تسکین درد برای زنان تحت بازیابی اووسیت در تکنیکهای کمک‐باروری
چکیده
پیشینه
روشهای متنوعی برای آرامسازی و آنالژزی (conscious sedation and analgesia; CSA) در طول بازیابی اووسیت برای کمک‐باروری (assisted reproduction) استفاده شدهاند. انتخاب عامل دارویی تحت تاثیر کیفیت داروهای آرامسازی و آنالژزیک و ملاحظات مربوط به تاثیرات زیانبار احتمالی بر پیامدهای تولید مثل قرار داشته است.
اهداف
ارزیابی اثربخشی و ایمنی روشهای مختلف آرامسازی و آنالژزی برای تسکین درد و پیامدهای بارداری در زنانی که تحت بازیابی اووسیت از طریق ترانسواژینال قرار میگیرند.
روشهای جستوجو
در نوامبر 2017 پایگاه ثبت تخصصی زنان و باروری در کاکرین؛ CENTRAL؛ MEDLINE؛ Embase؛ PsycINFO؛ CINAHL؛ و پایگاههای ثبت کارآزماییها را جستوجو کردیم. همچنین فهرست منابع را چک کرده و برای دستیابی به مطالعات بیشتر با نویسندگان مطالعات تماس گرفتیم.
معیارهای انتخاب
کارآزماییهای تصادفیسازی و کنترل شده (randomised controlled trials; RCTs) را وارد مرور کردیم که به مقایسه روشها و پروتکلهای مختلف استفاده از آرامسازی آگاهانه و آنالژزی در طول بازیابی اووسیت پرداخته بودند.
گردآوری و تجزیهوتحلیل دادهها
از روشهای استاندارد روششناسی توصیه شده توسط کاکرین استفاده کردیم. پیامدهای اولیه ما عبارت بودند از درد حین و پس از جراحی. پیامدهای ثانویه عبارت بودند از بارداری بالینی، رضایتمندی بیمار، عوارض جانبی آنالژزیک و عوارض پس از جراحی.
نتایج اصلی
ما 24 RCT (3160 زن) را در پنج مقایسه وارد مرور کردیم. مقایسههای مهم را در زیر گزارش میکنیم. کیفیت شواهد عمدتا به دلیل گزارشدهی ضعیف و عدم دقت، به طور کلی پائین یا بسیار پائین بود.
1. CSA در برابر سایر مداخلات فعال
تمامی شواهد برای این مقایسه دارای کیفیت بسیار پائین بود.
CSA در برابر CSA به علاوه طب سوزنی (acupuncture) یا طب سوزنی الکتریکی (electroacupuncture)
دادهها نشان میدهند که CSA به علاوه طب سوزنی (تفاوت میانگین (MD): 1.00؛ 95% فاصله اطمینان (CI): 0.18 تا 1.82؛ 62 زن) یا طب سوزنی الکتریکی (MD: 3.00؛ 95% CI؛ 2.23 تا 3.77؛ 62 زن) در تسکین درد حین جراحی روی مقیاس آنالوگ بصری (visual analogue scale; VAS) 0 تا 10 اثربخشتر هستند.
دادهها همچنین نشان میدهند که CSA به علاوه طب سوزنی (MD: ‐0.60؛ 95% CI؛ 0.10 تا 1.30؛ 61 زن) یا طب سوزنی الکتریکی (MD: 2.10؛ 95% CI؛ 1.40 تا 2.80؛ 61 زن) در تسکین درد پس از جراحی (0 تا 10 VAS) اثربخشتر هستند.
شواهد برای نشان دادن اینکه نرخهای بارداری بالینی بین CSA و CSA به علاوه طب سوزنی تفاوت داشته یا خیر، کافی نیست (نسبت شانش (OR): 0.61؛ 95% CI؛ 0.20 تا 1.86؛ 61 زن). CSA به تنهایی ممکن است با بارداریهای کمتری نسبت به CSA به علاوه طب سوزنی الکتریکی همراه باشد (OR: 0.22؛ 95% CI؛ 0.07 تا 0.66؛ 61 زن).
شواهد برای نشان دادن اینکه تفاوتی از لحاظ نرخهای استفراغ بین CSA و CSA به علاوه طب سوزنی (OR: 1.64؛ 95% CI؛ 0.46 تا 5.88؛ 62 زن) یا طب سوزنی الکتریکی (OR: 1.09؛ 95% CI؛ 0.33 تا 3.58؛ 62 زن) وجود داشته یا خیر، کافی نبود.
نویسندگان کارآزماییها هیچ گونه داده قابل استفادهای را برای سایر پیامدهای مورد نظر مطالعه ارائه نکرده بودند.
CSA در برابر داروهای بیحسی عمومی (general anaesthesia)
تسکین درد پس از جراحی در گروه CSA بیشتر بود (0 تا 3 لیکرت: تفاوت میانگین (MD): 1.9؛ 95% CI؛ 2.24 تا 1.56؛ یک RCT؛ 50 زن).
شواهد برای نشان دادن اینکه نرخهای بارداری بالینی بین گروهها مختلف بوده یا خیر، کافی نبود (OR: 1.00؛ 95% CI؛ 0.43 تا 2.35؛ دو RCT؛ 108 زن؛ I2 = 0%).
شواهد برای نشان دادن اینکه نرخهای استفراغ (OR: 0.46؛ 95% CI؛ 0.08 تا 2.75؛ یک RCT؛ 50 زن) یا انسداد راه هوایی (OR: 0.14؛ 95% CI؛ 0.02 تا 1.22؛ یک RCT؛ 58 زن،) بین گروهها مختلف بوده یا خیر، کافی نبود. تعداد زنان کمتری در گروه CSA به ماسک ونتیلاسیون احتیاج پیدا کرده بودند (OR: 0.05؛ 95% CI؛ 0.01 تا 0.20؛ یک RCT؛ 58 زن).
شواهد همچنین برای نشان دادن اینکه گروهها به لحاظ نرخ رضایتمندی متفاوت هستند یا خیر، کافی نبود (OR: 0.66؛ 95% CI؛ 0.11 تا 4.04؛ دو RCT؛ 108 زن؛ I2 = 34%؛ شواهد با کیفیت بسیار پائین).
نویسندگان کارآزماییها هیچ داده قابل استفادهای را برای پیامدهای مورد نظر مطالعه ارائه نکرده بودند.
2. CSA + بلوک پاراسرویکال (PCB) در برابر سایر مداخلات
CSA + PCB در برابر طب سوزنی الکتریکی + PCB
نمرات درد حین عمل در گروه CSA + PCB کمتر بودند (0 تا 10 در VAS: MD: ‐0.66؛ 95% CI؛ 0.93‐ تا 0.39‐؛ 781 زن؛ I2 = 76%؛ شواهد با کیفیت پائین).
شواهد کافی برای نشان دادن اینکه نرخهای بارداری بالینی بین گروهها مختلف بود یا خیر، وجود نداشت (OR: 0.96؛ 95% CI؛ 0.72 تا 1.29؛ 783 زن؛ I2 = 9%؛ شواهد با کیفیت پائین).
نویسندگان کارآزماییها هیچ گونه داده قابل استفادهای را برای سایر پیامدهای مورد نظر مطالعه ارائه نکرده بودند.
CSA + PCB در برابر داروی بیحسی عمومی
شواهد برای نشان دادن اینکه نمرات درد پس از جراحی بین گروهها متفاوت بودند یا خیر، کافی نبود (0 تا 10 در VAS: MD: ‐0.49؛ 95% CI؛ 0.13 تا 1.11؛ 50 زن؛ شواهد با کیفیت بسیار پائین).
شواهد کافی برای نشان دادن اینکه نرخهای بارداری بالینی بین گروهها مختلف بود یا خیر، وجود نداشت (OR: 0.70؛ 95% CI؛ 0.22 تا 2.26؛ 51 زن؛ شواهد با کیفیت بسیار پائین).
نویسندگان کارآزماییها هیچ گونه داده قابل استفادهای را برای سایر پیامدهای مورد نظر مطالعه ارائه نکرده بودند.
CSA + PCB در برابر داروی بیحسی نخاعی (spinal anaesthesia)
نمرات درد پس از جراحی در گروه CSA + PCB بالاتر بودند (0 تا 10 در VAS: MD: 1.02؛ 95% CI؛ 0.48 تا 1.56؛ 36 زن؛ شواهد با کیفیت بسیار پائین).
شواهد کافی برای نشان دادن اینکه نرخهای بارداری بالینی بین گروهها مختلف بود یا خیر، وجود نداشت (OR: 0.93؛ 95% CI؛ 0.24 تا 3.65؛ 38 زن؛ شواهد با کیفیت بسیار پائین).
نویسندگان کارآزماییها هیچ گونه داده قابل استفادهای را برای سایر پیامدهای مورد نظر مطالعه ارائه نکرده بودند.
CSA + PCB در برابر PCB
شواهد کافی برای نشان دادن اینکه نرخهای بارداری بالینی (OR: 0.93؛ 95% CI؛ 0.44 تا 1.96؛ 150 زن؛ شواهد با کیفیت پائین) یا رضایتمندی (OR: 1.63؛ 95% CI؛ 0.68 تا 3.89؛ 150 زن؛ شواهد با کیفیت پائین) بین گروهها مختلف بود یا خیر، وجود نداشت.
نویسندگان کارآزماییها هیچ گونه داده قابل استفادهای را برای سایر پیامدهای مورد نظر مطالعه ارائه نکرده بودند.
CSA + PCB در برابر CSA به تنهایی
شواهد کافی برای نشان دادن اینکه نرخهای بارداری بالینی بین گروهها مختلف بود یا خیر، وجود نداشت (OR: 0.62؛ 95% CI؛ 0.28 تا 1.36؛ یک RCT؛ 100 زن؛ شواهد با کیفیت بسیار پائین). نرخهای تهوع و استفراغ پس از جراحی در گروه CS + PCB پائینتر بودند (OR: 0.42؛ 95% CI؛ 0.18 تا 0.97؛ دو RCT؛ 140 زن؛ I2 = 40%؛ شواهد با کیفیت بسیار پائین).
نویسندگان کارآزماییها هیچ گونه داده قابل استفادهای را برای سایر پیامدهای مورد نظر مطالعه ارائه نکرده بودند.
نتیجهگیریهای نویسندگان
شواهد از برتری یک روش یا تکنیک خاص بر روش یا تکنیک دیگر از نظر آرامسازی و آنالژزی برای تسکین درد حین و پس از بازیایی اووسیت، حمایت نمیکند. استفاده همزمان از داروی آرامسازی در ترکیب با آنالژزی از جمله مخدرها (opiates) و تسهیل شده از طریق بلوک پاراسرویکال (paracervical block) یا تکنیکهای طب سوزنی (acupuncture)، در مقایسه با استفاده از یک مودالیتی به تنهایی، درد را بهتر تسکین میدهد. شواهد کافی برای اینکه به طور قطعی نشان دهند هر یک از مداخلات بر نرخهای بارداری تاثیرگذار بوده یا خیر، وجود نداشت. تمامی تکنیکهای مرور شده با درجه بالایی از رضایتمندی بیمار رابطه داشتند. ترجیحات زنان و دسترسپذیری منابع برای انتخاب گزینه درمانی برای تسکین درد، بهتر است در عمل مورد توجه قرار بگیرد.
PICOs
خلاصه به زبان ساده
تسکین درد برای زنان تحت بازیابی اووسیت در تکنیکهای کمک‐باروری
سوال مطالعه مروری
نویسندگان مرور کاکرین اثربخشی و ایمنی روشهای مورد استفاده برای تسکین درد در زنان در طول بازیابی اووسیت از طریق ترانسواژینال (transvaginal oocyte retrieval)‐ تکنیک مورد استفاده برای جمعآوری تخمکها از تخمدانها، برای باروری خارج از بدن ‐ را بررسی کردند.
پیشینه
آرامسازی آگاهانه (conscious sedation) عبارت است از استفاده از یک یا تعدادی دارو برای ایجاد حالتی از آرامش (relaxation) که امکان اجرای پروسه درمانی را فراهم کرده و در آن ارتباط کلامی با بیمار در طول دوره آرامسازی برقرار بماند. آرامسازی و آنالژزی روشهای هستند که برای رفع درد در طول جراحی برای بازیابی تخمکهای به دست آمده از تخمدانها به عنوان بخشی از پروسیجرهای باروری آزمایشگاهی (in vitro fertilisation) (یعنی یک محیط مصنوعی مانند آزمایشگاه) استفاده میشوند. نگرانیهایی درباره داروهای آرامسازی و تسکین دهنده درد وجود دارد مبنی بر اینکه آنها ممکن است دارای عوارض جانبی روی نرخهای بارداری باشند.
ویژگیهای مطالعه
این مرور منجر به شناسایی 24 کارآزمایی تصادفیسازی و کنترل شده، شامل 3160 زن شد که به مقایسه تاثیرات پنج روش مختلف آرامسازی و تسکین درد شامل بیحسی عمومی (general anaesthesia) پرداخته بودند. یک کارآزمایی تصادفیسازی و کنترل شده از روشهای پژوهش استفاده میکند که هدف آنها کاهش سوگیری در زمان تست یک روش درمانی جدید از طریق تخصیص شرکتکنندگان به صورت تصادفی (برای مثال بر اساس شانس) بین گروه درمان و کنترل است. شواهد تا نوامبر 2017 بهروز است.
نتایج کلیدی
شواهد از برتری یک روش یا تکنیک خاص بر روش یا تکنیک دیگر از نظر آرامسازی و آنالژزی برای تسکین درد حین و پس از بازیایی اووسیت، حمایت نمیکند. استفاده همزمان از داروی آرامسازی در ترکیب با آنالژزی از جمله مخدرها (opiates) و تسهیل شده از طریق بلوک پاراسرویکال (paracervical block) یا تکنیکهای طب سوزنی (acupuncture)، در مقایسه با استفاده از یک مودالیتی به تنهایی، درد را بهتر تسکین میدهد. شواهد کافی برای اینکه به طور قطعی نشان دهند هر یک از مداخلات بر نرخهای بارداری تاثیرگذار بوده یا خیر، وجود نداشت. تمامی تکنیکهای مرور شده با درجه بالایی از رضایتمندی بیمار رابطه داشتند. ترجیحات زنان و دسترسی به منابع برای انتخاب گزینه درمانی برای تسکین درد، بهتر است در عمل مورد توجه قرار بگیرد.
کیفیت شواهد
کیفیت شواهد به طور کلی به دلیل ضعیف بودن روشهای گزارشدهی و کوچک بودن حجم نمونه با نرخ حوادث کم، پائین یا بسیار پائین بود. از آنجایی که تجربه درد در زنان و آگاهی آنها از استراتژیهای مقابله با آن متنوع است، گزینه درمانی بهینه ممکن است مختص فرد (individualised) طراحی شود.
Authors' conclusions
Summary of findings
| Conscious sedation and analgesia (CSA) compared with CSA+acupuncture for women undergoing oocyte retrieval for assisted reproduction | ||||||
| Patient or population: women undergoing oocyte retrieval for assisted reproduction | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No. of participants | Quality of the evidence | Comments | |
| Risk with CSA + acupuncture | Risk with CSA only (95% CI) | |||||
| Intraoperative pain | Mean intraoperative pain score in the comparison group was 4.9 points on a 0 to 10 VAS. | Mean score in the CSA‐only group was 1 point higher | ‐ | 62 | ⊕⊝⊝⊝ | |
| Postoperative pain | Mean postoperative pain score in the comparison group was 3.2 on a 0 to 10 VAS. | Mean score in the CSA‐only group was 0.6 points higher | ‐ | 61 | ⊕⊝⊝⊝ | |
| Pregnancy | 344 per 1000 | 242 per 1000 (95 to 493) | OR 0.61 (0.20 to 1.86) | 61 | ⊕⊝⊝⊝ | |
| Patient satisfaction | No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| Side effects (postoperative vomiting and/or vomiting) | 156 per 1000 | 233 per 1000 | OR 1.64 | 62 | ⊕⊝⊝⊝ | |
| Postoperative complications | No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| *The risk in the intervention group (and its 95% confidence interval) is based on the risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence. | ||||||
| aDowngraded one level for serious risk of bias: unclear risk of bias in one or two domains. bDowngraded two levels for very serious imprecision: very small sample size and low event rate and/or wide confidence intervals compatible with benefit in either group or no effect. | ||||||
| Conscious sedation and analgesia (CSA) compared with CSA + electro‐acupuncture for women undergoing oocyte retrieval for assisted reproduction | ||||||
| Patient or population: women undergoing oocyte retrieval for assisted reproduction | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No. of participants | Quality of the evidence | Comments | |
| Risk with CSA + electro‐acupuncture | Risk with CSA only (95% CI) | |||||
| Intraoperative pain | Mean intraoperative pain score in the comparison group was 2.9 points on a 0 to 10 VAS. | Mean score in the CSA‐only group was 3 points higher | ‐ | 62 | ⊕⊝⊝⊝ | |
| Postoperative pain | Mean postoperative pain score in the comparison group was 1.1 on a 0 to 10 VAS. | Mean score in the CSA‐only group was 2.1 points higher | ‐ | 61 | ⊕⊝⊝⊝ | |
| Pregnancy | 594 per 1000 | 243 per 1000 (95 to 491) | OR 0.22 (0.07 to 0.66) | 61 | ⊕⊝⊝⊝ | |
| Patient satisfaction | No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| Side effects (postoperative vomiting and/or vomiting) | 218 per 1000 | 233 per 1000 | OR 1.09 | 62 | ⊕⊝⊝⊝ | |
| Postoperative complications | Airway obstruction: No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| Need for mask ventilation: No studies reported this outcome. | Not estimable | ‐ | ‐ | |||
| *The risk in the intervention group (and its 95% confidence interval) is based on the risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence. | ||||||
| aDowngraded one level for serious risk of bias: unclear risk of bias in one or two domains. bDowngraded two levels for very serious imprecision: very small sample size and event rate. | ||||||
