Grabado del esmalte para adherir los aparatos ortodónticos fijos
Resumen
Antecedentes
El grabado de las superficies del diente con ácido para promover la adhesión de los ataches ortodónticos al esmalte ha sido un procedimiento habitual en el tratamiento ortodóntico desde los años sesenta. En las últimas cinco décadas, se han introducido diversos tipos de agentes de grabado ortodónticos y técnicas de grabado. Aunque se ha publicado una gran cantidad de información sobre este tema, hay una falta significativa de consenso con respecto a los efectos clínicos de los diferentes agentes de grabado dentales y las distintas técnicas de grabado.
Objetivos
Comparar los efectos de diferentes agentes de grabado dentales y diferentes técnicas de grabado para adherir los aparatos ortodónticos fijos.
Métodos de búsqueda
Se realizaron búsquedas en las siguientes bases de datos electrónicas: registro de ensayos del Grupo Cochrane de Salud Oral (Cochrane Oral Health Group) (hasta el 8 marzo 2013), Registro Cochrane Central de Ensayos Controlados (Cochrane Central Register of Controlled Trials) (CENTRAL) (The Cochrane Library 2013, número 2), MEDLINE vía OVID (hasta el 8 marzo 2013), EMBASE vía OVID (hasta el 8 marzo 2013), Chinese Biomedical Literature Database (hasta el 12 marzo 2011), la WHO International Clinical Trials Registry Platform (hasta el 8 marzo 2013) y el National Institutes of Health Clinical Trials Registry (hasta el 8 marzo 2013). Un grupo de búsqueda manual actualizó la búsqueda manual de las revistas, la cual se realizó como parte del Cochrane Worldwide Handsearching Programme, hasta el número más actual. No hubo restricciones en cuanto al idioma o fecha de publicación.
Criterios de selección
Ensayos controlados aleatorizados (ECA) que compararan diferentes materiales de grabado, o diferentes técnicas de grabado que utilizaran los mismos agentes de grabado, para adherir los brackets ortodónticos fijos a los incisivos, los caninos y los premolares en niños y adultos.
Obtención y análisis de los datos
Dos autores de la revisión extrajeron los datos y evaluaron el riesgo de sesgo de los estudios incluidos de forma independiente y por duplicado. Los desacuerdos se resolvieron mediante discusión entre el equipo de revisión. Si fue necesario, se estableció contacto con los autores correspondientes de los estudios incluidos para obtener información adicional.
Resultados principales
Se incluyeron 13 estudios que asignaron al azar a 417 participantes con 7184 dientes/brackets. Dos estudios (15%) se evaluaron como en riesgo bajo de sesgo, diez estudios (77%) como en riesgo alto de sesgo y un estudio (8%) como en riesgo incierto de sesgo.
Autograbantes versus agentes de grabado convencionales
Once estudios compararon los efectos de los autograbantes con los agentes de grabado convencionales. Sólo cinco de estos estudios (tres de diseño de boca dividida y dos de diseño paralelo) informaron los datos a nivel de los participantes, y los estudios restantes informaron a nivel del diente, por lo cual omitieron el agrupamiento/la naturaleza pareada de los datos. Un metanálisis de estos cinco estudios, con un seguimiento que varió de cinco a 37 meses, proporcionó evidencia de baja calidad que fue insuficiente para determinar si hay diferencias en la tasa de fracaso de la adhesión entre los autograbantes y los agentes de grabado convencionales (riesgos relativos 1,14; intervalo de confianza (IC) del 95%: 0,75 a 1,73; 221 participantes). Las dudas en cuanto a los IC incluyen tanto ningún efecto como efectos beneficiosos y perjudiciales apreciables. El análisis de subgrupos no demostró diferencias entre los estudios de boca dividida y los estudios paralelos.
No se disponía de datos que permitieran evaluar los resultados: descalcificación, satisfacción de los participantes y costo‐efectividad. Un estudio informó sobre la descalcificación, aunque sólo a nivel del diente.
Autograbantes versus autograbantes
Dos estudios compararon dos autograbantes diferentes. Ambos estudios informaron la tasa de fracaso de la adhesión, y uno de los estudios también informó sobre la descalcificación. Sin embargo, debido a que ambos estudios informaron los resultados sólo a nivel del diente, no hubo datos disponibles para evaluar la superioridad de ninguno de los autograbantes sobre los otros investigados con respecto a cualquiera de los resultados de esta revisión.
No se encontraron estudios aptos que evaluaran diferentes materiales de grabado (p.ej., ácido fosfórico, ácido poliacrílico, ácido maléico), concentraciones o tiempo de grabado.
Conclusiones de los autores
Se encontró evidencia de baja calidad que fue insuficiente para establecer la conclusión de si existe una diferencia en la tasa de fracaso de la adhesión entre los autograbantes y los sistemas de grabado convencional al adherir aparatos ortodónticos fijos durante un seguimiento de cinco a 37 meses. Tampoco se disponía de datos suficientes para poder extraer conclusiones sobre la superioridad de los autograbantes o el grabado convencional para los resultados: descalcificación, satisfacción de los participantes y eficacia en función de los costos, o sobre la superioridad de los diferentes materiales, concentraciones o tiempos de grabado, o de cualquiera de los autograbantes sobre otro. Se necesitan ECA adicionales bien diseñados sobre este tema para aportar más evidencia y responder a estas preguntas clínicas.
PICO
Resumen en términos sencillos
Preparación de las superficies del diente para adherir los aparatos ortodónticos fijos
Pregunta de la revisión
La principal pregunta que se aborda en esta revisión es: ¿cuál es el mejor método para preparar el esmalte de la superficie de los dientes con objeto de mejorar la adhesión de los aparatos ortodónticos fijos?
Antecedentes
Muchas personas necesitan usar dispositivos ortodónticos fijos, como ortodoncias, para corregir problemas con los dientes y la mandíbula (p.ej., el apiñamiento o los dientes frontales que sobresalen o que se encuentran retroinclinados). La forma en que se fijan estas ortodoncias será de interés para dichos pacientes. Para adherir un dispositivo ortodóntico, como una ortodoncia, a un diente, en primer lugar, debe prepararse la superficie del diente pertinente para que pueda retener el pegamento o el agente adhesivo utilizado con objeto de permitir que el dispositivo se adhiera de un modo seguro. Durante los últimos 50 años, la forma habitual de realizar dicho procedimiento ha sido grabar (volver áspera) la superficie del diente con ácido, comúnmente ácido fosfórico, aunque a veces también se utiliza ácido maléico o ácido poliacrílico. Los daños posibles del grabado incluyen la pérdida permanente del esmalte (superficie dura) de la superficie del diente, lo cual lo hace más propenso a perder calcio o a debilitarse durante y después del tratamiento. Recientemente, para reducir la duración y la complejidad del proceso, se ha desarrollado una técnica que utiliza autograbantes como una alternativa a los agentes de grabado o a los ácidos convencionales. Sin embargo, aún debe determinarse si los autograbantes o los agentes de grabado convencionales son mejores, y el autograbante, el ácido, la concentración y el tiempo de grabado más adecuados.
Características de los estudios
El Grupo Cochrane de Salud Oral (Cochrane Oral Health Group) realizó esta revisión de los estudios existentes, que incluye evidencia actual hasta el 8 de marzo de 2013. Esta revisión incluye 13 estudios publicados en los cuales un total de 417 niños y adultos recibieron al azar preparaciones diferentes de los dientes antes de adherir los aparatos ortodónticos fijos a los dientes. Once de estos estudios compararon autograbantes con grabado convencional, y dos compararon dos autograbantes diferentes.
