Agentes antimicrobianos para la prevención de la peritonitis en pacientes con diálisis peritoneal
Resumen
Antecedentes
La diálisis peritoneal (DP) es un tratamiento importante para los pacientes con insuficiencia renal terminal y se utiliza en más de 200 000 de estos pacientes a nivel global. Sin embargo, su valor a menudo está limitado por la aparición de infecciones como la peritonitis y las infecciones del orificio de salida y del túnel. Para reducir el riesgo de peritonitis se han desarrollado estrategias múltiples que incluyen los antibióticos, los desinfectantes tópicos en el orificio de salida y los agentes antimicóticos. Sin embargo, la efectividad de estas estrategias ha sido variable y se basa en un escaso número de ensayos controlados aleatorizados (ECA). Las estrategias preventivas óptimas para reducir la aparición de la peritonitis todavía no están claras.
Ésta es una actualización de una revisión Cochrane publicada por primera vez en 2004.
Objetivos
Evaluar los efectos beneficiosos y perjudiciales de las estrategias antimicrobianas utilizadas para prevenir la peritonitis en los pacientes con DP.
Métodos de búsqueda
Se realizaron búsquedas en el registro especializado del Grupo Cochrane de Riñón y trasplante (Cochrane Kidney and Transplant) hasta el 4 octubre 2016, mediante contacto con el documentalista, utilizando términos de búsqueda relevantes para esta revisión. Los estudios contenidos en el registro especializado se identifican mediante estrategias de búsqueda diseñadas específicamente para CENTRAL, MEDLINE y EMBASE; búsquedas manuales en resúmenes de congresos, y búsquedas en la Plataforma de registros internacionales de ensayos clínicos (ICTRP) y en ClinicalTrials.gov.
Criterios de selección
Se incluyeron los ECA o los ensayos controlados cuasialeatorizados en pacientes que reciben DP crónica, que evaluaran cualquier agente antimicrobiano utilizado de forma sistémica o local para prevenir la peritonitis o la infección del orificio de salida/túnel.
Obtención y análisis de los datos
Dos autores, de forma independiente, evaluaron el riesgo de sesgo y extrajeron los datos. Las estimaciones resumidas del efecto se obtuvieron mediante un modelo de efectos aleatorios y los resultados se expresaron como razón de riesgos (RR) e intervalos de confianza (IC) del 95%.
Resultados principales
Se incluyeron 39 estudios con 4435 pacientes asignados al azar. Se han incluido 20 estudios adicionales en esta actualización. Los dominios de riesgo de sesgo a menudo fueron inciertos o altos; el riesgo de sesgo se consideró bajo en 19 (49%) estudios para la generación de la secuencia aleatoria, en 12 (31%) estudios para la ocultación de la asignación, en 22 (56%) estudios para el informe incompleto de los desenlaces y en 12 (31%) estudios para el informe selectivo de los desenlaces. El cegamiento de los participantes y el personal se consideró con bajo riesgo de sesgo en ocho estudios (21%), así como el cegamiento de los evaluadores de desenlace en diez estudios (26%). Se debe señalar que el cegamiento de los participantes y del personal no fue posible en muchos de los estudios debido a la naturaleza de la intervención o del tratamiento control.
La administración de antibióticos orales o tópicos en comparación con placebo/ningún tratamiento no tuvo efectos claros sobre el riesgo de infección del orificio de salida/túnel (tres estudios, 191 pacientes, evidencia de calidad baja: RR 0,45; IC del 95%: 0,19 a 1,04) ni sobre el riesgo de peritonitis (cinco estudios, 395 pacientes, evidencia de calidad baja: RR 0,82; IC del 95%: 0,57 a 1,19).
La administración de antibióticos nasales en comparación con placebo/ningún tratamiento no tuvo efectos claros sobre el riesgo de infección del orificio de salida/túnel (tres estudios, 338 pacientes, evidencia de calidad baja: RR 1,34; IC del 95%: 0,62 a 2,87) ni sobre el riesgo de peritonitis (tres estudios, 338 pacientes, evidencia de calidad baja: RR 0,94; IC del 95%: 0,67 a 1,31).
La vancomicina intravenosa pre/perioperatoria en comparación con ningún tratamiento podría reducir el riesgo de peritonitis temprana (un estudio, 177 pacientes, evidencia de calidad baja: RR 0,08; IC del 95%: 0,01 a 0,61), pero no tuvo un efecto claro sobre el riesgo de infección del orificio de salida/túnel (un estudio, 177 pacientes, evidencia de calidad baja: RR 0,36; IC del 95%: 0,10 a 1,32).
La administración de desinfectante tópico en comparación con la atención estándar u otro tratamiento activo (antibiótico u otro desinfectante) no tuvo efectos claros sobre el riesgo de infección del orificio de salida/túnel (ocho estudios, 973 pacientes, evidencia de calidad baja, RR 1,00; IC del 95%: 0,75 a 1,33) ni sobre el riesgo de peritonitis (seis estudios, 853 pacientes, evidencia de calidad baja: RR 0,83; IC del 95%: 0,65 a 1,06).
La profilaxis antimicótica con nistatina/fluconazol oral en comparación con placebo/ningún tratamiento podría reducir el riesgo de peritonitis micótica que ocurre después que el paciente ha recibido un ciclo con antibiótico (dos estudios, 817 pacientes, evidencia de calidad baja: RR 0,28; IC del 95%: 0,12 a 0,63).
Ninguna intervención redujo el riesgo de extracción ni de reemplazo del catéter. En su mayoría los estudios disponibles fueron pequeños y de calidad subóptima. Sólo seis estudios incluyeron 200 pacientes o más.