| Conscious sedation and analgesia (CSA) compared to general analgesia for women undergoing oocyte retrieval for assisted reproduction | ||||||
| Patient or population: women undergoing oocyte retrieval for assisted reproduction | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No. of participants | Quality of the evidence | Comments | |
| Risk with GA | Risk with CSA only (95% CI) | |||||
| Intraoperative pain | No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| Postoperative pain | Mean postoperative pain score in the comparison group was 2.1 points on a 0 to 3 Likert scale. | Mean score in the CSA‐only group was 1.9 points lower | ‐ | 50 | ⊕⊝⊝⊝ | |
| Pregnancy | 278 per 1000 | 278 per 1000 (142 to 475) | OR 1.00 (0.43 to 2.35) | 108 | ⊕⊝⊝⊝ | |
| Patient satisfaction (report of 'satisfactory') | 981 per 1000 | 972 per 1000 (854 to 995) | OR 0.66 (0.11 to 4.04) | 108 | ⊕⊝⊝⊝ | |
| Side effects (postoperative vomiting and/or vomiting) | 160 per 1000 | 81 per 1000 | OR 0.46 | 50 | ⊕⊝⊝⊝ | |
| Postoperative complications | Airway obstruction: 207 per 1000 | 35 per 1000 | OR 0.14 | 58 | ⊕⊝⊝⊝ | |
| Need for mask ventilation: 793 per 1000 | 161 per 1000 | OR 0.05 | 58 | ⊕⊝⊝⊝ | ||
| *The risk in the intervention group (and its 95% confidence interval) is based on the risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence. | ||||||
| aDowngraded two levels for very serious imprecision: very small sample size and event rate and/or wide confidence intervals compatible with benefit in either group or no effect. bDowngraded one level for serious risk of bias: unclear risk of bias in one or two domains. | ||||||
| Conscious sedation and analgesia (CSA) plus PCB compared with electro‐acupuncture plus PCB for women undergoing oocyte retrieval for assisted reproduction | ||||||
| Patient or population: women undergoing oocyte retrieval for assisted reproduction | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No. of participants | Quality of the evidence | Comments | |
| Risk with electro‐acupuncture + PCB | Risk with CSA + PCB (95% CI) | |||||
| Intraoperative pain | Mean intraoperative pain score in the comparison group was 2.6 to 4.85 points on a 0 to 10 VAS. | Mean score in the CSA‐only group was 0.66 points lower | ‐ | 781 | ⊕⊕⊝⊝ | |
| Postoperative pain | No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| Pregnancy | 367 per 1000 | 358 per 1000 (295 to 428) | OR 0.96 (0.72 to 1.29) | 783 | ⊕⊕⊝⊝ | |
| Patient satisfaction | No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| Side effects (postoperative vomiting and/or vomiting) | No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| Postoperative complications | No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| *The risk in the intervention group (and its 95% confidence interval) is based on the risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence. | ||||||
| aDowngraded one level for serious risk of bias: unclear risk of bias in one or two domains. bDowngraded one level for serious inconsistency (I2 = 76%). cDowngraded one level for serious imprecision: wide confidence intervals compatible with benefit in either group or no effect. | ||||||
| Conscious sedation and analgesia (CSA) plus paracervical block (PCB) compared with general anaesthetic (GA) for women undergoing oocyte retrieval for assisted reproduction | ||||||
| Patient or population: women undergoing oocyte retrieval for assisted reproduction | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No. of participants | Quality of the evidence | Comments | |
| Risk with GA | Risk with CSA + PCB (95% CI) | |||||
| Intraoperative pain | ||||||
| Postoperative pain | Mean postoperative pain score in the comparison group was 0.68 points on a 0 to 10 VAS. | Mean score in the CSA‐only group was 0.49 points higher | ‐ | 50 | ⊕⊝⊝⊝ | |
| Pregnancy | 375 per 1000 | 296 per 1000 (117 to 576) | OR 0.70 (0.22 to 2.26) | 51 | ⊕⊝⊝⊝ | |
| Patient satisfaction | No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| Postoperative complications | No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| *The risk in the intervention group (and its 95% confidence interval) is based on the risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence. | ||||||
| aDowngraded one level for serious risk of bias: unclear risk of bias in one or two domains. bDowngraded two levels for very serious imprecision: small sample size and low event rate, wide confidence intervals compatible with benefit in either group or no effect. | ||||||
| Conscious sedation and analgesia (CSA) plus paracervical block (PCB) compared with spinal anaesthesia for women undergoing oocyte retrieval for assisted reproduction | ||||||
| Patient or population: women undergoing oocyte retrieval for assisted reproduction | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No. of participants | Quality of the evidence | Comments | |
| Risk with spinal anaesthesia | Risk with CSA + PCB (95% CI) | |||||
| Intraoperative pain | No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| Postoperative pain | Mean postoperative pain score in the comparison group was 0.15 on a 0 to 10 VAS, | Mean score in the CSA‐only group was 1.02 points higher | ‐ | 36 | ⊕⊝⊝⊝ | |
| Pregnancy | 375 per 1000 | 358 per 1000 (126 to 687) | OR 0.93 (0.24 to 3.65) | 38 | ⊕⊝⊝⊝ | |
| Patient satisfaction | No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| Side effects (postoperative vomiting and/or vomiting) | No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| Postoperative complications | No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| *The risk in the intervention group (and its 95% confidence interval) is based on the risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence. | ||||||
| aDowngraded one level for serious risk of bias: unclear risk of bias in one or two domains. bDowngraded two levels for very serious imprecision: very small sample size and low event rate, wide confidence intervals compatible with benefit in either group or no effect. | ||||||
| Conscious sedation and analgesia (CSA) plus paracervical block (PCB) compared with PCB only for women undergoing oocyte retrieval for assisted reproduction | ||||||
| Patient or population: women undergoing oocyte retrieval for assisted reproduction | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No. of participants | Quality of the evidence | Comments | |
| Risk with PCB only | Risk with CSA + PCB (95% CI) | |||||
| Intraoperative pain | No studies reported this outcome. | Not estimable | ‐ | ‐ | ‐ | |
| Postoperative pain | No studies reported this outcome. | Not estimable | ‐ | ‐ | ‐ | |
| Pregnancy | 253 per 1000 | 240 per 1000 (130 to 399) | OR 0.93 (0.44 to 1.96) | 150 | ⊕⊕⊝⊝ | |
| Patient satisfaction | 800 per 1000 | 867 per 1000 | OR 1.63 (0.68 to 3.89) | 150 | ⊕⊕⊝⊝ | |
| Side effects (postoperative vomiting and/or vomiting) | No studies reported this outcome | Not estimable | ‐ | ‐ | ||
| Postoperative complications | No studies reported this outcome | Not estimable | ‐ | ‐ | ||
| *The risk in the intervention group (and its 95% confidence interval) is based on the risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence. | ||||||
| aDowngraded two levels for very serious imprecision: low event rates and wide confidence intervals compatible with benefit in either group or no effect. | ||||||
| Conscious sedation and analgesia (CSA) plus paracervical block (PCB) compared with CSA alone | ||||||
| Patient or population: women undergoing oocyte retrieval for assisted reproduction | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No. of participants | Quality of the evidence | Comments | |
| Risk with CSA alone | Risk with CSA + PCB (95% CI) | |||||
| Intraoperative pain | No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| Postoperative pain | No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| Pregnancy | 600 per 1000 | 482 per 1000 (296 to 671) | OR 0.62 (0.28 to 1.36) | 100 | ⊕⊝⊝⊝ | |
| Patient satisfaction | No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| Side effects (postoperative vomiting and/or vomiting) | 300 per 1000 | 153 per 1000 | OR 0.42 | 140 | ⊕⊝⊝⊝ | |
| Postoperative complications | No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| *The risk in the intervention group (and its 95% confidence interval) is based on the risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence. | ||||||
| aDowngraded one level for serious risk of bias: unclear risk of bias in one or two domains. bDowngraded two levels for very serious imprecision: small sample size, very low event rates, and wide confidence intervals compatible with benefit in the CSA + PCB group or with no meaningful effect. | ||||||
Background
Description of the condition
Transvaginal retrieval of oocytes from the ovary is a fundamental step of in vitro fertilisation (IVF) treatment. Although this approach is less invasive and of shorter duration than laparoscopic retrieval of oocytes, which is no longer common clinical practice, it remains a stressful and painful procedure, which requires analgesia and conscious sedation (Ng 2001).
Description of the intervention
Conscious sedation is defined by the American Society of Anaesthetists as “a drug‐induced depression of consciousness during which patients respond purposefully to verbal commands, either alone or accompanied by light tactile stimulation. No interventions are required to maintain a patent airway, and spontaneous ventilation is adequate. Cardiovascular function is usually maintained” (ASA 2015). Loss of consciousness should be unlikely due to the agents and techniques selected (Skelly 1996).
Analgesia is defined as “a state of reduced pain perception” (White 1987). An ideal analgesia is one that has the capability of offering pain relief without impairing consciousness.
Conscious sedation and analgesia may be combined for optimal effect. A variety of drugs and combinations thereof have been used to modify pain and anxiety during oocyte retrieval. Methods currently used to provide pain relief during transvaginal oocyte retrieval include conscious sedation, neuraxial anaesthesia (epidural or spinal), injection of local anaesthetic agents into the cervix (paracervical block), and alternative treatments such as acupuncture or electroacupuncture (Sharma 2015). General anaesthesia may be used for transvaginal oocyte retrieval; however, this approach has important resource requirements and many IVF units opt for conscious sedation and analgesia.
The primary goal of clinicians is to provide safe and effective sedation and analgesia that contribute to optimum surgical conditions and fast postoperative recovery. The aims of general and regional (epidural and spinal) anaesthesia are clear. The former renders the patient unconscious with no awareness of pain, and the latter achieves the endpoint of no sensation (of pain) while consciousness is maintained. Sedation, however, is much less clear or well defined than anaesthesia and has a smaller evidence base to guide practice. Giving too much or too little sedation can be hazardous, as too much sedation would be dangerous and too little would be ineffective. In addition, analgesics such as fentanyl and pethidine in high dosages can produce sedation, and intravenous anaesthetics such as propofol (sedative and analgesia) at subanaesthetic dosages can have sedative effects.
How the intervention might work
The pain experienced by patients during oocyte retrieval is caused by puncture of vaginal skin and the ovarian capsule by the aspirating needle and manipulation of the needle within the ovary during the procedure. It has been suggested that the pain associated with oocyte retrieval is intermittent rather than continuous (Zelcer 1992). Thus, an ideal strategy for pain relief is one that allows maximum flexibility to respond to the changing requirements of women undergoing oocyte retrieval. Patient‐controlled analgesia may facilitate an individualised approach by allowing women a degree of control over drug administration.
Acupuncture practices are based on the hypothesis that human physiological functions are controlled by Yin and Yang channels, which allow the flow of hypothetical “Qi” through the body (Han 2011). It is believed that blockage of these channels can lead to illness and pain. Insertion of acupuncture needles into specific acupuncture sites to resolve blockage and allow free flow of “Qi” is traditionally believed to relieve patient symptoms and is often used for pain relief (Han 2011).