Resultados clave
Sólo cinco de los estudios proporcionaron evidencia utilizable para esta revisión y los resultados combinados no permitieron establecer una conclusión acerca de si hay una diferencia en el fracaso de la adhesión (cuando los dispositivos ortodónticos fijos se desprenden del diente) entre los autograbantes y el grabado convencional. Tampoco hubo evidencia utilizable para sugerir si los autograbantes o los agentes de grabado convencionales dan lugar a menos caries cerca del sitio del grabado, o si se asocian con costos menores o con una mayor satisfacción de los participantes. Tampoco hubo evidencia utilizable para permitir establecer conclusiones acerca de cuál fue el autograbante, el ácido, la concentración o el tiempo de grabado más adecuado.
Calidad de la evidencia
La evidencia presentada es de baja calidad debido a cuestiones relacionadas con la forma en la cual se realizaron algunos de los estudios.
Authors' conclusions
Summary of findings
| Participants or population: Children and adults with fixed orthodontic brackets Settings: Clinical (typically university dental clinics) Intervention: Self etching primers (one‐step etchant and primer system) Comparison: Conventional etchants (two‐step etch and prime method using 37% phosphoric acid) | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Conventional etchants | Self etching primers | |||||
| Bond failure rate (5 to 37 months) | 196 per 1000 | 223 per 1000 | RR 1.14 (0.75 to 1.73) | 221 | ⊕⊕⊝⊝1, 2 | Five more studies, which we were unable to include in the meta‐analysis, reported mixed results (Additional Table 2) |
| Decay (decalcification) associated with or around the etching field | Only one study (Ghiz 2009) assessed this outcome but data were reported at the tooth level rather than at the participant level and therefore was not amenable to analysis using Cochrane methods | |||||
| Participant satisfaction | No studies assessed this outcome | |||||
| Cost of treatment | No studies assessed this outcome | |||||
| Damage to the teeth | No studies assessed this outcome | |||||
| *The assumed risk is the median control group risk across studies. The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Two studies at low risk of bias, one at unclear risk, but two with serious risk of selection bias. | ||||||
Background
Description of the condition
Orthodontic treatment involves the use of both removable and fixed appliances. It is widely documented that fixed appliances are more efficient at correcting malocclusions than removable appliances (O'Brien 1993; Richmond 1993), and therefore fixed appliances are more commonly used in contemporary orthodontic practice. Fixed orthodontic treatment depends on, among other factors, the successful bonding of orthodontic brackets to tooth enamel. Conventional orthodontic bonding of a bracket using composite relies on the production, by phosphoric acid, of a reproducible etch pattern on the tooth enamel that allows mechanical retention of the adhesive (Buonocore 1955). Although composites, glass ionomers and compomers have been assessed for bracket bonding, composite resins remain the most effective and reliable adhesive available for bonding orthodontic attachments (Mandall 2003). For composite resins, both chemical and light‐cured adhesives are used routinely as part of fixed appliance therapy using conventional two‐stage enamel etching and priming (Sunna 1998). The conventional bonding of orthodontic brackets to enamel uses the etch‐and‐rinse bonding approach and provides good adhesive results. However, this bonding approach is time‐consuming because a series of steps have to be followed (Aljubouri 2004; Bishara 2001). Even though the acid etching technique is useful in orthodontics, improved techniques are needed to maintain clinically useful bond strengths while minimizing enamel loss and to simplify the technique by reducing the number of steps.
Description of the intervention
The process of etching tooth surfaces with phosphoric acid in order to bond acrylic resin to tooth enamel was first introduced in 1955 by Buonocore, who used 85% phosphoric acid for 30 seconds and reported that the bonding strength of acrylic restorative resins was significantly increased by the etching of the enamel surface (Buonocore 1955). In 1965, with the advent of epoxy resin bonding, Newman began to apply these findings to the direct bonding of orthodontic attachments (Newman 1978). It was not until 1977, however, that the first detailed post‐treatment evaluation of direct bonding over a full period of orthodontic treatment in a large sample of individuals was published. The clinical implication of this study, that acid etching and bonding would henceforth be widely accepted in orthodontics, has indeed been verified by orthodontists worldwide (Zachrisson 1977). Phosphoric acid (gel or solution) has remained the primary enamel etchant since this technique was introduced. However, other etchants such as maleic acid and polyacrylic acid have been considered as alternatives by various investigators (Olsen 1997).
The introduction of the acid‐etch bonding technique has given rise to dramatic changes in the practice of clinical orthodontics. It has several advantages, such as enhancing the ability of the individual to remove plaque, minimizing soft tissue irritation and hyperplastic gingivitis, eliminating the need for separation, facilitating the application of attachments to partially erupted teeth, eliminating post‐treatment band spaces, minimizing the risk of decalcification with loose bands, facilitating the detection and treatment of dental caries, as well as resulting in a better esthetic appearance for the recipient (Zachrisson 1976). However, it has been widely reported that permanent loss of enamel during the etching procedure may make the enamel surface more susceptible to decalcification during and after orthodontic treatment (Sadowsky 1976).
When bonding fixed orthodontic appliances to enamel, most orthodontists use a conventional technique that involves separate steps of etching and conditioning of tooth enamel. Initially the enamel is etched with etchant and then a hydrophilic primer is placed on the etched, rinsed and dried surface. The brackets are then bonded with an adhesive resin composite. This procedure has some obvious disadvantages. First, a potential problem can be contamination by saliva or from a faulty air or water syringe tip after the enamel is prepared for resin bonding using the etchant and a separate primer. Second, these multiprocedural steps can be very time consuming. Therefore, in 1998, Bishara et al applied a modified one‐step etchant‐and‐primer system to clinical orthodontics and demonstrated that use of such a system to bond orthodontic brackets to tooth enamel could provide acceptable shear bond strength (Bishara 1998). This procedure can reduce the number of procedural steps involved in the application, and decrease technique sensitivity and chair‐side time, without compromising outcome.
How the intervention might work
There is a significant lack of consensus regarding the effectiveness of different dental etchants. A 50% phosphoric acid concentration has been suggested by Retief (Retief 1973), whereas Silverstone and Gorelick consider a 30% to 50% phosphoric acid concentration ideal (Gorelick 1977; Silverstone 1974). To reduce the potential risk of significant enamel loss, various investigators have considered alternative ways of treating the enamel surface before the bonding procedure, including the use of maleic acid or polyacrylic acid (Olsen 1997; Triolo 1993). Bishara et al compared different enamel etching materials and indicated that the use of polyacrylic acid resulted in a 30% reduction in bond strength compared with the use of phosphoric acid (Bishara 1993). In the early 1990s, Barkmeier and Erickson compared the use of 10% maleic acid and 37% phosphoric acid, and reported that the resulting bond strengths were essentially similar (Barkmeier 1994).
There is still controversy as to the effectiveness of self etching primers (SEPs) compared with conventional etchants. Barkmeier et al examined the effect of Clearfil Liner Bond 2 on enamel through shear bond testing and demonstrated that the resin penetrated the enamel surface and that adequate conditioning was achieved (Barkmeier 1995). Bishara and Gordon compared the shear bond strength of orthodontic brackets attached to enamel that had been etched using 37% phosphoric acid, 10% maleic acid or an acidic primer solution and concluded that acidic primer systems used to bond orthodontic attachments to tooth enamel could provide acceptable shear bond strength (Bishara 1998). Ryan et al compared the orthodontic bonding strength of a recently developed SEP and a conventional etchant, and found no significant difference between them (Ryan 2002).