Conclusiones de los autores
En esta actualización se identificaron datos limitados de ECA y ensayos controlados cuasialeatorizados que evaluaron estrategias para prevenir la peritonitis y las infecciones del orificio de salida/túnel. Esta revisión muestra que la vancomicina intravenosa pre/perioperatoria podría reducir el riesgo de peritonitis temprana y que la profilaxis antimicótica con nistatina o fluconazol orales reduce el riesgo de peritonitis micótica posterior a un ciclo con antibiótico. Sin embargo, ninguna otra intervención antimicrobiana tiene una eficacia comprobada. En particular, el uso de antibióticos nasales para erradicar el Staphylococcusaureus, no tuvo un efecto claro sobre el riesgo de peritonitis y plantea interrogantes sobre la utilidad de este enfoque. Debido al gran número de pacientes con DP y a la importancia de la peritonitis, es sorprendente la falta de ECA de alta calidad y con un poder estadístico suficiente para informar la toma de decisiones acerca de las estrategias para prevenir la peritonitis.
PICO
Resumen en términos sencillos
Agentes antimicrobianos para la prevención de la peritonitis en pacientes con diálisis peritoneal
¿Cuál es el problema?
Las personas con insuficiencia renal pueden ser tratadas con diálisis peritoneal, que consiste en insertar un catéter permanente en el peritoneo (revestimiento alrededor del contenido abdominal) a través de la pared abdominal y hacer circular líquido estéril hacia fuera y hacia dentro varias veces al día. La complicación grave más frecuente es la infección del peritoneo, denominada peritonitis. La peritonitis puede ser causada por la transferencia accidental de bacterias desde el catéter.
¿Qué se hizo?
Se buscó en la bibliografía hasta el 4 de octubre de 2016 y se identificaron 39 estudios aleatorizados con 4435 pacientes sometidos a diálisis peritoneal que se evaluaron en esta revisión.
¿Qué se encontró?
Se encontró que la administración de antibióticos cuando se implanta un catéter de diálisis peritoneal podría reducir el riesgo de peritonitis temprana, pero no de infección del orificio de salida/túnel. La profilaxis antimicótica con nistatina o fluconazol orales reduce el riesgo de peritonitis micótica después de un ciclo con antibiótico. Los estudios disponibles proporcionaron evidencia de calidad baja y, por lo tanto, no está claro si hay efectos beneficiosos con la administración de mupirocina nasal o desinfectantes tópicos u otras intervenciones para reducir la infección del orificio de salida/túnel o la peritonitis.
Authors' conclusions
Summary of findings
| Oral or topical or intraperitoneal antibiotics versus placebo/no treatment for preventing peritonitis in peritoneal dialysis patients | ||||||
| Patient or population: patients with CKD on peritoneal dialysis | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Oral or topical or intraperitoneal antibiotics versus placebo/no treatment | |||||
| Peritonitis (number of patients with one or more episodes) | Study population | RR 0.82 | 395 (5) | ⊕⊕⊝⊝ | ||
| 360 per 1000 | 295 per 1000 | |||||
| Moderate | ||||||
| 385 per 1000 | 316 per 1000 | |||||
| Exit‐site/tunnel infection (number of patients with one or more episodes) | Study population | RR 0.45 | 191 (3) | ⊕⊕⊝⊝ | ||
| 176 per 1000 | 79 per 1000 | |||||
| Moderate | ||||||
| 231 per 1000 | 104 per 1000 | |||||
| Catheter removal or replacement (number of patients) | Study population | RR 0.82 | 395 (5) | ⊕⊕⊝⊝ | ||
| 115 per 1000 | 94 per 1000 | |||||
| Moderate | ||||||
| 156 per 1000 | 128 per 1000 | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Unclear or high risk of bias in 3 of 5 studies Abbreviations: CKD ‐ chronic kidney disease; GRADE ‐ Grading of Recommendations Assessment, Development and Evaluation | ||||||
| Nasal antibiotics versus no treatment for preventing peritonitis in peritoneal dialysis patients | ||||||
| Patient or population: patients with CKD on peritoneal dialysis | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No. of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Nasal antibiotics versus placebo/no treatment | |||||
| Peritonitis (number of patients with one or more episodes) | Study population | RR 0.94 | 338 (3) | ⊕⊕⊝⊝ | ||
| 294 per 1000 | 276 per 1000 | |||||
| Moderate | ||||||
| 331 per 1000 | 311 per 1000 | |||||
| Exit‐site/ tunnel infection (number of patients with one or more episodes) | Study population | RR 1.34 | 338 (3) | ⊕⊕⊝⊝ | ||
| 165 per 1000 | 221 per 1000 | |||||
| Moderate | ||||||
| 188 per 1000 | 252 per 1000 | |||||
| Catheter removal or replacement (number of patients) | Study population | RR 0.92 | 289 (2) | ⊕⊕⊝⊝ | ||
| 103 per 1000 | 95 per 1000 | |||||
| Moderate | ||||||
| 265 per 1000 | 244 per 1000 | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio | ||||||
| GRADE Working Group grades of evidence | ||||||
| ¹ Unclear risk of bias for allocation concealment in largest study (Mupirocin Study 1996) Abbreviations: CKD ‐ chronic kidney disease; GRADE ‐ Grading of Recommendations Assessment, Development and Evaluation | ||||||
