomes | Relative effect | No of participants | Quality of the evidence |
| State anxiety | The mean state anxiety in the intervention groups was | 288 | ⊕⊕⊝⊝ |
| Heart rate | The mean heart rate in the intervention groups was | 338 | ⊕⊝⊝⊝ |
| Respiratory rate | The mean respiratory rate in the intervention groups was | 357 | ⊕⊝⊝⊝ |
| Systolic blood pressure mmHg | The mean systolic blood pressure in the intervention groups was | 269 | ⊕⊝⊝⊝ |
| Diastolic blood pressure mmHg | The mean diastolic blood pressure in the intervention groups was | 269 | ⊕⊝⊝⊝ |
| Mean arterial pressure mmHg | The mean arterial pressure in the intervention groups was | 98 | ⊕⊝⊝⊝ |
| Oxygen saturation level | The mean oxygen saturation level in the intervention groups was | 193 | ⊕⊕⊝⊝ |
| CI: Confidence interval | |||
| GRADE Working Group grades of evidence | |||
| 1 The majority of the trials were assessed as high risk of bias studies | |||
Background
Description of the condition
Mechanical ventilation often causes major distress and anxiety in patients. The sensation of breathlessness, frequent suctioning, inability to talk, uncertainty regarding surroundings or condition, discomfort, isolation from others, and fear contribute to high levels of anxiety (Lindgren 2005; Wong 2001). Increased anxiety may in turn lead to breathing difficulty and greater distress during weaning attempts, that is, the process of liberating the patient from mechanical support and from the tracheal tube (Boles 2007; Lindgren 2005). Moreover, mechanically ventilated patients often experience adverse events, including constriction of arteries and the airways in the lungs, caused by this anxiety (Ledingham 1988). Therefore, analgesia and sedation are considered important in the management of patients who require mechanical ventilation.
Complications related to the use of analgesic and sedative agents are common, however, and the immobility resulting from sedation may contribute to venous thrombosis or pressure damage to the nerves and skin. Furthermore, immune responses may be weakened from extensive use of sedative medications (Suter 2002). These side effects may lead to the prolongation of mechanical ventilation and, subsequently, to a longer length of hospitalization and increased costs (Bobek 2001; Egerod 2002; Kollef 1998). Additionally, an increase in morbidity and mortality has been found in anxious, critically ill patients (Moser 1996).
Description of the intervention
A review of the literature on treatment interventions for mechanically ventilated patients (Thomas 2003) indicated that the four most frequently perceived stressors for mechanically ventilated patients are dyspnoea or difficulty breathing, anxiety, fear, and pain. Few non‐pharmacological interventional studies looking at ways to reduce these stressors were found. Four interventions, that is, hypnosis and relaxation, patient education and information sharing, music therapy, and supportive touch have been investigated and results indicate that they may be helpful in reducing patient stress (Thomas 2003).
Music has been used in different medical fields to meet physiological, psychological, and spiritual needs of adult and paediatric patients. Research on the effects of music or music therapy for medical patients has burgeoned during the past 20 years and has included a variety of outcome measures in a wide range of specialty areas (Dileo 2005). Specifically, the anxiolytic effects of music have been studied in a variety of medical patients including surgical (Bradt 2013a; Bringman 2009; Koch 1998; Mok 2003), cardiac (Bradt 2013b; Hamel 2001; Mandel 2007; White 1999), and oncology (Bradt 2011; Bufalini 2009; Nguyen 2010) patients.
It is important to make a clear distinction between music interventions administered by medical or healthcare professionals (music medicine) and those implemented by trained music therapists (music therapy). A substantive set of data (Dileo 2005) indicates that music therapy interventions with medical patient populations are significantly more effective than music medicine interventions for a wide variety of outcomes. This difference might be attributed to the fact that music therapists individualize their interventions to meet patients' specific needs; more actively engage the patients in the music making; and employ a systematic therapeutic process, including assessment, treatment, and evaluation. As defined by Dileo (Dileo 1999), interventions are categorized as music medicine when listening to pre‐recorded music is offered by medical personnel or is self‐administered by the patient. In contrast, music therapy requires the implementation of a music intervention by a trained music therapist, the presence of a therapeutic process, and the use of personally tailored music experiences. These music experiences include:
-
listening to live, improvised, or pre‐recorded music;
-
performing music on an instrument;
-
improvising music spontaneously using voice or instruments, or both;
-
composing music; and
-
music combined with other modalities (e.g., movement, imagery, art) (Dileo 2007).
Heiderscheit and colleagues (Heiderscheit 2011) point out that music listening as a self‐administered intervention (that is with minimal or no assistance from a music therapist) can play an important role in the self‐management of anxiety and distress in intensive care unit (ICU) environments. They emphasize that this type of music intervention can "empower a patient to utilize the music whenever they may need it and as often as they need it. This type of non‐pharmacological and patient‐directed approach gives the patient options to manage their symptoms even when a music therapist is not present or available" (Heiderscheit 2011 pp. 2‐3). This might be of particular importance to adolescent patients. Given that adolescents, on average, listen to music 2.5 hours per day (Rideout 2005), continued use of music listening during mechanical ventilation may be especially effective in providing them with a sense of safety, control, and normalcy. Ghetti (Ghetti 2013) furthermore advocates for the use of live music, in contrast to pre‐recorded music, with children and adolescents in paediatric ICUs as it allows for "the therapist to remain responsive to the changing needs of the child and family, to provide emotional support in real‐time, to improvise lyrics based on the surroundings, and to incorporate family members into the provision of music".
A major advantage of listening to pre‐recorded or live music for patients who are mechanically ventilated is that it does not require focused concentration or sustained energy levels (Chlan 2009).
Patients should select music they prefer since unfamiliar music or music disliked by the patient could increase anxiety and agitation (Heiderscheit 2011). In the case of mechanically ventilated patients, assessment of music preference may be challenging. Therefore, assessment of music preferences by a trained music therapist is recommended (Chlan 2009; Heiderscheit 2011). A music assessment intervention tool (MAT) for this purpose and guidelines for implementation have been published (Chlan 2009).
How the intervention might work
As outlined by Bradt and colleagues (Bradt 2013a), a common theory regarding the anxiety‐reducing effects of music is that music can help patients focus their attention away from stressful events to something pleasant and soothing (Mitchell 2003; Nilsson 2008). Even though this is an important mechanism in anxiety reduction, it is important to emphasize that music does more than refocusing patients’ attention. It provides the patient with an aesthetic experience that can offer comfort and peace during times of distress. In music interventions provided by a trained music therapist, the music therapist furthermore adapts the live music interactions to the in‐the‐moment needs of the patients. This often provides a deeply humanizing and validating experience for the patient. In addition, listening to self‐selected pre‐recorded music, initiated by the patient him or herself, may result in an increased sense of control and empowerment in a critical care environment where most aspects of care are beyond the patient's control (Chlan 2013).
On a neurophysiological level, it has been postulated that music induces relaxation through its impact on automated and central nervous responses (Beaulieu‐Boire 2013; Gillen 2008; Lai 2006). More specifically, it is believed that the anxiolytic or anxiety‐reducing effect of music is achieved through its suppressive action on the sympathetic nervous system, leading to decreased adrenergic activity (that is, reduced release of the stress hormone adrenaline) and decreased stimulation of nerves and muscles (Chlan 1998; Gillen 2008). Music furthermore triggers the limbic system, a section of the brain that plays an important role in the regulation of emotional responses, to release endorphins; these neurotransmitters play an important role in enhancing a sense of well‐being (Arslan 2008; Beaulieu‐Boire 2013). However, Gillen (Gillen 2008) has suggested that more research is needed to examine the physiological mechanisms that explain the anxiolytic effects of music.
It is important to note that there are a number of individual factors that may influence responses to music. These include, but are not limited to, age, gender, cognitive function, severity of stress, anxiety, discomfort and pain, training in music, familiarity with and preference for the music, culture, and personal associations with the music (Pelletier 2004; Standley 1986; Standley 2000). Music also evokes various types of imagery in many individuals. Thus, the individual's unique imagery experience will influence his or her responses to the music. Therefore, it cannot be assumed that sedative music will always have positive effects on individuals; careful monitoring of individual effects is needed.
Why it is important to do this review
Several research studies on the effects of music on mechanically ventilated patients have reported positive results. A number of these studies, however, have suffered from small sample size (Almerud 2003; Besel 2006; Chlan 1995; Wong 2001). In addition, differences in factors such as study design, methods of intervention, and types of music have led to varying results. A systematic review is needed to more accurately gauge the efficacy of music medicine or music therapy as anxiety‐reducing interventions for mechanically ventilated patients, as well as to identify variables that may moderate the effects.
Objectives
To update the previously published review that examined the effects of music therapy or music medicine interventions (as defined by the authors) on anxiety and other outcomes in mechanically ventilated patients. Specifically, the following objectives are addressed in this review.
