Tapones anales para tratar la incontinencia fecal
Referencias
Referencias de los estudios incluidos en esta revisión
Referencias adicionales
Referencias de otras versiones publicadas de esta revisión
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Randomised controlled trial (2:1) | |
| Participants | Forty eight patients took part in the trial (28 children, age > 4 years; and 20 young adults, age 16 to 45 years) | |
| Interventions | 1. Polyurethane anal plug (Conveen, Coloplast) (two sizes) | |
| Outcomes | ‐ Functional Status II‐R ‐SF‐36 ‐ a Patient‐Generated Index of Quality of Life (PGI) ‐ a Carer‐Generated Index (CGI) of Quality of Life ‐ the Dartmouth COOP Charts ‐ a condition‐ specific measure developed for the research ‐ qualitative data: advantages and disadvantages of the plug ‐ health service utilisation data ‐ costs data ‐ evaluation of education package | |
| Notes | 31 (16 children and 15 adults) allocated plugs; 17 (12 children and 5 adults) allocated to no plugs. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
| Methods | Randomised cross‐over trial | |
| Participants | Adult outpatients (n = 34) attending a specialist colorectal hospital after failure of previous treatment | |
| Interventions | 1. Polyurethane anal plug (Conveen, Coloplast) 37 mm diameter when open | |
| Outcomes | ‐ comfort of inserting plug ‐ comfort of plug in use ‐ comfort of taking plug out ‐ capacity of controlling faecal leakage ‐ preference ‐ patient characteristics which predict when the plug will help the most | |
| Notes | Of the 34 patients offered the plug, 4 refused as they disliked the idea, 2 failed to attend, 8 dropped out after trying first plug, because of discomfort and 9 dropped out after trying one size of plug, refusing to try the second size. 11 patients completed the protocol. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Methods | Randomised cross‐over trial | |
| Participants | 38 partially continent or incontinent patients following imperforate anus repair (age > 6 to 15) | |
| Interventions | 1. Polyurethane anal plug (Conveen, Coloplast) (size closed/open diameter of 14.5/38mm or 15.5/45mm; depending on anal canal diameter) | |
| Outcomes | ‐ stool consistency | |
| Notes | 38 patients included. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Methods | Randomised cross‐over trial | |
| Participants | 7 patients (4 to 12 yrs; 3 girls and 4 boys) with high type of imperforate anus; and 9 patients with spina bifida (6 to 13 yrs, 2 girls and 7 boys) | |
| Interventions | 1. Polyurethane anal plug (Conveen, Coloplast) (size 12 or 13mm; depending on preference). | |
| Outcomes | ‐ number of stools | |
| Notes | 16 patients included. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size | |||||||||
| 1 General health improved ‐ adults Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | ||||||||||
| Analysis 1.1  Comparison 1 Anal plugs versus no plugs, Outcome 1 General health improved ‐ adults. | |||||||||||||
| 2 Bodily pain improved ‐ adults Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | ||||||||||
| Analysis 1.2  Comparison 1 Anal plugs versus no plugs, Outcome 2 Bodily pain improved ‐ adults. | |||||||||||||
| 3 Well being (adults) improved Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | ||||||||||
| Analysis 1.3 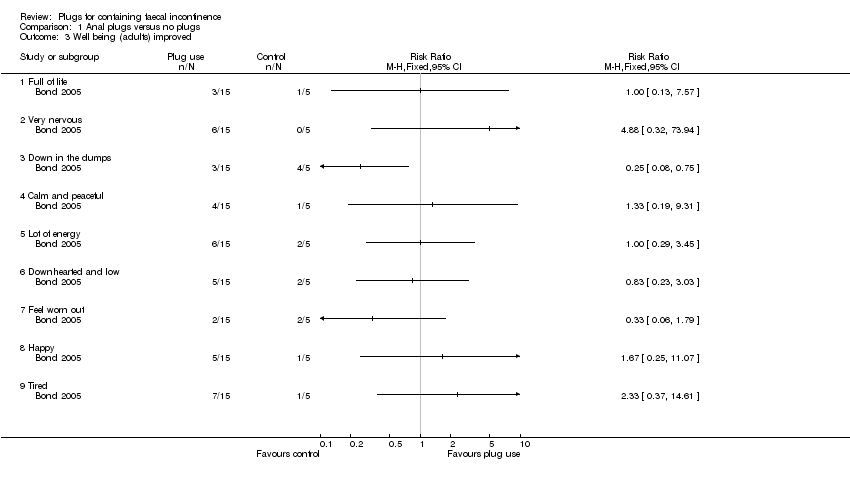 Comparison 1 Anal plugs versus no plugs, Outcome 3 Well being (adults) improved. | |||||||||||||
| 3.1 Full of life | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | ||||||||||
| 3.2 Very nervous | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | ||||||||||
| 3.3 Down in the dumps | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | ||||||||||
| 3.4 Calm and peaceful | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | ||||||||||
| 3.5 Lot of energy | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | ||||||||||