| Topical disinfectants versus standard care or other active treatment (antibiotic or other disinfectant) for preventing peritonitis in peritoneal dialysis patients | ||||||
| Patient or population: patients with CKD on peritoneal dialysis | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No. of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Topical disinfectants versus standard care or other active treatment (antibiotic or other disinfectant) | |||||
| Peritonitis (number of patients with one or more episodes) | Study population | RR 0.83 | 853 (6) | ⊕⊕⊝⊝ | ||
| 235 per 1000 | 195 per 1000 | |||||
| Moderate | ||||||
| 152 per 1000 | 126 per 1000 | |||||
| Exit‐site/tunnel infection (number of patients with one or more episodes) | Study population | RR 0.97 | 913 (7) | ⊕⊕⊝⊝ | ||
| 238 per 1000 | 230 per 1000 | |||||
| Moderate | ||||||
| 222 per 1000 | 215 per 1000 | |||||
| Catheter removal or replacement (number of patients) | Study population | RR 0.89 | 792 (6) | ⊕⊕⊝⊝ | ||
| 97 per 1000 | 86 per 1000 | |||||
| Moderate | ||||||
| 93 per 1000 | 83 per 1000 | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Unclear allocation in several studies Abbreviations: CKD ‐ chronic kidney disease; GRADE ‐ Grading of Recommendations Assessment, Development and Evaluation | ||||||
| Antifungal versus placebo/no treatment for preventing fungal peritonitis in peritoneal dialysis patients | ||||||
| Patient or population: patients with CKD on peritoneal dialysis | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No. of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Antifungal versus placebo/no treatment | |||||
| Fungal peritonitis (number of patients with one or more episodes) | Study population | RR 0.28 | 817 (2) | ⊕⊕⊝⊝ | ||
| 64 per 1000 | 18 per 1000 | |||||
| Moderate | ||||||
| 64 per 1000 | 18 per 1000 | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 High risk of bias in one study (Lo 1996) Abbreviations: CKD ‐ chronic kidney disease; GRADE ‐ Grading of Recommendations Assessment, Development and Evaluation | ||||||
Background
Peritoneal dialysis (PD) is one of the renal replacement therapies available to people with end‐stage kidney disease (ESKD). There is considerable variation in its use from country to country, with the proportion of total dialysis patients on PD in developed countries ranging from 3.3% (Japan), to 7.0% (USA), 8.3% (Greece), 17.0 % (UK), 36.3% (New Zealand), and up to 79.4% (Hong Kong) (Jain 2012). Because PD and haemodialysis have similar outcomes and patients feel that PD, compared with HD, allows them to live life more fully (Morton 2011), PD should be used more frequently than it is but the perceived risk of peritonitis may prevent this from occurring (Heaf 2004; Piraino 1998).
Description of the condition
Peritonitis due to various organisms(e.g.Staphylococcus aureus, Pseudomonas aeruginosa, coagulase‐negative staphylococci) is a leading complication of PD resulting in technique failure (Woodrow 1997), hospitalisation (Choi 2004; Churchill 1997), peritoneal membrane failure, switching to haemodialysis (Jaar 2009; Piraino 1989) and increased mortality (Annigeri 2001; Digenis 1990; Fried 1996; Piraino 2000). There has been a dramatic reduction in the rates of peritonitis from the start of continuous ambulatory PD (CAPD), but rates above the minimum acceptable peritonitis rate recommended by the International Society for Peritoneal Dialysis (ISPD) of one episode every 33 months (0.36 episodes/year at risk) are still common (Piraino 2011).
Risk factors for peritonitis include older age (Nessim 2009; Oxton 1994; Salusky 1997), depression (Troidle 2003), coexisting diseases such as diabetes (Chow 2005; Ghali 2011) and cardiovascular disease (McDonald 2004; Nolph 1987), obesity (McDonald 2004), connection methodology (Daly 2001), presence of a peritoneal catheter exit‐site infection (Lloyd 2013; van Diepen 2012), and the presence of nasal carriage of S. aureus (Golper 1996; Mupirocin Study 1996; Perez‐Fontan 1993; Schaefer 2003). Race is also an independent risk factor, with African‐American, native Canadian and indigenous Australian Aborigines on PD being shown to be at increased risk (Farias 1994; Fine 1994; Golper 1996; Holley 1993; Lim 2005).
Description of the intervention
Different antimicrobial interventions are used at PD catheter insertion and on an ongoing basis to prevent peritonitis. These include intravenous antibiotics, oral antibiotics, topical antibiotics (Thodis 2000), topical disinfectants, prophylactic treatment of S. aureus nasal carriage primarily with intranasal antibiotic ointment (Piraino 2002), different exit‐site dressing systems and antifungal prophylaxis. All of these strategies, particularly the use of antibiotic at catheter insertion and the cleansing and disinfection of the exit‐site, are widely accepted, but practice patterns are variable and it is not clear which practices have most benefit (Piraino 2011; Van Biesen 2014). Studies on preventing PD‐related infections are limited in number and quality (Piraino 2011). International guidelines differ in their recommendations on preventing PD‐related infections, with some countries not having relevant guidelines (Table 1).