-
To conduct a meta‐analysis to compare the effects of participation in standard care combined with music therapy or music medicine interventions with standard care alone.
-
To compare the effects of patient‐selected music with researcher‐selected music.
-
To compare the effects of different types of music interventions (e.g., music therapy versus music medicine).
Methods
Criteria for considering studies for this review
Types of studies
We included all randomized controlled trials (RCT) and controlled clinical trials (CCTs) with quasi‐randomized or systematic methods of treatment allocation in any language, published and unpublished.
Types of participants
The review included studies of mechanically ventilated patients in an intensive or critical care unit, long term acute care hospital (LCAT), or 'step‐down' unit. We imposed no restrictions as to age, gender, or ethnicity. We included both patients undergoing ventilation and patients who were being weaned after prolonged mechanical ventilation. The most frequently used modes of ventilatory support included synchronized intermittent mandatory ventilation and a pressure support mode. Types of airway management included oral endotracheal tube, nasal endotracheal tube, and tracheostomy tube.
Types of interventions
We included all studies in which standard treatment combined with music therapy or music medicine interventions (as defined by the authors) were compared with:
-
standard care alone;
-
standard care combined with other therapies; or
-
standard care with placebo. Placebo treatment involved the use of headphones for the patients wherein no music stimuli were provided or another type of auditory stimulus was provided (e.g., white noise (hiss), pink noise (sound of ocean waves), or nature sounds).
Types of outcome measures
Primary outcomes
-
State anxiety (defined as a temporary unpleasant emotional arousal in the face of threatening demands or dangers; this is in contrast with trait anxiety, which reflects the existence of stable individual differences in reactions (Spielberger 1983)), as reported by the study authors
Secondary outcomes
-
Sedative drug intake, as reported by the study authors
-
Physiological outcomes (e.g., heart rate, systolic blood pressure, diastolic blood pressure, respiratory rate, oxygen saturation, airway pressure)
-
Quality of life, as reported by the study authors
-
Patient satisfaction, as reported by the study authors
-
Post‐discharge patient outcomes (e.g., functional status, post‐discharge quality of life), as reported by the study authors
-
Mortality
-
Cost‐effectiveness
Search methods for identification of studies
Electronic searches
We used the search strategy for MEDLINE as was listed in the protocol (Appendix 1) and adapted it for the other databases. We updated the previously run searches from 2010 (Appendix 16). We searched the following electronic databases and trials registers:
-
Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library 2014, Issue 2);
-
MEDLINE (1966 to March 2014);
-
EMBASE (1980 to March 2014);
-
CINAHL (1982 to March 2014);
-
PsycINFO (1967 to March 2014);
-
LILACS ( 1982 to March 2014);
-
AMED (1985 to January 2010) (we no longer had access to AMED after this date);
-
Science Citation Index (1980 to March 2014);
-
the specialist music therapy research database at www.musictherapyworld.net (database is no longer functional) (1 March 2008);
-
CAIRSS for Music (March 2014);
-
Proquest Digital Dissertations (1980 to March 2014);
-
ClinicalTrials.gov (www.clinicaltrials.gov/) (2000 to March 2014);
-
Current Controlled Trials (www.controlled‐trials.com/) (1998 to March 2014);
-
National Research Register at http://www.nihr.ac.uk/Pages/NRRArchive.aspx (2000 to September 2007) (register is no longer maintained);
-
NIH CRISP (March 2014).
The original search was performed in January 2010 (Bradt 2010).
Searching other resources
We handsearched the following journals, from the first available date:
-
Australian Journal of Music Therapy (March 2014);
-
Canadian Journal of Music Therapy (March 2014);
-
The International Journal of the Arts in Medicine (December 2007, latest issue was published in 1999);
-
Journal of Music Therapy (March 2014);
-
Musik‐,Tanz‐, und Kunsttherapie (Journal for Art Therapies in Education, Welfare and Health Care) (March 2014, latest issue available online 2013(1));
-
Musiktherapeutische Umschau (March 2014);
-
Music Therapy (December 2007, latest issue published in 1996);
-
Music Therapy Perspectives (March 2014);
-
Nordic Journal of Music Therapy (March 2014);
-
Music Therapy Today (online journal of music therapy) (December 2007, latest issue published December 2007);
-
Voices (online international journal of music therapy) (March 2014);
-
New Zealand Journal of Music Therapy (March 2014);
-
British Journal of Music Therapy (March 2014);
-
Japanese Music Therapy Association Journal (March 2014);
-
Music and Medicine (March 2014).
We checked the bibliographies of relevant studies and reviews. We contacted relevant experts for the identification of unpublished trials.
We imposed no language restrictions for either searching or trial inclusion.
Data collection and analysis
Selection of studies
One author (JB) scanned the titles and abstracts of each record retrieved from the searches for the original review, while a research assistant did this for the update. If information in the abstract clearly indicated that the trial did not meet the inclusion criteria, we rejected the trial. When a title or abstract could not be rejected with certainty, the authors independently inspected the full‐text article for the original review. This inspection was completed by JB and a research assistant for the update. We used an inclusion criteria form to assess the trial's eligibility for inclusion. We checked the inter‐rater reliability for trial selection. If a trial was excluded, we kept a record of both the article and the reason for exclusion.
Data extraction and management
The lead author (JB) and a research assistant independently extracted data from the selected trials using a standardized coding form. There were no disagreements in the data extraction.
Assessment of risk of bias in included studies
JB and a research assistant assessed all included trials for risk of bias in the original review and were blinded to each other's assessments. For the updated review, JB and CD completed these assessments independently. Any disagreements were resolved by discussion. The authors used the following criteria for quality assessment.
Random sequence generation
-
Low risk
-
Unclear risk
-
High risk
Random sequence generation was rated as low risk if every participant had an equal chance to be selected for either condition and if the investigator was unable to predict which treatment the participant would be assigned to. Use of date of birth, date of admission, or alternation resulted in high risk of bias.
Allocation concealment
-
Low risk methods to conceal allocation included:
-
-
central randomization;
-
serially numbered, opaque, sealed envelopes;
-
other descriptions with convincing concealment.
-
-
Unclear risk, authors did not adequately report on method of concealment.
-
High risk (e.g., alternation methods were used).
Blinding of participants and personnel
-
Low risk
-
Unclear risk
-
High risk
Since participants cannot be blinded in a music intervention trial, studies were not downgraded for not blinding the participants. As for personnel, in music therapy studies music therapists cannot be blinded because they are actively making music with the patients. In contrast, in music medicine studies blinding of personnel is possible by providing control group participants with headphones but no music (for example, a blank CD). Therefore, downgrading for not blinding personnel was only applied in studies that used listening to pre‐recorded music.
Blinding of outcome assessors
-
Low risk
-
Unclear risk
-
High risk
Incomplete outcome data
We recorded the proportion of participants whose outcomes were analysed. We coded losses to follow‐up for each outcome as:
-
low risk, if fewer than 20% of patients were lost to follow‐up and reasons for loss to follow‐up were similar in both treatment arms;
-
unclear risk, if loss to follow‐up was not reported;
-
high risk, if more than 20% of patients were lost to follow‐up or reasons for loss to follow‐up differed between treatment arms.
Selective reporting
-
Low risk, reports of the study were free of suggestion of selective outcome reporting
-
Unclear risk
-
High risk, reports of the study suggest selective outcome reporting
Other sources of bias
-
Low risk
-
Unclear risk
-
High risk
Information on potential financial conflicts of interest was considered as a possible source of additional bias.
The above criteria were used to give each article an overall quality rating, based on the Cochrane Handbook for Systematic Reviews of Interventions Section 8.7 (Higgins 2011).
A. Low risk of bias: all criteria met.
B. Moderate risk of bias: one or more of the criteria only partly met.
C. High risk of bias: one or more criteria not met.
Studies were not excluded based on a low quality score.
Measures of treatment effect
All outcomes but one in this review were presented as continuous variables. We calculated standardized mean differences with 95% confidence intervals (CI) for outcome measures using results from different scales. When there were sufficient data available from various studies using the same measurement instrument, we computed a mean difference (MD) with 95% CI. For one outcome (that is mortality) we calculated the risk ratio with 95% CI.
Unit of analysis issues
In all studies included in this review, participants were individually randomized to the intervention or the standard care control group. Post‐test values or change values on a single measurement for each outcome from each participant were collected and analysed.
Dealing with missing data
We analysed data on an endpoint basis, including only participants for whom a final data point measurement was obtained (available case analysis). We did not assume that participants who dropped out after randomization had a negative outcome.
Assessment of heterogeneity
We investigated heterogeneity using visual inspection of the forest plots as well as the I2 statistic, with I2 > 50% indicating significant heterogeneity.
Assessment of reporting biases
We tested for publication bias visually in the form of funnel plots (Higgins 2011).
