Terapia cognitivo‐conductual para los trastornos de ansiedad en niños y adolescentes
Resumen
Antecedentes
El 16 de noviembre de 2020 se publicó una nueva revisión Cochrane titulada “Terapia cognitivo-conductual para los trastornos de ansiedad en niños y adolescentes”que reemplaza a esta publicación.
Cita: James AC, Reardon T, Soler A, James G, Creswell C. Terapia cognitivo‐conductual para los trastornos de ansiedad en niños y adolescentes. Base de datos Cochrane de Revisiones Sistemáticas (Cochrane Database of Systematic Reviews) (Número 11, 2020). Art. No.: CD013162. DOI: 10.1002/14651858.CD013162.pub2.
Una revisión Cochrane anterior (James 2005) mostró que la terapia cognitivo‐conductual (TCC) fue efectiva para tratar los trastornos de ansiedad infantil; sin embargo, aún quedan preguntas con respecto a (1) la eficacia relativa de la TCC versus los tratamientos activos sin TCC; (2) la eficacia relativa de la TCC versus la medicación y la combinación de TCC y medicación versus placebo; y (3) los efectos a largo plazo de la TCC.
Objetivos
Examinar (1) si la TCC es un tratamiento efectivo para los trastornos de ansiedad en niños y adolescentes en comparación con (a) controles en lista de espera; (b) tratamientos activos sin TCC (es decir, placebo psicológico, biblioterapia y tratamiento habitual (TH)); y (c) medicación y la combinación de medicación y TCC versus placebo; y (2) los efectos a largo plazo de la TCC.
Métodos de búsqueda
Las búsquedas para esta revisión incluyeron el Registro Cochrane Central de Ensayos Controlados (Cochrane Central Register of Controlled Trials) (CENTRAL) y el registro del Grupo Cochrane de Depresión, Ansiedad y Neurosis (Cochrane Depression, Anxiety and Neurosis Group), que se compone de los ensayos controlados aleatorizados pertinentes de la bases de datos bibliográficas-The Cochrane Library (1970 hasta julio 2012), EMBASE, (1970 hasta julio 2012) MEDLINE (1970 hasta julio 2012) y PsycINFO (1970 hasta julio 2012).
Criterios de selección
Se examinaron todos los ensayos controlados aleatorizados (ECA) de la TCC versus lista de espera, condiciones de control activas, TH o medicación. Todos los participantes debían haber cumplido con los criterios del Diagnostic and Statistical Manual (DSM) o la International Classification of Diseases (ICD) de un diagnóstico de ansiedad, con la exclusión de la fobia común, el trastorno obsesivo‐compulsivo, el trastorno por estrés postraumático y el mutismo electivo.
Obtención y análisis de los datos
Tres autores de la revisión evaluaron de forma independiente la calidad metodológica de los ensayos incluidos. Para el resultado dicotómico de la remisión del diagnóstico de ansiedad, se utilizó el odds ratio (OR) con intervalos de confianza (IC) del 95%, basado en el modelo de efectos aleatorios, con un agrupamiento de los datos a través del método de ponderación de la varianza inversa. La significación se estableció en P < 0,05. Los datos continuos sobre los síntomas de ansiedad de cada niño se agruparon mediante la diferencia de medias estandarizada (DME).
Resultados principales
Cuarenta y un estudios con 1806 participantes fueron incluidos en los análisis. Los estudios incluyeron a niños y adolescentes con ansiedad de gravedad leve a moderada en ámbitos universitarios, escolares y de consultorios comunitarios. Para el resultado primario de la remisión de cualquier diagnóstico de ansiedad para la TCC versus controles en lista de espera, el análisis de intención de tratar (ITT) con 26 estudios y 1350 participantes mostró un OR de 7,85 (IC del 95%: 5,31 a 11,60; Z = 10,34; P < 0,0001), aunque con evidencia de heterogeneidad moderada (P = 0,05, I²= 30%). El número necesario a tratar (NNT) fue 3,0 (IC del 95%: 1,75 a 3,03). No se observó ninguna diferencia en el resultado entre los formatos individuales, grupales y familiares/paternos. Los análisis de ITT revelaron que la TCC no fue más efectiva que los tratamientos con controles activos sin TCC (seis estudios, 426 participantes) o que el TH para reducir los diagnósticos de ansiedad (dos estudios, 88 participantes). Los pocos estudios controlados de seguimiento (n = 4) indican que los beneficios del tratamiento en cuanto a la remisión del diagnóstico de ansiedad no son estadísticamente significativos.
Conclusiones de los autores
La terapia cognitivo‐conductual es un tratamiento efectivo para los trastornos de ansiedad en niños y adolescentes; sin embargo, la evidencia que indica que la TCC es más efectiva que los controles activos o el TH o la medicación en el seguimiento es limitada y no concluyente.
PICO
Resumen en términos sencillos
Terapia cognitivo‐conductual para la ansiedad en niños y jóvenes
¿Por qué es importante esta revisión?
Muchos niños y jóvenes sufren de ansiedad. Los niños y los jóvenes con ansiedad son más propensos a tener problemas con las amistades, la vida familiar y la escuela. Los tratamientos para niños y jóvenes con ansiedad pueden ayudar a prevenir el desarrollo de problemas de salud mental o de abuso de drogas y alcohol en la edad adulta. Las terapias de conversación como la terapia cognitivo‐conductual (TCC) pueden ayudar a los niños y a los jóvenes a manejar la ansiedad mediante el uso de nuevas formas de pensar. Muchos padres y niños prefieren probar las terapias de conversación en lugar de la medicación como los antidepresivos.
¿Quién estará interesado en esta revisión?
Padres, niños y jóvenes; personas que trabajan en la educación; profesionales que trabajan en servicios de salud mental para niños y jóvenes; y médicos generales.
¿Qué preguntas pretende contestar esta revisión?
Esta revisión es una actualización de una revisión Cochrane anterior de 2005, que indicó que la TCC es un tratamiento efectivo para los niños y los jóvenes con ansiedad.
En esta actualización, se intentan contestar las siguientes preguntas:
• ¿La TCC es más efectiva que ninguna terapia (lista de espera)?
• ¿La TCC es más efectiva que otras terapias “activas” como los libros de autoayuda dirigidos a los niños y los jóvenes?
• ¿La TCC es más efectiva que la medicación?
• ¿La TCC ayuda a reducir los síntomas de ansiedad en los niños y los jóvenes a más largo plazo?
¿Qué estudios se incluyeron en la revisión?
Se utilizaron bases de datos de búsqueda para encontrar todos los estudios de alta calidad de la TCC para la ansiedad en niños y jóvenes publicados entre 1970 y julio 2012. Para estar incluidos en la revisión, los estudios debían ser ensayos controlados aleatorizados y debían incluir a niños y jóvenes con un diagnóstico claro de ansiedad.
En la revisión se incluyeron 41 estudios con un total de 1806 participantes. Los autores de la revisión calificaron la calidad general de los estudios como “moderada”.
¿Qué nos dice la evidencia de la revisión?
La TCC es significativamente más efectiva que ninguna terapia para reducir los síntomas de ansiedad en los niños y los jóvenes.
No hay evidencia clara que indique que una forma de proporcionar la TCC es más efectiva que otra (p.ej., en grupo, individualmente, con los padres).
La TCC no es más efectiva que otras “terapias activas” como los libros de autoayuda.
El número pequeño de estudios significó que los autores de la revisión no pudieran comparar la TCC con la medicación.
Sólo cuatro estudios consideraron los resultados a más largo plazo después de la TCC. No hubo evidencia clara que mostrara una mejoría mantenida en los síntomas de ansiedad entre los niños y los jóvenes.
¿Qué debe suceder a continuación?
Los autores de la revisión recomiendan que la investigación futura considere más detalladamente qué hace que la TCC funcione mejor para los niños y los jóvenes, cómo puede proporcionarse la TCC de la forma más efectiva en función de los costes, y cómo la TCC puede adaptarse a diferentes grupos etarios.
Authors' conclusions
Summary of findings
| CBT compared to wait‐list for children and adolescents with anxiety disorders | ||||||
| Patient or population: children and adolescents with anxiety disorders | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
|---|---|---|---|---|---|---|
| Assumed risk | Corresponding risk | |||||
| Wait‐list | CBT | |||||
| Remission of anxiety diagnoses (ITT analysis) i.e. no longer meeting criteria for DSM or ICD anxiety diagnosis at the end of the trial. | 161 per 1000 | 600 per 1000 | OR 7.85 | 1350 | ⊕⊕⊕⊝ | |
| Participants lost to follow‐up | 104 per 1000 | 97 per 1000 | OR 0.94 | 1297 | ⊕⊕⊝⊝ | |
| Reduction in anxiety symptoms at the end of the trial | The mean reduction in anxiety symptoms in the intervention groups was | 1394 | ⊕⊕⊝⊝ | SMD ‐0.98 (‐1.21 to ‐0.74) standardised mean difference. [SMD (difference in means/pooled standard deviation) of 0.2 standard deviation units is to be considered a small difference between intervention groups, 0.5 a moderate difference, and 0.8 a large difference (Cohen 1988).] | ||
| Remission of anxiety diagnoses: long‐term follow‐up i.e. no longer meeting criteria for DSM or ICD anxiety diagnosis at the end of the follow‐up study period. | 516 per 1000 | 775 per 1000 | OR 3.22 | 124 | ⊕⊕⊝⊝ | |
| Reduction in anxiety symptoms: long‐term follow‐up, i.e. at the end of the follow‐up study period. | The mean reduction in anxiety symptoms: long‐term follow‐up in the intervention groups was | 186 | ⊕⊕⊝⊝ | SMD ‐1.55 (‐3.20 to 0.10) | ||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence: | ||||||
| 1 Moderate heterogeneity present. | ||||||
| CBT compared to active controls for children and adolescents with anxiety disorders | ||||||
| Patient or population: children and adolescents with anxiety disorders | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
|---|---|---|---|---|---|---|
| Assumed risk | Corresponding risk | |||||
| Active controls | CBT | |||||
| Remission of anxiety diagnoses (ITT) analysis i.e. no longer meeting criteria for DSM or ICD anxiety diagnosis at the end of the trial. | 372 per 1000 | 472 per 1000 | OR 1.51 | 426 | ⊕⊕⊕⊝ | |
| Reduction in anxiety symptoms at the end of the trial | The mean reduction in anxiety symptoms in the intervention groups was | 411 | ⊕⊕⊕⊝ | SMD ‐0.5 (‐1.09 to 0.09) standardised mean difference | ||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence: | ||||||
| 1 Widely differing estimates of the treatment effect. | ||||||
| CBT compared to treatment as usual (TAU) for children and adolescents with anxiety disorders | ||||||
| Patient or population: children and adolescents with anxiety disorders | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
|---|---|---|---|---|---|---|
| Assumed risk | Corresponding risk | |||||
| Treatment as usual (TAU) | CBT | |||||
| Remission of anxiety diagnoses (ITT analysis) i.e. no longer meeting criteria for DSM or ICD anxiety diagnosis at the end of the trial. | 556 per 1000 | 398 per 1000 | OR 0.53 | 88 | ⊕⊕⊕⊝ | |
| Reduction of anxiety symptoms at the end of the trial | The mean reduction in anxiety symptoms in the intervention groups was | 98 | ⊕⊕⊕⊝ | SMD ‐0.19 (‐0.79 to 0.4) standardised mean difference | ||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence: | ||||||
| 1 Small sample size. | ||||||
Background
Description of the condition
Anxiety disorders are amongst the most common psychiatric disorders, occurring in 5% to 19% of all children and adolescents (Costello 2004). In children younger than 12, prevalence varies between 2.6% and 5.2%, and separation anxiety is the most common disorder (Costello 2004; Ford 2003).