| Guideline | Country | Year | Recommendation |
| Kidney‐Disease Outcomes Quality Initiative | United States of America | NA | No guideline |
| The Renal Association | United Kingdom | April 2008 July 2010 | Guideline 3.1 ‐ PD Access: Implantation Protocol
Guideline 5.1.4 ‐ PD Infectious Complications: Prevention Strategies
Guideline 5.1.5 ‐ PD Infectious Complications: Prevention Strategies
Guideline 5.1.6 ‐ PD Infectious Complications: Prevention Strategies
|
| Canadian Society of Nephrology | Canada | NA | No guideline |
| European Renal Best Practice | Europe | NA | No guideline |
| International Society for Peritoneal Dialysis | NA | July 2010 November 2011 | Guideline 3.1: Implantation Protocol (1A)
Position Statement: Catheter Placement to Prevent Catheter Infections and the Related Peritonitis Episodes
Position Statement: Exit‐Site Care to Prevent Peritonitis
Position Statement: Prevention of Fungal Peritonitis
|
| Kidney Health Australia‐Caring for Australasians with Renal Impairment | Australia/ New Zealand | February 2014 | Guideline 6. Prophylactic Antibiotics for Insertion of PD Catheters
Guideline 8. Treatment of Peritoneal Dialysis‐Associated Fungal Peritonitis
Guideline 10. Prophylaxis for Exit‐site/Tunnel Infections Using Mupirocin
|
MRSA ‐ methicillin‐resistant S. aureus; NA ‐ not applicable; PD ‐ peritoneal dialysis
None of these interventions are free of risks or without cost. Antibiotic prophylaxis carries the risk of gastrointestinal toxicity and may be a cause of antibiotic resistance (Annigeri 2001; Bernardini 1996); it may also be ineffective when patients already have resistance to some antibiotics. Care should be taken that any disinfectant used is at a concentration that is non‐cytotoxic (Piraino 2011).
How the intervention might work
For a patient to be able to successfully use PD as a dialysis therapy, PD‐related infections (exit‐site infections, tunnel infections and peritonitis) need to be avoided. The most important infection is peritonitis and a number of prophylactic strategies have been employed to limit its occurrence. Bacteria are known to be able to gain entry to the peritoneum in a variety of ways and hence, various strategies have been used to prevent this occurring (Campbell 2015).
Oral antibiotics
Oral antibiotics such as rifampin have been given as prophylaxis to PD patients to reduce catheter infections and peritonitis due to S. aureus (Bernardini 1996; Zimmerman 1991). This organism is a major cause of PD catheter infections which can result in S. aureus peritonitis and catheter removal. S. aureus nasal carriage is known to be a significant risk factor for S. aureus PD‐related infections (Bernardini 1996). Cyclic oral rifampin is superior to placebo in preventing S. aureus infections. Other oral antibiotics used include ofloxacin (Sesso 1994), cephalexin (Low 1980), and trimethoprim/sulphamethoxazole (Churchill 1988).
Topical antibiotics
Topical antibiotics such as mupirocin have been applied to the exit site once daily because this antibiotic has good activity against gram‐positive organisms such as staphylococci and streptococci, which are a common cause of exit‐site infection and peritonitis in PD patients (Keane 2000; Troidle 1998; Ward 1986). However, mupirocin is less active against most gram‐negative bacilli and anaerobes (Sutherland 1985). Sodium fusidate ointment (2%) has also been applied to the exit site at one‐month intervals and is known to have activity against staphylococci (Sesso 1994). Gentamicin cream is active against both gram‐positive and gram‐negative organisms and has been used long term on a once‐daily basis at the exit site as prophylaxis for exit‐site infection (Bernardini 2005; Chu 2008). Gentamicin is active against both S. aureus and P. aeruginosa, two important causes of exit‐site infection (Bernardini 2005). Polysporin triple ointment (P3) consists of bacitracin/gramicidin/polymyxin and has bacteriostatic activity against a wide range of skin flora and other organisms including gram‐negative bacteria (MP3 Study 2008).
Nasal antibiotic prophylaxis
Various antibiotic treatments have been trialled in attempts to eliminate S. aureus nasal carriage in PD patients. The nasal carriage of S. aureus is a well‐recognised risk factor for the development of S. aureus infections in CAPD patients (Davies 1989; Luzar 1990; Piraino 1990). Neomycin sulphate ointment has been used prophylactically. Mupirocin has also been used to eliminate nasal S. aureus. While mupirocin is effective at reducing S. aureus nasal carriage rates, re‐colonisation frequently occurs. Sodium fusidate ointment (2%) has also been used and is effective at reducing S. aureus nasal carriage rates (Sesso 1994).
Pre/peri‐operative intravenous antibiotic prophylaxis
The administration of intravenous antibiotics at catheter insertion has been trialled in order to determine if this practice reduces the risk of post‐operative peritonitis or exit‐site infection after PD catheter insertion. Although the insertion of a PD catheter involves "clean surgery involving the placement of a prosthesis or implant", there is the potential for contamination of the peritoneum with micro‐organisms from the patient's own body during surgery. Hence, the giving of a single dose of antibiotic prophylaxis intravenously on starting anaesthesia is recommended (Collier 2008).
Topical disinfectants of the exit site
Topical disinfectants have been applied to the exit site for many years, in an attempt to reduce the bacterial load around the exit site. It has been shown that PD patients with a history of an exit‐site infection have twice the risk of experiencing a peritonitis episode (Canadian CAPD Clinical Trials Group 1989) so it is important to keep the exit‐site infection‐free. Povidone iodine ointment is a broad spectrum antiseptic ointment that has been used and has minimal adverse events associated with its use (Waite 1997). Povidone iodine solution (20g/L) has also been used and shown to successfully reduce the number of exit‐site infections (Luzar 1990). Other antiseptic agents such as hydrogen peroxide, sodium hypochlorite and chlorhexidine have been used (Piraino 2011). The daily use of antibacterial honey at the exit site was trialled in the HONEYPOT Study 2009 This agent was used because it does not induce antimicrobial resistance and has been shown to be active against a broad range of bacteria and fungi (Cho 2014).
Dressing systems for exit sites
A number of exit‐site dressing systems have been devised, all with the aim of reducing exit‐site/tunnel infection and any subsequent peritonitis. The agents used include topical disinfectants and different dressing types and require more or less frequent removal. More frequent removal is seen to risk damaging the skin around the exit site and less frequent removal is felt to possibly encourage the growth of anaerobes. The concentration of topical disinfectants used need to be at non‐cytotoxic levels.
