Uso de paños adhesivos plásticos durante la cirugía para la prevención de la infección del sitio quirúrgico
Referencias
References to studies included in this review
References to studies excluded from this review
Additional references
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Ir a:
| Methods | Study type: single‐centre RCT | |
| Participants | People undergoing acute hip fracture surgery | |
| Interventions | Opsite (Smith & Nephew) adhesive plastic incisional drapes compared with no incisional drapes | |
| Outcomes | Surgical wound infection (reported as deep and superficial infection). No definition of infection provided | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method not described |
| Allocation concealment (selection bias) | Unclear risk | Method not described |
| Blinding (performance bias and detection bias) | High risk | Masking was impossible for surgeons |
| Incomplete outcome data (attrition bias) | Low risk | The authors state that 120 patients were enrolled and results were available for all of these patients. No mention of intention‐to‐treat analysis was made |
| Selective reporting (reporting bias) | Low risk | Results for all expected outcomes were reported |
| Other bias | Low risk | No competing interests were declared. Although no data were shown, the authors stated that patients were matched for relevant risk factors at baseline |
| Methods | Study type: multi‐centre RCT | |
| Participants | Women undergoing caesarean section. Includes infected and possibly infected cases | |
| Interventions | Adhesive plastic incisional drapes compared with no adhesive plastic incisional drapes | |
| Outcomes | Surgical wound infection (defined as possibly infected if there was localised erythema and/or serous secretion without the presence of pus) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random allocation, using block design, in blocks of eight |
| Allocation concealment (selection bias) | Unclear risk | Not described. However, the study, which included eight hospitals, was carried out under the supervision of the Danish National Centre for Hospital Hygiene, so it is likely that an appropriate method of allocation concealment was used |
| Blinding (performance bias and detection bias) | High risk | Masking was impossible for surgeons |
| Incomplete outcome data (attrition bias) | Low risk | 64 patients were excluded before randomisation but details by group were not provided. No mention of intention‐to‐treat analysis was made |
| Selective reporting (reporting bias) | Low risk | Results for all expected outcomes were reported |
| Other bias | Low risk | No competing interests declared. No baseline data reported |
| Methods | Study type: single‐centre RCT | |
| Participants | People undergoing general surgery | |
| Interventions | Ioban (3M Company) iodine‐impregnated adhesive plastic incisional drapes compared with no incisional drapes | |
| Outcomes | Surgical wound infection (defined as a wound that discharged pus or if the fluid discharging from the wound was associated with a positive bacterial culture or if erythema was present more than 1cm lateral to the wound) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number table |
| Allocation concealment (selection bias) | Low risk | Surgeons sequentially selected the allocation from the random numbers table located in the operating room Consequently, surgeons would have been aware of the next allocation |
| Blinding (performance bias and detection bias) | High risk | Masking was impossible for surgeons |
| Incomplete outcome data (attrition bias) | Low risk | 86 (7.8%) patients were excluded after randomisation (40 for incomplete records and 46 because they were unable to be followed up for the three‐week period considered necessary). These were not displayed by group |
| Selective reporting (reporting bias) | Low risk | Results for all expected outcomes were reported |
| Other bias | Low risk | No competing interests declared. Patients equally distributed for all major risk factors for surgical site infection |
| Methods | Study type: single‐centre RCT | |
| Participants | People undergoing general surgery | |
| Interventions | Adhesive plastic incisional drapes (Band‐aid) compared with no adhesive plastic incisional drapes | |
| Outcomes | Surgical wound infection (defined as a wound discharging pus and included stitch abscess) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Spin of a coin |
| Allocation concealment (selection bias) | Low risk | The coin was 'spun' at the beginning of the operation. Allocation would have been concealed until then and the next allocation would be unpredictable |
| Blinding (performance bias and detection bias) | High risk | Masking was impossible for surgeons |
| Incomplete outcome data (attrition bias) | Low risk | Follow‐up data was reported on all enrolled participants |
| Selective reporting (reporting bias) | Low risk | Results for all expected outcomes were reported |
| Other bias | Unclear risk | The investigators "concurrently ran a test of an antibiotic spray in random cases." Results were to be reported separately. It is unclear if the spray was used equally between groups |
| Methods | Study type: Single‐centre RCT | |
| Participants | People undergoing abdominal surgery | |
| Interventions | Adhesive plastic incisional drapes compared with no adhesive plastic incisional drapes and a ring drape | |