One of the diagnostic challenges in this age group involves distinguishing normal, developmentally appropriate worries, fears and shyness from anxiety disorders. Distinguishing features of pathological anxiety include severity, persistence and associated impairment. An understanding of the developmental patterns of various anxieties is also important. School‐age children commonly have worries about injury and natural events, whereas older children and adolescents typically have worries and fears related to school performance, social competence and health issues.
The presentation of anxiety disorders varies with age. Young children can present with undifferentiated worries and fears and multiple somatic complaints ‐ muscle tension, headache or stomachache ‐ and sometimes angry outbursts. The latter may be misdiagnosed as oppositional defiant disorder (ODD), as the child tries to avoid anxiety‐provoking situations. Social anxiety disorder typically presents after puberty. Anxiety disorders with an onset in childhood often persist into adolescence (Last 1996) and early adulthood (Last 1997), and yet they often remain untreated, with many cases of social phobia (SOP) first diagnosed more than 20 years after onset (Schneier 1992).
The International Classification of Diseases (ICD) and Diagnostic and Statistical Manual (DSM) diagnostic systems distinguish various types of anxiety disorders, including generalized anxiety disorder (GAD), panic disorder (PD), social anxiety disorder (SAD) and specific phobias. These anxiety disorders are often associated with significant impairment in personal, social and academic functioning (Pine 2009). Comorbidities are common and include depression (Kovacs 1989), substance abuse (Kushner 1990) and subsequent adolescent anxiety disorders, social phobia (SOP), attention‐deficit/hyperactivity disorder (ADHD), conduct disorder (Bittner 2007), suicidal behaviours and suicide (Hill 2011), Social anxiety disorder (SAD) which peaks in adolescence, is associated with more malignant depression later on (Beesdo 2007). It is clear that anxiety disorders in this age group present serious health issues; therefore effective and readily accessible treatments are needed.
Description of the intervention
Current treatments for anxiety disorders in this age group include behavioural therapy, particularly for simple phobias, cognitive behavioural therapy (CBT) and/or medication. No specific guidelines on the indications for psychological treatment versus medication have been put forth, although given the prevalence of these disorders, the age of onset and public views on the acceptability of psychological treatments, these are often preferred as first‐line therapy. CBT is a collaborative psychological treatment that can be delivered in various formats-individual, child or adolescent, group, parents or family. CBT for anxiety disorders in children and adolescents usually takes nine to twenty sessions.
One of the first manualised CBT programmes was Coping Cat (Kendall 1994), which consisted of education, modification of negative cognitions, exposure, social competence training, coping behaviour and self‐reinforcement sessions. Others have followed, including the Cool Kids programme (http://education.qld.gov.au/studentservices/protection/sel/cool‐kids.html), the Coping Koala programme (Barrett 1996), Skills for Academic and Social Success (SASS) (Masia‐Warner 2007), ACTION (Waters 2009), Intervention With Adolescents With Social Phobia (IAFS) (Sánchez‐García 2009), the TAPS (Masia‐Warner 2011) and Building Confidence programme (Galla 2012). Some programmes have been specifically adapted for children with autism spectrum disorders (ASDs), including the Multimodal Anxiety and Social Skills Intervention (MASSI) programme (White 2012), TAFF (Schneider 2011) and Facing Your Fears (FYF) (Reaven 2012).
How the intervention might work
CBT for anxiety disorders in children and adolescents involves helping the child to (1) recognise anxious feelings and bodily or somatic reactions to anxiety, (2) clarify thoughts or cognitions in anxiety‐provoking situations (e.g. unrealistic or negative attributions and expectations), (3) develop coping skills (e.g. modifying anxious self‐talk into coping self‐talk) and (4) evaluate outcomes. Behavioural training strategies include modelling, reality exposure (in vivo exposure), role playing and relaxation training. Behavioural treatment is based on the premise that fear and anxiety are learnt responses (classically conditioned) that can be "unlearnt". A key CBT procedure is exposure (Silverman 1996). An element of treatment known as systematic desensitisation involves pairing anxiety stimuli, in vivo or by imagination, in a gradually increasing hierarchy with competing relaxing stimuli such as pleasant images and muscle relaxation.
Cognitive strategies are used, the most common of which are self‐control strategies which rely on self‐observation, self‐modification, self‐evaluation and self‐reward. For instance, according to the STOP acronym (Silverman 1996), children and adolescents learn first to identify when they are feeling anxious or Scared (S), then to identify their anxious Thoughts (T). Next, they learn to modify or restructure their anxious thoughts by generating Other alternative coping thoughts and behaviours (O). Finally, they learn to reward or Praise themselves for confronting their fears (P).
CBT has been adapted to include family and parents. The main aspects of CBT parent/family treatment guidelines involve (1) modifying parents’ beliefs about ways to help their anxious child and assisting parents to respond appropriately to the child’s anxious and avoidant behaviours, and (2) assisting parents to manage their own anxiety.
CBT can be applied only after the child has reached a certain level of cognitive development. Kendall (Kendall 1990b) argued that the ability to measure a thought or belief against the notion of a rational standard and the ability to understand that a thought or belief can cause a person to behave and feel in a certain way were central to its proper use. The question arises: At what age does a child have the cognitive capacities to undertake these cognitive operations? A recent study (Hirshfeld‐Becker 2010) reported positive effects in children younger than age 6; however, it is not clear whether children younger than 6 years of age are able to use de‐centring techniques such as narratives or stories. In line with this, recent work suggests that young children may be more responsive to the behavioural than the cognitive elements of this approach (Essau 2004). Recent work indicates that treatment of anxiety disorders in very young children may be effected by working directly with parents alone (Cartwright‐Hatton 2011).
Why it is important to do this review
Anxiety disorders in children and adolescents represent a considerable source of morbidity and are associated with later adult psychopathology. However, despite high prevalence and substantial morbidity, anxiety disorders in childhood remain under‐recognised and under‐treated (Esbjørn 2010) and as such represent an important public health issue. The evidence base for treatment of anxiety in children and adolescents is growing. Initial trials of CBT (Kendall 1994; Barrett 1996; Kendall 1997) were positive (Kendall 1997), and further randomised controlled trials (RCTs) and indeed reviews followed. What is needed now is synthesis of the growing body of evidence. This is an update of a previous Cochrane review of CBT for anxiety disorders in children and adolescents (James 2005), which found a positive response rate for the remission of anxiety diagnoses for CBT in 56% of cases. The current review was undertaken to provide comprehensive and up‐to‐date evidence on the efficacy of CBT in the treatment of anxiety disorders in children and adolescents, including the use of differing CBT formats-individual, group and family/parent. Further, this review will examine the efficacy of CBT relative to active treatments, such as educational support and treatment as usual (TAU). The question of the comparative efficacy of medication versus CBT and the combination of CBT and medication needs to be addressed. Last, this review will aim to assess whether treatment effects of CBT are maintained at long‐term follow‐up.
It is recognised that children and adolescents with autism spectrum disorders (ASDs) have high rates of anxiety disorders, particularly SOP (Settipani 2012); however, a recent review of CBT for anxiety disorders in ASD (Lang 2010) included only a few studies. Furthermore, it is unclear how anxiety disorders are recognised or, indeed, treated in those with intellectual impairments, indicating a pressing need for work in this particular area. Review of the efficacy of CBT in children and adolescents with ASD will be undertaken.
Recognition of the importance of anxiety disorders in childhood is increasing, as can be seen in several reviews on the treatment of anxiety in children and adolescents, including Cochrane reviews for post‐traumatic stress disorder (PTSD) (Bisson 2007), obsessive‐compulsive disorder (OCD) (O'Kearney 2006) and pharmacological treatments (Ipser 2009). These disorders will not be included in this review.
Objectives
-
To carry out a meta‐analysis of identified studies to determine whether CBT leads to remission of childhood and adolescent anxiety disorders and/or a clinically significant reduction in anxiety symptoms in comparison with passive (waiting list-W/L) controls, active controls or treatment as usual (TAU).
-
To carry out a subgroup analysis of different types of CBT according to format (individual, group and parent/family).
-
To determine the comparative efficacy of CBT alone, and the combination of CBT and medication, versus placebo.
-
To determine whether post‐treatment gains of CBT are maintained at follow‐up.
Methods
Criteria for considering studies for this review
Types of studies
RCTs, including cross‐over trials and cluster‐randomised trials, of manualised and documented modular CBT of at least nine sessions, involving direct contact with the child, were included, as were follow‐up data with comparators (W/L, active controls or TAU).
Types of participants
Participant characteristics
Children and adolescents older than four years and younger than 19 years.
Diagnosis
Participants meeting diagnostic criteria of the DSM (DSM III, III‐R, IV and IV‐TR) (APA 1980; APA 1987; APA 1994; APA 2000) or of ICD9 and ICD10 (WHO 1978, WHO 1992) for anxiety disorder, including one or more disorders of GAD, over‐anxious disorder, SAD, SOP or PD, but excluding PTSD, simple phobias, elective mutism and OCD.
Comorbidity
All comorbidities allowable for anxiety disorders under the rules of DSM and ICD were included, such as ASD, intellectual impairment and physical disorders.
Settings
All settings such as research settings (i.e. university outpatient clinics, inpatient services, community clinics, and schools) were included.
Exclusion criteria