Data synthesis
We entered all trials included in the systematic review into Review Manager (RevMan 5.2). We anticipated that some individual studies would have used final scores whereas others might have used change scores. We combined these different types of analyses as mean difference (MD). We calculated pooled estimates using the more conservative random‐effects model. We determined the levels of heterogeneity by the I2 statistic (Higgins 2002).
The following treatment comparison was made: music interventions versus standard care alone.
Subgroup analysis and investigation of heterogeneity
The following subgroup analyses were determined a priori, but these could not be carried out because of insufficient numbers of studies:
a. type of intervention (music therapy or music medicine);
b. dosage of music therapy or music medicine; and
c. music preference.
Subgroup analyses would have been conducted as described by Deeks et al (Deeks 2001) and as recommended in section 9.6 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011).
Sensitivity analysis
The influence of study quality was examined using a sensitivity analysis wherein the results of including and excluding lower quality studies in the analysis were compared. Specifically, we assessed the impact of studies that used alternate group assignment as a randomization method.
Results
Description of studies
Results of the search
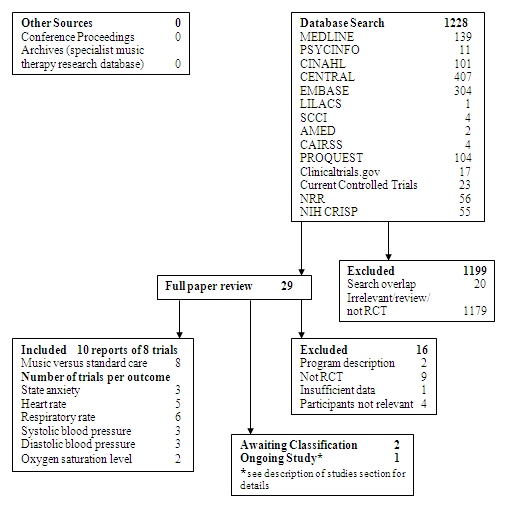
The database searches and handsearching of conference proceedings, journals, and reference lists resulted in 1228 citations (see Figure 1) for the original review. One author (JB) examined the titles and abstracts and identified 29 studies as potentially relevant, which were retrieved for further assessment. These were then independently screened by the two authors.
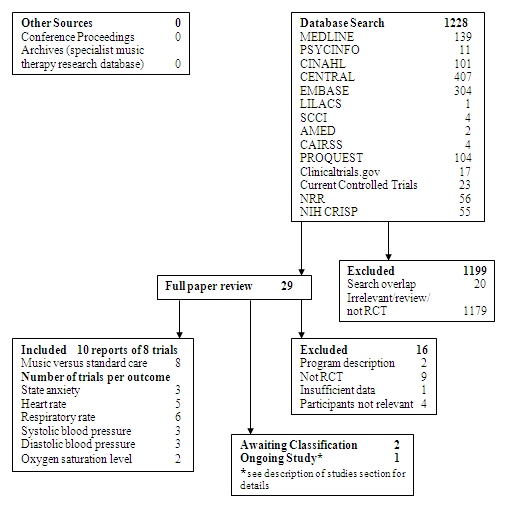
Study Flow Diagram ‐ Original Review.
The 2014 update of the search resulted in 1557 extra citations (Figure 2). One review author (JB) and research assistant examined the titles and abstracts and retrieved full‐text articles where necessary. This resulted in the addition of seven references reporting six new studies.

Study flow diagram ‐ updated review.
Seventeen references reporting 14 trials were included in this review (see Characteristics of included studies) (Beaulieu‐Boire 2013; Chlan 1995; Chlan 1997; Chlan 2007a; Chlan 2013; Conrad 2007; Dijkstra 2010; Han 2010; Jaber 2007; Korhan 2011; Lee 2005; Phillips 2007; Wong 2001; Wu 2008). Where necessary, we contacted chief investigators to obtain additional information on study details and data.
Included studies
We included 14 studies with a total of 805 patients in this review. These studies examined the effects of music on physiological and psychological outcomes in mechanically ventilated patients. Slightly more patients included in these studies were male (58%). The average age was 58 years. Eight studies provided details on ethnicity (Chlan 1997; Chlan 2007a; Chlan 2013; Han 2010; Korhan 2011; Lee 2005; Wong 2001; Wu 2008). For four of those studies (Chlan 1997; Chlan 2007a; Chlan 2013; Korhan 2011) the participants were predominantly white. For the other four studies all participants were Asian. Five studies were conducted in the USA (Chlan 1995; Chlan 1997; Chlan 2007a; Chlan 2013; Phillips 2007); three in China (Han 2010; Lee 2005; Wong 2001); one in Taiwan (Wu 2008); one in Canada (Beaulieu‐Boire 2013); one in Germany (Conrad 2007); one in the Netherlands (Dijkstra 2010); one in Turkey (Korhan 2011); and one in France (Jaber 2007). Trial sample size ranged from 10 to 266 participants.
Eight studies (Beaulieu‐Boire 2013; Chlan 1997; Chlan 2007a; Dijkstra 2010; Han 2010; Korhan 2011; Lee 2005; Wong 2001) included details on the ventilatory support modes used. Synchronized intermittent mandatory ventilation and the pressure support mode were most frequently used. Five studies (Han 2010; Jaber 2007; Lee 2005; Wong 2001; Wu 2008) detailed the type of airway management. The majority of the patients had an oral endotracheal tube or a tracheostomy tube. Few patients had a nasal endotracheal tube. Eleven studies (Beaulieu‐Boire 2013; Chlan 1995; Chlan 1997; Chlan 2007a; Chlan 2013; Dijkstra 2010; Han 2010; Korhan 2011; Lee 2005; Wong 2001; Wu 2008) provided information related to the average number of days on mechanical ventilation before the onset of the study. The average number of days was 8.53 with a range of 0 days to 161 days. All patients were alert.
A variety of medical diagnoses were included in each study, except for Conrad (Conrad 2007), with the primary diagnoses being pulmonary‐related problems in most studies. Other medical problems included post‐surgical complications, cardiac disease, trauma injuries, cancer, and sepsis. Conrad's study only included postoperative patients. Not all studies measured all outcomes identified for this review.
Details of the studies included in the review are shown in the table Characteristics of included studies.
Thirteen studies were categorized as music medicine studies (as defined by the review authors in the background section). One study (Phillips 2007) was categorized as music therapy. All music medicine studies used music listening as the main intervention. The music therapy study used live music selected by the patient. The music therapist initially matched the music to the respiratory rate of the patient. The tempo of the music was then gradually decelerated to decrease the rate of vital signs to ranges suitable for extubation.
Most studies offered one 20 to 30‐minute music session to the patients. Three studies offered 60‐minute sessions (Beaulieu‐Boire 2013; Chlan 2007a; Korhan 2011). Three studies offered two or more music sessions (Beaulieu‐Boire 2013; Chlan 2013; Dijkstra 2010). In most clinical settings that serve patients on mechanical ventilation, listening to pre‐recorded music can be easily implemented at low cost. However, studies are needed that compare the effect of different frequencies, durations, and timing of music sessions. Offering multiple music listening sessions allows for the patient to give feedback about the music, select different music if needed, and become more skilled in using music for relaxation purposes. In the case of music therapy interventions, multiple sessions allow for the development of a therapeutic relationship and deepening of the therapeutic process through the music. This may lead to greater health benefits.
Except for one study (Conrad 2007), none of the music medicine studies in the original review provided detailed information about the music that was used. The authors only reported the different styles of music that were offered to the participants (for example, jazz, easy listening, country and western, classical music) without any composition‐specific or performance‐specific information. Conrad provided information about the specific compositions that were used (see Characteristics of included studies table). Only one study (Chlan 1997) provided tempo information. Four of the six studies that were included in the update reported more details regarding the music that was used (Beaulieu‐Boire 2013; Dijkstra 2010; Han 2010; Korhan 2011). One study (Chlan 2013) conducted a detailed assessment of music preference with each patient and personalized playlists were used.
Eleven studies used patient‐selected music, whereas three studies (Beaulieu‐Boire 2013; Conrad 2007; Korhan 2011) used researcher‐selected music. In some trials, only classical music choices were offered without a good rationale for this music selection. In several trials, participants were allowed to select the music from a variety of music that was offered. This decision was based on the assumption that music preference plays an important part in the effectiveness of music relaxation. However, it needs to be noted that participants could only select from a limited number of music styles presented by the researcher. It is likely that the preferred music of some of the participants was not included in the music selection offered and, even if it were, that they may not have liked the specific compositions or songs being played. Lee explicitly stated that four participants disliked the music (Lee 2005). Another researcher reported that five patients refused to participate because they disliked the music selections that were being offered, whereas five other participants expressed a dislike for the music after they completed participation in the music intervention (Wong 2001). An exception to this were the trials by Chlan 2013 and Han 2010. In the study by Chlan and colleagues, a music therapist conducted detailed assessments of patient preferences. Han offered participants over 40 pieces of music in a variety of styles to select from.