Why it is important to do this review
Although enamel etching has been widely accepted by professionals for the bonding of fixed orthodontic braces, and vast amounts of information on this topic have been published, there is a significant lack of consensus regarding the clinical efficacy and security of the application of enamel etching. Controversy remains as to: (1) the effectiveness of different dental etchants; (2) the optimal etching duration and concentration of specific etchants; (3) the effectiveness of SEPs compared with conventional etchants; and (4) the clinical efficacy of different SEPs.
Such uncertainty indicates that there is a need to evaluate the existing evidence for this procedure and identify best practice and further areas for good‐quality primary research.
Objectives
To compare the effects of different dental etchants and different etching techniques for the bonding of fixed orthodontic appliances.
Methods
Criteria for considering studies for this review
Types of studies
We included randomized controlled trials (RCTs) comparing different etching materials or different etching techniques. These include split‐mouth trials using quadrants (even if contralateral quadrants are given the same intervention) but not those randomizing individual teeth or using alternate teeth, with the initial selection of the teeth sequence being randomized.
Types of participants
We included participants, both children and adults, with fixed orthodontic brackets attached to their incisors, canines and premolars. We excluded individuals with a cleft lip or palate or both, or with other craniofacial deformities/syndromes. We also excluded those with hypoplastic or fluorotic teeth.
Types of interventions
Any kind of etching materials and techniques used in the intervention group compared with different etching materials, times and acid concentrations, or an alternative etching technique in the control group.
Types of outcome measures
We excluded studies that compared different dental etchants or different etching techniques but did not report any of the outcomes listed below.
Primary outcomes
-
Bond failure rate of braces (the rate at which braces fall off the teeth during treatment).
Secondary outcomes
-
The presence or absence of decay (decalcification) associated with or around the etching field.
-
Participant satisfaction.
-
Cost of treatment.
Search methods for identification of studies
For the identification of studies included or considered for this review, we developed detailed search strategies for each database searched. These were based on the search strategy developed for MEDLINE (OVID) but revised appropriately for each database. The search strategy used a combination of controlled vocabulary and free text terms, and was linked with the Cochrane Highly Sensitive Search Strategy for identifying RCTs in MEDLINE: sensitivity maximizing version (2008 revision), as referenced in Chapter 6.4.11.1 and detailed in Box 6.4.c of the Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (Higgins 2011). Details of the MEDLINE search are provided in Appendix 3. The search of EMBASE was linked to the Cochrane Oral Health Group filter for identifying RCTs (see Appendix 4 for details).
Electronic searches
We searched the following electronic databases for relevant studies:
-
Cochrane Oral Health Group's Trials Register (to 8 March 2013) (Appendix 1);
-
Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library 2013, Issue 2) (Appendix 2);
-
MEDLINE via OVID (1948 to 8 March 2013) (Appendix 3);
-
EMBASE via OVID (1980 to 8 March 2013) (Appendix 4);
-
WHO International Clinical Trials Registry Platform (to 8 March 2013) (Appendix 5);
-
National Institutes of Health Clinical Trials Registry (www.ClinicalTrials.gov) (to 8 March 2013) (Appendix 6);
-
Chinese Biomedical Literature Database (CBM, 1978 to 12 March 2011, in Chinese).
Cochrane Oral Heath's Information Specialist, Anne Littlewood, searched the first six databases; we searched the remainder.
Searching other resources
We searched the online abstract indices of the conference proceedings for meetings, such as the AAO (American Association of Orthodontics), IADR (International Association for Dental Research), British Orthodontic Conference and European Orthodontic Conference, to find any relevant ongoing or unpublished trials.
We contacted manufacturers and first authors of included trial reports in order to identify any unpublished or ongoing clinical trials, and to clarify data as necessary. We screened reference lists of included studies for further trials.
In June 2013, a handsearching group updated the handsearching of the following journals to the most current issue,as part of the Cochrane Worldwide Handsearching Programme:
-
American Journal of Orthodontics and Dentofacial Orthopedics (1970 to March 2012);
-
Angle Orthodontist (1978 to March 2012);
-
European Journal of Orthodontics (1979 to March 2012);
-
Journal of Orthodontics (formerly British Journal of Orthodontics) (1978 to March 2012);
-
Journal of Clinical Orthodontics (1978 to March 2012);
-
Orthodontics and Craniofacial Research (1978 to March 2012).
In addition, the following Chinese journals were handsearched within relevant fields:
-
Journal of Stomatology (1981 to June 2013);
-
Chinese Journal of Dental Material and Devices (1992 to June 2013);
-
West China Journal of Stomatology (1983 to June 2013);
-
Journal of Clinical Stomatology (1985 to June 2013);
-
Journal of Comprehensive Stomatology (1985 to June 2013);
-
Journal of Modern Stomatology (1987 to June 2013);
-
Chinese Journal of Stomatology (1953 to June 2013);
-
Beijing Journal of Stomatology (1993 to June 2013);
-
Shanghai Journal of Stomatology (1992 to June 2013).
Data collection and analysis
Selection of studies
Two review authors assessed the titles and abstracts (when available) of all studies resulting from the search, independently and in duplicate. We obtained full copies of all relevant and potentially relevant studies (those which appeared to meet the inclusion criteria), or studies for which the information in the titles and abstracts was not sufficient to make a clear decision. The same two review authors assessed full text copies independently and we resolved any disagreements on eligibility through discussion, involving a third review author where necessary. We excluded any study that did not match the inclusion criteria and their details and reasons for exclusion were noted in the Characteristics of excluded studies table. The review authors were not blinded to author(s), institution or site of publication.
Data extraction and management
Two review authors independently extracted data from the included studies using a specially designed data extraction table that was pilot‐tested on four of the included studies. Contents of the data extraction included the following.
-
Basic information of the trial: trial ID, title, authors, journal information, reviewer ID, date of data extraction.
-
Eligibility re‐assessment: all items in the inclusion criteria, final decision.
-
Study design: methods of randomization, allocation concealment and blinding, centres, country, time frame, ethics.
-
Participant information: inclusion and exclusion criteria, demographics (age, sex, etc), types of malocclusion, number of participants in each group, baseline status.
-
Intervention and comparison: details of the intervention and control groups, details of the active treatments applied to both groups, follow‐up period, number of participants lost to follow‐up and reasons.
-
Outcome: outcome variables and assessment methods, observation time, detailed results (including a 2 x 2 table for dichotomous data, and means and standard deviations (SD) or medians and quarters for continuous data (P, t, Chi2, etc.)).
-
Correspondence: contact addresses of original authors, questions to be asked.
Assessment of risk of bias in included studies
Two review authors carried out the assessment of risk of bias in the included studies, independently and in duplicate, using The Cochrane Collaboration's two‐part tool for assessing risk of bias. In the case of any discrepancies, a third review author also assessed the study. We completed a 'Risk of bias' table under the Characteristics of included studies for each study, as outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011).
Assessment of the risk of bias in included studies was carried out for the following seven domains:
-
sequence generation (selection bias);
-
allocation concealment (selection bias);
-
blinding of participants and personnel (performance bias);
-
blinding of outcome assessors (detection bias);
-
incomplete outcome data (attrition bias);
-
selective reporting (reporting bias);
-
other bias.