We excluded PTSD and OCDs because they are covered by separate Cochrane reviews (Bisson 2007; O'Kearney 2006). In line with other reviews (Reynolds 2012), simple phobias were excluded because established behavioural treatments necessarily involve cognitive interventions.
Types of interventions
Experimental intervention
Manualised CBT, or modular CBT, alone or in combination with medication was required. A documented, written protocol stating the specific treatment at each stage of at least nine sessions provided by trained therapists under regular supervision was required. The choice of nine sessions is arbitrary; nonetheless, all major published protocols consist of at least this number of sessions.
CBT had to be administered according to standard principles as a psychological model of treatment involving helping the child to (1) recognise anxious feelings and somatic reactions to anxiety, (2) clarify cognitions in anxiety‐provoking situations, (3) develop coping skills that involve modification of these anxiety‐provoking cognitions and (4) respond to behavioural training strategies with exposure in vivo or by imagination, usually in a gradual, hierarchical manner, and relaxation training. No concurrent medications for the treatment of anxiety were to be administered naturalistically.
CBT can be delivered individually, in a group format or with family or parental involvement. The latter spans a range of direct involvement such as (rarely) the whole family and (more usually) the parents for some conjoint or separate sessions. Family/parental CBT may include providing psycho‐education for parents or even teaching parents to be co‐therapists.
The control groups were W/L or TAU. Comparison of the latter group against CBT allows one to demonstrate any added effect or not of CBT over other active treatments, whereas the comparison of CBT against W/L yields a baseline or estimate of CBT versus no treatment.
Comparator interventions
-
Waiting list and no treatment for anxiety during that period.
-
Psychological treatment that did not include CBT elements, or attention only (e.g. support but with no elements of CBT).
-
TAU.
-
Drug placebo.
Types of outcome measures
Primary outcomes
-
Remission ‐ the absence of a diagnosis of an anxiety disorder, as diagnosed by reliable and valid structured interviews for DSM or ICD child and adolescent anxiety disorders, including:
-
-
-
Anxiety Disorder Interview Schedule for Parents (ADIS‐P) (Silverman 1987).
-
Anxiety Disorder Interview Schedule for Children (ADIS‐C) (Silverman 1987).
-
Diagnostic Interview Schedule for Children, Adolescents and Parents (DISCAP) (Holland 1995).
-
-
The diagnostic interviews were required to be carried out independently of the treatment team.
In addition we included non‐specific rating scales such as the Clinical Global Impression scale (CGI‐I) (Guy 1976), a validated seven‐item scale used to assess treatment responders. Treatment response was deemed as a score of 1 (very much improved) or 2 (much improved) on the CGI‐I.
-
Acceptability, as determined by the numbers of participants who were lost to follow‐up.
Secondary outcomes
-
Reduction in anxiety symptoms ‐ to be measured using psychometrically robust measures of anxiety symptoms (Myers 2002) that yield symptom scores on continuous scales, such as:
-
-
-
Revised Children's Manifest Anxiety Scale (RCMAS) (Reynolds 1985).
-
Fear Survey for Children-Revised (FSSC‐R) (Ollendick 1998).
-
Social Phobia and Anxiety Inventory for Children (SPAI‐C) (Beidel 1995).
-
Child Behaviour Checklist (CBCL) (Achenbach 1991).
-
Social Anxiety Scale for Adolescents (SAS‐A) (La Greca 1998).
-
State‐Trait Anxiety Inventory for Children (STAI‐C) (Spielberger 1973).
-
Screen for Child Anxiety Related Emotional Disorders (SCARED) (Birmaher 1999).
-
SCAS (Spence Child Anxiety Scale, Child and Parent Versions) (Spence 1997).
-
-
These scales are self‐report or are completed by a parent or guardian or an independent rater. Where possible, the child’s or adolescent’s report was used. Often multiple measures were reported, and the most validated, best recognised, or most frequently used measures were included in the analysis.
A crucial issue is how well these measures discriminate between clinical and non‐clinical levels of anxiety. A meta‐analysis of 43 articles (Seligman 2004) found a large effect size for the measures RCMAS, STAI‐C and CBCL in discriminating children and adolescents with anxiety disorders versus controls and those with externalising disorders, but not affective disorders. The RCMAS, STAI‐C and CBCL were also moderately sensitive to treatment gains.
Search methods for identification of studies
We identified all studies that might describe RCTs of CBT for anxiety disorders in children and adolescents from the Depression, Anxiety and Neurosis Cochrane Review Group Trials Registers (CCDANCTR) (most recent search, 01/05/2012).
Electronic searches
CCDAN's Specialized Register (CCDANCTR)
The Cochrane Depression, Anxiety and Neurosis Group (CCDAN) maintains two clinical trials registers at its editorial base in Bristol, UK: a references register and a studies‐based register. The CCDANCTR‐References Register contains more than 31,500 reports of trials in depression, anxiety and neurosis. Approximately 65% of these references have been tagged to individual, coded trials. The coded trials are held in the CCDANCTR‐Studies Register, and records are linked between the two registers through the use of unique Study ID tags. Coding of trials is based on the EU‐Psi coding manual. Please contact the CCDAN Trials Search Co‐ordinator for further details. Reports of trials for inclusion in the Group's registers are collated from routine (weekly), generic searches of MEDLINE (1950‐), EMBASE (1974‐) and PsycINFO (1967‐), from quarterly searches of the Cochrane Central Register of Controlled Trials (CENTRAL) and from review‐specific searches of additional databases. Reports of trials are also sourced from international trial registers c/o the World Health Organization's trials portal (ICTRP), as well as from drug companies and from the handsearching of key journals, conference proceedings and other (non‐Cochrane) systematic reviews and meta‐analyses.
Details of CCDAN's generic search strategies can be found on the Group's Website.
-
The CCDANCTR‐Studies register was searched using the following search strategy:
Condition = (anxiety or anxious or “phobic disorder*" or “panic disorder*” or “social phobia”)
AND
Intervention = (behavior* or behaviour* or cognitive*)
AND
Age = (child* or adolescent* or unclear or “not stated”).
-
The CCDANCTR‐References register was searched using a more sensitive set of free‐text terms to identify additional untagged/uncoded reports of RCTs:
(CBT or cognitive* or behavior* or behaviour*) and (anxiety or anxious or *phobi* or panic*) and (child* or adolesc* or juvenil* or school* or pediatri* or paediatri* or teen* or young or youth*).
-
Additional searches:
A complementary search of MEDLINE and MEDLINE In‐Process was conducted in September 2009 when the CCDANCTR was out‐of‐date as the result of a changeover of staff at the editorial base (Appendix 1).
-
The WHO Trials portal (ICTRP) and ClinicalTrials.gov were also searched to identify additional unpublished and/or ongoing studies.
Searching other resources
-
The following journals were handsearched up until 2004:
Cognitive Therapy and Research 1977‐2004
Journal of Child Psychology and Psychiatry 1970‐2004
British Journal of Psychiatry 1970‐2004
Behavioural and Cognitive Psychotherapy 1970‐2004
British Journal of Clinical Psychology 1970‐2004
Psychological Medicine 1970‐2004
Journal of the American Academy of Child and Adolescent Psychiatry 1970‐2004
Journal of Consulting and Clinical Psychology 1970‐2004
Journal of Clinical Child and Adolescent Psychology 1997‐2004
Journal of Abnormal Psychology 1970‐2004
Journal of Abnormal Child Psychology 1970‐2004
Journal of Behaviour Therapy Experimental Psychiatry 1970‐2004
Behaviour Research and Therapy 1970‐2004
Behaviour Therapy 1970‐2004
These journals are now available online; therefore it was not deemed necessary to handsearch for the years 2005 through to 2012.
-
Reference lists
The reference lists of all identified studies were inspected for additional studies.
-
Personal communication
The lead author on all included studies and other experts in the field were approached to request details of any further published or unpublished studies.
-
Book chapters
Textbooks on child and adolescent psychiatry and anxiety disorders were searched for additional relevant studies.
Data collection and analysis
Selection of studies
All citations identified by searching were separately inspected by four reviewers (ACJ, FAC, GJ and AS) to ensure reliability. All articles that possibly met our inclusion criteria were obtained so that the full text could be independently assessed as to whether they met review criteria. Authors were not blinded to the names of authors, institutions, journals of publication and results, when they applied the inclusion criteria. Any disagreement on the eligibility of a study was discussed with the other review authors, and, where necessary, the authors of the studies were contacted for further information.
Data extraction and management
References were organised using Reference Manager. Data extraction forms were developed a priori and included information regarding study methods, participant details, treatment details and adherence to treatment protocol and outcome measures. Data were extracted and assessed by FAC, GJ and ACJ independently. Consensus was reached through discussion. In cases of disagreement, the other review authors were consulted. Any areas of remaining uncertainty were resolved by contacting the author of the study.
Main comparisons
-
CBT compared with waiting list controls.
-
CBT compared with other active treatments.
-
CBT compared with TAU.
-
CBT compared with medication or placebo.
-
CBT and medication combination compared with placebo.
Assessment of risk of bias in included studies
For each included study, three review authors (ACJ, FAC and GJ) independently assessed risk of bias using the seven domains set out below from the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011), with ratings of 'low risk', 'high risk' and 'unclear risk':
-
Sequence generation.
-
Allocation concealment.
-
Blinding of participants and personnel.
-
Blinding of outcome assessors.
-
Incomplete outcome data.
-
Selective outcome reporting.
-
Other bias: CBT non‐manualisation.
Risk of bias was assessed using the Cochrane Risk of Bias tool, a summary of which is displayed in Figure 1 and Figure 2. Selection bias was identified by assessing the adequacy of the randomisation process in terms of the description of adequacy of sequence generation and the concealment of treatment group allocation. Given the nature of psychological interventions, blinding of either participants or personnel delivering the treatments was possible only in those studies involving CBT versus active controls or TAU; therefore performance bias was assessed only in those studies. Detection bias was assessed by identifying whether study personnel carrying out outcome assessments were blinded to the treatment status of participants. Attrition bias was assessed by determining whether studies provided a description of withdrawals and dropouts (Figure 2).