The data for one study (Chlan 2007a) could not be pooled with the other studies because of severe validity issues. The lead author expressed the following concerns: there was wide variability in mean levels of biomarkers, a very small sample size, and several confounding factors (for example, administration of intravenous morphine sulphate to two control patients; and two experimental patients needed endotracheal suctioning during the intervention). The data for two additional studies (Conrad 2007; Korhan 2011) were only provided in narrative form in this review because of insufficient data reporting. Finally, the data from the study by Chlan and colleagues (Chlan 2013) could not be pooled with other studies because the report detailed the results of statistical modelling but did not provide means and SDs.
Excluded studies
In the original review, we excluded a total of 16 studies for the following reasons: (a) programme descriptions only (Chlan 2000; Fontaine 1994); (b) studies were not randomized controlled trials or controlled clinical trials (Besel 2006; Burke 1995; Chlan 2001; Chlan 2006; Chou 2003; Hansen‐Flachen 1994; Hunter 2010; Iriarte 2003; Twiss 2006); (c) study participants did not meet the inclusion criteria (Caine 1991; Lorch 1994; Standley 1995; Wiens 1995); and (d) insufficient data reporting (Almerud 2003).
For the update, we excluded an additional seven studies for the following reasons: (a) studies were not randomized controlled trials or controlled clinical trials (Chlan 2011); (b) no music intervention (Tate 2010); (c) review article (Austin 2010; Davis 2012; Ho 2012); and (d) a commentary (Bauer 2002; Nilsson 2011).
The reasons for exclusion are listed in the table Characteristics of excluded studies.
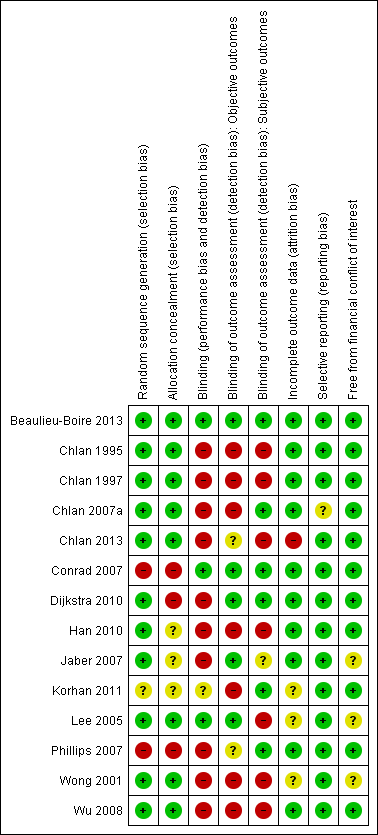
Risk of bias in included studies
Allocation
We included studies that used appropriate methods of randomization (for example, a computer‐generated table of random numbers, drawing of lots, flip of coins) (11 studies) (Beaulieu‐Boire 2013; Chlan 1995; Chlan 1997; Chlan 2007a; Chlan 2013; Dijkstra 2010; Han 2010; Jaber 2007; Lee 2005; Wong 2001; Wu 2008) as well as studies that used non‐random methods of allocation (for example, alternate group assignment) (three studies) (Conrad 2007; Korhan 2011; Phillips 2007). The impact of method of randomization was examined by sensitivity analyses. Fifty‐seven per cent of the studies (eight studies) used allocation concealment (Beaulieu‐Boire 2013; Chlan 1995; Chlan 1997; Chlan 2007a; Chlan 2013; Lee 2005; Wong 2001; Wu 2008) and for three studies (21%) the use of allocation concealment was unclear (Han 2010; Jaber 2007; Korhan 2011).
Blinding
In music intervention studies, participants cannot be blinded (unless they are in studies that compare different types of music interventions). Three studies reported blinding personnel (Beaulieu‐Boire 2013; Conrad 2007; Lee 2005). This was achieved by having both music group and control group participants wear headsets and listen to a CD. The control group listened to a blank CD.
Only five trials reported blinding of the outcome assessors for objective outcomes (Beaulieu‐Boire 2013; Conrad 2007; Dijkstra 2010; Jaber 2007; Lee 2005). For two trials the use of blinding was unclear (Chlan 2013; Phillips 2007). The other trials did not use blinding for objective outcomes. For subjective outcomes, (for example, the State and Trait Anxiety Inventory (STAI) (Spielberger 1983)), blinding of outcome assessors was not possible unless the participants were blinded to the intervention. We would like to point out that the assessment of risk of bias figure lists several studies as having used blinding for subjective outcomes. However, these were studies that did not include subjective outcomes. A rating of low risk was assigned if studies did not include subjective outcomes.
Incomplete outcome data
The dropout rate was small for most trials, namely between 0% and 11%. One trial (Chlan 2013) reported a dropout rate of more than 20%. For three trials it was unclear whether there were any participant withdrawals (Korhan 2011; Lee 2005; Wong 2001) . Most trials reported reasons for dropout. Detailed information on the dropout rates and reasons is included in the Characteristics of included studies table.
Selective reporting
Publication bias for respiratory rate as an outcome was examined visually in the form of a funnel plot (Figure 3). The funnel plot suggests that all but one of the included studies had small standard errors (that is they were plotted towards the top of the graph). Publication bias may be present in that no studies were included with findings that were not statistically significant.
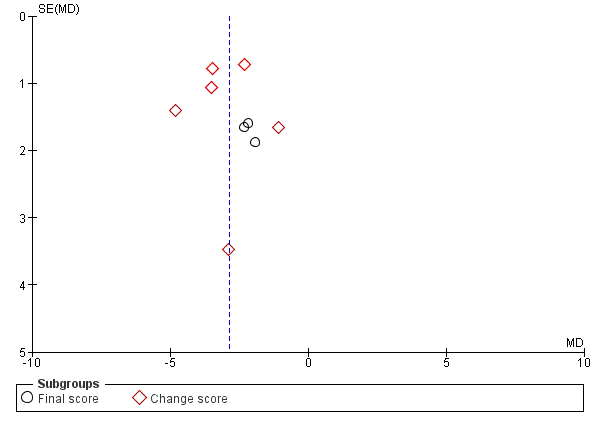
Funnel plot of comparison: 1 Music versus standard care, outcome: 1.4 Respiratory rate.
Other potential sources of bias
We did not identify any other potential sources of bias in the studies included in this review.
As a result of the risk of bias assessment, we concluded that one trial was at low risk of bias (Beaulieu‐Boire 2013). All other trials were at high risk of bias. The main reason for receiving a high risk of bias rating was the lack of blinding. As mentioned before, blinding is often impossible in music therapy and music medicine studies that use subjective outcomes, unless the music intervention is compared to another treatment intervention (for example, progressive muscle relaxation or a different type of music intervention). Therefore, it appears impossible for these types of studies to receive a low or moderate risk of bias even if all other risk factors (for example, randomization, allocation concealment, etc.) have been adequately addressed.
As all but one trial were rated at the same level (high risk), we did not carry out sensitivity analysis on the basis of overall quality rating. Instead, we conducted a sensitivity analysis to examine the impact of the method of random sequence generation. Excluding those studies that used alternate assignment or for which the randomization method was unclear did not alter the findings of this review. Specific sensitivity analysis findings are reported in the Effects of interventions section.
Risk of bias is detailed for each trial in the risk of bias tables included in the Characteristics of included studies table, and the 'Risk of bias' summary (Figure 4). In addition, an overall assessment of risk of bias can be viewed in Figure 5.
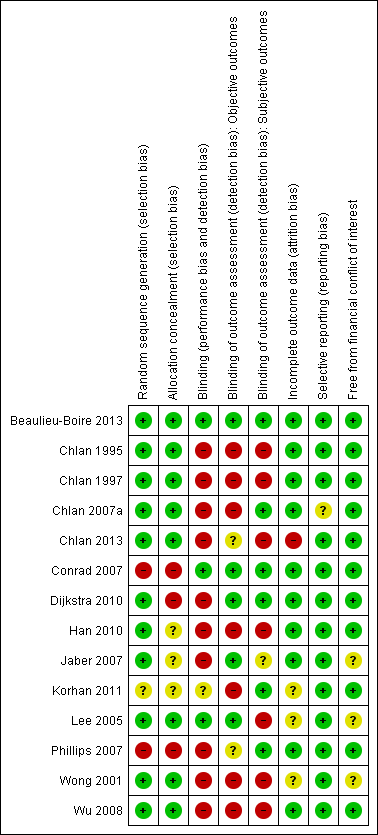
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
Effects of interventions
Primary outcomes
State anxiety
Six studies (Chlan 1997; Chlan 2013; Han 2010; Lee 2005; Wong 2001; Wu 2008) examined the effects of music listening on state anxiety in mechanically ventilated patients. Four studies (Chlan 1997; Han 2010; Lee 2005; Wong 2001) used the Spielberger State and Trait Anxiety Inventory (STAI), State Anxiety Short Form, whereas the other studies used a visual analogue scale for anxiety (VAS‐A) (Chlan 2013; Wu 2008). The pooled estimate of five of these studies (N = 288) indicated that music listening may have a beneficial effect on anxiety (SMD ‐1.11, 95% CI ‐1.75 to ‐0.47, P = 0.0006). Statistical heterogeneity across the trials (I² = 83%) was due to some trials (Chlan 1997; Han 2010) reporting much larger beneficial effects of music interventions than others (Analysis 1.1).