We documented a description of what was reported to have happened in the study for each domain within each 'Risk of bias' table, together with our assessment of the risk of bias for that domain: either 'low risk', 'unclear risk' or 'high risk'. We contacted the study authors to seek clarification in the event of uncertain data.
For objective outcomes, such as the primary outcome of this review (bond failure rate), we considered that blinding was unlikely to have any effect, and thus assigned a judgement of 'low risk' of performance bias to all studies that reported this outcome. We grouped objective outcomes together, as suggested in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011).
We summarized risk of bias in the included studies using the following criteria.
| Risk of bias | Interpretation | In outcome | In included studies |
| Low risk of bias | Plausible bias unlikely to seriously alter the results | Low risk of bias for all key domains | Most information is from studies at low risk of bias |
| Unclear risk of bias | Plausible bias that raises some doubt about the results | Unclear risk of bias for one or more key domains | Most information is from studies at low or unclear risk of bias |
| High risk of bias | Plausible bias that seriously weakens confidence in the results | High risk of bias for one or more key domains | The proportion of information from studies at high risk of bias is sufficient to affect the interpretation of results |
The risk of bias is presented graphically in Figure 1.
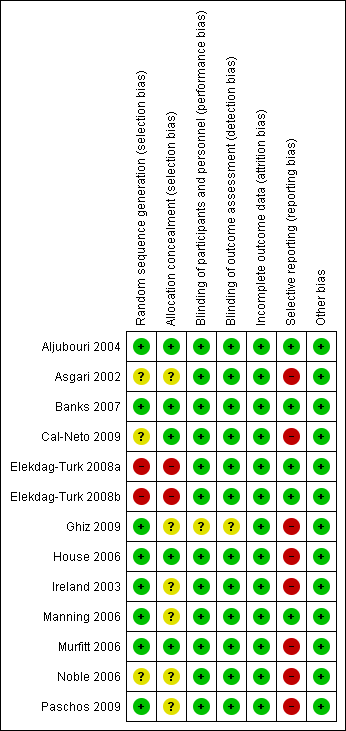
Risk of bias summary: review authors' judgments about each risk of bias item for each included study.
Measures of treatment effect
The measures of treatment effect differed according to data type. We treated bond failure rate as dichotomous data (as only failure or no failure was reported). We would have treated the secondary outcomes as dichotomous data or continuous data depending on the individual study.
Dichotomous data
We calculated risk ratios (RR) and 95% confidence intervals (CIs) for dichotomous data.
Continuous data
We would have calculated mean differences (MD) and 95% CIs for continuous outcomes that were assessed using the same scale, and standardized mean differences (SMD) and 95% CIs if different scales were used.
Unit of analysis issues
We based the unit of analysis on the participant, not on the tooth or quadrant; however, we also considered the analysis of studies with non‐standard designs.
Parallel studies
Because some of the original reports of parallel studies could include inappropriate analyses, as described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011), in order to avoid such statistical errors, we intended to calculate approximate analyses according to guidelines from the handbook.
Split‐mouth studies
We assessed the carry‐over effect for all split‐mouth studies. We intended to approximate a paired analysis, following the guidance of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). In the case of an ideal study (i.e. one that reported means and SD for both groups, and the MD and SD/standard error (SE) between the two groups), we intended to calculate intra‐group correlation coefficients (ICC); if we identified more than one ideal study, we intended to calculate the mean ICC, which we would have adopted in the calculation of the MD and SD/SE for other, similar split‐mouth studies. If no ideal study was identified, then we assumed that the ICC was 0.5.
Studies with multiple intervention arms
For RCTs with multiple treatment arms, we intended to combine similar arms. If this was not possible, we would select the most relevant treatment and control groups for analyses.
Dealing with missing data
Where data were missing, we adopted the following strategies.
-
Contact of study authors to request missing data whenever possible.
-
If SD was not provided but SE, 95% CI, t or P values were available, we intended to use these data to calculate exact SD (under such circumstances, there was no need to request such data from the study author).
-
If both mean and SD were reported in graphical rather than numerical format, we planned to amplify the relevant graphic and calculate or measure the mean and SD.
Assessment of heterogeneity
We assessed heterogeneity using the Chi2 test, where a P value less than 0.1 indicates statistically significant heterogeneity. We quantified heterogeneity using the I2 statistic, using the following rough guide to interpretation given in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011):
-
0% to 40%: heterogeneity may not be important;
-
30% to 60%: may represent moderate heterogeneity;
-
50% to 90%: may represent substantial heterogeneity;
-
75% to 100%: may represent considerable heterogeneity.
If heterogeneity greater than 50% was present, we planned to attempt to explain the heterogeneity based on the clinical characteristics of the included studies and to perform subgroup analyses to explore the lack of homogeneity.
Assessment of reporting biases
If we included more than 10 studies in a meta‐analysis, we planned to use a funnel graph to assess publication bias, using Egger's or Begg's method (Begg 1994; Egger 1997). Asymmetry of the funnel plot and a P value less than 0.10 would have been taken as indicating the possibility of reporting bias.
Data synthesis
We carried out meta‐analyses only of studies reporting the same comparisons and outcomes. We combined RR for dichotomous outcomes (and would have combined MD if we had found any usable continuous data) using a random‐effects model. We intended to use a fixed‐effect model if we identified fewer than four studies suitable for meta‐analysis.
Subgroup analysis and investigation of heterogeneity
To identify reasons for clinical or methodological heterogeneity in any meta‐analysis and to explore the effect of modification of participants and treatment types, we carried out subgroup analyses, where sufficient numbers of studies were available, according to:
-
study design: parallel design or split‐mouth design;
-
interventions: different brace systems (e.g. self ligating or edgewise brackets systems), different observation periods (e.g. short term or long term) or different etching times.
Sensitivity analysis
Where feasible, and if sufficient numbers of studies were found, we intended to carry out sensitivity analyses to assess all included studies by:
-
excluding any unpublished studies;
-
excluding studies with a high risk of bias;
-
comparing different models of intention‐to‐treat analysis (worst‐case scenario analysis versus best‐case scenario analysis);
-
using different assumptions of ICC (0.3 versus 0.7).
Summary of findings table
We developed a summary of findings table using GRADEPro software in order to assess the quality of the body of evidence (GRADE 2004). This was assessed with reference to the overall risk of bias of the included studies, the directness of the evidence, the inconsistency of the results, the precision of the estimates and the risk of publication bias. The quality of the body of evidence for each assessable outcome was categorized as high, moderate, low or very low.
Results
Description of studies
Results of the search
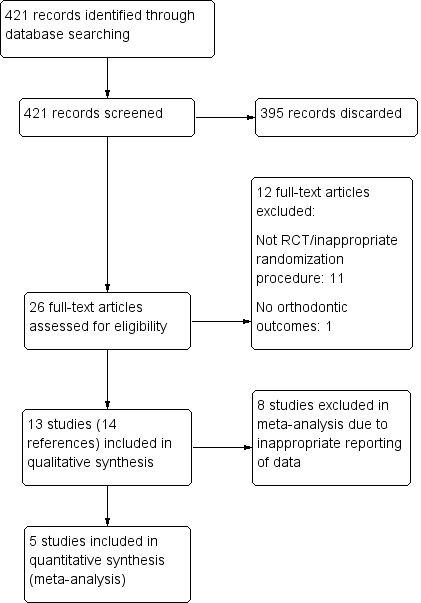
We identified 421 publications during the searching process, of which 395 were discarded after reviewing the titles and abstracts. We obtained full articles for the remaining 26 publications, and excluded a further 12 after screening. As two of the remaining 14 publications that met the inclusion criteria for this review were reports of the same RCT, we linked these together under a single primary reference (Manning 2006). We therefore included 13 RCTs in this review (Aljubouri 2004; Asgari 2002; Banks 2007; Cal‐Neto 2009; Elekdag‐Turk 2008a; Elekdag‐Turk 2008b; Ghiz 2009; House 2006; Ireland 2003; Manning 2006; Murfitt 2006; Noble 2006; Paschos 2009). For details of the studies examined and reasons for inclusion or exclusion, see the Characteristics of included studies and Characteristics of excluded studies tables. We outline the process of study identification in Figure 2.