Manual acupuncture involves insertion and manipulation of acupuncture needles within specific predetermined acupuncture sites. In electrical acupuncture, an additional current is administered through the acupuncture needles to stimulate acupoints (Zhao 2008).
Why it is important to do this review
Most oocyte retrievals are performed with the patient under conscious sedation: This approach is applied in 84% of IVF clinics in the UK (Elkington 2003), as well as 95% of IVF centres in the United States (Ditkoff 1997). However, 16% of UK clinics and about 50% of clinics in Germany have used general anaesthesia for IVF procedures (Rjosk 1993). Another survey showed that 48% of IVF clinics in the UK used conscious sedation; 29% general anaesthesia; 12% sedation combined with regional anaesthesia; and 2% regional anaesthesia; 9% offered a choice of anaesthesia for IVF procedures (Bokhari 1999). These reported variations in methods used for pain relief raise questions about the potential advantages and disadvantages of different methods and protocols for conscious sedation and analgesia. The efficacy of the various sedative‐analgesic combinations, including general anaesthesia, for women undergoing oocyte retrieval is of interest to practitioners. This systematic review aims to assess the effectiveness and safety of different methods of achieving conscious sedation and analgesia in women undergoing transvaginal oocyte retrieval, in terms of pain relief during and after the procedure, pregnancy outcomes, postoperative complications, and patient satisfaction.
Objectives
To assess the effectiveness and safety of different methods of conscious sedation and analgesia for pain relief and pregnancy outcomes in women undergoing transvaginal oocyte retrieval.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled trials (RCTs) only and excluded quasi‐randomised and cross‐over trials.
Types of participants
Women undergoing transvaginal oocyte retrieval during IVF treatment.
Types of interventions
-
Conscious sedation and analgesia versus no treatment or placebo
-
Conscious sedation and analgesia versus different methods such as general and spinal anaesthesia, including acupuncture and paracervical block
-
Different protocols of conscious sedation and analgesia such as patient‐controlled or physician‐controlled sedation
We excluded from this review trials involving the use of local anaesthesia such as vaginal lidocaine gel.
Types of outcome measures
Primary outcomes
-
Intraoperative pain score, defined as pain reported during or immediately after oocyte retrieval as measured on a visual analogue scale (VAS), a Likert scale, or another defined numerical or non‐numerical scale
-
Postoperative pain score, defined as pain reported at some time (minutes or hours) after oocyte retrieval as measured on a VAS, a Likert scale, or another defined numerical or non‐numerical scale
For the purposes of this review, we have defined postoperative pain as pain measured at some time after oocyte retrieval. In addition, none of the studies reporting pregnancy defined it, and in this review, we assumed that clinical pregnancy was reported, unless otherwise stated.
We converted to a 0 to 10 scale all VAS data related to pain.
Secondary outcomes
-
Live birth rate and ongoing pregnancy rate (beyond 20 weeks) per woman
-
Clinical pregnancy rate per woman (established by pregnancy test and confirmed by ultrasound)
-
Fertilisation rate per woman
-
Side effects of analgesia (nausea and vomiting)
-
Postoperative complications (airway, blood pressure, recovery time, spinal headache)
-
Patient satisfaction (women's reports of satisfaction with pain relief and anaesthetic care throughout the oocyte retrieval procedure)
Search methods for identification of studies
Electronic searches
We searched the Cochrane Gynaecology and Fertility Group (CGFG) Specialised Register (Procite platform), on 11 November 2017, to identify all RCTs that compared different methods of conscious sedation and analgesia for pain control during oocyte retrieval (refer to Appendix 1), without language restriction and in consultation with the CGFG Information Specialist.
We conducted electronic searches within the following electronic databases.
-
CENTRAL CRSO, web platform (Appendix 2) (searched 9 November 2017).
-
MEDLINE, Ovid platform, (Appendix 3) (searched from 1946 to 9 November 2017).
-
Embase, Ovid platform (Appendix 4) (searched from 1980 to 9 November 2017).
-
PsycINFO, Ovid platform (Appendix 5) (searched from 1806 to 9 November 2017).
-
CINAHL, Ebsco platform (Appendix 6) (searched from 1982 to 9 November 2017).
-
ClinicalTrials.gov search strategy; web platform (Appendix 7) (searched 10 January 2017).
-
WHO ICTRP search strategy, web platform (Appendix 8) (searched 10 December 2016).
-
Web of Science, web platform (Appendix 9) (searched 12 January 2017).
-
Portal Regional da BVS, web platform (Appendix 10) (searched 12 January 2017).
-
OpenGrey, web platform (Appendix 11) (searched 12 January 2017).
Searching other resources
We searched and checked the reference lists of the included studies. We translated one article from Turkish, one from Spanish, and four from Chinese.
Data collection and analysis
Selection of studies
Three review authors (IK, EP, RW) independently examined the titles and abstracts of articles retrieved by the search and retrieved full texts of all potentially eligible studies. Each review author independently applied the selection criteria to the trial reports, resolving disagreements by discussion and, if necessary, by consultation with one other review author (SB). IK contacted trial authors for clarification of details related to study eligibility such as allocation method.
Data extraction and management
We conducted data collection and analysis in accordance with the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). Three review authors (IK, EP, RW) independently extracted data from eligible studies using a data extraction form designed and pilot‐tested by the review authors. Review authors were not blinded to trial authors or journal of publication when doing this. We compared results and resolved any differences by discussion. A fourth review author (SB) resolved any disagreement that arose between these three review authors. Where information provided in the published report was insufficient, IK contacted the study authors to request further information and clarification.
Assessment of risk of bias in included studies
Three review authors (IK, EP, RW) independently assessed each trial for risk of bias according to the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011).
We assessed random sequence generation, concealment of allocation, blinding, completeness of outcome data (including use of intention‐to‐treat analysis), and selective outcome reporting for each trial. We also assessed other potential sources of bias. We categorised each trial as having low, unclear, or high risk of bias for each domain by applying the standards described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). When the method used to conceal allocation was not reported clearly, IK contacted the study authors for clarification.
Measures of treatment effect
For dichotomous data, we used the numbers of events in control and intervention groups of each study to calculate Mantel‐Haenszel odds ratios (ORs). For continuous data, we calculated the mean difference (MD) between treatment groups. We have presented 95% confidence intervals (CIs) for all outcomes.
Unit of analysis issues
The primary analysis was per woman randomised. For reported data that did not allow valid analysis (e.g. 'per cycle' rather than 'per woman' when women contributed more than one cycle), we computed to obtain results ‘per woman’, if possible.
Dealing with missing data
We analysed data on an intention‐to‐treat basis as far as possible, and IK contacted the trial authors to request any missing data. When no additional information was forthcoming, we assumed any missing data were the result of failure to achieve the outcome.
Assessment of heterogeneity
For each meta‐analysis, we assessed statistical heterogeneity by using I2 and Chi2 statistics. We determined that substantial heterogeneity was present if I2 was greater than 50%, or if P < 0.10 in the Chi2 test for heterogeneity (Higgins 2011). For the remaining studies, we have presented a descriptive summary of study outcomes.
Assessment of reporting biases
We planned to present a funnel plot if publication bias was questionable because some trials had not been identified (Higgins 2011), but no analysis included sufficient studies to warrant this.
Data synthesis
When appropriate, we combined dichotomous data for meta‐analysis using RevMan software and the Mantel‐Haenszel method to estimate pooled ORs with 95% CIs based on a fixed‐effect model. For continuous data, we computed weighted MDs with 95% CIs, also using a fixed‐effect model in the meta‐analysis.
We classified and analysed interventions under broad categories or strategies of pain relief, for example, types of conscious sedation and analgesia methods and administration protocols. The interventions examined were so diverse that it was not possible to quantitatively combine the results of all 24 studies. However, we were able to combine the data from four trials that compared the effects of electro‐acupuncture versus conventional medical analgesia. We also attempted meta‐analysis of the four trials comparing patient‐controlled and physician‐controlled sedation and analgesia. For the remaining studies, we have presented a descriptive summary of the outcomes of each trial.
Subgroup analysis and investigation of heterogeneity
We did not perform subgroup analysis in this review. We assessed statistical heterogeneity using the Chi2 test (with P < 0.1 as evidence of significant heterogeneity) and the I2 statistic (Higgins 2011).
Sensitivity analysis
We performed sensitivity analysis for the primary outcomes to assess whether findings of the analysis were robust, or whether the conclusions would have differed if eligibility was restricted to studies without high risk of bias.
Overall quality of the body of evidence: "Summary of findings" table
We prepared "Summary of findings" tables using GRADEpro and Cochrane methods (Higgins 2011). These tables evaluate the overall quality of the body of evidence for review outcomes (intraoperative pain, postoperative pain, pregnancy outcomes, side effects of analgesia (nausea and vomiting), postoperative complications, and patient satisfaction) for the main review comparisons (conscious sedation and analgesia vs other active interventions; conscious sedation and analgesia plus paracervical block vs other active interventions). We assessed the quality of evidence using the following GRADEpro criteria: risk of bias, consistency of effect, imprecision, indirectness, and publication bias. Two review authors working independently made judgements about evidence quality (high, moderate, low, or very low) and resolved disagreements by discussion. Review authors justified, documented, and incorporated judgements into reporting of results for each outcome.
Results
Description of studies
See Characteristics of included studies.
Results of the search
In the original review, our search strategy yielded 390 reports, 27 of which were potentially eligible for inclusion in the review. After full‐text review, we excluded 16 reports because conscious sedation was not one of the comparators (see Characteristics of excluded studies). Twelve papers met our inclusion criteria (Ben‐Shlomo 1999; Bhattacharya 1997; Cook 1993; Humaidan 2004; Lok 2002; Ng 2001; Ocal 2002; Ramsewak 1990; Stener‐Victorin 1999; Stener‐Victorin 2003; Thompson 2000; Zelcer 1992). These trials involved 1350 women who underwent oocyte retrieval. For the 2012 review update, we identified nine additional studies involving 1624 women (Coskun 2011; Gejervall 2005; Guasch 2005; Gunaydin 2007; Ma 2008; Meng 2008; Meng 2009; Ozturk 2006; Sator‐Katzenschlager 2006). For the 2018 review update, we identified three new studies involving 186 women (Elnabtity 2017; Lier 2014; Matsota 2012).
The study flow is shown in Figure 1.