Silver ring system on catheter
The addition of a silver ring device mounted onto the PD catheter was trialled by German researchers in the 1990s (SIPROCE Study 1997). The silver ring was used because of the antimicrobial properties of silver. The use of silver‐coated catheters in animals had shown a reduction in infectious events (Dasgupta 1994; Fung 1996) and offered a non‐pharmaceutical approach to reducing PD catheter‐related infections.
Antistaphylococcal vaccine
An antistaphylococcal vaccine was trialled in the 1990s for the purpose of immunising patients with an anti‐staphylococcal agent. The expectation was that the vaccine would promote a significant increase in the dialysate level of specific antibodies against S. aureus and that this would lead to reduced peritonitis and exit‐site/tunnel infection rates (Poole‐Warren 1991).
Antifungal agents
Antifungal prophylaxis to prevent fungal peritonitis when a PD patient receives an antibiotic course is based on the fact that most episodes of fungal peritonitis are preceded by courses of antibiotics (Piraino 2011). Patients receiving prolonged or repeated antibiotic courses are at increased risk of fungal peritonitis, mostly due to Candida spp. The co‐administration of an oral antifungal agent with an antibiotic course has been trialled to determine if this practice reduces the risk of fungal peritonitis (Lo 1996; Restrepo 2010).
Why it is important to do this review
The aim of this update was to include any new studies of antimicrobial interventions designed to prevent peritonitis in PD patients that have been published since the original review was published in 2004. We also aim to provide a critical appraisal of the current available evidence. As peritonitis is a significant problem for patients using PD, frequently leading to morbidity and technique failure and sometimes to mortality, we have updated the review.
Objectives
To evaluate the benefits and harms of antimicrobial strategies used to prevent peritonitis in PD patients.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled trials (RCTs) and quasi‐RCTs (studies in which allocation to treatment was obtained by alternation, use of alternate medical records, date of birth or other predictable methods) in which antimicrobial interventions designed to prevent peritonitis were compared in patients on PD.
Types of participants
We included adults and children with ESKD who were undergoing PD treatment.
Types of interventions
We included studies involving the use of any antimicrobial agent, whether the interventions were tested between themselves (head‐to‐head) or against placebo/no treatment. The inclusion criteria have been expanded in this update, with the intervention "oral antibiotics" becoming "oral or topical or intraperitoneal antibiotics" and with the interventions "dressing systems for exit sites" and "silver ring system on catheter" being added.
Specifically, the following antimicrobial interventions were analysed.
-
Oral or topical or intraperitoneal antibiotics
-
Nasal antibiotic prophylaxis (mupirocin, rifampicin, other)
-
Pre/peri‐operative intravenous antibiotic prophylaxis
-
Topical disinfectants of the exit‐site (povidone‐iodine, chlorhexidine, triclosan, soap and water, other)
-
Germicidal systems for connection devices
-
Dressing systems for exit sites
-
Silver ring system on catheter
-
Antistaphylococcal vaccine
-
Antifungal agents
Types of outcome measures
-
Peritonitis‐number of patients with peritonitis and peritonitis rate (peritonitis defined as dialysate count of > 100 cells/mm3 with > 50% being polymorphonuclear leukocytes; peritonitis rate defined as number of episodes of peritonitis over total patient months on PD)
-
Peritonitis relapse (reoccurrence of peritonitis due to the same organism within two to four weeks)
-
Death due to peritonitis
-
All‐cause mortality
-
Exit‐site and tunnel infection‐number of patients with exit‐site and tunnel infections and exit‐site and tunnel infection rate
-
Catheter removal/catheter replacement
-
Technique failure (transfer from PD to haemodialysis/transplant due to peritonitis)
-
Toxicity of antimicrobial treatments (nasal irritation, sneezing, generalised pruritus, headache, diarrhoea, nausea, vomiting, jaundice, local irritation, rash)
-
Time to first peritonitis episode
Primary outcomes
-
Peritonitis
-
Exit‐site infection/tunnel infection
-
Catheter removal/catheter replacement
Secondary outcomes
-
Peritonitis relapse
-
Death due to peritonitis
-
All‐cause mortality
-
Technique failure
-
Toxicity of antimicrobial treatments
-
Time to first peritonitis episode
Search methods for identification of studies
Electronic searches
We searched the Cochrane Kidney and Transplant Specialised Register to 4 October 2016 through contact with the Information Specialist using search terms relevant to this review. The Cochrane Kidney and Transplant Specialised Register contains studies identified from the following sources.
-
Monthly searches of the Cochrane Central Register of Controlled Trials CENTRAL
-
Weekly searches of MEDLINE OVID SP
-
Handsearching of kidney‐related journals & the proceedings of major kidney conferences
-
Searching of the current year of EMBASE OVID SP
-
Weekly current awareness alerts for selected kidney journals
-
Searches of the International Clinical Trials Register (ICTRP) Search Portal & ClinicalTrials.gov.
Studies contained in the Specialised Register are identified through search strategies for CENTRAL, MEDLINE, and EMBASE based on the scope of Cochrane Kidney and Transplant. Details of these strategies, as well as a list of handsearched journals, conference proceedings and current awareness alerts, are available in the Specialised Register section of information about Cochrane Kidney and Transplant.
See Appendix 1 for search terms used in strategies for this review.
Searching other resources
-
Reference lists of review articles, relevant studies and clinical practice guidelines.
-
Letters seeking information about unpublished or incomplete studies to investigators known to be involved in previous studies.
Data collection and analysis
Selection of studies
The search strategy described was used to obtain titles and abstracts of studies that were potentially relevant to the review. The titles and abstracts were screened independently by two authors, who discarded studies that were not applicable. However, studies and reviews that might include relevant data or information on studies were retained initially. Two authors independently assessed retrieved abstracts and where necessary, the full text of these studies, to determine which satisfied the inclusion criteria.