Flow diagram of study inclusion.
Included studies
See Characteristics of included studies table.
Design
Ten of the included studies were of split‐mouth design, and the remaining three were of parallel design. In nine of the split‐mouth studies (Aljubouri 2004; Asgari 2002; Elekdag‐Turk 2008a; Elekdag‐Turk 2008b; House 2006; Ireland 2003; Murfitt 2006; Noble 2006; Paschos 2009) participants were randomly allocated to have the upper right and lower left quadrants bonded with the same etching technique, using either a self etching primer (SEP) or a conventional etching system; the remaining quadrants were bonded using the alternative technique. In the remaining split‐mouth study (Ghiz 2009), participants were randomly assigned to have a conventional etching system used on one arch and an SEP on the other arch. In the three parallel studies (Banks 2007; Cal‐Neto 2009; Manning 2006), participants were randomized to receive conventional etching or SEP.
Sample sizes
The sample size ranged from 20 to 60 participants with 339 to 871 brackets. Seven of the 13 studies undertook a priori sample size calculation on the basis of previous research in order to detect a significant difference between the two intervention groups (Aljubouri 2004; Banks 2007; Cal‐Neto 2009; House 2006; Manning 2006; Murfitt 2006; Paschos 2009), whereas sample size calculation was not mentioned in the remaining six studies. We contacted the authors of four of these studies and were informed that the authors of three studies carried out a power analysis from previous studies as a guideline for sample size determination (Elekdag‐Turk 2008a; Elekdag‐Turk 2008b; Ghiz 2009). However, we received no reply from the authors of the remaining study (Ireland 2003).
Setting
Of the 13 studies, five were conducted in UK (Aljubouri 2004; Banks 2007; House 2006; Ireland 2003; Manning 2006), three in the USA (Asgari 2002; Ghiz 2009; Noble 2006), two in Turkey (Elekdag‐Turk 2008a; Elekdag‐Turk 2008b), one in Brazil (Cal‐Neto 2009), one in New Zealand (Murfitt 2006) and one in Germany (Paschos 2009).
Participants
In total, this systematic review included 417 participants with 7184 teeth/brackets. The age distribution ranged from 11 to 36 years, and most of the participants were teenagers. Most studies reported inclusion/exclusion criteria for the selection of participants. Five studies did not report participants' sex (Asgari 2002; Ghiz 2009; House 2006; Ireland 2003; Noble 2006), whereas four studies did not report age (Asgari 2002; Ghiz 2009; House 2006; Ireland 2003).
Interventions
Eleven studies compared the effectiveness of SEPs with conventional etchants for the bonding of fixed orthodontic appliances (Aljubouri 2004; Asgari 2002; Banks 2007; Cal‐Neto 2009; Elekdag‐Turk 2008a; Elekdag‐Turk 2008b; Ghiz 2009; House 2006; Ireland 2003; Manning 2006; Murfitt 2006). Ten of these studies compared Transbond Plus SEP (3M Unitek) and 37% phosphoric acid. One study compared Ideal 1 SEP (GAC Orthodontic Products) and 37% phosphoric acid (House 2006). Finally, two studies compared two SEPs: Transbond Plus (3M Unitek) versus Clearfil Protect Bond (Kuraray Medical) (Paschos 2009) and Transbond Plus (3M Unitek) versus First Step SEP (Reliance Orthodontic Products) (Noble 2006).
We identified no eligible trial that examined the effects of conventional etchants with respect to different etching concentrations or etching times for the bonding of fixed orthodontic appliances.
Outcomes
Some of the outcomes of interest in this systematic review were evaluated in the included studies.
-
Bond failure rate: overall bond failure rate (Aljubouri 2004; Asgari 2002; Banks 2007; Cal‐Neto 2009; Elekdag‐Turk 2008a; Elekdag‐Turk 2008b; House 2006; Ireland 2003; Manning 2006; Murfitt 2006; Noble 2006; Paschos 2009); bond failure rate per participant (Aljubouri 2004; Banks 2007; Elekdag‐Turk 2008a; Elekdag‐Turk 2008b; Manning 2006) (for Elekdag‐Turk 2008a and Elekdag‐Turk 2008b, unpublished participant‐level data was provided on request by the study authors); and bond failure rate distributions with respect to dental arch, type of tooth and participant sex (Banks 2007; Cal‐Neto 2009; Elekdag‐Turk 2008a; Elekdag‐Turk 2008b; Manning 2006; Murfitt 2006; Noble 2006).
-
The presence or absence of decay (decalcification) associated with or around the etching field (Ghiz 2009; Paschos 2009).
No participant‐centered outcomes, such as satisfaction or the cost or duration of treatment, were reported in any of the included studies.
Excluded studies
See Characteristics of excluded studies table for further details.
We excluded 12 studies from this review. Eleven of these studies were either not RCTs or there were problems with the randomization procedure (i.e. teeth were alternately/sequentially randomized). One study did not report any orthodontic outcomes.
Risk of bias in included studies
See the 'Risk of bias' tables within Characteristics of included studies for further details. For a graphical summary, see Figure 1.
We assessed two studies as being at low risk of bias (Aljubouri 2004; Banks 2007) and 10 studies as being at high risk of bias (Asgari 2002; Cal‐Neto 2009; Elekdag‐Turk 2008a; Elekdag‐Turk 2008b; Ghiz 2009; House 2006; Ireland 2003; Murfitt 2006; Noble 2006; Paschos 2009). We assessed the remaining study as being at unclear risk of bias (Manning 2006).
Allocation
Sequence generation
Although all of the 13 included studies mentioned random allocation, after examination of the publications and further contact with several study authors, we considered only eight studies to be at low risk of bias for this domain (Aljubouri 2004; Banks 2007; Ghiz 2009; House 2006; Ireland 2003; Manning 2006; Murfitt 2006; Paschos 2009). Four of these studies used random number tables for random sequence generation (Banks 2007; House 2006; Ireland 2003; Manning 2006), one used coin tossing (Ghiz 2009), one used random permuted blocks (Murfitt 2006), one used drawing lots (Paschos 2009) and the remaining study stated that the randomization process was carried out by a trial statistician, which is likely to have been done adequately (Aljubouri 2004). Two studies by the same authors used coin tossing for the first participant, and then alternation afterwards. As alternation is not true randomization (Higgins 2011), we considered these two studies to be at high risk of bias for this domain (Elekdag‐Turk 2008a; Elekdag‐Turk 2008b). The remaining three trials did not describe the method of sequence generation and we assessed these as being at unclear risk of bias (Asgari 2002; Cal‐Neto 2009; Noble 2006).