Study flow diagram.
Included studies
We included in this review a total of 24 studies involving 3160 women (see Characteristics of included studies).
Study design and setting
All 24 included studies were RCTs published between 1990 and 2017. They involved a total of 3160 women (range 30 to 700) and were conducted in Austria (N = 1), China (N = 5), Israel (N = 1), Spain (N = 1), Sweden (N = 4), the Netherlands (N = 1), Greece (N = 1), Turkey (N = 4), Eygpt (N = 1), UK (N = 4), and USA (N = 1). Two were multi‐centred trials, one involving three IVF centres (Stener‐Victorin 1999), and the other involving five IVF centres (Stener‐Victorin 2003). None of these trials reported specifically that participants included egg donors. We did not identify any quasi‐randomised or cross‐over trials.
Participants
The studies included 3160 women ‐ 1545 in control groups and 1615 in intervention groups. Two trials did not report participant age (Cook 1993; Ramsewak 1990). Overall age reported in the other studies was similar, and mean participant age was between 31 and 34 years (range 22 to 46 years). All participants were women with infertility problems due to tubal factors, endometriosis, polycystic ovary syndrome (PCOS), male factors, or unexplained infertility. Three trials reported the duration of infertility as about four to five years (Bhattacharya 1997; Elnabtity 2017; Meng 2009).
Interventions
Interventions varied substantially between studies, and review authors grouped them into five broad categories for comparison.
-
Conscious sedation and analgesia versus placebo (Ramsewak 1990).
-
Conscious sedation and analgesia versus other active interventions such as general and acupuncture anaesthesia (Ben‐Shlomo 1999; Matsota 2012; Meng 2008; Meng 2009; Sator‐Katzenschlager 2006).
-
Conscious sedation and analgesia plus paracervical block versus other active interventions such as general, spinal, and acupuncture anaesthesia (Gejervall 2005; Guasch 2005; Gunaydin 2007; Humaidan 2004; Ng 2001; Ozturk 2006; Stener‐Victorin 1999; Stener‐Victorin 2003).
-
Patient‐controlled conscious sedation and analgesia versus physician‐administered conscious sedation and analgesia (Bhattacharya 1997; Lier 2014; Lok 2002; Thompson 2000; Zelcer 1992).
-
Conscious sedation and analgesia with different agents or dosages (Cook 1993; Coskun 2011; Ma 2008; Ocal 2002).
Outcomes
Primary outcomes
-
A total of 22 studies reported intraoperative pain
-
In all, 11 studies reported postoperative pain (Ben‐Shlomo 1999; Elnabtity 2017; Gejervall 2005; Guasch 2005; Humaidan 2004; Lier 2014; Lok 2002; Meng 2008; Sator‐Katzenschlager 2006; Stener‐Victorin 1999; Stener‐Victorin 2003)
-
Two studies reported the primary outcomes of pain but did not specify whether pain was measured intraoperatively or postoperatively (Meng 2009; Thompson 2000)
-
Two studies did not report the primary outcomes of pain (Cook 1993; Matsota 2012)
Secondary outcomes
-
1/24 studies reported live birth per woman (Stener‐Victorin 1999)
-
2/24 studies reported ongoing pregnancy per woman (Lier 2014; Stener‐Victorin 2003)
-
14/24 studies reported clinical pregnancy rate per woman (Ben‐Shlomo 1999; Coskun 2011; Gejervall 2005; Guasch 2005; Humaidan 2004; Lier 2014; Lok 2002; Matsota 2012; Ng 2001; Ozturk 2006; Sator‐Katzenschlager 2006; Stener‐Victorin 1999; Stener‐Victorin 2003; Thompson 2000)
-
5/24 studies reported fertilisation rate per woman (Ben‐Shlomo 1999; Lok 2002; Matsota 2012; Ng 2001; Ozturk 2006)
-
13/24 studies reported side effects (nausea and vomiting) (Coskun 2011; Elnabtity 2017; Guasch 2005; Gunaydin 2007; Lier 2014; Ma 2008; Matsota 2012; Meng 2009; Ozturk 2006; Sator‐Katzenschlager 2006; Stener‐Victorin 1999; Stener‐Victorin 2003; Zelcer 1992)
-
5/24 studies reported complications (transient loss of consciousness; loss of airway) (Cook 1993; Coskun 2011; Guasch 2005; Matsota 2012; Thompson 2000)
-
15/24 studies reported patient satisfaction (Ben‐Shlomo 1999; Bhattacharya 1997; Cook 1993; Coskun 2011; Elnabtity 2017; Gejervall 2005; Guasch 2005; Gunaydin 2007; Lier 2014; Lok 2002; Matsota 2012; Ng 2001; Ozturk 2006; Sator‐Katzenschlager 2006; Thompson 2000)
No studies reported the incidence of abandoned procedures.
Excluded studies
See Characteristics of excluded studies.
After full‐text screening, we excluded 25 studies for the following reasons.
-
20/25 studies did not include conscious sedation and analgesia as a comparator.
-
1/25 studies did not provide clear inclusion criteria for the population and we received no response from trial authors when contacted.
-
1/25 studies compared conscious sedation and analgesia between different populations.
-
3/25 studies were abstracts, and we were unable to obtain evidence of randomisation.
Risk of bias in included studies
See Risk of bias in included studies, Figure 2, and Figure 3.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Nineteen studies were at low risk of selection bias related to random sequence generation, as they used computer randomisation or a random numbers table. Six studies were at unclear risk of bias, as they did not describe the randomisation method used (Cook 1993; Elnabtity 2017; Gunaydin 2007; Ocal 2002; Ozturk 2006; Zelcer 1992). Eight studies did not describe allocation concealment and were at unclear risk of bias in this domain (Gejervall 2005; Guasch 2005; Lier 2014; Ma 2008; Meng 2009; Ocal 2002; Sator‐Katzenschlager 2006; Zelcer 1992).
Blinding
Blinding status could affect findings for the outcomes of pain, side effects, and women’s satisfaction. The subjective nature of pain has traditionally made it difficult to assess the efficacy of techniques for analgesia. We did not consider that blinding was likely to influence risk of performance bias for the outcomes of live birth and ongoing pregnancy. However, we noted the potential for bias for the outcomes of fertilisation and subsequent clinical pregnancy when operators were not blinded to allocation. Three studies reported adequate blinding of administrators of interventions to group allocation (Gejervall 2005; Ng 2001; Sator‐Katzenschlager 2006), and we consider these studies to be at low risk of bias. For 17 studies, blinding was not possible because of the nature of interventions such as general anaesthesia or techniques involving paracervical block (Ben‐Shlomo 1999; Bhattacharya 1997; Cook 1993; Gejervall 2005; Gunaydin 2007; Humaidan 2004; Lier 2014; Lok 2002; Matsota 2012; Meng 2008; Meng 2009; Ocal 2002; Ozturk 2006; Stener‐Victorin 1999; Stener‐Victorin 2003; Thompson 2000; Zelcer 1992), and we consider these studies to be at unclear risk of bias. Three studies described use of placebo identical to the intervention and were deemed to be at low risk of performance bias for both subjective and objective outcomes (Ng 2001; Ramsewak 1990; Sator‐Katzenschlager 2006).
Seven studies described blinding of outcome assessors for subjective outcomes of pain (Cook 1993; Gejervall 2005; Guasch 2005; Matsota 2012; Ng 2001; Sator‐Katzenschlager 2006; Zelcer 1992), and we consider these studies to be at low risk of performance bias for subjective outcomes. In one study (Coskun 2011), an independent blinded observer unaware of the women’s allocation status recorded postoperative side effects.
Incomplete outcome data
Eighteen studies analysed all or most (> 99%) randomised women, and we judged these studies to be at low risk of bias. For three studies, loss to follow‐up ranged from 4% to 20% (Lok 2002; Ramsewak 1990; Stener‐Victorin 2003). We judged these studies to be at unclear to high risk of attrition bias.
Selective reporting
All 24 studies reported outcomes prespecified in the methods section. Some outcomes such as plasma prolactin and follicular cortisol levels, sedation concentrations, recovery status, number of embryos transferred, oocyte retrieval rate, psychometric tests, and neuropeptide Y (NPY) level of follicular fluid were not of interest for this review (Cook 1993; Coskun 2011; Gejervall 2005; Guasch 2005; Gunaydin 2007; Ng 2001; Ozturk 2006); we neither extracted nor analysed these data.
Other potential sources of bias
We assessed publication bias by using a funnel plot for primary outcomes when appropriate. Ten studies did not compare causes of infertility in intervention and control groups (Ben‐Shlomo 1999; Cook 1993; Coskun 2011; Guasch 2005; Gunaydin 2007; Meng 2009; Ocal 2002; Ramsewak 1990; Thompson 2000; Zelcer 1992). Demographic details were absent from one study (Ramsewak 1990), and another study reported only women’s age (Ocal 2002). The risk of bias related to potential baseline differences between the two groups in these studies cannot be established, and we consider these studies to be at unclear risk of bias. In one study, women in the control group were younger than those in the intervention groups, although the cause of infertility was similar between groups (Lok 2002). We found no additional potential sources of other bias in the remaining studies.
Effects of interventions
See: Summary of findings for the main comparison Conscious sedation and analgesia (CSA) compared with CSA+acupuncture for women undergoing oocyte retrieval for assisted reproduction; Summary of findings 2 Conscious sedation and analgesia (CSA) compared with CSA + electro‐acupuncture for women undergoing oocyte retrieval for assisted reproduction; Summary of findings 3 Conscious sedation and analgesia compared with general analgesia for women undergoing oocyte retrieval for assisted reproduction; Summary of findings 4 Conscious sedation and analgesia (CSA) + paracervical block (PCB) versus electro‐acupuncture + PCB; Summary of findings 5 Conscious sedation and analgesia (CSA) + paracervical block (PCB) versus general anaesthesia; Summary of findings 6 Conscious sedation and analgesia (CSA) + paracervical block (PCB) versus spinal anaesthesia; Summary of findings 7 Conscious sedation and analgesia (CSA) + paracervical block (PCB) versus PCB; Summary of findings 8 Conscious sedation and analgesia (CSA) + paracervical block (PCB) versus CSA
We have summarised the effects of interventions as follows.
-
Conscious sedation and analgesia versus placebo.
-
Conscious sedation and analgesia versus other active interventions.
-
Conscious sedation plus paracervical block versus other active interventions.
-
Conscious sedation and analgesia: patient‐controlled versus physician‐controlled.
-
Conscious sedation and analgesia via different agents or dosages.
1. Conscious sedation and analgesia versus placebo
Only one study made this comparison (Ramsewak 1990).
Primary outcome
1.1 Intraoperative pain
Conscious sedation and analgesia was associated with less pain than placebo during needle insertion (mean difference (MD) on 0 to 10 VAS ‐1.70, 94% CI ‐2.38 to ‐1.02; N = 24; Analysis 1.1) and with less pain during follicle aspiration (MD on 0 to 10 VAS ‐1.30, 95% CI ‐1.88 to ‐0.72; N = 24; Analysis 1.2).
Other outcomes were not reported.
2. Conscious sedation and analgesia (CSA) versus other active interventions
Five studies made the following comparisons.
-
CSA plus placebo acupuncture versus CSA plus electro‐acupuncture or acupuncture (Sator‐Katzenschlager 2006).
-
CSA versus CSA plus electro‐acupuncture (Meng 2008; Meng 2009).
-
CSA versus general anaesthesia (Ben‐Shlomo 1999; Matsota 2012).
Primary outcomes
2.1 Intraoperative pain
See Analysis 2.1.
CSA plus placebo acupuncture versus CSA plus acupuncture or electro‐acupuncture
CSA plus placebo acupuncture (i.e. CSA without acupuncture) was associated with a higher pain score during oocyte retrieval than CSA plus acupuncture (MD on 0 to 10 VAS 1.00, 95% CI 0.18 to 1.82; N = 62; very low‐quality evidence) or CSA plus electro‐acupuncture (MD on 0 to 10 VAS 3.00, 95% CI 2.23 to 3.77; N = 62; very low‐quality evidence) (Sator‐Katzenschlager 2006).
This finding was supported by another study in which CSA only was associated with more pain during oocyte retrieval than conscious sedation plus electro‐acupuncture (MD on 1 to 12 numerical rating scale 1.7, 95% CI 1.07 to 2.33; N = 316). In this study, 99/170 (58%) versus 120/146 (82%) women rated pain as mild; 69/170 (41%) versus 23/146 (16%) rated pain as moderate; and 2/170 (1.2%) versus 3/146 (2%) rated pain as severe (P < 0.01) during oocyte retrieval (Meng 2008).
2.2 Postoperative pain
See Analysis 2.2.
CSA plus acupuncture versus CSA plus acupuncture or electro‐acupuncture
Postoperative pain was greater in the CSA plus placebo acupuncture (i.e. CSA without acupuncture) group than in the CSA plus acupuncture group (MD on 0‐10 VAS 0.60, 95% CI ‐0.10 to 1.30; N = 61; very low‐quality evidence) (Figure 4Sator‐Katzenschlager 2006).
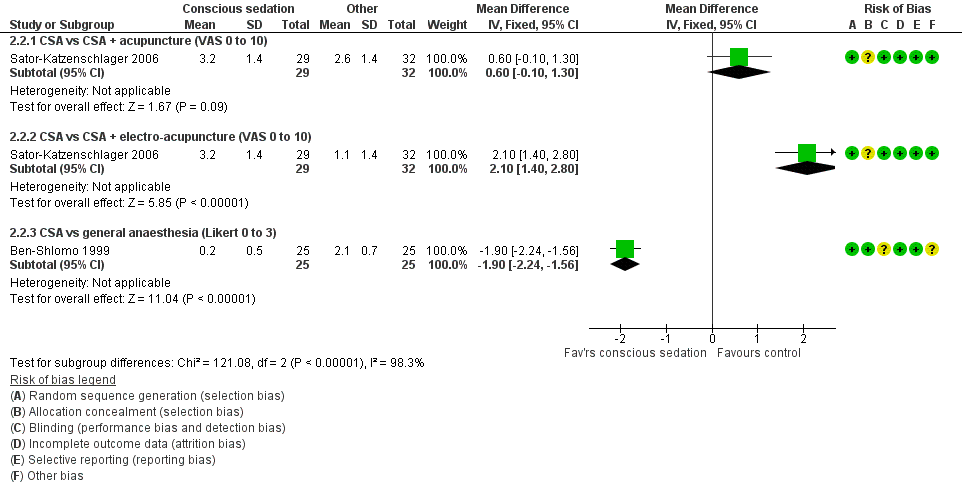
Forest plot of comparison: 2 Conscious sedation + analgesia (CSA) versus other active interventions, outcome: 2.2 Postoperative pain.
CSA plus placebo acupuncture was associated with a higher pain score after oocyte retrieval than conscious sedation plus electro‐acupuncture (MD on 0‐10 VAS 2.10, 95% CI 1.40 to 2.80; N = 61; very low‐quality evidence) (Sator‐Katzenschlager 2006).
This finding was supported by two other studies, which reported binary data, and in which conscious sedation only was associated with more pain at one hour postoperatively when compared with conscious sedation plus electro‐acupuncture (100/170 (59%) vs 47/146 (32%) reported pain), as well as at two to five hours postoperatively (70/170 (42%) vs 38/146 (26%) reported pain; P < 0.01; N = 316) (Meng 2008). Similarly, conscious sedation plus electro‐acupuncture was reported to be associated with lower cumulative pain scores than conscious sedation alone (insufficient data details; N = 694) (Meng 2009).
CSA versus general anaesthesia
CSA was associated with less pain (Likert scale 0 to 3) 30 minutes after completion of the procedure when compared with general anaesthesia (MD on 0 to 3 Likert scale ‐1.90, 95% CI ‐2.24 to ‐1.56; N = 50; very low‐quality evidence) (Ben‐Shlomo 1999).
Secondary outcomes
2.3 Live birth rate and ongoing pregnancy rate
These outcomes were not reported.
2.4 Clinical pregnancy rate
See Analysis 2.3.
Data show no clear evidence of a difference in pregnancy rate between CSA plus placebo and CSA plus acupuncture (OR 0.61, 95% CI 0.20 to 1.86; N = 61; P = 0.38; very low‐quality evidence) (Sator‐Katzenschlager 2006).
CSA plus placebo acupuncture was associated with a lower pregnancy rate per woman when compared with CSA plus electro‐acupuncture (OR 0.22, 95% CI 0.07 to 0.66; N = 61; very low‐quality evidence) (Sator‐Katzenschlager 2006).
Two studies reported that when researchers compared CSA with general anaesthetic, they found no evidence of a difference in the clinical pregnancy rate per woman (OR 1.00, 95% CI 0.43 to 2.35; two RCTs; N = 108; I2 = 0%; very low‐quality evidence; Analysis 2.3) (Ben‐Shlomo 1999; Matsota 2012).
2.5 Fertilisation rate
No study reported this outcome. One study reported oocyte fertilisation rate per oocytes retrieved (Matsota 2012).
2.6 Abandoned procedure of oocyte retrieval
This outcome was not reported.
2.7 Side effects of analgesia
See Analysis 2.4.
When investigators compared CSA plus placebo acupuncture versus CSA plus acupuncture, they provided insufficient evidence to show whether there was a difference in the number of women reporting nausea during oocyte retrieval (OR 1.64, 95% CI 0.46 to 5.88; N = 62; very low‐quality evidence). Similarly, when comparing CSA plus placebo acupuncture versus conscious sedation plus electro‐acupuncture, investigators found no clear evidence of differences between groups for this outcome (OR 1.09, 95% CI 0.33 to 3.58; N = 62; very low‐quality evidence). Two of 29 women (7%) in the CSA plus placebo group reported nausea and vomiting versus none in the other two groups one hour post treatment (Sator‐Katzenschlager 2006).
When investigators compared CSA plus placebo acupuncture versus conscious sedation plus electro‐acupuncture, they found no clear evidence of a difference in reported side effects for nausea and vomiting during oocyte retrieval (17/146 (12%) vs 28/170 (16%) and 3/146 (2%) vs 3/170 (1.8%), respectively; N = 80) nor at one hour postoperatively (13/146 (9%) vs 19/170 (11%) and 4/146 (2.7%) vs 2/170 (1.2%), respectively) nor at two to five hours postoperatively (15/146 (10%) vs 26/170 (15%) and 11/146 (7.5%) vs 15/170 (9%), respectively) (Meng 2008).
When comparing CSA with general anaesthetic, researchers found insufficient evidence to show whether there was a difference in postoperative vomiting (OR 0.46, 95% CI 0.08 to 2.75; N = 50) (Ben‐Shlomo 1999). In another study, researchers found no evidence of a difference in the number of women experiencing fewer than two episodes of vomiting (0/29 (0%) versus 2/29 (6.9%), and women experiencing more than two episodes of vomiting (0/29 (0%) versus 0/29 (0%), P = 0.15; respectively) (Matsota 2012).
2.8 Postoperative complications
See Analysis 2.6 and Analysis 2.7.
When comparing CSA versus general anaesthetic, investigators found no clear evidence of a difference in the rate of airway obstruction (OR 0.14, 95% CI 0.02 to 1.22; N = 58; very low‐quality evidence), but fewer women in the conscious sedation group needed mask ventilation (OR 0.05, 95% CI 0.01 to 0.20; N = 58; very low‐quality evidence) (Matsota 2012).
2.9 Patient satisfaction
When comparing CSA versus general anaesthesia, researchers found that women in both CSA and general anaesthesia groups were satisfied with the modality of pain relief and provided no evidence of a difference between groups, at 24/25 (96%) versus 25/25 (100%) (Ben‐Shlomo 1999). In another study, in which researchers did not assess pain as an outcome, women in both CSA and general anaesthesia groups were satisfied with treatment and were willing to repeat the procedure using the same anaesthesia protocols (27/29 (93%) vs 29/29 (100%)) (Matsota 2012). Combined data from these two studies show an OR of 0.66 (95% CI 0.11 to 4.04; two RCTs; N = 108; I2 = 34%; very low‐quality evidence; Analysis 2.5) (Ben‐Shlomo 1999; Matsota 2012).
3. Conscious sedation plus paracervical block (PCB) versus other active interventions
Eight studies compared these interventions as follows.
-
CSA plus PCB versus general anaesthesia (Guasch 2005).
-
CSA plus PCB versus spinal anaesthesia (Guasch 2005).
-
CSA plus PCB versus placebo plus PCB (Ng 2001).
-
CSA plus PCB versus CSA alone (Gunaydin 2007; Ozturk 2006).
-
CSA plus PCB versus electro‐acupuncture plus PCB (Gejervall 2005; Humaidan 2004; Stener‐Victorin 1999; Stener‐Victorin 2003).
Primary outcomes
3.1 Intraoperative pain
See Analysis 3.1 and Figure 5.