Risk of bias summary: risk of bias item for each included study.

Risk of bias graph: risk of bias item presented as percentages across all included studies.
We did not exclude studies from meta‐analysis on the basis of the 'risk of bias' assessment. We conducted a sensitivity analysis for the primary outcome, excluding trials with 'no' or 'unclear' ratings for allocation concealment if appropriate. We reported on the remainder of the risk of bias assessments for these trials and include discussion of this assessment in the Results and Discussion sections.
Measures of treatment effect
Post‐treatment outcomes were assessed using dichotomous data on remission of anxiety symptoms and continuous data on anxiety symptoms, with the use of standardised measures. These measures were also used to assess the maintenance of treatment effects versus W/L controls at follow‐up. For dichotomous data, the review used odds ratio (OR) and 95% confidence interval (CI), with pooling of data via the inverse variance method of weighting. Continuous data, measured in different ways across studies but conceptually the same (i.e. measuring anxiety), were pooled using the standardised mean difference (SMD). For both dichotomous and continuous data, a random‐effects model was used and significance was set at P < 0.05. Completer and intent‐to‐treat (ITT) analyses were undertaken. However, for symptoms, last observation carried forward (LOCF) analyses were not performed as we did not have access to raw data.
Unit of analysis issues
Cluster‐randomised trials
Cluster‐randomised controlled trials based in schools were included. Cluster‐randomised trials may, in principle, be combined with individually randomised trials in the same meta‐analysis (Higgins 2011). We did not estimate that there would be many cluster‐randomised trials; therefore identified cluster‐randomised trials will be included in the meta‐analyses and sensitivity analyses undertaken to investigate the robustness of any conclusions drawn. To correct the influence of any cluster trials, an average intraclass correlation coefficient of 0.02 was used (Health Services Research Unit 2004).
The effective sample size of a single intervention group in a cluster‐randomised trial is its original sample size divided by the ‘design effect’. The design effect is 1 + (M – 1) ICC, where M is the average cluster size and ICC is the intracluster correlation coefficient (Rao 1992). For dichotomous data, both the number of participants and the number experiencing the event were divided by the same design effect. For continuous data, only the sample size was reduced; means and standard deviations were not altered.
Cross‐over trials
For any cross‐over trials, paired analysis was to be undertaken if data were presented.
Studies with multiple treatment groups
Studies with more than two intervention arms can pose analytical problems in pair‐wise meta‐analysis. Where studies had two or more active treatment arms to be compared against TAU, data were managed in this review as follows:
Continuous data
The control group was divided equally into two and the means and SDs of these groups compared against the means and SDs of the two treatment arms.
Dichotomous data
For trials with two or more active treatment arms and a control group, participants in the control arm group were split equally between the active treatment arm.
Dealing with missing data
Missing statistics
In the first instance, attempts were made to contact the original researchers for any missing data. If only standard errors (SEs) were reported, standard deviations (SDs) were calculated.
Missing participants
ITT analyses were undertaken. For the analysis of dichotomous data, it was assumed that all non‐completers in the CBT group were treatment failures and non‐completers in the control group were treatment successes, thereby yielding the most conservative treatment estimate. LOCF analysis for symptoms was not performed.
Assessment of heterogeneity
Clinical heterogeneity was assessed by comparing differences in the distribution of important participant factors between trials (e.g. age, gender, specific diagnosis, duration and severity of disorder, associated comorbidities). We assessed methodological heterogeneity by comparing trial factors (randomisation, concealment, blinding of outcome assessment, losses to follow‐up). The Chi2 test and the I2 statistic were used to assess heterogeneity. Significance was set at P < 0.1. The Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011) recommends using a range for I2 and a guide to interpretation. For this review, if either moderate heterogeneity (I2 in the range of 30% to 60%) or substantial heterogeneity (I2 in the range of 50% to 90%) was found, subgroup and sensitivity analyses were used, with meta‐regression analyses (STATA 2009).
Assessment of reporting biases
Publication bias was investigated using funnel plots, and any asymmetry found was subjected to statistical investigation using the Egger's test (STATA 2009).
Data synthesis
Dichotomous data
The review used ORs and 95% CIs based on the random‐effects model, with pooling of data via the inverse variance method of weighting. Significance was set at P < 0.05. Where available, data from an interview with the child or adolescent were used; otherwise data from interviews with the parents were used. Where both endpoint and change data were available for the same outcome, the endpoint was presented. The number needed to treat (NNT) with 95% CIs was calculated (STATA 2009). For each comparison, a summary statistic of all those responding to treatment was calculated as a percentage of the total number of participants.
Continuous data
For those completing trials, analysis of continuous data, based on the random‐effects model, was conducted. Continuous data, measured in different ways across studies but conceptually the same (i.e. measuring anxiety), were pooled using the SMD. Where possible, the child's or adolescent's own measures were used; otherwise parental or clinician reports of anxiety were used. Where both endpoint and change data were available for the same outcome, the endpoint was presented. Significance was set at P < 0.05. Pretreatment data were used to assess the influence of severity on outcome using meta‐regression (STATA 2009).
Tables and figures
Data were entered into the Review Manager programme and were presented graphically, so that the area to the left of the line of no effect indicated a favourable outcome for CBT. Tables were used to display characteristics of the studies included. Excluded studies were presented in a table with reasons for exclusion. A figure was used to summarise the risk of bias in the included studies (Figure 1 and Figure 2), and a PRISMA flow chart (Moher 2009; Figure 3) was included.
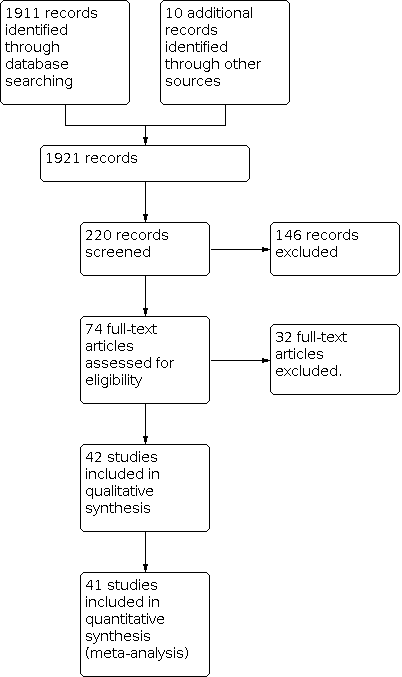
PRISMA Study flow diagram.
Subgroup analysis and investigation of heterogeneity
-
A subgroup analysis was undertaken to examine differences between individual, group and family/parental CBT formats.
-
A second analysis was carried out to identify whether CBT was more effective than other active treatments, with subgroups of active controls and TAU.
-
Last, maintenance of treatment gains was assessed using follow‐up data of treatment versus W/L follow‐up controls and CBT versus active controls.
The Chi2 test and the I2 statistic were used to assess statistical heterogeneity for all analyses and between groups. Significance was set at P < 0.1.
Sensitivity analysis
Sensitivity analysis is the study of how the uncertainty in the output of an analysis can be apportioned to different sources of uncertainty in its inputs. Sensitivity analyses can therefore be carried out to test the robustness of decisions made in the review process. Sensitivity analyses were carried out where there was evidence of the following:
-
Significant heterogeneity: Forest plots were inspected and each study in turn was examined to determine the source of any significant heterogeneity.
-
Selection bias: Those studies judged to be at high risk of bias for selection bias were excluded from the main analysis.
-
Allocation concealment: Those studies judged to be at high risk of bias for allocation concealment were excluded from the main analysis.
-
We also undertook all of the above for the completer analyses (Analysis 1.6; Analysis 2.6; Analysis 3.4).
Results
Description of studies
See: Characteristics of included studies; Characteristics of excluded studies; Characteristics of ongoing studies.
All studies were RCTs, and one was a school‐based cluster‐RCT (Dadds 1997). The active controls or the psychological placebo consisted of psycho‐education (Herbert 2009; Kendall 2008; Masia‐Warner 2007), bibliotherapy (Cobham 2012) and therapist and peer support (Ginsburg 2002).
Results of the search
We found 1921 citations using the search strategy run in July 2012, of which 220 were abstracts of potential interest. Among the retrieved articles, 74 studies were relevant for further assessment, and 42 of these were included (Figure 3).
In cases where clarification or further data were needed, the trial authors were contacted. We contacted 20 trialists, and 16 replied with the relevant data.
Included studies
Forty‐one studies met the inclusion criteria for the main analysis of this review (Barrett 1996; Barrett 1998; Barrington 2005; Chalfant 2007; Cobham 2012; Dadds 1997; Dadds 1999; Flannery‐Schroeder 2000; Galla 2012; Gil‐Bernal 2009; Ginsburg 2002; Ginsburg 2012; Hayward 2000; Herbert 2009; Hirshfeld‐Becker 2010; Hudson 2009; Kendall 1994; Kendall 1997; Kendall 2008; Lau 2010; McNally Keehn 2012; Melfsen 2011; Mendlowitz 1999; Muris 2002; Nauta 2003; Olivares 2005; Reaven 2012; Sánchez‐García 2009; Schneider 2011; Shortt 2001; Silverman 1999; Spence 2000; Spence 2006; Sung 2011; Walkup 2008; Waters 2009; Masia‐Warner 2005; Masia‐Warner 2007; Masia‐Warner 2011; White 2012; Wood 2009).
Design
The studies were randomised controlled studies; some had three arms: one control group and two CBT formats (individual and group or family/parental). Two studies were pilot studies (Hayward 2000; Ginsburg 2002). One study tested a CBT protocol in very young children (4 to 7 years) (Hirshfeld‐Becker 2010), and three studies included slightly older but still young children (Lau 2010; Waters 2009; Schneider 2011).
Eleven studies (Ginsburg 2002; Muris 2002; Barrington 2005; Masia‐Warner 2007; Kendall 2008; Sánchez‐García 2009; Herbert 2009; Hudson 2009; Sung 2011; Ginsburg 2012) were considered in the secondary analysis of the effectiveness of CBT compared with other active treatments or TAU. With regard to the comparison of CBT with medication, only one study (Walkup 2008) was included in this review; therefore no meta‐analysis was possible.
Last, follow‐up publications from studies involved in the main analysis were retained and included in a separate analysis. In total only four studies were eligible, involving waiting list controls at follow‐up (Dadds 1999; Gil‐Bernal 2009; Hayward 2000; Sánchez‐García 2009). The follow‐up period ranged from 6 months to 24 months (mean 13.5 months, SD 7.5). Other studies, which purported to show the persistence of the effects of CBT, did not include follow‐up of controls.
Sample sizes
The 41 studies involved 1034 participants and 921 controls. The numbers of participants in the studies are shown in Table 1.
|
| Number of studies | Mean | Std. Dev. | Min | Max |
| Individual CBT | 7 | 29.14 | 15.75 | 12 | 60 |
| Individual Controls | 7 | 21.57 | 10.71 | 10 | 43 |
| Group CBT | 13 | 24.77 | 14.71 | 6 | 64 |
| Group Controls | 13 | 21.92 | 14.41 | 5 | 67 |
| Family/Parental CBT | 11 | 25 | 13.02 | 6 | 54 |
| Family/Parental Controls | 11 | 17.18 | 6.62 | 5 | 29 |
Settings
Most of the studies were initially conducted in research settings (i.e. university outpatient clinics); however, later studies were conducted in community clinics and inner city schools, and included various cultures such as Hong Kong Chinese (Lau 2010). No studies involved inpatients.
Participants
Participants were recruited from the community via local advertisements or outpatient clinics. All met criteria for a psychiatric diagnosis of an anxiety disorder, ranging from mild to moderate, but not severe.
Conditions
Anxiety disorders included in the studies were: separation anxiety disorder (SAD) 21; overanxious disorder (OAD) 6; social phobia (SOP) 20; panic disorder (PD) 4; generalised anxiety disorder (GAD) 17 and specific phobia (SP) 4.