The study by Chlan and colleagues (Chlan 2013) was not included in any of the meta‐analyses because the authors presented their findings as statistical modelling results and not as post‐test means or change scores with respective standard deviations (SDs). Therefore, the findings of this study were only reported in the narrative. Chlan (Chlan 2013) reported the results of statistical modelling that used either sedation frequency or sedation intensity. The models suggested that music listening lowered VAS‐A scores consistently by more than 19 mm on the VAS (sedation frequency ß ‐19.5, 95% CI ‐32.2 to ‐6.8; sedation intensity ß ‐19.3, 95% CI ‐32 to ‐6.6; P = 0.003 for both) compared to usual care.
Secondary outcomes
Sedative and analgesic drug intake
Three studies (Beaulieu‐Boire 2013; Chlan 2013; Conrad 2007) provided data on the effect of music on sedative and analgesic drug intake. Beaulieu‐Boire reported separate data for intake of fentanyl, benzodiazepines, and propofol. Chlan reported data on sedation intensity and sedation frequency. Sedation intensity was computed by "dose amounts of medications from disparate drug classes by using a weight‐adjusted dose (adjusting for differing patient weights) of each sedative administered during 4‐hour time blocks during mechanical ventilation" (p. 2336) (for additional information on these computations see Chlan 2013). Sedation frequency score was computed by dividing "a 24‐hour day into six 4‐hour time blocks and, for each of the 8 drugs, the occurrences in which a sedative was administered at least once during that interval were summed. This approach to sedative exposure accounts for medications administered to patients from nonequivalent, disparate drug classes" (p. 2337). Conrad only provided a narrative summary of the findings on propofol consumption.
Beaulieu‐Boire and colleagues (Beaulieu‐Boire 2013) reported a trend toward reduction in fentanyl daily consumption for the music listening group (means ± SD: 1597 ± 1418 μg pre‐ and 1343 ± 1342 μg post‐music versus 1593 ± 1986 μg pre‐ and 1715 ± 1859 μg post‐control) but the difference between the two groups was not statistically significant (P = 0.06). There was no difference between the groups for the intake of other sedative drugs. For daily consumption of benzodiazepines, the following means and SDs were reported: 42 ± 88 mg pre‐ and 36 ± 94 mg post‐music versus 46 ± 107 mg pre‐ and 45 ± 109 mg post‐control). For propofol daily consumption, the following means and SDs were reported: 291 ± 732 mg pre‐ and 284 ± 730 mg post‐music versus 282 ± 677 mg pre‐ and 395 ± 928 mg post‐control.
Chlan (Chlan 2013) reported that the music listening group had a greater decrease in change over time of the sedation intensity score (ß ‐0.18, 95% CI ‐0.36 to ‐0.004, P = 0.05) as well as the sedation frequency score (ß ‐0.21, 95% CI ‐0.37 to ‐0.05, P = 0.01) compared with the usual care group. The authors also reported group differences for the fifth study day, which represented the average time patients were enrolled in the study. Whereas an average usual care group participant received five doses of any one of the eight commonly administered sedative and analgesic medications (midazolam, lorazepam, propofol, dexmedetomidine, morphine, fentanyl, hydromorphone, and haloperidol), an equivalent music group participant received just three doses. In terms of sedation intensity scores, an average usual care participant had a sedation intensity score of 4.4 whereas an equivalent music listening group participant had a sedation intensity score of 2.8. This represented a relative reduction of 38% for sedation frequency score and 36% for sedation intensity score.
Conrad (Conrad 2007) reported that "patients in the music group did not require additional sedation by propofol, whereas among patients in the control group, propofol was occasionally necessary to allow sufficient patient‐ventilator coordination" (p. 2710). Other authors reported that, as part of the protocol, no medication was provided to the participants for the duration of the intervention (Chlan 1995; Jaber 2007).
One study (Dijkstra 2010) examined the effect of music listening on level of sedation by means of Ramsay scores rather than on sedative drug intake. Significantly higher sedation scores were obtained in the music listening group compared to the control group after the first session (MD 6.60, 95% CI 5.64 to 7.56, P < 0.0001). A trend for higher scores in the music group remained for the second and third sessions but these were no longer statistically significant.
Heart rate
The pooled estimate of eight studies (Chlan 1995; Chlan 1997; Dijkstra 2010; Han 2010; Jaber 2007; Lee 2005; Phillips 2007; Wu 2008) (N = 338) indicated that listening to music significantly reduced heart rate (MD ‐3.95, 95% CI ‐6.62 to ‐1.27, P = 0.004; I² = 62%). The results were not consistent across studies with seven studies reporting a greater heart rate reduction in the music listening group compared to the control and one study (Wu 2008) reporting a slightly greater reduction in the control group (Analysis 1.2). A sensitivity analysis examining the impact of randomization methods revealed that inclusion of an alternate assignment study (Phillips 2007) did not inflate the effect size. In contrast, excluding this study led to a higher pooled estimate (MD ‐4.01, 95% CI ‐6.80 to ‐1.22, P < 0.005) (Analysis 1.3).
Conrad (Conrad 2007) reported that the heart rate in the control group increased from 120 beats per minute (BPM) (SD = 9) to 125 bpm (SD = 7), whereas it remained the same in the music group. However, no significant differences between the groups were found. Because no means and SDs were reported for the music group, these data could not be included in the meta‐analysis. Conrad was unable to provide the original data.
One cross‐over study (Beaulieu‐Boire 2013) reported that music listening did not alter overall vital signs (heart rate, respiratory rate, and arterial blood pressure) compared with the placebo‐control condition but no statistical information was provided. The authors were unable to provide means and SDs for these outcomes.
Respiratory rate
Listening to music also had a significant effect on respiratory rate (9 studies, N = 357; MD ‐2.87, 95% CI ‐3.64 to ‐2.10, P < 0.00001) and the results were consistent across studies (I2 = 0%) (Analysis 1.4) (Chlan 1995; Chlan 1997; Dijkstra 2010; Han 2010; Jaber 2007; Lee 2005; Phillips 2007; Wong 2001; Wu 2008). One study (Korhan 2011) could not be included in the meta‐analysis because no means and SDs were reported. The results of this study indicated a statistically significant difference between the music group and the control group for respiratory rate (P = 0.04).
A sensitivity analysis excluding the Phillips study (Phillips 2007) because of its inadequate randomization method did not change the pooled estimate (MD ‐2.87, 95% CI ‐3.64 to ‐2.09, P < 0.00001; I2 = 0%) (Analysis 1.5).
Blood pressure
Seven studies (Chlan 1995; Dijkstra 2010; Han 2010; Jaber 2007; Korhan 2011; Lee 2005; Wu 2008) examined the effects of music listening on blood pressure. The study by Korhan (N = 60) could not be included in the meta‐analysis because of lack of statistical information. The pooled estimate of the other studies (N = 269) indicated a beneficial effect for the music intervention on systolic blood pressure (SBP) (MD ‐4.22, 95% CI ‐6.38 to ‐2.06, P = 0.0001) that was consistent across studies (I2 = 0%) (Analysis 1.6). A pooled estimate of ‐2.16 mm Hg (95% CI ‐4.40 to 0.07) was found for diastolic blood pressure (DBP), however this effect was not statistically significant (P = 0.06). (Analysis 1.7). Korhan reported a statistically significant difference between the music group and the control group for SBP (P = 0.02) and DBP (P = 0.02).
The pooled estimate of three studies (Dijkstra 2010; Wong 2001; Wu 2008) indicated no strong evidence of effect for the music intervention on mean arterial pressure (MAP) (MD ‐1.79, 95% CI ‐4.56 to 0.99, P = 0.21; I2 = 0%) (Analysis 1.8). In contrast, Conrad (Conrad 2007) reported a significant difference (P = 0.014) between the intervention group (N = 5) and the control group (N = 5) but no means and SDs were provided and, therefore, these study results could not be pooled with the results of the other studies.