Forest plot of comparison: 3 Conscious sedation + paracervical block versus other interventions, outcome: 3.1 Intraoperative pain (VAS).
Four trials reported data suitable for analysis (Gejervall 2005; Humaidan 2004; Stener‐Victorin 1999; Stener‐Victorin 2003), showing that CSA plus PCB was associated with less intraoperative pain during oocyte retrieval when compared with electro‐acupuncture plus PCB MD on a VAS 0 to 10 scale of ‐0.66 (95% CI ‐0.93 to ‐0.39; four RCTs; N = 781; I2 = 76%; low‐quality evidence). Heterogeneity was high, but the direction of effect was consistent.
Three trials reported data unsuitable for analysis (Gunaydin 2007; Ng 2001; Ozturk 2006).
Investigators in Ng 2001 found that CSA plus PCB was associated with less pain when compared with placebo plus PCB (median on 0 to 10 VAS scale 1.2 vs 3.0 during vaginal punctures, and 1.65 vs 4.30 for corresponding abdominal pain, respectively).
When comparing CSA plus PCB versus CSA only, researchers measured pain at five‐minute intervals during oocyte retrieval and found that CSA plus PCB was associated with less pain (mean VAS) when compared with CSA only (data presented graphically; N = 40) (Gunaydin 2007). Trialists considered a pain score higher than 3 on a simple numerical rating scale (SNRS) as significant. In a second study of the same comparison, CSA plus PCB was associated with less pain than CSA only at the first ovarian puncture (SNRS > 3: 0/50 (0%) vs 6/50 (12%); P < 0.05; N = 100) but SNRS scores at the second ovarian puncture were similar in the two groups (SNRS > 3: 3/50 (6%) vs 3/50 (6%); N = 100) (Ozturk 2006).
3.2 Postoperative pain
See Analysis 3.2.
CSA plus PCB was associated with a higher pain score at four hours postoperatively than was obtained with general anaesthesia (MD on 0 to 10 VAS scale of 0.49, 95% CI ‐0.13 to 1.11; N = 50; very low‐quality evidence). CSA plus PCB was associated with a higher pain score when compared with spinal anaesthesia (MD on 0 to 10 VAS scale 1.02, 95% CI 0.48 to 1.56; N = 36; very low‐quality evidence) (Guasch 2005).
Trials yielding data unsuitable for analysis have reported that when CSA plus PCB was compared with electro‐acupuncture plus PCB, data show no difference in pain between the two groups at 30 minutes (Humaidan 2004) nor at 60 minutes (Gejervall 2005) after oocyte retrieval. At two hours after retrieval, one trial found less pain in the electro‐acupuncture plus PCB group than in the CSA plus PCB group (median VAS 1.1, 95% CI 0 to 7 vs 1.6, 95% CI 0 to 9; P < 0.01; N = 274) (Stener‐Victorin 2003), but the other trial reported no meaningful differences between groups (mean VAS 2.29 (SD 2.34) vs 2.18 (SD 2.14); N = 149) (Stener‐Victorin 1999).
Secondary outcomes
3.3 Live birth rate and ongoing pregnancy rate
See Analysis 3.3.
CSA plus PCB was associated with a higher live birth rate per woman than was electro‐acupuncture plus PCB (OR 2.35, 95% CI 1.09 to 5.05; N = 149) (Stener‐Victorin 1999). Researchers provided no clear evidence of a difference between the two groups in ongoing pregnancy rates per woman (OR 0.86, 95% CI 0.50 to 1.47; N = 274) (Stener‐Victorin 2003).
3.4 Clinical pregnancy rate
See Analysis 3.4.
Evidence is insufficient to show whether there was a difference in pregnancy rates when researchers compared CSA versus general anaesthesia (OR 0.70, 95% CI 0.22 to 2.26; N = 51; very low‐quality evidence) or versus spinal anaesthesia (OR 0.93, 95% CI 0.24 to 3.65; N = 38; very low‐quality evidence) (Guasch 2005).
When CSA with PCB was compared with placebo plus PCB, evidence was insufficient to show whether there was a difference between the two groups in clinical pregnancy rate (OR 0.93, 95% CI 0.44 to 1.96; N = 150; Analysis 3.4) (Ng 2001).
Data show no evidence of a difference in pregnancy rates between electro‐acupuncture plus PCB and CSA plus PCB (OR 0.96, 95% CI 0.72 to 1.29; four RCTs; N = 783; I2 = 9%) and no significant heterogeneity (P = 0.78; Analysis 3.4) (Gejervall 2005; Humaidan 2004; Stener‐Victorin 1999; Stener‐Victorin 2003).
CSA plus PCB was associated with a lower pregnancy rate per woman when compared with CSA alone (OR 0.62, 95% CI 0.28 to 1.36; N = 100) (Ozturk 2006).
3.5 Fertilisation rate
Comparison of CSA with PCB versus placebo plus PCB yielded no evidence of a difference between the two groups in fertilisation rates (OR 0.83, 95% CI 0.42 to 1.66; N = 150; Analysis 3.5) (Ng 2001).
Comparison of CSA alone versus CSA with PCB yielded no evidence of a difference between groups in fertilisation rate per woman (35/50 (69.8%) vs 37/50 (73.3%); N = 100) (Ozturk 2006).
3.6 Abandoned procedure of oocyte retrieval
This outcome was not reported.
3.7 Side effects of analgesia
Two trials compared CSA and PCB versus CSA alone (Gunaydin 2007; Ozturk 2006). CSA with PCB was associated with a lower likelihood of nausea and vomiting when compared with CSA only (OR 0.42, 95% CI 0.18 to 0.97; two RCTs; N = 140; I2 = 40%; very low‐quality evidence). Data show no statistically significant heterogeneity (P = 0.26; Analysis 3.6).
Two trials reported data unsuitable for analysis (Guasch 2005; Ng 2001).
Trials comparing CSA plus PCB versus electro‐acupuncture plus PCB have provided no evidence of a difference in reports of nausea between the two groups at recovery (mean VAS 6.5 (13.0) vs 4.6 (8.8); N = 158) (Gejervall 2005) or at two hours after oocyte retrieval (mean VAS 4.1 (SD 8.0) vs 3.0 (SD 7.2); N = 149) (Stener‐Victorin 1999). Another study reported less nausea in the electro‐acupuncture and PCB group (2/136 (1.5%) vs 13/138 (9.4%) (VAS < 75; P < 0.01; N = 274) (Stener‐Victorin 2003).
3.8 Postoperative complications
This outcome was not reported.
3.9 Patient satisfaction
Comparisons of CSA plus PCB versus general or spinal anaesthesia show that all women reported a high degree of satisfaction (90% vs 88% vs 90%, respectively) (Guasch 2005).
Comparisons of CSA with PCB versus placebo plus PCB yielded no evidence of a difference in satisfaction rates, at 88% versus 80% who were very satisfied or satisfied (OR 1.63, 95% CI 0.68 to 3.89; N = 150; Analysis 3.7) (Ng 2001).
Comparisons of CSA with PCB versus CSA alone yielded no evidence of a difference in satisfaction rates between groups in either trial (47/50 (94%) vs 48/50 (96%) and 20/20 (100%) vs 20/20 (100%) rated satisfaction as moderate and good, respectively) (Gunaydin 2007; Ozturk 2006).
Data show that when CSA plus PCB was compared with electro‐acupuncture plus PCB, electro‐acupuncture plus PCB was associated with a higher satisfaction score in relation to oocyte aspiration than CSA plus PCB (VAS 15.3 (SD 16.3) vs 9.8 (SD 12.6); P = 0.039; N = 158) (Gejervall 2005).
4. Patient‐controlled conscious sedation and analgesia (CSA) versus physician‐controlled CSA
Five studies compared these interventions (Bhattacharya 1997; Lier 2014; Lok 2002; Thompson 2000; Zelcer 1992). One of these studies reported that patient‐controlled CSA was administered with the use of inhalational isodesox (Thompson 2000).
Primary outcomes
4.1 Intraoperative pain
Two trials found that patient‐controlled CSA was associated with higher pain scores than were reported with physician‐controlled CSA (mean VAS 0 to 10 scale 5.3 vs 3.5; N = 106; and 4.68 vs 3.41; N = 112, respectively) (Lok 2002; Thompson 2000). Trialists in the other two studies found no evidence of a difference between groups (mean VAS 0 to 10 scale 3.85 vs 4.63; N = 81; and 2.9 vs 2.5; N = 80, respectively) (Bhattacharya 1997; Zelcer 1992). Combined data on intraoperative pain scores from these four trials show a mean difference in VAS of 0.60 (95% CI 0.16 to 1.03; four RCTs; N = 379; I2 = 83%; Analysis 4.1) (Figure 6) and significant heterogeneity (P = 0.006) favouring physician‐controlled CSA. Exclusion of the single trial in which patient‐controlled CSA was administered with the use of inhalational isodesox yielded a mean VAS score of 0.47 (95% CI ‐0.01 to 0.95; three RCTs; N = 271; I2 = 87%; Analysis 4.2) and significant statistical heterogeneity (P = 0.004) (Thompson 2000).