Data extraction and management
Data extraction and assessment of the risk of bias were performed independently by the same authors using standardised data extraction forms. Studies reported in non‐English language journals were translated before assessment. Where more than one publication of one study existed, reports were grouped together and the publication with the most complete data was used in the analyses. Where relevant outcomes were only published in earlier versions, these data were used. Any discrepancy between published versions was highlighted. Any further information required from the original author was requested by written correspondence and any relevant information obtained in this manner was included in the review.
Assessment of risk of bias in included studies
The following items were assessed using the risk of bias assessment tool (Higgins 2011) (see Appendix 2).
-
Was there adequate sequence generation (selection bias)?
-
Was allocation adequately concealed (selection bias)?
-
Was knowledge of the allocated interventions adequately prevented during the study?
-
Participants and personnel (performance bias)
-
Outcome assessors (detection bias)
-
-
Were incomplete outcome data adequately addressed (attrition bias)?
-
Are reports of the study free of suggestion of selective outcome reporting (reporting bias)?
-
Was the study apparently free of other problems that could put it at a risk of bias?
Measures of treatment effect
For dichotomous outcomes (peritonitis (number), peritonitis (rate), death due to peritonitis, all‐cause mortality, exit‐site/tunnel infection (number), exit‐site/tunnel infection (rate), catheter removal/replacement, technique failure, toxicity of antimicrobial treatments) results were expressed as risk ratios (RR) with 95% confidence intervals (CI). No continuous outcomes were identified.
Unit of analysis issues
Where data on the number of subjects with events (e.g. number of subjects with one or more episodes of peritonitis) were available, the RR was calculated as the ratio of the incidence of the event (one or more episodes) in the experimental treatment group over the incidence in the control group. Where data on the number of episodes were available the RR was calculated as the ratio of the rate of the outcome (e.g. the peritonitis rate) in the experimental treatment group (given by number of episodes of the outcome over total patient months on PD) over the rate in the control group.
Dealing with missing data
Where necessary, we contacted triallists to request missing patient data due to loss to follow‐up and exclusion from study analyses in an effort to conduct intention‐to‐treat analyses. With the update, four authors responded to our requests. Where missing dichotomous data were few, and unlikely to affect the overall results, we analysed available data.
Assessment of heterogeneity
Heterogeneity was analysed using a Chi2 test on N‐1 degrees of freedom, with an alpha of 0.05 used for statistical significance and with the I2 test (Higgins 2003). I2 values of 25%, 50% and 75% correspond to low, medium and high levels of heterogeneity.
Assessment of reporting biases
The search strategy included searching major databases, conference proceedings and prospective trial registers without language restriction in an attempt to reduce publication bias related to failure of authors to publish negative results or inability to publish negative results in journals indexed in major databases. Insufficient studies were available to assess for publication bias using funnel plots. Where multiple publications of the same study were identified, data were included from the most recent publication, and preferably, the definitive publication. However, all publications were reviewed to identify outcomes not reported in the index publication in an attempt to reduce outcome reporting bias.
Data synthesis
Data were pooled using the random‐effects model for dichotomous data.
Subgroup analysis and investigation of heterogeneity
Subgroup analysis was planned to explore potential sources of variability in observed treatment effect where possible (paediatric versus adult population, diabetic versus non‐diabetic, time on PD before beginning of antimicrobial treatment). However, no subgroup analyses were performed due to lack of available data from the included studies.
Sensitivity analysis
Sensitivity analysis was planned to investigate the effect of year of study and study performance. However, there were insufficient studies to do this.
Summarising and interpreting results
We used the GRADE approach to assess the quality of evidence for each of the key outcomes (Guyatt 2008). We used the GRADE profiler to create 'Summary of Findings' tables (Schünemann 2011a).
For assessments of the overall quality of evidence for each outcome that included pooled data from RCTs, we downgraded the evidence from 'high quality' by one level for serious study limitations and by two levels for very serious study limitations. The evidence was appraised using the five GRADE considerations: risk of bias, imprecision of effect estimates, inconsistency, indirectness and potential publication bias. None were upgraded to moderate or high quality as most pooled estimates did not reveal a large magnitude of effect, there was potential for impact by confounders, and most did not show a strong dose‐response gradient (Schünemann 2011b). The exception was the pooled estimate obtained for the comparison of the use of an antifungal agent versus placebo/no treatment for preventing fungal peritonitis, but the evidence was not upgraded from 'low' because only two studies contributed data for the outcome of fungal peritonitis and one of the studies had a high risk of bias. We used these assessments and the evidence for absolute benefit or harm of the interventions and the sum of available data on all important outcomes from each study included for each comparison, to arrive at conclusions about the effectiveness of antimicrobial agents at preventing catheter‐related infection or the need for catheter removal/replacement in PD patients.
'Summary of Findings' tables consisted of the following clinically important outcomes identified in the selected studies:
-
Peritonitis (number of patients with one or more episodes)
-
Exit‐site/tunnel infection (number of patients with one or more episodes)
-
Catheter removal or replacement (number of patients)
-
Fungal peritonitis (number of patients with one or more episodes).
Results
Description of studies
See: Characteristics of included studies; Characteristics of excluded studies; Characteristics of ongoing studies.
Results of the search
For this update we searched the Specialised Register to 4 October 2016 and identified 48 new reports. After full‐text assessment 31 new studies were identified. Twenty new studies (33 reports) were included, 10 were excluded (14 reports), and one ongoing study was identified. We also identified four new reports of four existing included studies. Search results are shown in Figure 1.