Oxygen saturation levels
Five studies examined the effects of music listening on oxygen saturation levels (Chlan 1995; Han 2010; Korhan 2011; Phillips 2007; Wu 2008). The study by Korhan could not be included in the meta‐analysis because of lack of statistical information. In the pooled estimate the four remaining studies did not find support for an effect of music (MD ‐0.05, 95% CI ‐0.67 to 0.57, P = 0.88; I2 = 42%) (Analysis 1.9). Similarly, Korhan (Korhan 2011) did not find a statistically significant difference between the music group and the control group for this outcome (P = 0.86). Chlan (Chlan 1995) commented that the lack of improvement in oxygen saturation level may be due to the fact that when a patient was already 100% saturated, there could be no increase in oxygen saturation level. She suggested that mixed venous oxygen saturation monitoring may be a more sensitive measure for oxygen consumption.
Hormone levels
Conrad (Conrad 2007) obtained blood samples for the participants before and after the intervention to measure concentrations of dehydroepiandrosterone (DHEAS), growth hormone, epinephrine, norepinephrine, adrenocorticotrophic hormone (ACTH), cortisol, interleukin‐6 (IL‐6), prolactin, and prolactin monomer. Conrad examined the effects of music listening on these hormone levels in an attempt to elucidate the physiological mechanisms by which music may have a stress‐reducing effect. The specific neuroendocrine outcomes were selected based on current literature on the human neurohormonal stress response (Conrad 2007). Significant differences were found between the music and the control groups for DHEAS (P = 0.011), growth hormone (P = 0.032), IL‐6 (P = 0.028), and epinephrine (P = 0.014). No significant between‐group differences were found for prolactin (P = 0.27), prolactin monomer (P = 0.08), norepinephrine (P = 0.22), ACTH (P = 0.36), or cortisol (P = 0.92). The sample size in this study was very small (N = 10) and no means and SDs were reported.
Likewise, Beaulieu‐Boire and colleagues (Beaulieu‐Boire 2013) examined the impact of music listening on hormone levels. Study outcomes included cortisol, ACTH/cortisol ratios, prolactin, IL‐6, C‐reactive protein (CRP), and methionine‐enkephalin content (MET‐enkephalin). The results indicated that cortisol levels decreased in the music listening group (mean ± SD: 815 ± 126 at pre‐test, 727 ± 98 nmol/L at post‐test) but not in the control group (741 ± 71 at pre‐test, 746 ± 68 nmol/L at post‐test) and this difference between the groups was statistically significant (P < 0.05). ACTH/cortisol ratios increased in the music listening group (+0.04 ± 0.016) but not in the control group (‐0.028 ± 0.02) (P = 0.015). Music listening decreased blood prolactin levels (29.3 ± 3.5 μg/L at pre‐test, 27.4 ± 3.4 μg/L at post‐test) while no changes were found in the control group (28.8 ± 4.1 μg/L at pre‐test, 28.4 ± 4 μg/L at post‐test) (P < 0.05). Blood leptin and MET‐enkephalin were not affected by music listening (leptin: 19 ± 4 ng/mL at pre‐test, 19.6 ± 4 ng/mL at post‐test; MET‐enkephalin: 251 ± 63 pg/mL at pre‐test, 252 ± 68 pg/mL at post‐test). Finally, CRP levels did not change in the music condition or the control condition whereas IL‐6 decreased in the music condition but this was not statistically significant (158 ± 29 pg/mL at pre‐test, 147 ± 29 pg/mL at post‐test, P = 0.11).
Chlan (Chlan 2007a) also obtained serum levels of stress hormones, including epinephrine, norepinephrine, corticotropin, and cortisol, but found no significant differences between the music group (N = 5) and the control group (N = 5). Chlan suspected that the results were influenced by the fact that two participants in the music group needed endotracheal suctioning before the blood sample was obtained. In addition, five participants in the rest control group received intravenous morphine sulfate immediately prior to or during the implementation of the protocol, potentially influencing the epinephrine and norepinephrine levels.
In a later study, Chlan and colleagues (Chlan 2013) examined the effects of patient‐directed music (PDM) listening on urine free cortisol (UFC) levels in 65 mechanically ventilated participants. PDM did not result in greater reductions in UFC compared to the control group. The authors reported that the lack of statistical significance was likely due to the small sample size and the large variability among participants in UFC levels. Patterns of UFC in the music group did suggest a potential buffering effect as evidenced by less extreme values over time as compared to the increased UFC levels in the control group.
Mortality
Two studies reported data on mortality rates (Dijkstra 2010; Han 2010) during the hospital stay. Results suggested that music interventions did not have a statistically significant effect on mortality (RR 0.76, 95% CI 0.38 to 1.51, P = 0.43) (Analysis 1.10).
No studies were identified that addressed the other secondary outcomes listed in the protocol, namely quality of life, patient satisfaction, post‐discharge patient outcomes, and cost‐effectiveness.
Discussion
Summary of main results
State anxiety
The results of six studies suggest that music listening may have a beneficial effect on anxiety in mechanically ventilated patients. Although the magnitude of the effect differed across the studies, the trials agreed on the direction of the point estimates. This anxiety‐reducing result (SMD ‐1.11) is considered large in size according to interpretation guidelines put forth by Cohen (Cohen 1988). Cohen suggested that an effect size of 0.2 be considered a small effect, an effect size of 0.5 medium, and an effect size of 0.8 large.
Sedative and analgesic drug intake
One large‐scale study reported a decrease in intake of sedatives and analgesics and one study reported a trend toward reduction in daily fentanyl consumption. A third study examined sedation levels of participants and found that music listening resulted in significantly higher levels of sedation after one session.
Physiological outcomes
The results of this review indicate that listening to music reduces heart rate but the results were not consistent across studies. Music listening reduces respiratory rate consistently across studies. A reduction in these physiological responses is considered indicative of a relaxation response.
Mixed results were found for blood pressure. According to six studies, music listening consistently reduces systolic blood pressure. However, those same studies found no strong evidence for the effect of music on diastolic blood pressure. Based on the results of three studies, no strong evidence was found for an effect of music listening on mean arterial pressure. These results indicate that the physiology underlying haemodynamic responses in mechanically ventilated patients is complicated and may be confounded by ventilator settings as well as medications.
Music listening did not improve oxygen saturation levels according to five studies. However, one could question the usefulness of oxygen saturation as an indicator of a relaxation response in mechanically ventilated patients as this outcome is greatly influenced by ventilator settings.
Mixed results were found for blood hormone levels with one study reporting greater improvements in the music listening group for DHEAS, growth hormone, IL‐6, and epinephrine but not for prolactin, norepinephrine, ACTH, or cortisol. The lack of effect of music listening on cortisol (urinary free cortisol) was supported by another small study. However, a third study with a much larger sample size reported beneficial effects for music listening on cortisol, ACTH/cortisol ratios, and prolactin but not on leptin, MET‐enkephalin, or IL‐6.
Finally, two studies reported on mortality rates. No strong evidence was found for an effect of music listening.
No studies could be found that examined the effects of music interventions on quality of life, patient satisfaction, post‐discharge outcomes, and cost‐effectiveness in mechanically ventilated patients.
Overall completeness and applicability of evidence
Results of this review indicate that music listening consistently reduces anxiety in mechanically ventilated patients and this difference is considered large and clinically significant. This relaxation response is supported, in part, by results of the effects of music listening on physiological responses. In addition, some trials suggested a beneficial effect of music listening on sedative and analgesic drugs intake but more research is needed in this area before this evidence can influence clinical decision‐making.
All but one trial (Phillips 2007) used listening to pre‐recorded music as the clinical intervention and were categorized as music medicine intervention trials. This prevented us from addressing the third objective of this review, namely to compare the effects of different types of music interventions. It remains unclear whether music therapy interventions, using live music to meet specific in‐the‐moment needs of the patients, are more effective than listening to pre‐recorded music. Furthermore, most trials used patient‐selected music. Therefore, we could not address the second objective of this review, namely to compare the use of patient‐selected versus researcher‐selected music.
All but three trials (Beaulieu‐Boire 2013; Chlan 2013; Dijkstra 2010) used one music intervention session. In the original review we posed questions about the relationship between the frequency and duration of treatment and treatment effect, and recommended further investigation into the optimal frequency and duration of music interventions for critically ill patients. Chlan and colleagues (Chlan 2013) conducted a study examining this very question. In their study, patients were asked to self‐direct the use of music for anxiety management; they could listen to music whenever they wanted and for as long as they desired. Participants used headphones that contained a data logger system to capture each PDM session and the total daily music listening time. Participants listened to music for an average 79.8 (SD = 126) minutes per day. The authors presented statistical modelling results that suggested that sedation frequency decreased by an average of 0.17 points per day for all patients, regardless of group assignment. However, for patients in the music listening group the dose frequency decreased by another 0.21 points per day. Frequency dose was furthermore influenced by age and gender. The authors explained that their patient‐directed music (PDM) protocol was modelled on the patient‐controlled analgesia (PCA) intervention, an intervention that has been shown to result in better pain control and patient satisfaction (Chlan 2013). The authors continued that the PDM protocol "empowers patients in their own anxiety management" (p. 2340). The results of this study suggested that patients, on average, opt to listen to music more or longer, or both, than what has been implemented in other research studies (namely one 30‐minute session).