Comorbid conditions were included and most often involved other secondary anxiety diagnoses: depression, conduct disorders (CDs) and oppositional defiant disorder (ODD) and attention‐deficit/hyperactivity disorder (ADHD).
Interventions
The number of sessions varied, with a mean of 13.1 (SD 2.9) and a range of 9 to 20. Active controls included a psychological placebo such as educational and bibliotherapy/supportive work with no elements of CBT. TAU was described as including family therapy, play therapy, supportive psychotherapy, psychodynamic psychotherapy and non‐CBT eclectic approaches. In this review the only medication included in a trial of CBT versus medication and in combination versus placebo was sertraline.
The 41 studies involved 1038 participants and 768 controls. Most of the studies were initially conducted in research settings (i.e. university outpatient clinics); however, later studies were undertaken in community clinics and inner city schools and included differing cultures such as Hong Kong Chinese (Lau 2010). No studies involved inpatients. Comorbid conditions were included and most often involved other secondary anxiety diagnoses: depression, CDs and ODD and ADHD. Participants were recruited from the community via local advertisements or outpatient clinics. All met criteria for a psychiatric diagnosis of anxiety disorder; the range was from mild to moderate, and severe cases were not included.
Outcomes
Valid and reliable assessment is regarded as essential to the successful application of CBT (Thyrer 1991). All studies used semi‐structured instruments to diagnose anxiety disorders: ADIS (the Anxiety Disorder Interview Schedule) (Barrett 1996; Barrett 1998; Barrington 2005; Dadds 1997; Flannery‐Schroeder 2000; Ginsburg 2002; Ginsburg 2012; Hayward 2000; Herbert 2009; Hudson 2009; Kendall 1994; Kendall 1997; Kendall 2008; Lau 2010; Nauta 2003; Olivares 2005; Silverman 1999; Spence 2000; Spence 2006; Masia‐Warner 2005; Masia‐Warner 2007; Masia‐Warner 2011; Reaven 2012; Sánchez‐García 2009; Waters 2009; White 2012; Wood 2009); the Kiddie‐Schedule for Affective Disorders and Schizophrenia (Hirshfeld‐Becker 2010; Lau 2010); DISCAP (Diagnostic Interview Schedule for Children, Adolescents and Parents) (Shortt 2001; Mendlowitz 1999) or the Kinder‐DIPS (Schneider 2011). Only one study did not use a structured interview (Sung 2011). ADIS is administered separately to parents and child, and results are then combined for an overall diagnosis; however, several studies used approaches different from this practice to determine diagnosis (parents only) (Shortt 2001; Spence 2000) (children only) (Olivares 2005) and treatment outcomes (parents only) (Flannery‐Schroeder 2000; Kendall 1994; Kendall 1997; Shortt 2001; Spence 2000; Spence 2006).
Anxiety symptoms were assessed using a wide range of rating scales, making comparisons difficult; some rating scales were used in only one or two studies. Scales that were used frequently include the following: the Revised Children's Manifest Anxiety Scale (RCMAS) (Dadds 1997; Flannery‐Schroeder 2000; Kendall 1994; Kendall 1997; Kendall 2008; Mendlowitz 1999; Shortt 2001; Silverman 1999; Spence 2000; Spence 2006); the Fear Survey for Children Revised (FSSC‐R) (Barrett 1996; Barrett 1998; Kendall 1994; Nauta 2003; Silverman 1999); the Social Anxiety Scale for Adolescents (SAS‐A) (Ginsburg 2002; Herbert 2009; Olivares 2005); the Social Phobia and Anxiety Inventory for Children (SPAI) (Hayward 2000; Herbert 2009; Olivares 2005); the Mood and Anxiety Symptom Scale (MASQ) (Kendall 2008); the Spence Child Anxiety Scale, child and parent versions (SCAS) (Hudson 2009; Lau 2010;; Nauta 2003; Spence 2000; Spence 2006); the Child Behavior Checklist (CBCL) (Barrett 1996; Barrett 1998; Dadds 1997; Flannery‐Schroeder 2000; Gil‐Bernal 2009; Kendall 1994; Kendall 2008; Nauta 2003; Shortt 2001; Silverman 1999; Spence 2006) and the Clinical Global Impressions scale (Herbert 2009; Hirshfeld‐Becker 2010). All the measures used have been assessed as having reasonably good psychometric properties in terms of reliability, validity and efficacy in measuring internalising symptoms (Myers 2002). In view of poor agreement between child and parent reporting of anxiety symptoms (Grills 2003), child self‐report ratings were preferred when data were entered into the meta‐analysis. Data on the CBCL were presented in two forms-raw scores and transformed scores-which did not allow direct comparative analysis.
Excluded studies
Eleven studies were excluded (Blagg 1984; King 1998; Last 1998; Lowry‐Webster 2003; Mifsud 2005; Olivares 2007; Ordeig 2004; Sofronoff 2005; Warren 1984) because some participants did not have verifiable anxiety diagnoses, or they did not provide a primary outcome measure. Four studies involved SOPs only or a large majority of simple phobias or participants with OCD, and the authors of these studies were unable to provide the data with these participants removed (Cornwall 1996; Menzies 1993; Silverman 1999b; Sofronoff 2005). Nine studies were primarily concerned with issues of comorbidity and/or presented data previously reported elsewhere or were preliminary studies or follow‐up studies (Flannery‐Schroeder 1998; Flannery‐Schroeder 2005; Garcia‐Lopez 2006; Forman 2007; Holmes 2006; Kendall 2001; Kendall 2009; Suveg 2009; Wood 2009b). In one foreign language study, cases were allocated on an alternating basis (Joorman 2002), and in another study an active but unspecified control treatment was administered (Beidel 2000). Two studies were excluded because the intervention (Social Effectiveness Therapy for Children and Adolescents) was primarily a behavioural treatment rather than CBT (Baer 2005; Beidel 2007).
Risk of bias in included studies
Allocation
Ten studies provided a clear description of the process of adequate sequence generation (Walkup 2008;Masia‐Warner 2011;Reaven 2012;White 2012; Ginsburg 2012;Ginsburg 2002;Hudson 2009;Kendall 2008Spence 2006;Melfsen 2011). In six studies (Herbert 2009;Flannery‐Schroeder 2000;Galla 2012;Schneider 2011;Sung 2011;Wood 2009), restricted randomisation was used, whereby participants were allocated in blocks. In the pilot study (Hayward 2000), participants were recruited to the control group following the process of randomisation, and the results were reported as from a single control group. One study used coin tossing as a means of randomising allocation (Spence 2006), and in another the process of randomisation involved picking numbers out of a box (White 2012). In other included studies, the process of sequence generation was unclear. A sensitivity analysis (not shown) for those studies reporting clear processes of randomisation showed similar direction of results as the main analysis with all studies included, with CBT being effective versus W/L controls for the remission of anxiety diagnoses (OR 0.1, 95% CI 0.05 to 0.18, Z = 7.48, P < 0.00001).
Blinding
Thirty‐two of the studies in the main analysis and the sub‐analyses had blinded outcome evaluations (Barrett 1996; Barrett 1998; Barrington 2005; Cobham 2012; Dadds 1997; Dadds 1999; Galla 2012: Ginsburg 2002; Hayward 2000; Herbert 2009; Hirshfeld‐Becker 2010; Hudson 2009; Kendall 1994; Kendall 2008; Lau 2010; McNally Keehn 2012; Melfsen 2011; Muris 2002; Reaven 2012; Schneider 2011; Shortt 2001; Silverman 1999; Spence 2000; Spence 2006; Sánchez‐García 2009; Sung 2011; Walkup 2008; Masia‐Warner 2005; Masia‐Warner 2007; Masia‐Warner 2011; Waters 2009;; White 2012; Wood 2009). In the remainder of included studies, it was unclear whether outcome assessors were blinded to the treatment status of participants, leading to the possibility of a moderate to severe degree of detection bias in these studies.
Performance bias was assessed only in the trials of CBT versus active treatment or TAU, as plainly this was not possible or sensible in the case of CBT versus W/L controls. In the former studies, measures were taken and described to ensure comparability of treatments, so that non‐specific confounders such as length of treatment, etc, did not influence the outcome in either arm of the trial.
Incomplete outcome data
Overall accounting for participants was complete; however, a CONSORT flow diagram was used in only 11 studies (11/41 = 26.8%). No difference was noted with regard to withdrawals or dropouts between CBT and W/L controls (Z = 0.27, P = 0.78). No exclusions were reported, and a low but consistent rate of reported dropouts was described (CBT 10.8% vs W/L 10.3%).
Selective reporting
Reporting bias, which refers to any systematic difference between reported and unreported findings, is regarded as one of the most substantial biases affecting results from individual studies (Chan 2005). Systematic examination revealed no cases of unreported findings in the studies included in this meta‐analysis.
Other potential sources of bias
Treatment protocols
Use of a protocol not only allows reproducibility-an important goal of research and, ultimately, for introduction into clinical practice-it should prevent unintentional differences or indeed 'drift', but not necessarily documented changes away from the core treatment design. In most of the studies, a defined, published protocol was used and supervision was included at various stages of treatment. In two studies (Barrett 1998; Kendall 1997), a small number of participants were treated flexibly, but the treatment delivered was in accord with a manual. Modular but documented CBT was delivered in three studies (Galla 2012; Ginsburg 2012; White 2012). Most of the therapists were post‐doctorate psychologists.Individual, group and family formats were included. Groups were often staged according to age, for instance, as older and younger children. Family formats differed and included some sessions with the child or adolescent; others involved sessions with parent(s) or guardian(s) separately. Considerable variation was noted in length of treatment (from 7.5 hours (Ginsburg 2002) to 27 hours (Flannery‐Schroeder 2000)) and in the number of sessions (mean 13.2, SD 2.9, range 9 to 20). Five studies (Dadds 1997; Ginsburg 2002; Olivares 2005; Galla 2012; Ginsburg 2012) were school based, and others were clinic based. Controls were participants who either (1) remained on the waiting list without treatment for anxiety before they were offered CBT, or (2) received a form of treatment with a therapeutic element that was not CBT based (active control) or were given only attention or TAU.
Effects of interventions
See: Summary of findings 1 CBT compared to wait‐list for children and adolescents with anxiety disorders; Summary of findings 2 CBT compared to active controls for children and adolescents with anxiety disorder; Summary of findings 3 CBT compared to treatment as usual (TAU) for children and adolescents with anxiety disorder
Comparison one: CBT versus waiting list
Primary outcomes
1.1 Remission of anxiety diagnoses (ITT analysis)
Twenty‐six studies (Barrett 1996; Barrett 1998; Chalfant 2007; Cobham 2012; Dadds 1997; Flannery‐Schroeder 2000; Galla 2012; Gil‐Bernal 2009; Hayward 2000; Hirshfeld‐Becker 2010; Kendall 1994; Kendall 1997; Lau 2010; Melfsen 2011; McNally Keehn 2012; Nauta 2003; Olivares 2005; Schneider 2011;Shortt 2001; Silverman 1999; Spence 2000; Spence 2006; Masia‐Warner 2005; Masia‐Warner 2011; Waters 2009; Wood 2009) were included in the final analysis on remission of any anxiety diagnosis. The ITT analysis included 808 CBT participants and 542 controls, with a response rate for remission of any anxiety diagnosis of 58.9% for CBT versus 16 % for controls (OR 7.85, 95% CI 5.31 to 11.60) (Analysis 1.1). Most of the studies (72%,18 out of 25) reported findings in the direction of showing clear benefit for CBT (95% CI does not cross 1, indicating equivalence of response) (Analysis 1.1;Figure 4). Evidence of heterogeneity was found (I2 = 30%, Chi2 = 44.58, d.f. = 31, P = 0.05). Heterogeneity was investigated using meta‐regression (STATA 2009), which showed that only modest variability was accounted for by participant age (1.06%), sex (5.32%), level of comorbidity (6.7%), initial level of anxiety (5.5%) or number of CBT sessions (0.23%). No difference in outcome was noted for the differing formats of CBT-individual, group and family (Chi2 = 0.06, d.f. = 2; P = 0.97)-or for heterogeneity between formats (I2 = 0%).