| Outcomes | Surgical wound infection (defined as erythema around sutures or wound edge with an accompanying pyrexia; | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method not described |
| Allocation concealment (selection bias) | Unclear risk | Method not described |
| Blinding (performance bias and detection bias) | High risk | Masking was impossible for surgeons |
| Incomplete outcome data (attrition bias) | Low risk | All enrolled patients were accounted for in the results |
| Selective reporting (reporting bias) | Low risk | Results for all expected outcomes were reported |
| Other bias | Unclear risk | No baseline data were reported. No competing interests reported |
| Methods | Study type: single‐centre RCT | |
| Participants | People at high risk undergoing cardiac surgery | |
| Interventions | Iodine‐impregnated adhesive plastic incisional drapes compared with no incisional drapes | |
| Outcomes | Surgical wound infection. No clear definition of infection but included drainage, redness, tenderness or instability | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Pieces of paper marked with equal numbers of the different allocations were placed in a sack |
| Allocation concealment (selection bias) | Low risk | When an eligible patient was identified, a piece of paper containing the allocation was drawn out of the sack by the operating room Charge Nurse |
| Blinding (performance bias and detection bias) | High risk | Masking was impossible for surgeons |
| Incomplete outcome data (attrition bias) | Low risk | All enrolled patients were followed up |
| Selective reporting (reporting bias) | Low risk | Results for all expected outcomes were reported |
| Other bias | Low risk | Patients equal at baseline for risk factors (communication with authors). No competing interests |
| Methods | Study type: single‐centre RCT | |
| Participants | Women undergoing caesarean section | |
| Interventions | Incise (Smith & Nephew) adhesive plastic incisional drapes compared with no adhesive plastic incisional drapes | |
| Outcomes | Surgical wound infection (defined as having to include 2 of the following: erythema around sutures or wound edge; seropurulent discharge from the wound; positive swab culture) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number table |
| Allocation concealment (selection bias) | Low risk | Allocation contained in opaque unmarked envelope |
| Blinding (performance bias and detection bias) | Low risk | Masking was impossible for surgeons |
| Incomplete outcome data (attrition bias) | Low risk | Of the 620 patients randomised, 15 (2.4%) had critical data missing from their records and a further two patients were excluded, one for an existing infection and one for early discharge |
| Selective reporting (reporting bias) | Low risk | Results for all expected outcomes were reported |
| Other bias | Unclear risk | Patients were only followed up for 5 days; some infections would have occurred after this time. Baseline risk factors were equally distributed between groups |
Characteristics of excluded studies [ordered by study ID]
Ir a:
| Study | Reason for exclusion |
| Not a RCT | |
| Not a RCT | |
| Not a RCT | |
| Did not report wound infection rate | |
| Did not report wound infection rate | |
| Did not report wound infection rate | |
| Number of participants in each treatment arm not reported | |
| Did not report wound infection rate | |
| Not a RCT | |
| Plastic incisional drape not used | |
| Plastic incisional drape not used | |
| Not a RCT | |
| Plastic incisional drape not used | |
| Not a RCT |
RCT: randomised controlled trial
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Surgical site infection (all wound classifications) Show forest plot | 5 | 3082 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.23 [1.02, 1.48] |
| Analysis 1.1  Comparison 1 Adhesive drapes versus no adhesive drapes, Outcome 1 Surgical site infection (all wound classifications). | ||||
| 2 Surgical site infection (by wound classification) Show forest plot | 1 | 921 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.20 [0.86, 1.66] |
| Analysis 1.2  Comparison 1 Adhesive drapes versus no adhesive drapes, Outcome 2 Surgical site infection (by wound classification). | ||||
| 2.1 Clean | 1 | 363 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.37 [0.53, 3.53] |
| 2.2 Potentially infected | 1 | 486 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.24 [0.80, 1.92] |
| 2.3 Infected | 1 | 72 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.60, 1.75] |
| 3 Length of hospital stay Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.3  Comparison 1 Adhesive drapes versus no adhesive drapes, Outcome 3 Length of hospital stay. | ||||
| 3.1 Infected wound | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 No infected wound | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Surgical site infection Show forest plot | 2 | 1113 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.66, 1.60] |
| Analysis 2.1  Comparison 2 Iodine‐impregnated adhesive drapes versus no adhesive drapes, Outcome 1 Surgical site infection. | ||||
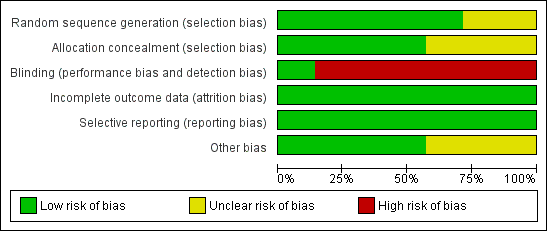
Methodological quality graph: review authors' judgements about each methodological quality item presented as percentages across all included studies.