Presently, no data can be provided regarding costs or cost‐effectiveness of music medicine applications in the care of mechanically ventilated patients as these data were not included in the studies reviewed. Furthermore, no data were provided regarding costs for music therapy interventions; therefore, no comparisons can be conducted between these two types of treatments. It is recommended that future research include cost‐effectiveness measures of these two interventions as well as cost comparisons between them.
Trials included in the original review, in general, included very limited information about the music selections used, except for mentioning general music styles (for example, classical, easy listening, jazz, country). Several trials included in the update of this review reported greater details about the music selections that were used. Because music within each music style can vary widely, it is important that researchers continue to provide detailed information regarding music selections as this is useful for clinical decision‐making. Details on specific music selections for each study can be found in the Characteristics of included studies table.
None of the studies included children. Therefore, these results cannot be generalized to a paediatric population.
Because little information was provided in these studies about the ethnic make‐up of the patient samples, one can question the generalizability of these results to various ethnic groups. Persons' cultures may influence their music preferences and their potential acceptance and use of music as a therapeutic agent, especially during high‐stress medical situations such as mechanical ventilation. This in turn may influence the anxiety‐reducing potential of music, in greater or lesser degrees.
Quality of the evidence
In general the quality of reporting was poor, with only four studies detailing the methods of randomization and allocation concealment, and level of blinding (Beaulieu‐Boire 2013; Lee 2005; Wong 2001; Wu 2008). The chief investigators of most studies needed to be contacted to provide additional methodological and statistical information. All but one study (Beaulieu‐Boire 2013) received a high risk of bias rating.
Because of the large number of trials at high risk of bias, the findings of this review need to be interpreted with caution. It is important to be mindful that many studies received a high risk of bias rating because of lack of blinding. Often blinding of participants is not possible in music medicine or music therapy studies unless a comparative design is used (for example, comparing listening to pre‐recorded music with interactive music making with a therapist). When participants cannot be blinded to the intervention, there is definitely an opportunity for bias when participants are asked to report on subjective outcomes such as anxiety. However, this also means that trials that meet all other requirements for a low risk of bias rating are assigned a high risk of bias because of the inability to meet the blinding requirement for subjective outcomes.
For anxiety, respiratory rate, and systolic blood pressure, consistent effects were obtained across studies. For the other outcomes included in the protocol inconsistent results were obtained or not enough studies were available. Most trials that were included were small (average n = 57; range of sample size 10 to 266), except for Chlan 2013 (n = 266) and Han 2010 (n = 137). This resulted in a lack of precision of treatment effects as evidenced by the rather large confidence intervals. This, combined with the high risk of bias, requires that the results of this review be interpreted with caution.
In summary, the quality of evidence was low (summary of findings Table for the main comparison).
Potential biases in the review process
This review included 14 trials. The strength of our review is that we searched all available databases and a large number of music therapy journals (in English, German, and French language), checked reference lists of all relevant trials, contacted relevant experts for identification of unpublished trials, and included publications without restricting language. In spite of such a comprehensive search, it is still possible we missed some published and unpublished trials. We requested additional data, where necessary, for all trials we considered for inclusion. This allowed us to get accurate information on the trial quality and data for most trials, and helped us make well‐informed trial selection decisions.
It is possible that we did not identify some grey literature; however, it is doubtful that this would have had a significant impact on our results. Grey literature tends to include trials with relatively small numbers of participants and inconclusive results (McAuley 2000).
Agreements and disagreements with other studies or reviews
A review by Davis and Jones (Davis 2012) detailed study characteristics and statistical findings of seven individual clinical trials (English language only) on the use of music interventions with mechanically ventilated patients. The review authors did not provide a reason for not applying meta‐analytic procedures to the study results. They concluded that "music therapy in ventilated patients is a safe and effective treatment" (p. 165). They recommended that future studies should investigate the impact of different music styles, and duration, and frequency of music listening. They furthermore recommended that future randomized controlled trials measure outcomes related to number of ventilator days, ICU stay, and hospital length of stay.
One review article (Austin 2010) on the use of music with paediatric patients on mechanical ventilation reported that no clinical trials with this population could be identified. The author did report on a music therapy case study with two children on mechanical ventilation and one clinical trial with cardiac paediatric patients in the ICU. Austin concluded that the lack of evidence on the use of music with mechanically ventilated paediatric patients, and the inability to generalize the results of clinical trials from adult to paediatric populations, prevented reaching conclusions about the effectiveness of music interventions with mechanically ventilated paediatric patients.
The aim of this review was to update the previous version (Bradt 2010) with the results of trials completed during the three years since its publication. Overall, the results of this review are similar to those of the previous version. The findings on state anxiety were strengthened because of additional studies. In addition, whereas there was no strong evidence for an effect on blood pressure in the previous review, the results of the updated review indicate a beneficial effect of music listening on systolic blood pressure. The review was expanded with some additional outcomes, namely sedative and analgesic intake, mean arterial pressure, and mortality. However, at this time, there were not enough studies to provide strong evidence for an effect of music interventions on these outcomes.
The anxiety‐reducing effects of music interventions found in this review are consistent with the findings of three other Cochrane systematic reviews on the use of music with coronary heart disease patients (Bradt 2013b), cancer patients (Bradt 2011), and pre‐surgical patients (Bradt 2013a).
Study Flow Diagram ‐ Original Review.

Study flow diagram ‐ updated review.
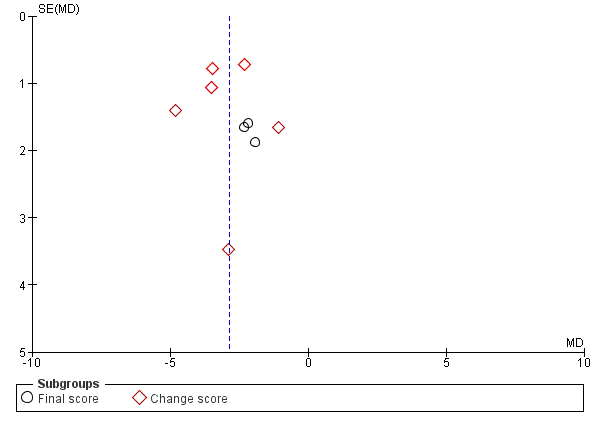
Funnel plot of comparison: 1 Music versus standard care, outcome: 1.4 Respiratory rate.
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
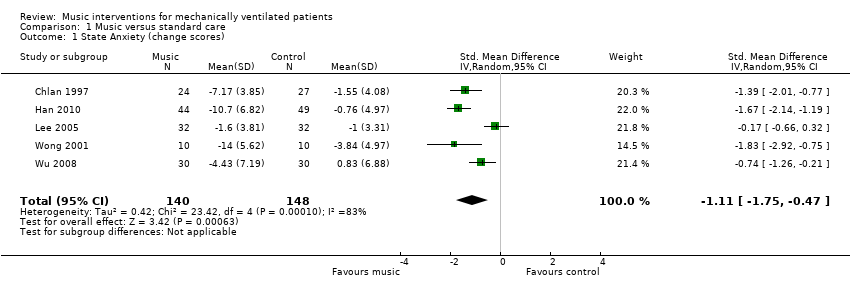
Comparison 1 Music versus standard care, Outcome 1 State Anxiety (change scores).
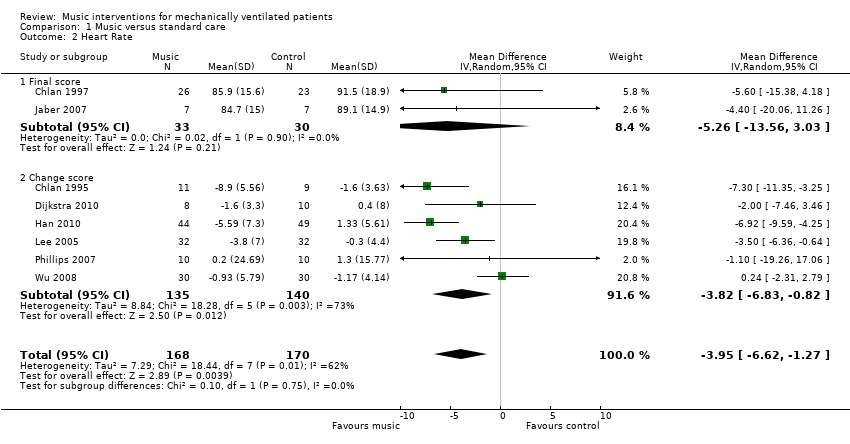
Comparison 1 Music versus standard care, Outcome 2 Heart Rate.