Forest plot of comparison: 4 Patient‐controlled versus physician‐controlled sedation + analgesia (CSA), outcome: 4.1 Intraoperative pain score (VAS 0 to 10).
In a study without data suitable for analysis, the numeric rating scale (NRS) pain score in the patient‐controlled CSA group was lower than in the physician‐administered CSA group but the difference did not reach statistical significance (median NRS 4 (3 to 7) vs 6 (4 to 8); P = 0.13; one RCT; N = 76) (Lier 2014).
4.2 Postoperative pain
Patient‐controlled CSA was associated with higher pain scores than physician‐controlled CSA two hours after oocyte retrieval (MD on a 0 to 10 VAS scale 1.20, 95% CI 0.26 to 2.14; N = 106; Analysis 4.3) (Lok 2002).
In the study without data suitable for analysis, the pain score in the patient‐controlled CSA group 30 minutes after oocyte retrieval was higher than in the physician‐controlled CSA group (median NRS 2 (1 to 5) vs 1 (0 to 3); P = 0.016; N = 76), but this occurred at the cost of higher sedation in the physician‐controlled CSA group. Pain and discomfort five days post puncture were similar between the two groups (pain scores in NRS presented graphically) (Lier 2014).
Secondary outcomes
4.3 Ongoing pregnancy rate and clinical pregnancy rate
Data show no clear evidence of a difference in pregnancy rates per woman between patient‐controlled and physician‐administered CSA (OR 0.90, 95% CI 0.51 to 1.60; three RCTs; N = 294; I2 = 0%; P = 0.48; Analysis 4.4) (Lier 2014; Lok 2002; Thompson 2000).
4.4 Fertilisation rate
Comparisons of patient‐controlled CSA versus physician‐administered CSA yielded no evidence of a difference between the two groups in fertilisation rate per woman (OR 1.17, 95% CI 0.54 to 2.50; N = 106; Analysis 4.5) (Lok 2002).
4.5 Abandoned procedure of oocyte retrieval
One study reported that oocyte retrieval was completed in all trial participants (Lier 2014).
4.6 Side effects of analgesia
Comparisons of patient‐controlled CSA versus physician‐administered CSA yielded no evidence of a difference between the two groups in the degree of nausea noted during retrieval (nausea score 5.0 (SD 9.0) vs 9.0 (SD 18.0)) or two hours after oocyte retrieval (nausea score 7.0 (SD 1.0) vs 13.0 (18.0)) (Lok 2002) nor in the occurrence of postoperative nausea (8% vs 8%) (OR 1.00, 95% CI 0.19 to 5.28; N = 80; Analysis 4.6) and vomiting (3% vs 0%) (Zelcer 1992).
Data show no evidence of a difference between the patient‐controlled CSA group and the physician‐controlled CSA group in reports of 'drowsiness or spinning sensations' and 'dry mouth' during the oocyte retrieval procedure (20/36 (56%) vs 15/40 (38%), and 4/36 (11%) vs 14/40 (35%)). At 30 minutes after completion of the procedure, 'drowsiness or spinning sensations' were reported less frequently in the patient‐controlled CSA group than in the physician‐controlled CSA group (4/36 (11.1%) vs 21/40 (52.5%); P < 0.001) (Lier 2014).
4.6 Postoperative complications
Trialists have reported that when patient‐controlled CSA was compared with physician‐administered CSA in 112 women, one individual in the group in which patient‐controlled CSA was administered via inhalational isodesox needed airway support perioperatively (Thompson 2000).
4.7 Patient satisfaction
Data show no evidence of a difference between the two groups in reported satisfaction with the procedure (OR 1.95, 95% CI 0.34 to 11.28; N = 81; Analysis 4.7) (Bhattacharya 1997), nor in patient satisfaction (MD on VAS 0 to 10 scale 0.20, 95% CI ‐0.64 to 1.04; N = 106; Analysis 4.8) (Lok 2002); satisfaction was high in both groups (95% vs 95%) (Thompson 2000).
The patient‐controlled CSA group reported a higher satisfaction score than was reported by the physician‐controlled CSA group (median NRS 9 (8 to 10) vs 7 (4 to 9); P = 0.013) (Lier 2014).
5. Conscious sedation and analgesia (CSA) via different agents or dosages
Five studies compared different drug regimens for CSA.
-
CSA with pethidine versus pethidine plus piroxicam (Ocal 2002).
-
CSA with midazolam plus fentanyl versus CSA with propofol plus fentanyl (Ma 2008).
-
CSA with dexmedetomidine + paracervical block versus CSA with midazolam + paracervical block (Elnabtity 2017).
-
Patient‐controlled CSA with propofol versus patient‐controlled CSA with midazolam (Cook 1993).
-
Target‐controlled infusion of CSA plus propofol and remifentanil, with comparison of different infusion rates (Coskun 2011).
Primary outcomes
5.1 Intraoperative pain
Comparisons of CSA with pethidine versus CSA with pethidine plus piroxicam show that women in the pethidine group were more likely to report no pain and less likely to report intense pain than women given intramuscular pethidine plus oral piroxicam or oral piroxicam only (12% vs 0% vs 0%, and 0% vs 4% vs 31%, respectively; P = 0.035; N = 58) (Ocal 2002).
Comparisons of CSA with midazolam plus fentanyl versus CSA with propofol plus fentanyl yielded no evidence of a difference between groups in pain reported during oocyte retrieval (37/40 (93%) vs 36/40 (90%) reported no pain, 2/40 (5%) vs 2/40 (5%) reported mild pain, and 1/40 (2.5%) vs 2/40 (5%) reported severe pain; N = 316) (Ma 2008).
One study measured mean intraoperative pain at five‐minute intervals. CSA with dexmedetomidine plus PCB was associated with significantly less intraoperative pain when compared with CS with midazolam plus PCB at five minutes (MD on 0 to 10 VAS ‐0.74, 95% CI ‐1.48 to 0.00; N = 52; Analysis 5.1) and at 10 minutes (MD on 0 to 10 VAS ‐0.90, 95% CI ‐1.64 to ‐0.16; N = 52; Analysis 5.2), respectively. Data show no significant differences in mean pain scores between the two groups at 15, 20, and 25 minutes during oocyte retrieval (Elnabtity 2017).
Target‐controlled infusion (TCI) is a system that maintains a particular target plasma drug concentration via standard pharmacokinetic equations. Comparison of different doses of TCI yielded no evidence of a difference in pain between the three groups (TCI with remifentanil 1.5 ng/mL, 2 ng/mL, and 2.5 ng/mL, respectively) after the first puncture at five minutes (mean pain score on a 10‐point scale 0.7 (SD 0.3) vs 0.29 (SD 0.17) vs 0.35 (SD 0.19)) or at 10 minutes (1 (SD 1) vs 0.3 (SD 0.36) vs 0.28 (SD 0.28), respectively; N = 69) or at 15 and 20 minutes (mean pain score 0.57 (SD 0.57) vs 0 (SD 0) vs 0.11 (SD 0.11) and 2 (SD 0) vs 0 (SD 0) vs 0 (SD 0), respectively; N = 69). Data show no evidence of differences in pain between the three groups at completion of the procedure (mean pain score 0.13 (SD 0.1) vs 0.09 (SD 0.09) vs 0 (SD 0), respectively; N = 69) (Coskun 2011).
5.2 Postoperative pain
CSA with dexmedetomidine plus PCB was associated with less pain than CSA with midazolam plus PCB at 20 minutes postoperatively (MD on 0 to 10 VAS 0.42, 95% CI ‐0.04 to 0.88; N = 52; Analysis 5.3). Data show no significant difference in mean pain scores between the two groups at 40 and 60 minutes postoperatively (Elnabtity 2017).
Secondary outcomes
5.3 Live birth rate and ongoing pregnancy rate
This outcome was not reported.
5.4 Clinical pregnancy rate
When researchers compared different doses of TCI (remifentanil 1.5 ng/mL, 2 ng/mL, and 2.5 ng/mL respectively), they found no evidence of a difference in pain between the three groups and no evidence of a difference in pregnancy rate between the three groups (10/23 (43%) vs 10/23 (43%) vs 12/23 (52%), respectively; N = 69) (Coskun 2011).
Pregnancy rates per embryo transfer were similar with CSA with dexmedetomidine plus PCB and CSA with midazolam plus PCB (10/26 (38.4%) vs 10/26 (38.4%)) (Elnabtity 2017).
5.5 Fertilisation rate
This outcome was not reported.
5.6 Abandoned procedure of oocyte retrieval
This outcome was not reported.
5.7 Side effects of analgesia
When investigators compared CSA with midazolam plus fentanyl versus CSA with propofol plus fentanyl, they found that midazolam plus fentanyl was associated with less nausea and vomiting (10/40 (25%) and 4/40 (10%) vs 13/40 (32.5%) and 11/40 (27.5%); P < 0.05, respectively; N = 316) (Ma 2008).
Comparisons of different doses of target‐controlled CSA infusion (remifentanil 1.5 ng/mL, 2 ng/mL, and 2.5 ng/mL respectively) yielded no evidence of differences in reports of postoperative nausea and vomiting between the three groups (0/23 (0%) vs 1/23 (4%) vs 2/23 (9%), respectively; N = 69) (Coskun 2011).
Postoperative side effects (nausea, vomiting, dizziness, restlessness, and headache) were similar between CSA with dexmedetomidine plus PCB and CSA with midazolam plus PCB groups (Elnabtity 2017).
5.8 Postoperative complications
Trialists comparing patient‐controlled CSA with propofol versus patient‐controlled CSA with midazolam found that one participant in the midazolam group became transiently unresponsive and two women in the propofol group reported syncope (Cook 1993).
Researchers comparing different doses of target‐controlled CSA infusion (remifentanil 1.5 ng/mL, 2 ng/mL, and 2.5 ng/mL respectively) reported that five women needed a jaw thrust followed by brief periods of assisted masked ventilation (Coskun 2011).
5.9 Patient satisfaction
Comparison of patient‐controlled CSA with propofol versus patient‐controlled CSA with midazolam revealed that both groups reported that they would like to be given the same drug again for a future procedure (20/22 (91%) in the midazolam group vs 24/25 (96%) in the propofol group) (OR 0.42, 95% CI 0.04 to 4.94; N = 47; Analysis 5.4) (Cook 1993).
Patient satisfaction scores were significantly higher in the group given CSA with dexmedetomidine plus PCB than in the group given CSA with midazolam plus PCB (OR 3.07, 95% CI 0.98 to 9.59; N = 52; Analysis 5.4) (Elnabtity 2017).
Comparisons of different doses of target‐controlled CSA infusion (remifentanil 1.5 ng/mL, 2 ng/mL, and 2.5 ng/mL respectively) revealed that 66 women (95%) who were free from postoperative nausea and vomiting were satisfied with their care (Coskun 2011).
Discussion
Summary of main results
This review included 24 trials examining five broad categories of pain relief methods of conscious sedation and analgesia that involved 3160 women undergoing oocyte retrieval. Women’s experience of pain showed conflicting results. No one particular modality of conscious sedation and analgesia was better than any other in providing effective pain relief. However, use of more than one method simultaneously, as when combined with acupuncture or paracervical block, resulted in better pain relief. Patient‐controlled sedation and analgesia was associated with greater intraoperative pain than was physician‐administered sedation and analgesia. Neither of these methods appeared to affect pregnancy rates. However, confidence intervals were wide in most comparisons; therefore these results should be interpreted with caution. Fifteen studies reported high levels of satisfaction in both intervention and comparison groups.
The procedure of oocyte retrieval is painful, as has been demonstrated by higher pain scores among women receiving placebo in Ramsewak 1990 and lower pain scores associated with the intervention. Regardless of the nature of the drug or the dose used, opiates such as fentanyl were effective in reducing the perception of pain. Addition to the opiate of a second drug or intervention, such as paracervical block (PCB), conferred further benefit. The principle of a balanced multi‐modal approach to analgesia has been shown to be effective for treating individuals with pain in other clinical settings such as cancer (World Health Organization (WHO) pain ladder; http://www.who.int/cancer/palliative/painladder/en/) (accessed 10 July 2017).
Paracervical block reduced abdominal pain during oocyte retrieval (Ng 1999); this was also demonstrated in a trial that reported higher pain scores in a placebo plus PCB group (Ng 2001). In trials evaluating PCB, women who were given additional intravenous fentanyl reported lower intraoperative pain scores. Meta‐analysis of the intraoperative pain scores associated with intravenous fentanyl plus PCB versus electro‐acupuncture plus PCB favoured intravenous fentanyl. However, in these two studies, the group given fentanyl also received premedication, whereas the group undergoing electro‐acupuncture received no premedication (Gejervall 2005; Humaidan 2004).
Two studies administered additional analgesia as needed during oocyte retrieval (Cook 1993; Gejervall 2005). One study investigated the dose‐effect relationship of target‐controlled infusion (TCI) of remifentanil and propofol. TCI is a system that maintains a particular target plasma drug concentration via standard pharmacokinetic equations. This study described the need to 'adjust' the dosage of the analgesic agent by increasing or decreasing the dosage (Coskun 2011). This is likely to have caused some women to change treatment groups, accounting for an important limitation in reporting of pain based on the allocated intervention.
Women who received conscious sedation and analgesia combined with electro‐acupuncture reported less pain than women who received conscious sedation and analgesia only (Meng 2008; Meng 2009; Sator‐Katzenschlager 2006). However, the overall result is inconclusive, as pooled data from four trials show that the pain score was higher among women who received auricular electro‐acupuncture and PCB than among women given conscious sedation and analgesia with PCB only (Gejervall 2005; Humaidan 2004; Stener‐Victorin 1999; Stener‐Victorin 2003).
Five trials evaluated the effect of conscious sedation plus acupuncture or electro‐acupuncture on pregnancy rate; the result was inconclusive. Evidence on live birth rate, based on the findings of one small trial, was also inconclusive (Stener‐Victorin 1999).
Several trials (15 out of 24) reported insufficient evidence upon comparison of rates of postoperative nausea and vomiting in the two groups. A trial that compared propofol and midazolam in the context of patient‐controlled sedation and analgesia reported that two women in the propofol group were unable to complete the assessment after completion of the procedure. One was emotionally upset by a difficult oocyte retrieval, and the other fainted upon sitting up. One woman in the midazolam group became transiently unresponsive intraoperatively when given rescue alfentanil by the anaesthetist (Cook 1993). One woman in the PCS via inhalational isodesox group needed perioperative airway support (Thompson 2000). Two women had perforation and one had vaginal bleeding after completion of the procedure (group not reported) (Guasch 2005). In another study, five women needed brief periods of assisted mask ventilation (Coskun 2011). The remaining reviewed trials documented no other serious adverse effects or cancellations of the oocyte retrieval procedure. It is unclear whether no adverse effects actually occurred, or whether these effects were simply unreported.
Patient satisfaction was high with all modalities of conscious sedation and analgesia that were reviewed. No one particular method or delivery system appeared to be clearly better than the other, although use of one method simultaneously with acupuncture or paracervical block resulted in better pain relief than was attained by use of one modality alone. In choosing conscious sedation and analgesia for oocyte retrieval, a balance may need to be struck between effectiveness, safety, and availability of resources. In this update, two studies measured women’s satisfaction as well as their well‐being (fear, stress, and anxiety), and this provided some indication of the quality of women's experiences (Gejervall 2005; Sator‐Katzenschlager 2006).
It is unclear whether global satisfaction can be regarded as a meaningful outcome in determining the effectiveness of the nature, dose, and delivery system of sedation and analgesia used for oocyte retrieval. It is possible that the overall success of the operative procedure (in terms of oocytes collected) and anxiety about side effects of drugs may override any distress caused by the pain. The effectiveness and adequacy of sedation and analgesia, important as they are, may not be the most important outcomes for women undergoing oocyte retrieval when compared with the satisfaction related to a good (or bad) experience of this painful but short and stressful procedure. When patient‐controlled analgesia was used, patients pressed the demand button only when the pain became intolerable (Chumbley 1998). It has also been reported that some patients were reluctant to eliminate pain completely, even when encouraged to do so (Hawkins 1993). The generally high satisfaction levels may reflect the fact that the overall success of the procedure had the potential to counteract the discomfort of the procedure.
In this review, most of the mean differences in pain on a visual analogue scale (VAS) (0 to 10) between different CSA methods were below 2.0, but a few exceeded 2.0, which we believe could represent a clinically important difference. However, tolerance and the experience of pain varied among individuals, making it difficult to interpret the findings of this outcome. General anaesthesia would eliminate pain altogether but is likely to have cost implications. For women who wish to avoid pharmacological analgesia and the side effects of opiates, general anaesthesia, or any agent, electro‐acupuncture may be an effective alternative, depending on the resources available. The ideal regimen of conscious sedation and analgesia would reduce pain to a tolerable level in all patients without risk of adverse respiratory or cardiovascular events. This review demonstrates the variety of approaches available to achieve this and underlines the difficulty of identifying the most superior method(s).
Overall completeness and applicability of evidence
We identified five main interventions comprising 14 dissimilar comparisons, with little consistency in the choice of outcomes. Intraoperative pain was reported in 22 studies, and 11 studies reported the outcome of only postoperative pain. Even when similar drugs were used, routes of administration and doses varied widely. Use of complex interventions in many trials impaired our ability to assess the effects of individual pain relief measures. When pain was the chosen outcome, data show marked differences in the timing of pain assessment and the measuring instruments used, which included the visual analogue scale (VAS), the Likert scale, and other numerical and non‐numerical rating scales. Although it is clear that intraoperative pain was measured during oocyte retrieval, the definition of postoperative pain ranged from pain immediately after oocyte retrieval (end of procedure) to time periods (minutes or hours) following oocyte retrieval. This ambiguity is likely to influence the applicability of the evidence on pain relief. Heterogeneity in the wide range of interventions, dosing regimens, and outcome measures limited our ability to aggregate data meaningfully and to generate conclusions. The subjective nature of pain and satisfaction and the different measures used to assess them limit our ability to interpret and aggregate these outcomes satisfactorily.
In many of the studies reviewed, it is not clear whether pain was measured retrospectively. It is also impossible to ascertain whether a low pain score was due to the increased efficacy of intravenous fentanyl, or whether the premedication altered pain perception or interfered with a person's ability to report the experience of pain. Co‐interventions such as premedication might distort the memory of pain. This must be taken into account in interpreting data from trials that measured pain retrospectively and highlights the difficulty of disentangling the individual anxiolytic, sedative, and analgesic effects of a sedative‐analgesic combination. For example, analgesics such as fentanyl and pethidine in high dosages can produce sedation, and intravenous anaesthetics such as propofol (sedative and analgesic) can have sedative effects at subanaesthetic dosages.
Measuring intraoperative pain would not be possible in two of the trials that used general anaesthesia as a comparator (Ben‐Shlomo 1999;Guasch 2005). Unlike the combination of midazolam and ketamine (Ben‐Shlomo 1999), short‐acting fentanyl may lack adequate residual analgesic effect to provide postoperative pain relief. The amnesic effect of midazolam may be an important confounder, as it can potentially obliterate the memory of pain. Pethidine was reported to be a more effective pain relief agent than piroxicam (Ocal 2002), a non‐steroidal anti‐inflammatory drug.
Comparison of the delivery system and the actual agents used in Bhattacharya 1997,Lier 2014,Lok 2002,Thompson 2000, and Zelcer 1992 shows that the validity of the comparison could be affected in trials of patient‐controlled sedation and analgesia (PCS). Although the theoretical advantage of PCS is that it allows women to administer as much pain relief as they need, this advantage may be limited by (1) the way the pump is set up to deliver a metered dose, and (2) a built‐in lockout time for reasons of safety. A physician may anticipate painful episodes and may give a dose larger than a PCS pump would permit. Meta‐analysis of the intraoperative pain score between patient‐controlled and physician‐administered sedation and analgesia shows that less pain was experienced by patients in the physician‐controlled group. However, this finding must be interpreted with caution in the light of different sedative and analgesic agents and dosages used in these trials.
Quality of the evidence
Using GRADE methods, review authors assessed evidence to be generally of low or very low quality, mainly owing to poor reporting and imprecision.
Risk of bias in the included trials varied. Six trials did not report the method of randomisation used. Methods of allocation concealment were unclear in nine studies, which were at unclear risk of bias. Attempts to contact trial authors by email and letter for clarification met with limited success. Seven trials did not carry out intention‐to‐treat analyses. Overall the sample size ranged from 30 to 700 women. To attain 80% power of detecting a difference of 7 mm on the VAS at the 5% significance level, a minimum of 70 women would be needed. Thirteen trials did not report sample size calculation. Although blinding of women was not feasible owing to the nature of the interventions (such as patient‐controlled sedation and analgesia vs physician‐administered sedation and analgesia), five trials reported blinding of participants and six reported blinding of outcome assessors, which is essential in principle to minimise measurement bias. Figure 1 and Figure 2 show the review authors’ judgements about risk of bias among the trials included in this review.
Potential biases in the review process
We did not exclude studies on the grounds of language. However, some bias in the review process may have arisen from inclusion of trials with insufficient information or outcome data and from lack of response of trial authors to our enquiries.
Agreements and disagreements with other studies or reviews
A systematic review of pain relief in oocyte retrieval restricted itself to trials comparing electro‐acupuncture versus other conscious sedation methods (Stener‐Victorin 2005). The findings of that review were similar to our findings in this population.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
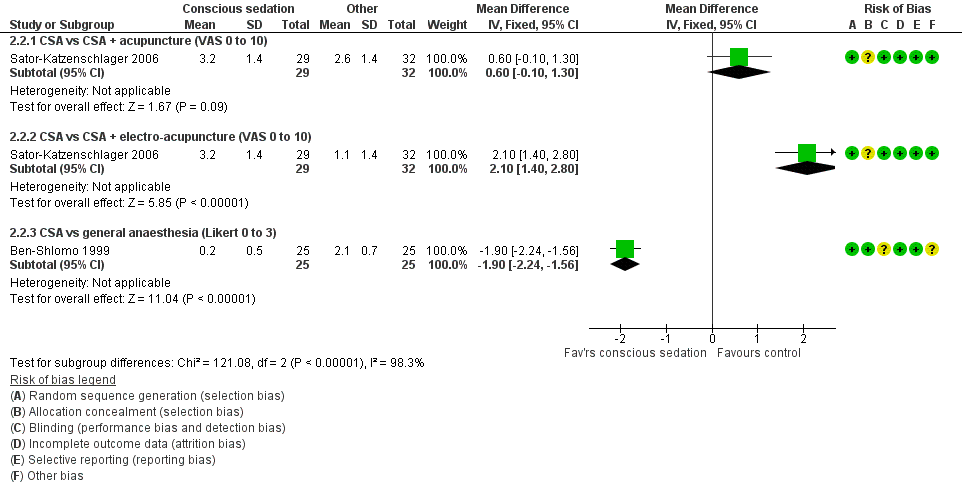
Forest plot of comparison: 2 Conscious sedation + analgesia (CSA) versus other active interventions, outcome: 2.2 Postoperative pain.