Methodological quality summary: review authors' judgements about each methodological quality item for each included study.
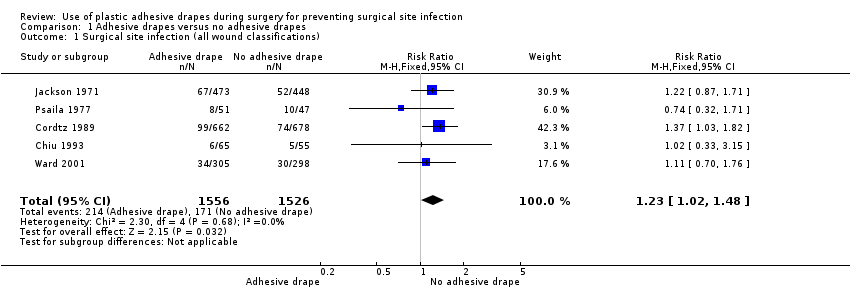
Comparison 1 Adhesive drapes versus no adhesive drapes, Outcome 1 Surgical site infection (all wound classifications).

Comparison 1 Adhesive drapes versus no adhesive drapes, Outcome 2 Surgical site infection (by wound classification).

Comparison 1 Adhesive drapes versus no adhesive drapes, Outcome 3 Length of hospital stay.
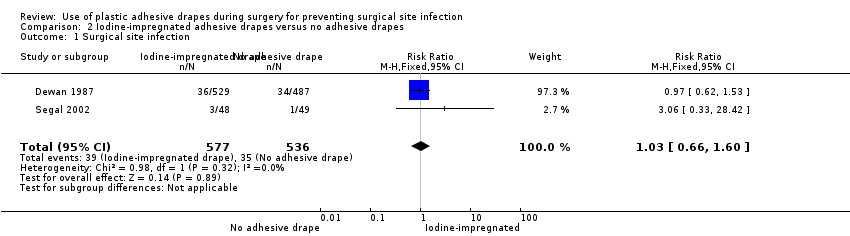
Comparison 2 Iodine‐impregnated adhesive drapes versus no adhesive drapes, Outcome 1 Surgical site infection.
| Adhesive drapes compared with no adhesive drapes for preventing surgical site infection | ||||||
| Patient or population: Patients undergoing surgery Comparison: No adhesive drapes | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No. of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Adhesive drapes versus no adhesive drapes | |||||
| Surgical site infection (all wound classifications) | Medium risk population | RR 1.23 | 3082 | ⊕⊕⊕⊕ | ||
| 109 per 1000 | 134 per 1000 | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Various definitions of infection were used; we accepted the authors definition in each case. | ||||||
| Iodophore‐impregnated adhesive drapes compared with no adhesive drapes for preventing surgical site infection | ||||||
| Patient or population: Patients undergoing surgery | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No. of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| No adhesive drapes | Iodophore‐impregnated adhesive drapes | |||||
| Surgical site infection | Medium risk population | RR 1.03 | 1113 | ⊕⊕⊕⊝ | ||
| 45 per 1000 | 46 per 1000 | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 A number of definitions of wound infection were used across the trials. We accepted the authors definition in all cases. | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Surgical site infection (all wound classifications) Show forest plot | 5 | 3082 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.23 [1.02, 1.48] |
| 2 Surgical site infection (by wound classification) Show forest plot | 1 | 921 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.20 [0.86, 1.66] |
| 2.1 Clean | 1 | 363 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.37 [0.53, 3.53] |
| 2.2 Potentially infected | 1 | 486 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.24 [0.80, 1.92] |
| 2.3 Infected | 1 | 72 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.60, 1.75] |
| 3 Length of hospital stay Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3.1 Infected wound | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 No infected wound | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Surgical site infection Show forest plot | 2 | 1113 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.66, 1.60] |