Study flow diagram.
Included studies
We included 39 studies in the review, 19 of which had been included in the original review. Of the 20 new studies, 10 had been published since the search was done for the previous review and 10 (Axelrod 1973; Cheng 1999a; Cocksedge 1993; Fuchs 1990; Moore 1989; Ryckelynck 1987; Sharma 1971; SIPROCE Study 1997; Wadhwa 1995; Wadhwa 1997) had not been identified in the previous search. There was one four‐arm study (Swartz 1991), three three‐arm studies (Fuchs 1990; Gadallah 2000c; Sesso 1994), and the remaining studies were two‐arm studies. No cross‐over studies were identified.
Of the 39 studies included (4435 randomised participants), all were parallel group studies. All participants were chronic PD patients treated in‐centre or in satellite facilities. Two studies (Axelrod 1973; Sharma 1971) reported the number of dialyses but not the number of participants in each group and hence, the data from these studies could not be added to the meta‐analyses. Most studies included only adult patients; two studies (Blowey 1994; Mendoza‐Guevara 2007) included only children and young adults on PD. Twenty‐six studies (Bernardini 2005; Bernardini 1996; Chu 2008; Cocksedge 1993; Fuchs 1990; Gadallah 2000c; HONEYPOT Study 2009; Lo 1996; Luzar 1990; Lye 1992; MP3 Study 2008; Mupirocin Study 1996; Nolph 1985; Nunez‐Moral 2014; Perez‐Fontan 1992; Poole‐Warren 1991; Restrepo 2010; Sesso 1994; SIPROCE Study 1997; Swartz 1991; Wadhwa 1995; Wadhwa 1997; Waite 1997; Wikdahl 1997; Wong 2003; Zimmerman 1991) identified the proportion of patients who had diabetes mellitus.
Most studies reported only some of the primary outcomes of interest to this review. The primary outcomes reported in the studies were as follows: peritonitis ‐ number of patients (22 studies), peritonitis rate (14 studies), exit‐site/tunnel infection ‐ number of patients (22 studies), exit‐site/tunnel infection ‐ rate (12 studies) and catheter removal/replacement (15 studies). Other outcomes reported included death due to peritonitis (2 studies), all‐cause mortality (13 studies), technique failure (3 studies) and toxicity of antimicrobial treatments (5 studies). No studies had data on peritonitis relapse and only two had time to first peritonitis episode (HONEYPOT Study 2009; MP3 Study 2008).
Three study authors responded to queries about study methods and/or requests for additional unpublished information (Chu 2008; Danguilan 2003; HONEYPOT Study 2009).
Oral or topical antibiotics versus placebo/no treatment
In seven studies (469 participants), patients were randomised to oral, or topical (exit site, nasal) or intraperitoneal prophylactic antibiotics versus placebo or no treatment (Blowey 1994; Churchill 1988; Low 1980; Sesso 1994; Swartz 1991; Wong 2003; Zimmerman 1991). The duration of follow‐up ranged from one to 12 months.
Oral or topical antibiotics versus other antibiotic
Seven studies (640 participants) randomised patients to oral, or topical (exit site, nasal) or intraperitoneal antibiotics versus other antibiotics (Bernardini 1996; Bernardini 2005; Chu 2008; Danguilan 2003; MP3 Study 2008; Perez‐Fontan 1992; Sesso 1994) with follow‐up ranging from 7.8 to 18 months.
Nasal antibiotic prophylaxis versus placebo/no treatment
Three studies (338 participants) compared the use of nasal prophylactic antibiotics with placebo (Mupirocin Study 1996; Sesso 1994; Sit 2007). The duration of follow‐up ranged from 7.8 to 18 months.
Pre/peri‐operative antibiotic prophylaxis versus placebo/no treatment or other antibiotic
One study (178 participants) assessed the use of vancomycin with cefazolin as perioperative intravenous prophylaxis head‐to‐head (Gadallah 2000c), and four studies (379 patients) compared the use of perioperative intravenous antibiotic prophylaxis against no antibiotic treatment (Bennet‐Jones 1988; Gadallah 2000c; Lye 1992; Wikdahl 1997). Follow‐up periods ranged from 10 to 28 days.
Topical disinfectants versus standard care or other active treatment (antibiotic or other disinfectant)
Nine studies (1039 participants) evaluated the effect of topical disinfectants versus standard care or other intervention at the exit site on a range of outcomes (Cheng 1999a; HONEYPOT Study 2009; Luzar 1990; Mendoza‐Guevara 2007; Nunez‐Moral 2014; Wadhwa 1995; Wadhwa 1997; Waite 1997; Wilson 1997). The duration of follow‐up ranged from 6 to 24 months.
Other interventions
Other interventions included one study (167 participants) which compared the use of an ultraviolet germicidal chamber to disinfect the spike and the solution bag outlet port versus no treatment (Nolph 1985) while another study (50 participants) directed one group to soak their connectors in antiseptic before performing a bag exchange while the control group did not use antiseptic (Ryckelynck 1987). Three studies (140 participants) compared different dressing systems (Cocksedge 1993; Fuchs 1990; Moore 1989) and one study (195 participants) compared the addition of a silver ring device on the catheter versus no ring (SIPROCE Study 1997). One study (124 participants) compared the antistaphylococcal vaccine Staphypan Berna against placebo (Poole‐Warren 1991).
Antifungal prophylaxis versus placebo/no treatment interventions
Two studies (817 participants) compared the administration of an antifungal agent with an antibiotic course against no treatment (Lo 1996; Restrepo 2010). Follow‐up periods ranged from 1 to 18 months.