Forest plot of comparison: 3 Conscious sedation + paracervical block versus other interventions, outcome: 3.1 Intraoperative pain (VAS).

Forest plot of comparison: 4 Patient‐controlled versus physician‐controlled sedation + analgesia (CSA), outcome: 4.1 Intraoperative pain score (VAS 0 to 10).

Comparison 1 Conscious sedation + analgesia (CSA) versus placebo, Outcome 1 Pain during needle insertion (VAS 0 to 10).

Comparison 1 Conscious sedation + analgesia (CSA) versus placebo, Outcome 2 Pain during follicle aspiration (VAS 0 to 10).

Comparison 2 Conscious sedation + analgesia (CSA) versus other active interventions, Outcome 1 Intraoperative pain.

Comparison 2 Conscious sedation + analgesia (CSA) versus other active interventions, Outcome 2 Postoperative pain.

Comparison 2 Conscious sedation + analgesia (CSA) versus other active interventions, Outcome 3 Pregnancy.

Comparison 2 Conscious sedation + analgesia (CSA) versus other active interventions, Outcome 4 Postop vomiting and/or vomiting.

Comparison 2 Conscious sedation + analgesia (CSA) versus other active interventions, Outcome 5 Satisfaction.
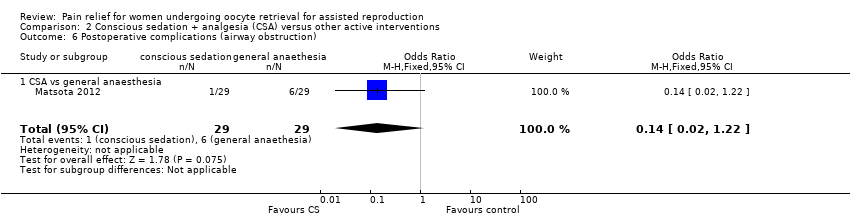
Comparison 2 Conscious sedation + analgesia (CSA) versus other active interventions, Outcome 6 Postoperative complications (airway obstruction).

Comparison 2 Conscious sedation + analgesia (CSA) versus other active interventions, Outcome 7 Postoperative complications (mask ventilation).

Comparison 3 Conscious sedation + analgesia (CSA) + paracervical block versus other interventions, Outcome 1 Intraoperative pain (VAS 0 to 10).

Comparison 3 Conscious sedation + analgesia (CSA) + paracervical block versus other interventions, Outcome 2 Postoperative pain.

Comparison 3 Conscious sedation + analgesia (CSA) + paracervical block versus other interventions, Outcome 3 Live birth or ongoing pregnancy.

Comparison 3 Conscious sedation + analgesia (CSA) + paracervical block versus other interventions, Outcome 4 Pregnancy.

Comparison 3 Conscious sedation + analgesia (CSA) + paracervical block versus other interventions, Outcome 5 Fertilisation rate per woman.

Comparison 3 Conscious sedation + analgesia (CSA) + paracervical block versus other interventions, Outcome 6 Postoperative nausea and/or vomiting.

Comparison 3 Conscious sedation + analgesia (CSA) + paracervical block versus other interventions, Outcome 7 Patient satisfaction by Likert scale: report of 'excellent and satisfactory'.
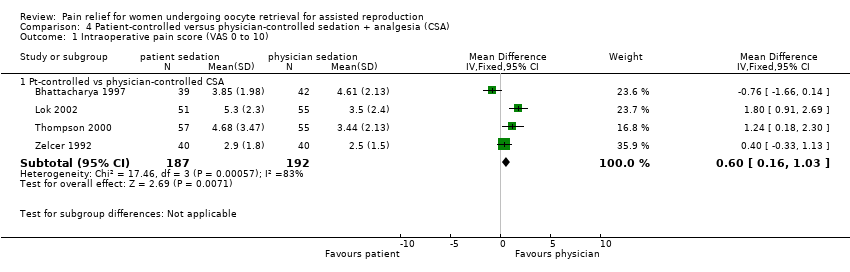
Comparison 4 Patient‐controlled versus physician‐controlled sedation + analgesia (CSA), Outcome 1 Intraoperative pain score (VAS 0 to 10).

Comparison 4 Patient‐controlled versus physician‐controlled sedation + analgesia (CSA), Outcome 2 Intraoperative pain score excluding inhalational sedation/analgesia (VAS 0 to 10).

Comparison 4 Patient‐controlled versus physician‐controlled sedation + analgesia (CSA), Outcome 3 Postoperative pain score (VAS 0 to 10).

Comparison 4 Patient‐controlled versus physician‐controlled sedation + analgesia (CSA), Outcome 4 Pregnancy rate per woman.

Comparison 4 Patient‐controlled versus physician‐controlled sedation + analgesia (CSA), Outcome 5 Fertilisation rate per woman.

Comparison 4 Patient‐controlled versus physician‐controlled sedation + analgesia (CSA), Outcome 6 Postoperative nausea: no. of patients.

Comparison 4 Patient‐controlled versus physician‐controlled sedation + analgesia (CSA), Outcome 7 Patient satisfaction by LIkert scale: report of 'very and moderately satisfied'.

Comparison 4 Patient‐controlled versus physician‐controlled sedation + analgesia (CSA), Outcome 8 Patient satisfaction (VAS 0 to 10).

Comparison 5 Conscious sedation (CSA) + analgesia via different agents or dosages, Outcome 1 Intraoperative pain score at 5 minutes (VAS 0 to 10).

Comparison 5 Conscious sedation (CSA) + analgesia via different agents or dosages, Outcome 2 Intraoperative pain score at 10 minutes (VAS 0 to 10).

Comparison 5 Conscious sedation (CSA) + analgesia via different agents or dosages, Outcome 3 Postoperative pain score at 20 minutes (VAS 0 to 10).