Allocation concealment
Five studies used sealed envelopes to conceal the allocation sequence from all those involved in the studies, and we therefore assessed these as being at low risk of bias for this domain (Aljubouri 2004; Banks 2007; Cal‐Neto 2009; House 2006; Murfitt 2006). Two studies that used coin tossing to allocate the first participant, and then alternation afterwards, could not have concealed the allocation sequence and we therefore considered these studies to be at high risk of bias for this domain (Elekdag‐Turk 2008a; Elekdag‐Turk 2008b). There was not enough information in the remaining six studies to determine whether or not the sequence was adequately concealed, so we judged these studies to be at unclear risk of bias for this domain (Asgari 2002; Ghiz 2009; Ireland 2003; Manning 2006; Noble 2006; Paschos 2009).
Blinding
Participants and personnel (performance bias)
The primary outcome of this review (bond failure rate) is highly objective and we considered that blinding was unlikely to have any effect on the outcome; hence, we assigned a judgement of 'low risk' of bias for this domain throughout. One study did not include our primary outcome, and measured only enamel decalcification and oral hygiene compliance (Ghiz 2009). As the outcomes in this study were considered more subjective, and blinding was unclear in the report, we considered this study to be at unclear risk of bias for this domain. We considered the remaining 12 studies to be at low risk of bias for this domain.
Outcome assessment (detection bias)
For the same reasons stated above, we assessed one study as being at unclear risk of bias (Ghiz 2009) and the remaining 12 studies to be at low risk of bias for this domain.
Incomplete outcome data
In eight studies there were no drop‐outs (Aljubouri 2004; Asgari 2002; Elekdag‐Turk 2008b; Ghiz 2009; House 2006; Ireland 2003; Noble 2006; Paschos 2009). In the remaining five studies, the number of drop‐outs were minimal and clearly described (Banks 2007; Cal‐Neto 2009; Elekdag‐Turk 2008a; Manning 2006; Murfitt 2006). Thus, we assessed all 13 studies as being at low risk of bias for this domain.
Selective reporting
In all 13 studies, the outcomes stated in the methods section of each study were reported in the results section. However, in eight studies we considered the reporting inappropriate as data were reported at tooth level rather than at participant level (Asgari 2002; Cal‐Neto 2009; Ghiz 2009; House 2006; Ireland 2003; Murfitt 2006; Noble 2006; Paschos 2009). Furthermore, teeth were treated independently in analyses, ignoring the clustering of teeth within the mouth. We were therefore unable to use the data from these studies in a meta‐analysis. For these reasons, we assessed all eight studies as being at high risk of bias for this domain. We assessed the remaining five studies as being at low risk of bias for this domain: three reported data at the participant level (Aljubouri 2004; Banks 2007; Manning 2006), and two provided such data on request (Elekdag‐Turk 2008a; Elekdag‐Turk 2008b).
We believe it is important to point out that none of the included studies mentioned a previously published protocol.
Other potential sources of bias
We were not able to identify any other sources of bias in any of the 13 studies, and they were all considered to be at low risk of bias for this domain.
Effects of interventions
Self etching primers versus conventional etchants
Although 11 RCTs compared the effect of SEPs and conventional etchants, a majority of the results could not be used for further analysis because the outcomes were reported at tooth level rather than at participant level. We considered only five studies, which reported the effects of different etching techniques at participant level, suitable for meta‐analysis (e.g. mean bond failure rate per participant).
1. Mean bond failure rate per participant
Five of the included studies, with 221 participants, reported the results of the bond failure rate at participant level and were pooled in a meta‐analysis (Aljubouri 2004; Banks 2007; Elekdag‐Turk 2008a; Elekdag‐Turk 2008b; Manning 2006). Two of these studies were parallel‐designed RCTs with low heterogeneity (Banks 2007; Manning 2006), and three were split‐mouth designed RCTs with moderate heterogeneity (Aljubouri 2004; Elekdag‐Turk 2008a; Elekdag‐Turk 2008b). We present the raw data for this outcome in Additional Table 1. We assessed two studies as being at low risk of bias (Aljubouri 2004; Banks 2007), two studies as being at high risk of bias (Elekdag‐Turk 2008a; Elekdag‐Turk 2008b) and the remaining study as at unclear risk of bias (Manning 2006). The duration of follow‐up in three of the studies was 12 months (Aljubouri 2004; Elekdag‐Turk 2008a; Manning 2006), whereas one study had six months of follow‐up (Elekdag‐Turk 2008b) and in the remaining study follow‐up ranged from 5 to 37 months (Banks 2007).
| SEP no failure | SEP ≥ 1 failure | Conventional no failure | Conventional ≥ 1 failure | Total | |
| 46 | 5 | 41 | 10 | 102 | |
| 27 | 12 | 34 | 5 | 78 | |
| 35 | 2 | 35 | 2 | 74 | |
| 17 | 13 | 19 | 11 | 60 | |
| 7 | 10 | 8 | 9 | 34 | |
| Total | 132 | 42 | 137 | 37 | 348 |
The actual total number of participants is 221, rather than 348, as the top three split‐mouth studies included the participants in both intervention groups.
SEP = self etching primer.
We considered the evidence insufficient to determine whether or not there is a difference in the bond failure rate between the SEP group and the conventional etching group (risk ratio (RR) 1.14; 95% confidence interval (CI) 0.75 to 1.73) (Analysis 1.1). The uncertainty in the CI includes both no effect and appreciable benefit and harm. Heterogeneity was low (I2 = 18%) and we considered this as probably not important. We conducted a subgroup analysis of the two types of study design to see whether it was appropriate to combine them in the meta‐analysis. There is no evidence that the proportion of bond failures is different for SEP or conventional etchants, either in the subgroup of split‐mouth studies (RR 1.09; 95% CI 0.37 to 3.26) or in the subgroup of parallel studies (RR 1.14; 95% CI 0.74 to 1.76). The test for subgroup differences was not significant (P value = 0.94), indicating that it was appropriate to combine both types of study in the meta‐analysis.
Five other studies compared SEPs and conventional etchants but did not report the mean bond failure rate per participant (Asgari 2002; Cal‐Neto 2009; House 2006; Ireland 2003; Murfitt 2006). These studies reported bond failure rate at the tooth level, and the results were mixed (see Table 2).
| Comparison | Results for bond failure rate (analyzed at tooth level) at 6 to 12 months | |
| Transbond Plus SEP versus conventional | "The 'p' value of .037 indicated that the bond failure rate using Transbond Plus Self Etching Primer was significantly less than the bond failure rate in those quadrants where a 37% phosphoric acid etchant was used" | |
| Transbond Plus SEP versus conventional | "There was no significant difference in terms of bracket failure risk over the 12 months between groups... P = 0.311)" | |
| Ideal 1 SEP versus conventional | Odds ratio at 12 months = 15.1 (95% confidence interval 7.7 to 29.3) for failure of SEP relative to conventional. Recruitment was stopped early due to high failure rate of SEP group | |
| Transbond Plus SEP versus conventional | "The difference between the failure proportions was ‐0.06 with an associated 95% confidence interval of ‐0.121 to 0.001. This study produced weak evidence to suggest that bond failures with a self‐etching primer will be higher than those with conventional etching and priming" | |
| Transbond Plus SEP versus conventional | "Transbond Plus SEP was found to have a significantly higher failure rate than the conventional 37 per cent phosphoric acid and primer (P = 0.001)" |
SEP = self etching primer.