| 3.6 Downhearted and low | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | ||||||||||
| 3.7 Feel worn out | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | ||||||||||
| 3.8 Happy | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | ||||||||||
| 3.9 Tired | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | ||||||||||
| 4 Condition‐specific measures of faecal incontinence improved Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | ||||||||||
| Analysis 1.4  Comparison 1 Anal plugs versus no plugs, Outcome 4 Condition‐specific measures of faecal incontinence improved. | |||||||||||||
| 4.1 Protection | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | ||||||||||
| 4.2 Rash/skin problems | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | ||||||||||
| 4.3 Unpleasant odour | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | ||||||||||
| 4.4 Staining/smearing | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | ||||||||||
| 4.5 Bowel movement in undergarments (last two weeks) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | ||||||||||
| 4.6 Frequency of unpleasant odours | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | ||||||||||
| 4.7 Bowel movements in undergarments (on average day) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | ||||||||||
| 4.8 Soiled/stained undergarment (on average day) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | ||||||||||
| 4.9 Prevents staying away from home | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | ||||||||||
| 4.10 Must avoid long journeys | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | ||||||||||
| 4.11 Must always have a toilet nearby | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | ||||||||||
| 5 Stool frequency Show forest plot | Other data | No numeric data | |||||||||||
| Analysis 1.5
Comparison 1 Anal plugs versus no plugs, Outcome 5 Stool frequency. | |||||||||||||
| 6 Costs Show forest plot | Other data | No numeric data | |||||||||||
| Analysis 1.6
Comparison 1 Anal plugs versus no plugs, Outcome 6 Costs. | |||||||||||||
| 7 Achievement of pseudo‐continence Show forest plot | Other data | No numeric data | |||||||||||
| Analysis 1.7
Comparison 1 Anal plugs versus no plugs, Outcome 7 Achievement of pseudo‐continence. | |||||||||||||
| 8 Intolerance of intervention Show forest plot | Other data | No numeric data | |||||||||||
| Analysis 1.8
Comparison 1 Anal plugs versus no plugs, Outcome 8 Intolerance of intervention. | |||||||||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size | |||||||||
| 1 Plug effectiveness: number of people with no soiling Show forest plot | Other data | No numeric data | |||||||||||
| Analysis 2.1
Comparison 2 One type of anal plug versus another type, Outcome 1 Plug effectiveness: number of people with no soiling. | |||||||||||||
| 2 Feeling of security Show forest plot | Other data | No numeric data | |||||||||||
| Analysis 2.2
Comparison 2 One type of anal plug versus another type, Outcome 2 Feeling of security. | |||||||||||||
| 3 Loss of plug Show forest plot | Other data | No numeric data | |||||||||||
| Analysis 2.3
Comparison 2 One type of anal plug versus another type, Outcome 3 Loss of plug. | |||||||||||||
| 4 Inconvenience Show forest plot | Other data | No numeric data | |||||||||||
| Analysis 2.4
Comparison 2 One type of anal plug versus another type, Outcome 4 Inconvenience. | |||||||||||||
| 5 Overall satisfaction Show forest plot | Other data | No numeric data | |||||||||||
| Analysis 2.5
Comparison 2 One type of anal plug versus another type, Outcome 5 Overall satisfaction. | |||||||||||||

PRISMA study flow diagram.

Comparison 1 Anal plugs versus no plugs, Outcome 1 General health improved ‐ adults.

Comparison 1 Anal plugs versus no plugs, Outcome 2 Bodily pain improved ‐ adults.

Comparison 1 Anal plugs versus no plugs, Outcome 3 Well being (adults) improved.