Forest plot of comparison: 1 CBT versus wait‐list, outcome: 1.1 Remission of anxiety diagnoses (ITT analysis).
1.2 Acceptability: participants lost to follow‐up
No difference was reported between CBT and W/L controls in terms of the rate of those lost to follow‐up (Analysis 1.2), indicating a similar degree of acceptability. In the CBT group, the rate of loss to follow‐up was 10.6% (82 out of 771) versus 10.6% (56 out of 550) in the control group (OR 0.94, 95% CI 0.58 to 1.51).Test for overall effect: Z = 0.27. P = 0.79.
Secondary outcomes
1.3 Reduction in anxiety symptoms
Thirty studies (Barrett 1996; Barrett 1998; Chalfant 2007; Cobham 2012; Dadds 1997; Gil‐Bernal 2009; Flannery‐Schroeder 2000; Galla 2012; Hayward 2000; Hirshfeld‐Becker 2010; Kendall 1994; Kendall 1997; Lau 2010; Melfsen 2011; McNally Keehn 2012; Mendlowitz 1999; Nauta 2003; Olivares 2005; Sánchez‐García 2009; Schneider 2011; Shortt 2001; Silverman 1999; Spence 2000; Spence 2006; Masia‐Warner 2005; Masia‐Warner 2011; Muris 2002; Waters 2009; White 2012; Wood 2009) were included in the final analysis on reduction of anxiety symptoms. The standard mean difference (SMD) was ‐0.98 (95% CI ‐1.21 to ‐0.74, Z = 8.21, P < 0.00001) with significant heterogeneity (I2 = 75%, Chi2 = 140.07, d.f. = 35, P < 0.00001) (Analysis 1.3). Heterogeneity was investigated using meta‐regression (STATA 2009), but no significant results were found for the covariates of age, sex, and length of treatment. Evidence revealed a significant subgroup difference between individual, group and family/parental formats of CBT (Chi2 = 7.48 d.f. = 2, P = 0.02), with considerable heterogeneity (I2 = 73.3%). Inspection of the forest plot and of the summary statistics for each subgroup suggests that both group and family/parental formats of CBT produce greater reduction of symptoms than is produced by individual CBT.
1.4 Remission of anxiety diagnoses-long‐term follow‐up
Three studies examined CBT participants and control follow‐ups (Dadds 1999; Gil‐Bernal 2009; Hayward 2000) at 24, 6 and 12 months, respectively (mean 13.5 months, SD 7.5). In terms of remission of anxiety diagnoses, a non‐significant effect was noted (OR 3.22, 95% CI 0.96 to 10.75, Z = 1.90, P = 0.06) (I2 = 38%) (Analysis 1.4).
1.5 Reduction in anxiety symptoms-long‐term follow‐up
With just four studies, a non‐significant effect was noted in the reduction of symptoms (SMD = ‐1.55, 95% CI ‐3.22 to 0.11, Z = 1.83, P = 0.07) with great heterogeneity (Chi2 = 49.69, d.f. 3, P = 0.00001, I2 = 94%) (Analysis 1.5).
Comparison two: CBT versus active controls
Primary outcomes
2.1 Remission of anxiety diagnoses (ITT analysis)
Six studies examined CBT versus active controls with respect to remission of anxiety diagnoses, which were non‐significant (OR 1.51, 95% CI 0.77 to 2.96, Z = 1.21, P = 0.23) (Analysis 2.1).
2.2 Acceptability: participants lost to follow‐up
Five studies examined CBT versus active controls with respect to participants lost to follow‐up, which were significant, favouring CBT over active controls (OR 0.52, 95% CI 0.31 to 0.91, Z = 2.28, P = 0.02) (Analysis 2.2).
Secondary outcomes
2.3 Reduction in anxiety symptoms
Eight studies examined reduction in anxiety symptoms (SMD = ‐0.50, 95% CI ‐1.09 to 0.09); findings were non‐significant (Z = 1.66, P = 0.1) (Analysis 2.3). The significant heterogeneity (I2 = 86%, P < 0.00001) was reduced to 3% with the removal of one study (Masia‐Warner 2007).
2.4 Remission of anxiety diagnoses-long‐term follow‐up
Two studies examined CBT versus active controls with respect to remission of anxiety diagnoses at follow‐up; findings were significant, favouring CBT over active controls (OR 2.03, 95% CI 1.22 to 3.36, Z = 2.74, P = 0.006) ( Analysis 2.4).
2.5 Reduction in anxiety symptoms-long‐term follow‐up
Four studies examined CBT versus active controls with respect to remission of anxiety symptoms at follow‐up; findings were non‐significant (SMD ‐0.92, 95% CI ‐2.12 to 0.29, Z = 1.49, P = 0.14) ( Analysis 2.5). The significant heterogeneity (I2 = 96%, P < 0.00001) was reduced to 0% with the removal of one study (Hudson 2009).
Comparison three: CBT versus treatment as usual (TAU)
Primary outcomes
3.1 Remission of anxiety diagnoses (ITT analysis)
Only two studies examined CBT versus TAU with respect to remission of anxiety diagnoses; findings were non‐significant (OR 0.53, 95% CI 0.23 to 1.25, Z = 1.03, P = 0.3) (Analysis 3.1).
3.2 Acceptability: participants lost to follow‐up
Two studies examined CBT versus TAU with respect to participants lost to follow‐up; findings were non‐significant (OR 1.01, 95% CI 0.31 to 3.31, Z = 0.02, P = 0.98) (Analysis 3.2).
Secondary outcomes
3.3 Reduction in anxiety symptoms
Three studies examined reduction in anxiety symptoms; findings were non‐significant (SMD = ‐0.19, 95% CI ‐0.79 to 0.40, Z = 0.64, P = 0.52) ( Analysis 3.3).
3.x Remission of anxiety diagnoses-long‐term follow‐up
No data were available.
3.x Reduction in anxiety symptoms-long‐term follow‐up
No data were available.
Comparisons four and five: CBT versus medication and combination versus placebo
Only one study was available (Walkup 2008), so no meta‐analysis was possible. This large multi‐centre comparative study of CBT versus medication with more than 400 participants showed that both CBT and sertraline-a selective serotonin re‐uptake inhibitor (SSRI) antidepressant-were more effective than placebo in treating paediatric anxiety disorders, and that the combination of CBT with medication was more effective than CBT or medication alone.
Sensitivity analyses
CBT versus waiting list: completers‐only analysis
1.6 Remission of anxiety diagnoses
Twenty‐six studies examined CBT versus waiting list with respect to remission of anxiety diagnoses; findings were highly significant (OR 11.09, 95% CI 7.47 to 16.45, Z = 12.24, P =< 0.0001) with no difference between formats-individual, group and family/parental (Chi2 = 0.03, d.f. 2, P = 0.99, I2 = 0%) (Analysis 1.6).
CBT versus active controls: completers‐only analysis
2.6 Remission of anxiety diagnoses
Five studies examined CBT versus active controls with respect to remission of anxiety diagnoses; findings were significant (OR 2.18, 95% CI 1.31 to 3.64, Z = 2.98, P = 0.003) (Analysis 2.6).
CBT versus treatment as usual (TAU): completers‐only analysis
3.4 Remission of anxiety diagnoses
Only two studies examined CBT versus TAU with respect to remission of anxiety diagnoses; findings were non‐significant (OR 1.10 95% CI 0.45 to 2.68, Z = 0.2, P = 0.84) (Analysis 3.4).
Other analyses
CBT for those with autism spectrum disorders (ASDs)
Post hoc analyses of those with high‐functioning ASD revealed a significant reduction in anxiety diagnoses compared with W/L controls (Chalfant 2007; McNally Keehn 2012; Schneider 2011; Wood 2009). Odds ratio was 16.74 (95% CI 6.30 to 44.48, Z = 5.65, P < 0.0001), with a significant reduction in anxiety symptoms (Chalfant 2007; McNally Keehn 2012; White 2012; Wood 2009) (SMD ‐1.6, 95% CI ‐3.00 to ‐0.2, Z = 2.24, P = 0.03, I² = 95%), indicating a positive outcome of CBT for children and adolescents with ASD.
Publication Bias
With respect to remission of anxiety diagnoses, an indication of publication bias was shown by an asymmetrical funnel plot (Figure 5), confirmed by a highly significant Egger’s test (bias ‐2.03, t = ‐3.95, P < 0.001). The funnel plot (with Egger’s regression line, not shown) indicates smaller studies (those with larger standard errors) tending to have larger (more beneficial) ORs-a finding compatible with publication bias. Although funnel asymmetry may indicate selection biases, in particular publication bias, other explanations include citation bias, true heterogeneity, with size of effect differing according to study size, intensity of intervention and differences in underlying risk. Data irregularities, poor methodological design of small studies and inadequate analyses may also result in asymmetry. A contour‐enhanced funnel plot (Peters 2008), however, showed that the studies in this review were in the region of statistical significance, indicating that the cause of the asymmetry was more likely to involve factors other than publication bias, such as variable study quality.