2. Presence or absence of decay (decalcification) associated with or around the etching field
Only one study reported this outcome (Ghiz 2009). This was a split‐mouth designed RCT involving 25 participants with 469 brackets, comparing enamel decalcification between an SEP group and a conventional etching group. However, the decalcification score was reported at tooth level rather than at participant level. We considered the evidence insufficient to conclude whether or not there is a difference in decalcification between SEPs and conventional etching.
Self etching primers versus self etching primers
Two split‐mouth studies compared two different SEPs (Noble 2006; Paschos 2009). However, the failure rates (and decalcification outcomes in Paschos 2009) were reported at tooth level rather than at participant level. We considered the evidence insufficient to conclude whether or not there is a difference in bond failures or decalcification between the different SEPs.
Discussion
Summary of main results
The objective of this review was to evaluate the effects of different etchants and etching techniques for the bonding of fixed orthodontic braces to tooth enamel. We included 13 RCTs that satisfied the inclusion criteria in this review.
Eleven studies compared the effectiveness of self etching primers (SEPs) with conventional etchants for bonding fixed orthodontic appliances. We considered only five of these studies, which reported data on bond failure rate at the participant level, suitable for inclusion in a meta‐analysis (Aljubouri 2004; Banks 2007; Elekdag‐Turk 2008a; Elekdag‐Turk 2008b; Manning 2006). We assessed the body of evidence for this comparison and outcome, using GRADE (GRADE 2004) which incorporates risk of bias of the included studies, the directness of the evidence, the inconsistency of the results, the precision of the estimates and the risk of publication bias (see summary of findings Table for the main comparison). We assessed this body of evidence, from five studies analyzing 221 participants and with follow‐up ranging from 5 to 37 months, as being low quality and insufficient to conclude whether or not there is a difference in the bond failure rate of SEPs and conventional etchants. There was a lot of uncertainty in the results, with the 95% confidence interval including both the possibility that SEPs have fewer failures, and that conventional etchants have fewer failures. Five other studies that compared SEPs with conventional etchants, but analyzing bond failure at the tooth level, also reported mixed results (Additional Table 2).
Two studies compared two different SEPs (Noble 2006; Paschos 2009). Neither study reported data at the participant level and we therefore consider that there is no evidence for the superior effects of any one of the SEPs investigated over the others.
Overall completeness and applicability of evidence
We used a thorough and systematic searching process, outlined in the 'Methods' section of this systematic review, in order to ensure completeness and maximize external validity. However, this systematic review has not been able to meet its objective as the results regarding bond failures were inconclusive. In addition, no eligible RCTs were found that compared the effects of different etching materials (e.g. phosphoric acid, polyacrylic acid, maleic acid), concentrations or etching times for the bonding of fixed orthodontic appliances. Furthermore, we identified only two eligible RCTs that compared different SEPs. Neither study compared the same two SEPs and neither study reported data at the participant level, which meant we were unable to perform a meta‐analysis on this comparison, and therefore were unable to form any conclusions on which is the most effective SEP.
We identified a number of additional eligible studies that we did not include in the meta‐analysis, as they presented data by tooth rather than by participant. These studies had frequently analyzed results using the Chi2 test, thus failing to take the pairing of the data within participants' mouths into account. We also excluded the data from these studies as teeth were treated independently in the analysis, ignoring the clustering of teeth within the mouth. As the participant is the unit of assessment for both bonding systems, it would have been more correct to report the mean bond failure rate (or mean decalcification score) per participant rather than the overall outcomes at tooth level, which can obscure the true nature of the data. This has been strongly recommended in a previous systematic review (Mandall 2003).
Only two of the included studies dealt with the effect of different etching techniques on the prevention of enamel decalcification (Ghiz 2009; Paschos 2009). However, they both reported data at tooth level. Any difference in the presence or absence of decay (decalcification) associated with or around the etching field is an important outcome, as fixed orthodontic appliances make it difficult for recipients to maintain adequate oral hygiene during treatment. Several studies have found increased plaque around orthodontic appliances (O'Reilly 1987; Ogaard 1988).
No studies reported the outcomes of participant satisfaction or treatment cost‐effectiveness, which are important outcomes that should be considered in future studies. The cost of the etching material, together with the bonding time and overall number of appointments required, as well as any additional appointments (e.g. for bracket rebonding because of failure) may play a key role in the selection of etching material and etching technique.
The current limited volume of evidence on the primary outcome of this review (bond failure rate) is not conclusive in demonstrating improved clinical outcomes for one method of etching over another. This may encourage the routine clinical use of SEPs as a good alternative to conventional etching as use of SEPs is associated with fewer clinical steps, less chair‐side time and a lower risk of salivary contamination. Further, high‐quality RCTs measuring all relevant outcomes and reporting results at a participant level are required before definitive conclusions and recommendations can be made with regard to enamel etching for the bonding of fixed orthodontic braces.
Quality of the evidence
We included 13 RCTs and 417 participants with 7184 teeth/brackets in this systematic review. Of the five studies comparing conventional etchants and SEPs that were suitable for pooling in a meta‐analysis for the outcome of bond failure rate, we considered two to be at low risk of bias overall, two to be at high risk and one to be at unclear risk. We downgraded the quality of the body of evidence due to serious concerns about the risk of selection bias in two of the studies, and also as a result of the imprecision of the results (there were a low number of events and the 95% confidence interval includes both no effect and an appreciable benefit and harm). The results therefore do not allow us to draw a robust conclusion regarding the objective of the review.
Many recent clinical trials comparing bonding systems have used the split‐mouth design where, typically, the mouth of each participant is divided into quadrants and the teeth in the maxillary left and mandibular right quadrants receive one pre‐treatment, and the teeth in maxillary right and mandibular left quadrants receive the alternative pre‐treatment. The advantage of this is that factors pertaining to the participant (e.g. poor care of appliances) will be accounted for evenly, since each participant is his/her own control. However, one bonding agent might affect the performance of the other, and the bracket bonding technique might be altered and may not truly reflect clinical practice. Alternatively, the possibility of some cross‐over benefit, either local or systemic, has been suggested. For example, if the arch wire combines the whole maxillary/mandibular dentition as an integrate, the carry‐across effect could reduce the difference in outcomes between strong and weak interventions (Lesaffre 2009; Needleman 2006).
Other studies have used a parallel design by randomly allocating one etching technique to each participant to eliminate this problem.
Furthermore, while the included studies achieved the required sample size, the original sample size calculations did not take into account clustering of brackets within the participants, modeling using other covariates or multiple testing issues. The use of clusters in these included studies reduces the power of the trial, and multiple testing increases the chance of false‐positive results, so an increase in sample size is required (Kerry 1998). Future RCTs in orthodontics should take these issues into account and increase the sample size required accordingly (Manning 2006).
Although there was low heterogeneity in the studies that we meta‐analyzed, further studies should consider the standardizing of study design in order to make results more comparable. This would involve factors such as the appliance system (e.g. self ligating or edgewise brackets systems), observation period (e.g. short or long term) and etching time (e.g. 15 or 30 seconds using 37% phosphoric acid), which may have been important confounders among the studies included.