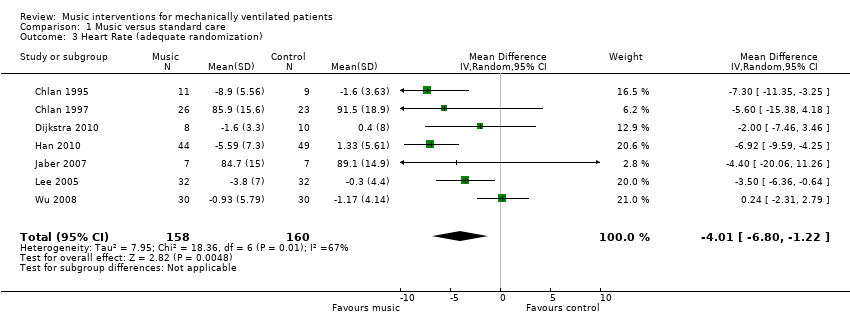
Comparison 1 Music versus standard care, Outcome 3 Heart Rate (adequate randomization).

Comparison 1 Music versus standard care, Outcome 4 Respiratory Rate.

Comparison 1 Music versus standard care, Outcome 5 Respiratory Rate (adequate randomization).

Comparison 1 Music versus standard care, Outcome 6 Systolic Blood Pressure.
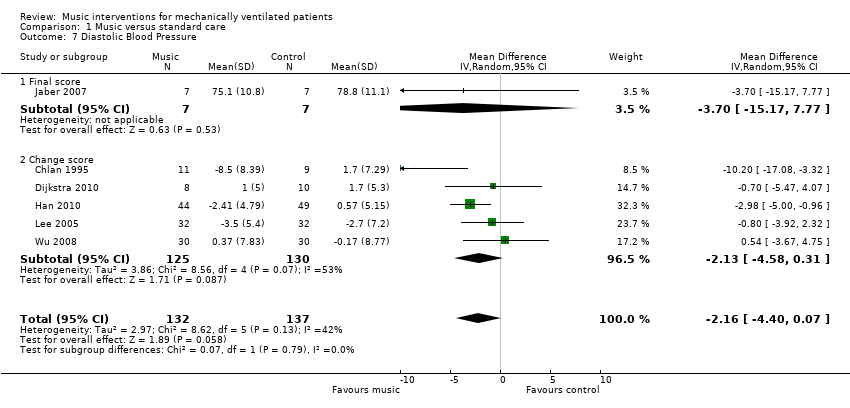
Comparison 1 Music versus standard care, Outcome 7 Diastolic Blood Pressure.
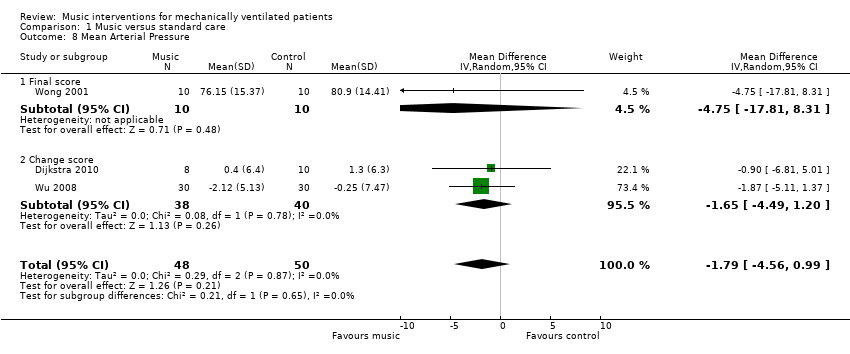
Comparison 1 Music versus standard care, Outcome 8 Mean Arterial Pressure.
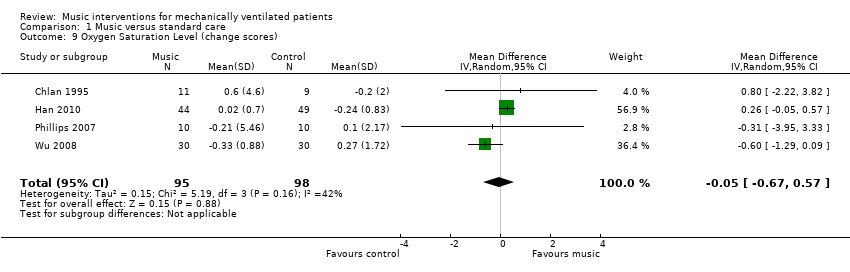
Comparison 1 Music versus standard care, Outcome 9 Oxygen Saturation Level (change scores).
Comparison 1 Music versus standard care, Outcome 10 Mortality.
| Music compared to standard care for mechanically ventilated patients | |||
| Patient or population: mechanically ventilated patients | |||
| Outcomes | Relative effect | No of participants | Quality of the evidence |
| State anxiety | The mean state anxiety in the intervention groups was | 288 | ⊕⊕⊝⊝ |
| Heart rate | The mean heart rate in the intervention groups was | 338 | ⊕⊝⊝⊝ |
| Respiratory rate | The mean respiratory rate in the intervention groups was | 357 | ⊕⊝⊝⊝ |
| Systolic blood pressure mmHg | The mean systolic blood pressure in the intervention groups was | 269 | ⊕⊝⊝⊝ |
| Diastolic blood pressure mmHg | The mean diastolic blood pressure in the intervention groups was | 269 | ⊕⊝⊝⊝ |
| Mean arterial pressure mmHg | The mean arterial pressure in the intervention groups was | 98 | ⊕⊝⊝⊝ |
| Oxygen saturation level | The mean oxygen saturation level in the intervention groups was | 193 | ⊕⊕⊝⊝ |
| CI: Confidence interval | |||
| GRADE Working Group grades of evidence | |||
| 1 The majority of the trials were assessed as high risk of bias studies | |||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 State Anxiety (change scores) Show forest plot | 5 | 288 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.11 [‐1.75, ‐0.47] |
| 2 Heart Rate Show forest plot | 8 | 338 | Mean Difference (IV, Random, 95% CI) | ‐3.95 [‐6.62, ‐1.27] |
| 2.1 Final score | 2 | 63 | Mean Difference (IV, Random, 95% CI) | ‐5.26 [‐13.56, 3.03] |
| 2.2 Change score | 6 | 275 | Mean Difference (IV, Random, 95% CI) | ‐3.82 [‐6.83, ‐0.82] |
| 3 Heart Rate (adequate randomization) Show forest plot | 7 | 318 | Mean Difference (IV, Random, 95% CI) | ‐4.01 [‐6.80, ‐1.22] |
| 4 Respiratory Rate Show forest plot | 9 | 357 | Mean Difference (IV, Random, 95% CI) | ‐2.87 [‐3.64, ‐2.10] |
| 4.1 Final score | 3 | 83 | Mean Difference (IV, Random, 95% CI) | ‐2.14 [‐4.06, ‐0.22] |
| 4.2 Change score | 6 | 274 | Mean Difference (IV, Random, 95% CI) | ‐3.01 [‐3.85, ‐2.17] |
| 5 Respiratory Rate (adequate randomization) Show forest plot | 8 | 337 | Mean Difference (IV, Random, 95% CI) | ‐2.87 [‐3.64, ‐2.09] |
| 6 Systolic Blood Pressure Show forest plot | 6 | 269 | Mean Difference (IV, Random, 95% CI) | ‐4.22 [‐6.38, ‐2.06] |
| 6.1 Final score | 1 | 14 | Mean Difference (IV, Random, 95% CI) | ‐9.0 [‐22.40, 4.40] |
| 6.2 Change score | 5 | 255 | Mean Difference (IV, Random, 95% CI) | ‐4.09 [‐6.28, ‐1.90] |
| 7 Diastolic Blood Pressure Show forest plot | 6 | 269 | Mean Difference (IV, Random, 95% CI) | ‐2.16 [‐4.40, 0.07] |
| 7.1 Final score | 1 | 14 | Mean Difference (IV, Random, 95% CI) | ‐3.70 [‐15.17, 7.77] |
| 7.2 Change score | 5 | 255 | Mean Difference (IV, Random, 95% CI) | ‐2.13 [‐4.58, 0.31] |
| 8 Mean Arterial Pressure Show forest plot | 3 | 98 | Mean Difference (IV, Random, 95% CI) | ‐1.79 [‐4.56, 0.99] |
| 8.1 Final score | 1 | 20 | Mean Difference (IV, Random, 95% CI) | ‐4.75 [‐17.81, 8.31] |
| 8.2 Change score | 2 | 78 | Mean Difference (IV, Random, 95% CI) | ‐1.65 [‐4.49, 1.20] |
| 9 Oxygen Saturation Level (change scores) Show forest plot | 4 | 193 | Mean Difference (IV, Random, 95% CI) | ‐0.05 [‐0.67, 0.57] |
| 10 Mortality Show forest plot | 2 | 271 | Risk Ratio (M‐H, Random, 95% CI) | 0.76 [0.38, 1.51] |