Funnel plot of comparison: 1 CBT versus wait‐list, outcome: 1.1 Remission of anxiety diagnoses (ITT analysis).
Discussion
Summary of main results
Since the last Cochrane review (James 2005), the number of studies available for review increased considerably from 18 to 41, with more than two times the total number of participants. This larger, more adequately powered review should increase confidence in the findings. The present systematic review indicates that cognitive behavioural therapy (CBT) is a useful treatment for anxiety disorders in children and adolescents. Using conservative intention‐to‐treat (ITT) criteria, the remission rate for anxiety disorders (58.9% for CBT vs 16% for controls) is similar to that reported in a meta‐analysis by Cartwright‐Hatton (Cartwright‐H 2004). The number needed to treat (NNT) using conservative ITT data is 3.0 (95% CI 1.75 to 3.03), which means that for one additional participant to attain remission from anxiety disorder using CBT, one needs to treat thre participants. In terms of medical and psychological treatments, this is a very acceptable finding (Laupacis 1988), allowing one to recommend CBT in clinical practice. Research trials now include non‐specialist therapists in community clinic settings and inner city schools (Ginsburg 2012), suggesting that the findings are generalisable.
This review has shown CBT to be superior to waiting list controls; however, the notion that CBT might be superior to active controls, including psycho‐education, other supportive interventions, bibliotherapy and treatment as usual, was not confirmed, although the sensitivity analysis with completer‐only participants was significant for remission of anxiety diagnoses for CBT versus active controls (Z = 2.98, P = 0.003) (Analysis 2.6). Evidence is limited, however, by the small number of studies.
The question whether CBT is superior to medication, or indeed if there is any specificity to treatment response, remains unclear with only one study (Walkup 2008), although a study of a behavioural treatment with fluoxetine showed a similar pattern of results (Beidel 1995). Further work in this area is needed.
An important question is the durability of treatment effects. Evidence, unfortunately, is limited. Three studies examining the longitudinal reduction in anxiety diagnoses compared with follow‐up W/L controls (Dadds 1999; Hayward 2000; Gil‐Bernal 2009) with only 124 participants showed a non‐significant treatment effect (OR 3.22, 95% CI 0.96 to 10.75, Z = 1.89, P = 0.06)( Analysis 1.4)These studies were of relatively short duration. Many studies report the persistence of the treatment effects of CBT over periods of 2 to 24 months, and one up to eight years (Saavedra 2010); however, these studies were not controlled follow‐up studies; therefore, one cannot discount the natural remission rate.
Some uncertainty remains as to whether younger patients can use or benefit from CBT. Children need a certain level of cognitive maturity to participate in the treatment (Kendall 1990b), and in general they need to be able to use de‐centring techniques such as narratives or stories. It was not clear, for instance, whether children younger than six years of age were capable of these cognitive manoeuvres. A recent study (Hirshfeld‐Becker 2010) included in this review found positive effects in children younger than six years. It is likely that children respond more to the behavioural than to the demanding cognitive elements of CBT (Essau 2004). Researchers aware of the problems of using CBT with very young children have instead involved parents, directly or indeed entirely (Cartwright‐Hatton 2011).
It is recognised that children and adolescents with autism spectrum disorders (ASDs) have high rates of anxiety disorders (White 2009), particularly social phobia (Settipani 2012). Several trials are exploring the use of CBT for anxiety disorders in children and adolescents with ASD (Chalfant 2007; McNally Keehn 2012; Reaven 2012; Sung 2011; Wood 2009; White 2012), but none have included those with an intellectual disability specifically. In a review, Lang (Lang 2010) noted the need for CBT to be modified for individuals with ASD by adding interventional components typically associated with applied behaviour analysis (e.g. systematic prompting and differential reinforcement). It is interesting to note that a post‐hoc analysis suggests that CBT is particularly effective for children and adolescents with ASD.
This review did not confirm previous findings that severity of anxiety and comorbidity were related to outcome (Liber 2010); indeed age, severity of the initial anxiety disorder, gender, and the number of sessions did not substantially affect the outcome. It has to be noted, however, that the numbers of sessions in this review were restricted. Indeed, one study of brief CBT found a positive outcome (Gallagher 2004) with only three sessions but was not included, as per the original exclusion criteria.
Last, this review has shown that CBT is an acceptable form of therapy, as shown by comparison of the rates of those lost to follow‐up between CBT and control groups.
Overall completeness and applicability of evidence
Demographics and clinical characteristics
Apart from one pilot study (Hayward 2000), all studies included participants of both sexes and covered a range of socioeconomic classes. Nine studies did not give details on ethnicity (Barrett 1996; Barrett 1998; Hayward 2000; Mendlowitz 1999; Nauta 2003; Olivares 2005; Spence 2000; Spence 2006; Schneider 2011). Although overall age ranged from 4 to 18 years, only three studies included participants younger than the age of 7 (Hirshfeld‐Becker 2010; Lau 2010; Silverman 1999), which means that younger children were relatively under‐represented.
It is of note that only community or outpatient participants were included in these studies, so it is not possible to extrapolate the results to patients with the most severe cases of anxiety disorder, who might have received day patient or inpatient treatment. Comorbid disorders such as depression, other anxiety disorders, ADHD and conduct disorders were included, allowing more generalised conclusions to be drawn and comparison made with more routine clinical practice. Since the last Cochrane review, a number of studies (Chalfant 2007; McNally Keehn 2012; Reaven 2012; Sung 2011; White 2012; Wood 2009) have focused on children and adolescents with high‐functioning ASD. CBT appears effective in these groups of participants. A considerable limitation, however, is the exclusion of participants with learning disabilities, who were not represented in this review.
The consistency of the rate of remission of anxiety diagnosis using CBT versus waiting list controls in this review and other reviews and meta‐analyses (Compton 2004; Cartwright‐H 2004; James 2005; Scott 2005; Silverman 2008; Seligman 2011; Reynolds 2012) is encouraging and suggests that this is a fairly robust finding. Evidence for CBT versus active controls or TAU is negative, but a smaller number of studies are available. Only one study (Walkup 2008) looked at the comparative efficacy of CBT versus pharmacotherapy and combination therapy (Walkup 2008); therefore it is clear that further work is needed in this area.
The number of follow‐up studies with controls is very limited (n = 4), making it difficult to draw any conclusions. The findings are non‐significant. A number of studies show that the effects of CBT appear to persist, but the evidence is limited without controls. Most of the studies offer CBT to W/L controls after completion of the study.
Quality of the evidence
In considering these findings, several methodological issues need to be addressed. The review identified 41 studies (n = 41) with a reasonably large number of study participants (1806). Most of these studies (78%) were in the direction of showing benefit for CBT. For remission of anxiety diagnosis (OR 0.12, 95% CI 0.08 to 0.18), an estimate of effect size is medium, according to Cohen’s criteria (Cohen 1988), with tight confidence intervals suggesting some uniformity in the findings.
Methodological shortfalls were noted in some studies, most notably inadequate details on the process of randomisation and allocation. In the previous review (James 2005), reporting of those lost to therapy was inadequate; however, more recent studies have adopted the revised CONSORT criteria for RCTs (Consolidated Standards of Reporting Trials, http://www.consort‐statement.org) (Altman 2012). It is not possible in this type of research to blind the participants-an obvious potential for bias; however, the evaluations were carried out blind, although details of this processing in several cases were not made clear.
With respect to remission of anxiety diagnoses, evidence of moderate heterogeneity (Chi2 = 44.58, d.f. = 31, P = 0.05, I 2 = 30%) was noted across all formats, with no subgroup heterogeneity (I2 = 0%), indicating a similar degree of heterogeneity across formats for the delivery of CBT-individual, group and family/parental. Uniformity was noted in the variability in effect sizes, with no particular studies contributing to the heterogeneity as shown by sensitivity analyses. Meta‐regression (STATA 2009) showed that only modest variability was accounted for by participant age (1.06%), sex (5.32%), level of comorbidity (6.7%) or initial level of anxiety (5.5%) or by the number of CBT sessions (0.23%).
CBT is not a uniform intervention; considerable clinical variations are possible and hence heterogeneity in the methods of delivering CBT is noted, even within major groupings. For instance, within the family/parental CBT group, some therapists see whole families, others only parents, and family involvement may include elements of CBT or psycho‐education. Variations in the CBT programmes are evident in group and individual CBT studies with regard to the extent of cognitive versus behavioural work, and when and how this is carried out. One question, particularly with regard to anxiety symptoms, is whether the heterogeneity is due, in part, to the differing anxiety diagnoses such as generalised anxiety disorder (GAD), social phobia (SOP), etc.; however, it was not possible to analyse the diagnoses separately, although some studies focused specifically on social phobia (Gil‐Bernal 2009; Hayward 2000; Masia‐Warner 2005).
One of the sources of heterogeneity, particularly in comparisons of anxiety symptoms, is the large number of rating scales used, some of which measure non‐specific emotional symptoms rather than anxiety symptoms. Therefore, when studies are compared in the future, it would be important to use fewer, but more standardised, anxiety rating scales. A naturalistic problem is the wide range of anxiety disorders covered in this review under the term anxiety disorders, which may account for some of the heterogeneity. Subgroup analysis by diagnosis was not possible.
Although there was an indication of publication bias with an asymmetrical funnel plot and a highly significant Egger's test, further analysis with a contour‐enhanced funnel plot (Peters 2008) with all studies in the area of significance points, instead, to study variability as the cause of the asymmetrical funnel plot.
Potential biases in the review process
Meta‐analyses are limited by the robustness of any search method. The electronic search was thorough and large in scale with broad parameters. In this review we were able to obtain all the referenced papers, and we were able to be in contact with leading researchers in the field. Non‐English studies were also included.
The selection criteria may have limited the review as the length of the study was arbitrarily set at nine sessions. One study of brief CBT (Gallagher 2004) was reported to be effective, but as this study only involved three sessions, it was excluded. The analysis of studies with three arms-CBT in two formats versus waiting list controls or active controls-is problematic in that double counting of any group is wrong. We chose to split the controls sample into two equal halves between the CBT groups. However, analysis with some differing methods (lumping together) did not alter the outcome of the analyses.
Agreements and disagreements with other studies or reviews
A previous Cochrane review (James 2005) of eighteen studies with 498 participants and 311 controls found a response rate for remission of any anxiety diagnosis using an ITT analysis of 56% for CBT versus 28.2% for controls with the number needed to treat (NNT) of 3.0 (95% CI 2.5 to 4.5). For reduction in anxiety symptoms, the standardised mean difference (SMD) was ‐0.58 (95% CI ‐0.76 to ‐0.40). Overall, very considerable agreement is evident between meta‐analyses of CBT for the treatment of anxiety disorders in children and adolescents (Cartwright‐H 2004; Compton 2004; James 2005; Silverman 2008; Seligman 2011; Reynolds 2012). Using conservative ITT criteria, the remission rate for anxiety disorders of 58.9% for CBT versus 16 % for controls is similar to the findings of the meta‐analysis reported in the previous Cochrane review (James 2005), The finding that no advantage was derived, for instance, from adding parent training to individual CBT was in line with other meta‐analyses (Silverman 2008; Reynolds 2012) and a recent review (Breinholst 2012). One review in assessing 10 anxiety studies found moderate effect sizes (ESs) of 0.50 (SE 0.12) for changes in cognitive processes, with a noted smaller effect when CBT was compared with active controls (Chu 2007). Taken together, these provided a reasonably solid evidence base for the use of CBT in the treatment of childhood anxiety disorders.
A review of CBT for anxiety disorders in ASD (Lang 2010) has shown positive results of CBT, albeit with a smaller number of studies than were reviewed here (Chalfant 2007; McNally Keehn 2012; Reaven 2012; Schneider 2011; Sung 2011; Wood 2009; White 2012). Furthermore, CBT has to be modified in the ASD population because of cognitive biases, and it is not clear how CBT with a greater emphasis on behavioural rather than cognitive changes matches CBT delivered generally (Lang 2010). In a recent review (Reaven 2011), the lack of detail on parental involvement in treatment, particularly for teenagers, was noted; however, several studies in this review did include parents (Chalfant 2007; McNally Keehn 2012; Reaven 2012; Wood 2009; White 2012).