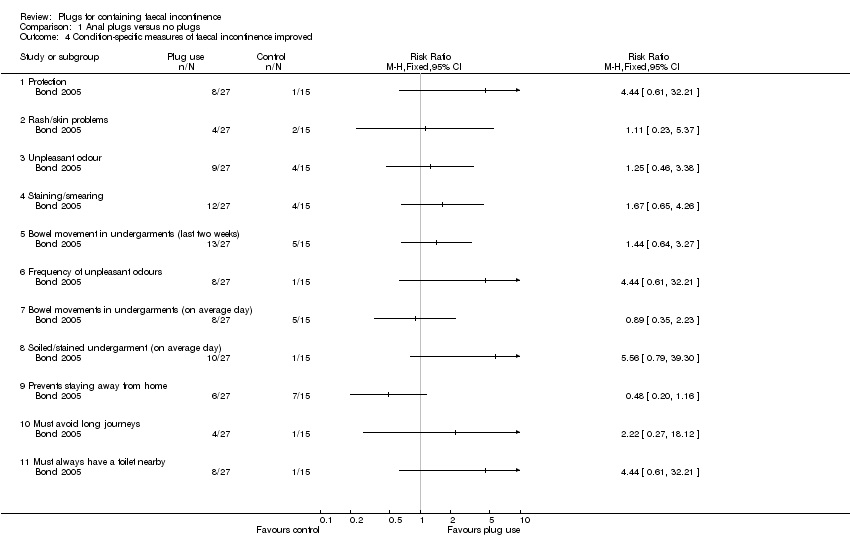
Comparison 1 Anal plugs versus no plugs, Outcome 4 Condition‐specific measures of faecal incontinence improved.
| Study | |
| Bond 2005 | No differences were observed between control and intervention group |
Comparison 1 Anal plugs versus no plugs, Outcome 5 Stool frequency.
| Study | |
| Bond 2005 | Little or no evidence that the plug led to significant reductions in the overall costs of care |
Comparison 1 Anal plugs versus no plugs, Outcome 6 Costs.
| Study | Anal plug period | Control period |
| Van Winckel 2005 | 6/12 | 0/12 |
Comparison 1 Anal plugs versus no plugs, Outcome 7 Achievement of pseudo‐continence.
| Study | Anal plug period | Control period |
| Van Winckel 2005 | 4/16 | 0/16 |
Comparison 1 Anal plugs versus no plugs, Outcome 8 Intolerance of intervention.
| Study | PU plug | PVA plug |
| Pfrommer 2000 | 15/23 | 14/23 |
Comparison 2 One type of anal plug versus another type, Outcome 1 Plug effectiveness: number of people with no soiling.
| Study | PU plug | PVA plug |
| Pfrommer 2000 | 16/23 | 10/23 |
Comparison 2 One type of anal plug versus another type, Outcome 2 Feeling of security.
| Study | PU plug | PVA plug |
| Pfrommer 2000 | 7/23 | 15/23 |
Comparison 2 One type of anal plug versus another type, Outcome 3 Loss of plug.
| Study | PU plug | PVA plug |
| Pfrommer 2000 | 9/23 | 16/23 |
Comparison 2 One type of anal plug versus another type, Outcome 4 Inconvenience.
| Study | PU plug | PVA plug |
| Pfrommer 2000 | 17/23 | 8/23 |
Comparison 2 One type of anal plug versus another type, Outcome 5 Overall satisfaction.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 General health improved ‐ adults Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Bodily pain improved ‐ adults Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3 Well being (adults) improved Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.1 Full of life | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Very nervous | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.3 Down in the dumps | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.4 Calm and peaceful | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.5 Lot of energy | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.6 Downhearted and low | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.7 Feel worn out | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.8 Happy | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.9 Tired | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Condition‐specific measures of faecal incontinence improved Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4.1 Protection | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 Rash/skin problems | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.3 Unpleasant odour | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.4 Staining/smearing | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.5 Bowel movement in undergarments (last two weeks) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.6 Frequency of unpleasant odours | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.7 Bowel movements in undergarments (on average day) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.8 Soiled/stained undergarment (on average day) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.9 Prevents staying away from home | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.10 Must avoid long journeys | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.11 Must always have a toilet nearby | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Stool frequency Show forest plot | Other data | No numeric data | ||
| 6 Costs Show forest plot | Other data | No numeric data | ||
| 7 Achievement of pseudo‐continence Show forest plot | Other data | No numeric data | ||
| 8 Intolerance of intervention Show forest plot | Other data | No numeric data | ||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Plug effectiveness: number of people with no soiling Show forest plot | Other data | No numeric data | ||
| 2 Feeling of security Show forest plot | Other data | No numeric data | ||
| 3 Loss of plug Show forest plot | Other data | No numeric data | ||
| 4 Inconvenience Show forest plot | Other data | No numeric data | ||
| 5 Overall satisfaction Show forest plot | Other data | No numeric data | ||