Comparison 5 Conscious sedation (CSA) + analgesia via different agents or dosages, Outcome 4 Patient satisfaction rate.
| Conscious sedation and analgesia (CSA) compared with CSA+acupuncture for women undergoing oocyte retrieval for assisted reproduction | ||||||
| Patient or population: women undergoing oocyte retrieval for assisted reproduction | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No. of participants | Quality of the evidence | Comments | |
| Risk with CSA + acupuncture | Risk with CSA only (95% CI) | |||||
| Intraoperative pain | Mean intraoperative pain score in the comparison group was 4.9 points on a 0 to 10 VAS. | Mean score in the CSA‐only group was 1 point higher | ‐ | 62 | ⊕⊝⊝⊝ | |
| Postoperative pain | Mean postoperative pain score in the comparison group was 3.2 on a 0 to 10 VAS. | Mean score in the CSA‐only group was 0.6 points higher | ‐ | 61 | ⊕⊝⊝⊝ | |
| Pregnancy | 344 per 1000 | 242 per 1000 (95 to 493) | OR 0.61 (0.20 to 1.86) | 61 | ⊕⊝⊝⊝ | |
| Patient satisfaction | No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| Side effects (postoperative vomiting and/or vomiting) | 156 per 1000 | 233 per 1000 | OR 1.64 | 62 | ⊕⊝⊝⊝ | |
| Postoperative complications | No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| *The risk in the intervention group (and its 95% confidence interval) is based on the risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence. | ||||||
| aDowngraded one level for serious risk of bias: unclear risk of bias in one or two domains. bDowngraded two levels for very serious imprecision: very small sample size and low event rate and/or wide confidence intervals compatible with benefit in either group or no effect. | ||||||
| Conscious sedation and analgesia (CSA) compared with CSA + electro‐acupuncture for women undergoing oocyte retrieval for assisted reproduction | ||||||
| Patient or population: women undergoing oocyte retrieval for assisted reproduction | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No. of participants | Quality of the evidence | Comments | |
| Risk with CSA + electro‐acupuncture | Risk with CSA only (95% CI) | |||||
| Intraoperative pain | Mean intraoperative pain score in the comparison group was 2.9 points on a 0 to 10 VAS. | Mean score in the CSA‐only group was 3 points higher | ‐ | 62 | ⊕⊝⊝⊝ | |
| Postoperative pain | Mean postoperative pain score in the comparison group was 1.1 on a 0 to 10 VAS. | Mean score in the CSA‐only group was 2.1 points higher | ‐ | 61 | ⊕⊝⊝⊝ | |
| Pregnancy | 594 per 1000 | 243 per 1000 (95 to 491) | OR 0.22 (0.07 to 0.66) | 61 | ⊕⊝⊝⊝ | |
| Patient satisfaction | No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| Side effects (postoperative vomiting and/or vomiting) | 218 per 1000 | 233 per 1000 | OR 1.09 | 62 | ⊕⊝⊝⊝ | |
| Postoperative complications | Airway obstruction: No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| Need for mask ventilation: No studies reported this outcome. | Not estimable | ‐ | ‐ | |||
| *The risk in the intervention group (and its 95% confidence interval) is based on the risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence. | ||||||
| aDowngraded one level for serious risk of bias: unclear risk of bias in one or two domains. bDowngraded two levels for very serious imprecision: very small sample size and event rate. | ||||||
| Conscious sedation and analgesia (CSA) compared to general analgesia for women undergoing oocyte retrieval for assisted reproduction | ||||||
| Patient or population: women undergoing oocyte retrieval for assisted reproduction | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No. of participants | Quality of the evidence | Comments | |
| Risk with GA | Risk with CSA only (95% CI) | |||||
| Intraoperative pain | No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| Postoperative pain | Mean postoperative pain score in the comparison group was 2.1 points on a 0 to 3 Likert scale. | Mean score in the CSA‐only group was 1.9 points lower | ‐ | 50 | ⊕⊝⊝⊝ | |
| Pregnancy | 278 per 1000 | 278 per 1000 (142 to 475) | OR 1.00 (0.43 to 2.35) | 108 | ⊕⊝⊝⊝ | |
| Patient satisfaction (report of 'satisfactory') | 981 per 1000 | 972 per 1000 (854 to 995) | OR 0.66 (0.11 to 4.04) | 108 | ⊕⊝⊝⊝ | |
| Side effects (postoperative vomiting and/or vomiting) | 160 per 1000 | 81 per 1000 | OR 0.46 | 50 | ⊕⊝⊝⊝ | |
| Postoperative complications | Airway obstruction: 207 per 1000 | 35 per 1000 | OR 0.14 | 58 | ⊕⊝⊝⊝ | |
| Need for mask ventilation: 793 per 1000 | 161 per 1000 | OR 0.05 | 58 | ⊕⊝⊝⊝ | ||
| *The risk in the intervention group (and its 95% confidence interval) is based on the risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence. | ||||||
| aDowngraded two levels for very serious imprecision: very small sample size and event rate and/or wide confidence intervals compatible with benefit in either group or no effect. bDowngraded one level for serious risk of bias: unclear risk of bias in one or two domains. | ||||||
| Conscious sedation and analgesia (CSA) plus PCB compared with electro‐acupuncture plus PCB for women undergoing oocyte retrieval for assisted reproduction | ||||||
| Patient or population: women undergoing oocyte retrieval for assisted reproduction | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No. of participants | Quality of the evidence | Comments | |
| Risk with electro‐acupuncture + PCB | Risk with CSA + PCB (95% CI) | |||||
| Intraoperative pain | Mean intraoperative pain score in the comparison group was 2.6 to 4.85 points on a 0 to 10 VAS. | Mean score in the CSA‐only group was 0.66 points lower | ‐ | 781 | ⊕⊕⊝⊝ | |
| Postoperative pain | No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| Pregnancy | 367 per 1000 | 358 per 1000 (295 to 428) | OR 0.96 (0.72 to 1.29) | 783 | ⊕⊕⊝⊝ | |
| Patient satisfaction | No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| Side effects (postoperative vomiting and/or vomiting) | No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| Postoperative complications | No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| *The risk in the intervention group (and its 95% confidence interval) is based on the risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence. | ||||||
| aDowngraded one level for serious risk of bias: unclear risk of bias in one or two domains. bDowngraded one level for serious inconsistency (I2 = 76%). cDowngraded one level for serious imprecision: wide confidence intervals compatible with benefit in either group or no effect. | ||||||
| Conscious sedation and analgesia (CSA) plus paracervical block (PCB) compared with general anaesthetic (GA) for women undergoing oocyte retrieval for assisted reproduction | ||||||
| Patient or population: women undergoing oocyte retrieval for assisted reproduction | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No. of participants | Quality of the evidence | Comments | |
| Risk with GA | Risk with CSA + PCB (95% CI) | |||||
| Intraoperative pain | ||||||
| Postoperative pain | Mean postoperative pain score in the comparison group was 0.68 points on a 0 to 10 VAS. | Mean score in the CSA‐only group was 0.49 points higher | ‐ | 50 | ⊕⊝⊝⊝ | |
| Pregnancy | 375 per 1000 | 296 per 1000 (117 to 576) | OR 0.70 (0.22 to 2.26) | 51 | ⊕⊝⊝⊝ | |
| Patient satisfaction | No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| Postoperative complications | No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| *The risk in the intervention group (and its 95% confidence interval) is based on the risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence. | ||||||
| aDowngraded one level for serious risk of bias: unclear risk of bias in one or two domains. bDowngraded two levels for very serious imprecision: small sample size and low event rate, wide confidence intervals compatible with benefit in either group or no effect. | ||||||
| Conscious sedation and analgesia (CSA) plus paracervical block (PCB) compared with spinal anaesthesia for women undergoing oocyte retrieval for assisted reproduction | ||||||
| Patient or population: women undergoing oocyte retrieval for assisted reproduction | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No. of participants | Quality of the evidence | Comments | |
| Risk with spinal anaesthesia | Risk with CSA + PCB (95% CI) | |||||
| Intraoperative pain | No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| Postoperative pain | Mean postoperative pain score in the comparison group was 0.15 on a 0 to 10 VAS, | Mean score in the CSA‐only group was 1.02 points higher | ‐ | 36 | ⊕⊝⊝⊝ | |
| Pregnancy | 375 per 1000 | 358 per 1000 (126 to 687) | OR 0.93 (0.24 to 3.65) | 38 | ⊕⊝⊝⊝ | |
| Patient satisfaction | No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| Side effects (postoperative vomiting and/or vomiting) | No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| Postoperative complications | No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| *The risk in the intervention group (and its 95% confidence interval) is based on the risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence. | ||||||
| aDowngraded one level for serious risk of bias: unclear risk of bias in one or two domains. bDowngraded two levels for very serious imprecision: very small sample size and low event rate, wide confidence intervals compatible with benefit in either group or no effect. | ||||||
| Conscious sedation and analgesia (CSA) plus paracervical block (PCB) compared with PCB only for women undergoing oocyte retrieval for assisted reproduction | ||||||
| Patient or population: women undergoing oocyte retrieval for assisted reproduction | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No. of participants | Quality of the evidence | Comments | |
| Risk with PCB only | Risk with CSA + PCB (95% CI) | |||||
| Intraoperative pain | No studies reported this outcome. | Not estimable | ‐ | ‐ | ‐ | |
| Postoperative pain | No studies reported this outcome. | Not estimable | ‐ | ‐ | ‐ | |
| Pregnancy | 253 per 1000 | 240 per 1000 (130 to 399) | OR 0.93 (0.44 to 1.96) | 150 | ⊕⊕⊝⊝ | |
| Patient satisfaction | 800 per 1000 | 867 per 1000 | OR 1.63 (0.68 to 3.89) | 150 | ⊕⊕⊝⊝ | |
| Side effects (postoperative vomiting and/or vomiting) | No studies reported this outcome | Not estimable | ‐ | ‐ | ||
| Postoperative complications | No studies reported this outcome | Not estimable | ‐ | ‐ | ||
| *The risk in the intervention group (and its 95% confidence interval) is based on the risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence. | ||||||
| aDowngraded two levels for very serious imprecision: low event rates and wide confidence intervals compatible with benefit in either group or no effect. | ||||||
| Conscious sedation and analgesia (CSA) plus paracervical block (PCB) compared with CSA alone | ||||||
| Patient or population: women undergoing oocyte retrieval for assisted reproduction | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No. of participants | Quality of the evidence | Comments | |
| Risk with CSA alone | Risk with CSA + PCB (95% CI) | |||||
| Intraoperative pain | No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| Postoperative pain | No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| Pregnancy | 600 per 1000 | 482 per 1000 (296 to 671) | OR 0.62 (0.28 to 1.36) | 100 | ⊕⊝⊝⊝ | |
| Patient satisfaction | No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| Side effects (postoperative vomiting and/or vomiting) | 300 per 1000 | 153 per 1000 | OR 0.42 | 140 | ⊕⊝⊝⊝ | |
| Postoperative complications | No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| *The risk in the intervention group (and its 95% confidence interval) is based on the risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence. | ||||||
| aDowngraded one level for serious risk of bias: unclear risk of bias in one or two domains. bDowngraded two levels for very serious imprecision: small sample size, very low event rates, and wide confidence intervals compatible with benefit in the CSA + PCB group or with no meaningful effect. | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain during needle insertion (VAS 0 to 10) Show forest plot | 1 | 24 | Mean Difference (IV, Fixed, 95% CI) | ‐1.70 [‐2.38, ‐1.02] |
| 2 Pain during follicle aspiration (VAS 0 to 10) Show forest plot | 1 | 24 | Mean Difference (IV, Fixed, 95% CI) | ‐1.30 [‐1.88, ‐0.72] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Intraoperative pain Show forest plot | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 CSA vs CSA + acupuncture (VAS 0 to 10) | 1 | 62 | Mean Difference (IV, Random, 95% CI) | 1.0 [0.18, 1.82] |
| 1.2 CSA vs CSA + electro‐acupuncture (VAS 0 to 10) | 1 | 62 | Mean Difference (IV, Random, 95% CI) | 3.00 [2.23, 3.77] |
| 1.3 CSA vs CSA + electro‐acupuncture (Pain scale 1 to 12) | 1 | 316 | Mean Difference (IV, Random, 95% CI) | 1.70 [1.07, 2.33] |
| 2 Postoperative pain Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.1 CSA vs CSA + acupuncture (VAS 0 to 10) | 1 | 61 | Mean Difference (IV, Fixed, 95% CI) | 0.60 [‐0.10, 1.30] |
| 2.2 CSA vs CSA + electro‐acupuncture (VAS 0 to 10) | 1 | 61 | Mean Difference (IV, Fixed, 95% CI) | 2.1 [1.40, 2.80] |
| 2.3 CSA vs general anaesthesia (Likert 0 to 3) | 1 | 50 | Mean Difference (IV, Fixed, 95% CI) | ‐1.90 [‐2.24, ‐1.56] |
| 3 Pregnancy Show forest plot | 3 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 CSA vs CSA + acupuncture | 1 | 61 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.61 [0.20, 1.86] |
| 3.2 CSA vs CSA + electro‐acupuncture | 1 | 61 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.22 [0.07, 0.66] |
| 3.3 CSA vs general anaesthesia | 2 | 108 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.43, 2.35] |
| 4 Postop vomiting and/or vomiting Show forest plot | 2 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4.1 CSA vs CSA + acupuncture | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 CSA vs general anaesthesia | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Satisfaction Show forest plot | 2 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5.1 CSA vs general anaesthesia | 2 | 108 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.66 [0.11, 4.04] |
| 6 Postoperative complications (airway obstruction) Show forest plot | 1 | 58 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.14 [0.02, 1.22] |
| 6.1 CSA vs general anaesthesia | 1 | 58 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.14 [0.02, 1.22] |
| 7 Postoperative complications (mask ventilation) Show forest plot | 1 | 58 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.05 [0.01, 0.20] |
| 7.1 CSA vs general anaesthesia | 1 | 58 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.05 [0.01, 0.20] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Intraoperative pain (VAS 0 to 10) Show forest plot | 4 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 CSA + paracervical block versus electro‐acupuncture + paracervical block | 4 | 781 | Mean Difference (IV, Fixed, 95% CI) | ‐0.66 [‐0.93, ‐0.39] |
| 2 Postoperative pain Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.1 CSA + paracervical block vs general anaesthesia | 1 | 50 | Mean Difference (IV, Fixed, 95% CI) | 0.49 [‐0.13, 1.11] |
| 2.2 CSA + paracervical block vs spinal anaesthesia | 1 | 36 | Mean Difference (IV, Fixed, 95% CI) | 1.02 [0.48, 1.56] |
| 3 Live birth or ongoing pregnancy Show forest plot | 2 | 393 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.20 [0.78, 1.86] |
| 3.1 CSA + paracervical block vs electro‐acupuncture + paracervical block | 1 | 149 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.35 [1.09, 5.05] |
| 3.2 CSA + paracervical block vs electro‐acupuncture + paracervical block | 1 | 244 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.86 [0.50, 1.47] |
| 4 Pregnancy Show forest plot | 7 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4.1 CSA + paracervical block vs general anaesthesia | 1 | 51 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.70 [0.22, 2.26] |
| 4.2 CSA + paracervical block vs spinal anaesthesia | 1 | 38 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.93 [0.24, 3.65] |
| 4.3 CSA + paracervical block vs paracervical block only | 1 | 150 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.93 [0.44, 1.96] |
| 4.4 CSA + paracervical block vs electro‐acupuncture + paracervical block | 4 | 783 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.72, 1.29] |
| 4.5 CSA + paracervical block vs CSA alone | 1 | 100 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.62 [0.28, 1.36] |
| 5 Fertilisation rate per woman Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5.1 CSA + paracervical block vs paracervical block only | 1 | 150 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.83 [0.42, 1.66] |
| 6 Postoperative nausea and/or vomiting Show forest plot | 2 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 6.1 CSA + paracervical block vs CS only | 2 | 140 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.42 [0.18, 0.97] |
| 7 Patient satisfaction by Likert scale: report of 'excellent and satisfactory' Show forest plot | 1 | 150 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.63 [0.68, 3.89] |
| 7.1 CSA + paracervical block vs paracervical block only | 1 | 150 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.63 [0.68, 3.89] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Intraoperative pain score (VAS 0 to 10) Show forest plot | 4 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 Pt‐controlled vs physician‐controlled CSA | 4 | 379 | Mean Difference (IV, Fixed, 95% CI) | 0.60 [0.16, 1.03] |
| 2 Intraoperative pain score excluding inhalational sedation/analgesia (VAS 0 to 10) Show forest plot | 3 | 267 | Mean Difference (IV, Fixed, 95% CI) | 0.47 [‐0.01, 0.95] |
| 2.1 Pt‐controlled vs physician‐controlled CSA | 3 | 267 | Mean Difference (IV, Fixed, 95% CI) | 0.47 [‐0.01, 0.95] |
| 3 Postoperative pain score (VAS 0 to 10) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 3.1 Pt‐controlled vs physician‐controlled CSA | 1 | 106 | Mean Difference (IV, Fixed, 95% CI) | 1.2 [0.26, 2.14] |
| 4 Pregnancy rate per woman Show forest plot | 3 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4.1 Pt‐controlled vs physician‐controlled CSA | 3 | 294 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.51, 1.60] |
| 5 Fertilisation rate per woman Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5.1 Pt‐controlled vs physician‐controlled CSA | 1 | 106 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.17 [0.54, 2.50] |
| 6 Postoperative nausea: no. of patients Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 6.1 Pt‐controlled vs physician‐controlled CSA | 1 | 80 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.19, 5.28] |
| 7 Patient satisfaction by LIkert scale: report of 'very and moderately satisfied' Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 7.1 Pt‐controlled vs physician‐controlled CSA | 1 | 81 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.95 [0.34, 11.28] |
| 8 Patient satisfaction (VAS 0 to 10) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 8.1 Pt‐controlled vs physician‐controlled CSA | 1 | 106 | Mean Difference (IV, Fixed, 95% CI) | 0.20 [‐0.64, 1.04] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Intraoperative pain score at 5 minutes (VAS 0 to 10) Show forest plot | 1 | 52 | Mean Difference (IV, Fixed, 95% CI) | ‐0.74 [‐1.48, 0.00] |
| 2 Intraoperative pain score at 10 minutes (VAS 0 to 10) Show forest plot | 1 | 52 | Mean Difference (IV, Fixed, 95% CI) | ‐0.90 [‐1.64, ‐0.16] |
| 3 Postoperative pain score at 20 minutes (VAS 0 to 10) Show forest plot | 1 | 52 | Mean Difference (IV, Fixed, 95% CI) | 0.42 [‐0.04, 0.88] |
| 4 Patient satisfaction rate Show forest plot | 2 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4.1 CSA with propofol vs CSA with midazolam | 1 | 47 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.42 [0.04, 4.94] |
| 4.2 CSA with dexmedetomidine vs CSA with midazolam (very satisfied) | 1 | 52 | Odds Ratio (M‐H, Fixed, 95% CI) | 3.07 [0.98, 9.59] |