Risk of bias summary: risk of bias item for each included study.

Risk of bias graph: risk of bias item presented as percentages across all included studies.
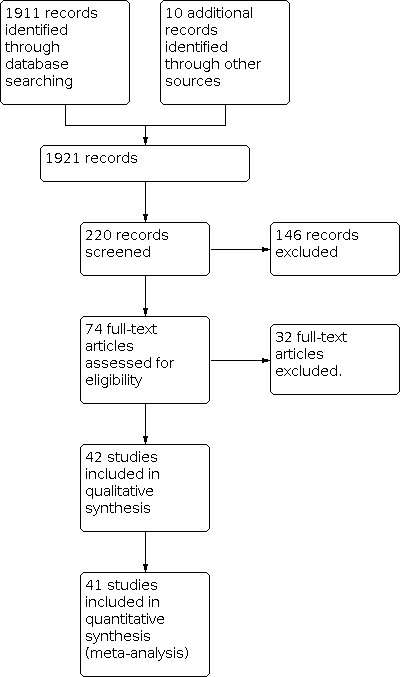
PRISMA Study flow diagram.

Forest plot of comparison: 1 CBT versus wait‐list, outcome: 1.1 Remission of anxiety diagnoses (ITT analysis).

Funnel plot of comparison: 1 CBT versus wait‐list, outcome: 1.1 Remission of anxiety diagnoses (ITT analysis).

Comparison 1: CBT versus wait‐list, Outcome 1: Remission of anxiety diagnoses (ITT analysis)

Comparison 1: CBT versus wait‐list, Outcome 2: Acceptability ‐participants lost to follow‐up

Comparison 1: CBT versus wait‐list, Outcome 3: Reduction in anxiety symptoms

Comparison 1: CBT versus wait‐list, Outcome 4: Remission of anxiety diagnoses: long term follow‐up

Comparison 1: CBT versus wait‐list, Outcome 5: Reduction in anxiety symptoms: long term follow‐up

Comparison 1: CBT versus wait‐list, Outcome 6: Sensitivity analysis: Remission of anxiety diagnoses (completers only analysis)

Comparison 2: CBT versus active controls, Outcome 1: Remission of anxiety diagnoses (ITT analysis)

Comparison 2: CBT versus active controls, Outcome 2: Acceptability ‐participants lost to follow‐up

Comparison 2: CBT versus active controls, Outcome 3: Reduction in anxiety symptoms

Comparison 2: CBT versus active controls, Outcome 4: Remission of anxiety diagnoses: long term follow‐up (ITT analysis)

Comparison 2: CBT versus active controls, Outcome 5: Reduction in anxiety symptoms: long term follow‐up

Comparison 2: CBT versus active controls, Outcome 6: Sensitivity analysis: remission of anxiety diagnoses (completers only analysis)

Comparison 3: CBT versus treatment as usual (TAU), Outcome 1: Remission of anxiety diagnoses (ITT analysis)

Comparison 3: CBT versus treatment as usual (TAU), Outcome 2: Acceptability ‐participants lost to follow‐up

Comparison 3: CBT versus treatment as usual (TAU), Outcome 3: Reduction of anxiety symptoms

Comparison 3: CBT versus treatment as usual (TAU), Outcome 4: Sensitivity analysis: remission of anxiety diagnoses (completers only analysis)
| CBT compared to wait‐list for children and adolescents with anxiety disorders | ||||||
| Patient or population: children and adolescents with anxiety disorders | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
|---|---|---|---|---|---|---|
| Assumed risk | Corresponding risk | |||||
| Wait‐list | CBT | |||||
| Remission of anxiety diagnoses (ITT analysis) i.e. no longer meeting criteria for DSM or ICD anxiety diagnosis at the end of the trial. | 161 per 1000 | 600 per 1000 | OR 7.85 | 1350 | ⊕⊕⊕⊝ | |
| Participants lost to follow‐up | 104 per 1000 | 97 per 1000 | OR 0.94 | 1297 | ⊕⊕⊝⊝ | |
| Reduction in anxiety symptoms at the end of the trial | The mean reduction in anxiety symptoms in the intervention groups was | 1394 | ⊕⊕⊝⊝ | SMD ‐0.98 (‐1.21 to ‐0.74) standardised mean difference. [SMD (difference in means/pooled standard deviation) of 0.2 standard deviation units is to be considered a small difference between intervention groups, 0.5 a moderate difference, and 0.8 a large difference (Cohen 1988).] | ||
| Remission of anxiety diagnoses: long‐term follow‐up i.e. no longer meeting criteria for DSM or ICD anxiety diagnosis at the end of the follow‐up study period. | 516 per 1000 | 775 per 1000 | OR 3.22 | 124 | ⊕⊕⊝⊝ | |
| Reduction in anxiety symptoms: long‐term follow‐up, i.e. at the end of the follow‐up study period. | The mean reduction in anxiety symptoms: long‐term follow‐up in the intervention groups was | 186 | ⊕⊕⊝⊝ | SMD ‐1.55 (‐3.20 to 0.10) | ||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence: | ||||||
| 1 Moderate heterogeneity present. | ||||||
| CBT compared to active controls for children and adolescents with anxiety disorders | ||||||
| Patient or population: children and adolescents with anxiety disorders | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
|---|---|---|---|---|---|---|
| Assumed risk | Corresponding risk | |||||
| Active controls | CBT | |||||
| Remission of anxiety diagnoses (ITT) analysis i.e. no longer meeting criteria for DSM or ICD anxiety diagnosis at the end of the trial. | 372 per 1000 | 472 per 1000 | OR 1.51 | 426 | ⊕⊕⊕⊝ | |
| Reduction in anxiety symptoms at the end of the trial | The mean reduction in anxiety symptoms in the intervention groups was | 411 | ⊕⊕⊕⊝ | SMD ‐0.5 (‐1.09 to 0.09) standardised mean difference | ||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence: | ||||||
| 1 Widely differing estimates of the treatment effect. | ||||||
| CBT compared to treatment as usual (TAU) for children and adolescents with anxiety disorders | ||||||
| Patient or population: children and adolescents with anxiety disorders | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
|---|---|---|---|---|---|---|
| Assumed risk | Corresponding risk | |||||
| Treatment as usual (TAU) | CBT | |||||
| Remission of anxiety diagnoses (ITT analysis) i.e. no longer meeting criteria for DSM or ICD anxiety diagnosis at the end of the trial. | 556 per 1000 | 398 per 1000 | OR 0.53 | 88 | ⊕⊕⊕⊝ | |
| Reduction of anxiety symptoms at the end of the trial | The mean reduction in anxiety symptoms in the intervention groups was | 98 | ⊕⊕⊕⊝ | SMD ‐0.19 (‐0.79 to 0.4) standardised mean difference | ||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence: | ||||||
| 1 Small sample size. | ||||||
|
| Number of studies | Mean | Std. Dev. | Min | Max |
| Individual CBT | 7 | 29.14 | 15.75 | 12 | 60 |
| Individual Controls | 7 | 21.57 | 10.71 | 10 | 43 |
| Group CBT | 13 | 24.77 | 14.71 | 6 | 64 |
| Group Controls | 13 | 21.92 | 14.41 | 5 | 67 |
| Family/Parental CBT | 11 | 25 | 13.02 | 6 | 54 |
| Family/Parental Controls | 11 | 17.18 | 6.62 | 5 | 29 |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1.1 Remission of anxiety diagnoses (ITT analysis) Show forest plot | 26 | 1350 | Odds Ratio (IV, Random, 95% CI) | 7.85 [5.31, 11.60] |
| 1.1.1 Individual CBT | 7 | 325 | Odds Ratio (IV, Random, 95% CI) | 7.92 [3.37, 18.63] |
| 1.1.2 Group CBT | 13 | 546 | Odds Ratio (IV, Random, 95% CI) | 7.86 [3.83, 16.12] |
| 1.1.3 Family/Parental CBT | 12 | 479 | Odds Ratio (IV, Random, 95% CI) | 8.65 [5.01, 14.92] |
| 1.2 Acceptability ‐participants lost to follow‐up Show forest plot | 26 | 1321 | Odds Ratio (IV, Random, 95% CI) | 0.94 [0.58, 1.51] |
| 1.3 Reduction in anxiety symptoms Show forest plot | 30 | 1483 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.98 [‐1.21, ‐0.75] |
| 1.3.1 Individual | 8 | 344 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.59 [‐0.82, ‐0.36] |
| 1.3.2 Group | 15 | 608 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.27 [‐1.74, ‐0.80] |
| 1.3.3 Family/Parental | 13 | 531 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.93 [‐1.29, ‐0.56] |
| 1.4 Remission of anxiety diagnoses: long term follow‐up Show forest plot | 3 | 124 | Odds Ratio (IV, Random, 95% CI) | 3.22 [0.96, 10.75] |
| 1.5 Reduction in anxiety symptoms: long term follow‐up Show forest plot | 4 | 186 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.55 [‐3.20, 0.10] |
| 1.6 Sensitivity analysis: Remission of anxiety diagnoses (completers only analysis) Show forest plot | 26 | 1365 | Odds Ratio (IV, Random, 95% CI) | 11.09 [7.47, 16.45] |
| 1.6.1 Individual CBT | 7 | 325 | Odds Ratio (IV, Random, 95% CI) | 11.09 [5.46, 22.56] |
| 1.6.2 Group CBT | 13 | 568 | Odds Ratio (IV, Random, 95% CI) | 11.36 [5.47, 23.59] |
| 1.6.3 Family/Parental CBT | 12 | 472 | Odds Ratio (IV, Random, 95% CI) | 11.35 [6.36, 20.25] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 2.1 Remission of anxiety diagnoses (ITT analysis) Show forest plot | 6 | 426 | Odds Ratio (IV, Random, 95% CI) | 1.51 [0.77, 2.96] |
| 2.2 Acceptability ‐participants lost to follow‐up Show forest plot | 5 | 424 | Odds Ratio (IV, Random, 95% CI) | 0.53 [0.31, 0.91] |
| 2.3 Reduction in anxiety symptoms Show forest plot | 8 | 411 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.50 [‐1.09, 0.09] |
| 2.4 Remission of anxiety diagnoses: long term follow‐up (ITT analysis) Show forest plot | 2 | 273 | Odds Ratio (IV, Random, 95% CI) | 2.03 [1.22, 3.36] |
| 2.5 Reduction in anxiety symptoms: long term follow‐up Show forest plot | 4 | 395 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.91 [‐2.06, 0.24] |
| 2.6 Sensitivity analysis: remission of anxiety diagnoses (completers only analysis) Show forest plot | 5 | 337 | Odds Ratio (IV, Random, 95% CI) | 2.18 [1.31, 3.64] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 3.1 Remission of anxiety diagnoses (ITT analysis) Show forest plot | 2 | 88 | Odds Ratio (IV, Random, 95% CI) | 0.53 [0.23, 1.25] |
| 3.2 Acceptability ‐participants lost to follow‐up Show forest plot | 2 | 90 | Odds Ratio (IV, Random, 95% CI) | 1.01 [0.31, 3.31] |
| 3.3 Reduction of anxiety symptoms Show forest plot | 3 | 98 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.21 [‐0.77, 0.36] |
| 3.4 Sensitivity analysis: remission of anxiety diagnoses (completers only analysis) Show forest plot | 2 | 78 | Odds Ratio (IV, Random, 95% CI) | 1.10 [0.45, 2.68] |