With respect to the observation period, describing the bond failure rate over the whole period of a course of treatment in randomly allocated individuals is recommended. Previous studies have shown that most bond failures occur within the first three or six months after bracket placement (Aljubouri 2004; Hegarty 2002; O'Brien 1989). There may be three possible reasons for this increased failure rate during the first six months of treatment. First, any deficiencies in the bond strength of any individual bracket/adhesive combination would become evident within this initial period of treatment. Second, the initial period of treatment is also a time of acclimatization and experimentation for recipients with regard to the type of food that can be tolerated by fixed orthodontic appliances. Finally, the initial phase of treatment may involve a period of overbite depression from heavy occlusal forces. Another study found that the failure rate for SEPs increased from 1.7% at six months to 7.0% at the completion of treatment, whereas that for a conventional system increased from 2.0% to 7.4%; thus failure rates increased for both materials over the treatment period (Manning 2006). The authors of this study stated that describing bond failure rate over the whole period of a course of treatment in randomly allocated individuals could eliminate any variation due to treatment length. If participants are followed up over a set time period (e.g. one year), this may fail to reveal whether the performance of one material deteriorates over time. In addition, a systematic review of orthodontic bonding studies performed by the Cochrane Oral Health Group recommended that bonding studies follow all trial participants to the end of fixed appliance treatment (Mandall 2003). We also suggest that future studies follow this recommendation.
A potential confounder may be etching time. All the included studies used 37% phosphoric acid as the conventional etching system, but applied it for different times. The teeth were etched for 15 seconds in several studies (Aljubouri 2004; Asgari 2002; Banks 2007; Cal‐Neto 2009; Ireland 2003; House 2006; Murfitt 2006) and for 30 seconds in others (Elekdag‐Turk 2008a; Elekdag‐Turk 2008b; Ghiz 2009; Manning 2006). Other previous studies have investigated the influence of different etching times on bracket bond failure rate, and the results indicated no significant difference in bond failure rate between groups using 37% phosphoric acid etching for 15 seconds versus either 30 seconds or 60 seconds (Carstensen 1986; Kinch 1988; Sadowsky 1990; Ye 2003). Furthermore, the manufacturer's instructions are sometimes not followed, making comparison with other reports inappropriate and difficult (dos Santos 2006). SEP (Transbond Plus) was applied for three to five seconds, according to the manufacturer's instructions, in several studies (Aljubouri 2004; Asgari 2002; Banks 2007; Cal‐Neto 2009; Elekdag‐Turk 2008a; Elekdag‐Turk 2008b; Ghiz 2009; Ireland 2003; Manning 2006; Murfitt 2006). However, other studies have recommended application of the SEP for 10 to 15 seconds because the prolonged application time was reported to improve the bonding deficiency of self etch systems to enamel (Ferrari 1997; dos Santos 2006).
Potential biases in the review process
We have taken steps to limit bias during the process of undertaking this systematic review. We have made every effort to identify all relevant studies by searching seven databases, with no exlusions of any study due to language of publication. Nevertheless, it is possible that the databases searched do not cover all the published, unpublished and ongoing studies available, and this may have led to bias. Furthermore, we attempted to contact some of the study authors for missing information and clarification. Since the publication of the protocol, we have added an exclusion criterion (studies comparing different etchants or etching techniques but not reporting any orthodontic outcomes) and also decided that the objective outcomes in this review would not be affected by blinding. We acknowledge that such post‐hoc changes could introduce bias but feel that they improve the quality, consistency and relevance of the review.
Agreements and disagreements with other studies or reviews
A recent systematic review compared SEPs with conventional etching and a meta‐analysis of five studies indicated a higher bond failure rate for SEPs over 12 months (odds ratio 1.35; 95% confidence interval 0.99 to 1.83) (Fleming 2012). The 95% confidence interval in the Fleming review was indicative of a more precise result than that obtained in our review, as the lower confidence limit implied only a slight chance that conventional etching was worse than etching using an SEP. Three of the studies in the meta‐analysis were included in our meta‐analysis (Aljubouri 2004; Banks 2007; Manning 2006). However, the Fleming review analyzed data at the tooth level. In agreement with the findings of our review, the Fleming review concluded that there was insufficient evidence to state whether there was a difference in demineralization between bonding techniques. The authors also concluded, however, that SEPs were associated with a slight but statistically significant time saving compared with conventional etching.

Risk of bias summary: review authors' judgments about each risk of bias item for each included study.
Flow diagram of study inclusion.

Comparison 1 Self etching primers versus conventional etchants, Outcome 1 Bond failure rate (5 to 37 months).
| Participants or population: Children and adults with fixed orthodontic brackets Settings: Clinical (typically university dental clinics) Intervention: Self etching primers (one‐step etchant and primer system) Comparison: Conventional etchants (two‐step etch and prime method using 37% phosphoric acid) | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Conventional etchants | Self etching primers | |||||
| Bond failure rate (5 to 37 months) | 196 per 1000 | 223 per 1000 | RR 1.14 (0.75 to 1.73) | 221 | ⊕⊕⊝⊝1, 2 | Five more studies, which we were unable to include in the meta‐analysis, reported mixed results (Additional Table 2) |
| Decay (decalcification) associated with or around the etching field | Only one study (Ghiz 2009) assessed this outcome but data were reported at the tooth level rather than at the participant level and therefore was not amenable to analysis using Cochrane methods | |||||
| Participant satisfaction | No studies assessed this outcome | |||||
| Cost of treatment | No studies assessed this outcome | |||||
| Damage to the teeth | No studies assessed this outcome | |||||
| *The assumed risk is the median control group risk across studies. The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Two studies at low risk of bias, one at unclear risk, but two with serious risk of selection bias. | ||||||
| SEP no failure | SEP ≥ 1 failure | Conventional no failure | Conventional ≥ 1 failure | Total | |
| 46 | 5 | 41 | 10 | 102 | |
| 27 | 12 | 34 | 5 | 78 | |
| 35 | 2 | 35 | 2 | 74 | |
| 17 | 13 | 19 | 11 | 60 | |
| 7 | 10 | 8 | 9 | 34 | |
| Total | 132 | 42 | 137 | 37 | 348 |
| The actual total number of participants is 221, rather than 348, as the top three split‐mouth studies included the participants in both intervention groups. SEP = self etching primer. | |||||
| Comparison | Results for bond failure rate (analyzed at tooth level) at 6 to 12 months | |
| Transbond Plus SEP versus conventional | "The 'p' value of .037 indicated that the bond failure rate using Transbond Plus Self Etching Primer was significantly less than the bond failure rate in those quadrants where a 37% phosphoric acid etchant was used" | |
| Transbond Plus SEP versus conventional | "There was no significant difference in terms of bracket failure risk over the 12 months between groups... P = 0.311)" | |
| Ideal 1 SEP versus conventional | Odds ratio at 12 months = 15.1 (95% confidence interval 7.7 to 29.3) for failure of SEP relative to conventional. Recruitment was stopped early due to high failure rate of SEP group | |
| Transbond Plus SEP versus conventional | "The difference between the failure proportions was ‐0.06 with an associated 95% confidence interval of ‐0.121 to 0.001. This study produced weak evidence to suggest that bond failures with a self‐etching primer will be higher than those with conventional etching and priming" | |
| Transbond Plus SEP versus conventional | "Transbond Plus SEP was found to have a significantly higher failure rate than the conventional 37 per cent phosphoric acid and primer (P = 0.001)" | |
| SEP = self etching primer. | ||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Bond failure rate (5 to 37 months) Show forest plot | 5 | 348 | Risk Ratio (Random, 95% CI) | 1.14 [0.75, 1.73] |
| 1.1 Split‐mouth studies | 3 | 254 | Risk Ratio (Random, 95% CI) | 1.09 [0.36, 3.25] |
| 1.2 Parallel studies | 2 | 94 | Risk Ratio (Random, 95% CI) | 1.14 [0.74, 1.76] |