See Table 2 for comparisons included in Strippoli 2004a and this 2017 update.
| Comparisons in 2004 review | Comparisons in 2017 review |
| Oral antibiotics versus none | Oral or topical antibiotics versus placebo/no treatment |
| Nasal antibiotics versus none | Oral or topical antibiotics versus other antibiotic |
| Peri‐operative IV prophylaxis versus none | Nasal antibiotics versus no treatment |
| Peri‐operative IV prophylaxis head‐to‐head | Pre/peri‐operative IV prophylaxis versus none or head‐to‐head |
| Topical disinfectants versus none | Topical disinfectants versus standard care or other active treatment (antibiotic or other disinfectant) |
| Germicidal chamber versus none | Germicidal chamber versus none |
| Antistaphylococcal vaccine (Staphypan) versus placebo | Dressing systems (any) |
| Antibiotic prophylaxis head‐to‐head agents | Silver ring system on catheter versus none |
| ‐‐ | Antistaphylococcal vaccine (Staphypan) versus placebo |
| ‐‐ | Antifungal versus placebo/no treatment |
Excluded studies
Twelve studies (17 reports) were excluded after full text review. The characteristics of the excluded studies are shown in "Characteristics of excluded studies". Reasons for excluding studies included focus of study was about treatment of PD‐related infection not prevention, report was of a pharmacokinetics study, agent used in intervention was not an antimicrobial, and PD‐related infection data was not readily available in the published report.
Risk of bias in included studies
The assessment of risk of bias is shown in Figure 2 and Figure 3. Figure 2 shows relative proportional rankings of studies for each risk of bias indicator. Figure 3 shows the risk of bias items for individual studies.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Randomisation of sequence generation was judged to be at low risk of bias in 19 studies (Axelrod 1973; Bennet‐Jones 1988; Bernardini 2005; Churchill 1988; HONEYPOT Study 2009; Low 1980; Luzar 1990; Mendoza‐Guevara 2007; MP3 Study 2008; Nolph 1985; Nunez‐Moral 2014; Perez‐Fontan 1992; Restrepo 2010; SIPROCE Study 1997; Sit 2007; Swartz 1991; Waite 1997; Wilson 1997; Zimmerman 1991). Randomisation method was unclear in 15 studies and was judged to be at high risk of bias in five studies (Chu 2008; Gadallah 2000c; Lo 1996; Lye 1992; Moore 1989).
Twelve studies reported allocation concealment adequately (Axelrod 1973; Bennet‐Jones 1988; Bernardini 2005; Churchill 1988; HONEYPOT Study 2009; Low 1980; Luzar 1990; MP3 Study 2008; Nolph 1985; Poole‐Warren 1991; Sharma 1971; SIPROCE Study 1997). Allocation concealment was unclear in 21 studies and six studies were judged to be at high risk of bias (Chu 2008; Gadallah 2000c; Lo 1996; Lye 1992; Moore 1989; Wikdahl 1997).
Blinding
Performance bias (blinding of participants and investigators) was judged to be at low risk of bias in eight studies (Axelrod 1973; Bennet‐Jones 1988; Bernardini 2005; Churchill 1988; Low 1980; MP3 Study 2008; Poole‐Warren 1991; Sharma 1971), was unclear in 15 studies, and was judged to be a high risk of bias in 16 studies (Bernardini 1996; Blowey 1994; Cheng 1999a; Chu 2008; Cocksedge 1993; Danguilan 2003; Fuchs 1990; Gadallah 2000c; HONEYPOT Study 2009; Lo 1996; Luzar 1990; Lye 1992; Moore 1989; Nolph 1985; SIPROCE Study 1997; Zimmerman 1991).
Detection bias (blinding of outcome assessors) was judged to be at low risk of bias in 10 studies (Axelrod 1973; Bennet‐Jones 1988; Bernardini 2005; Churchill 1988; Low 1980; Mendoza‐Guevara 2007; MP3 Study 2008; Poole‐Warren 1991; Sharma 1971; Waite 1997), was unclear in 13 studies, and was judged to be at high risk of bias in 16 studies (Bernardini 1996; Blowey 1994; Cheng 1999a; Chu 2008; Cocksedge 1993; Danguilan 2003; Fuchs 1990; Gadallah 2000c; HONEYPOT Study 2009; Lo 1996; Luzar 1990; Lye 1992; Moore 1989; Nolph 1985; SIPROCE Study 1997; Zimmerman 1991).
Incomplete outcome data
Outcomes data reporting was considered to be complete with a low risk of bias in 22 studies (Bennet‐Jones 1988; Bernardini 1996; Bernardini 2005; Blowey 1994; Churchill 1988; Fuchs 1990; Gadallah 2000c; Lo 1996; Low 1980; Luzar 1990; Lye 1992; MP3 Study 2008; Mupirocin Study 1996; Nunez‐Moral 2014; Perez‐Fontan 1992; Poole‐Warren 1991; Sit 2007; Swartz 1991; Waite 1997; Wikdahl 1997; Wilson 1997; Wong 2003). Eight studies (Axelrod 1973; Chu 2008; Danguilan 2003; HONEYPOT Study 2009; Nolph 1985; Sesso 1994; SIPROCE Study 1997; Zimmerman 1991) reported that from 9.2% to 77.7% of patients were excluded from analyses, so were considered to be at high risk of bias. The risk of bias was unclear in nine studies because there was insufficient information provided to determine if data from all patients who entered the study were included in the analysis.
Selective reporting
We identified 12 studies (Bernardini 2005; HONEYPOT Study 2009; Lye 1992; MP3 Study 2008; Mupirocin Study 1996; Poole‐Warren 1991; Sesso 1994; SIPROCE Study 1997; Wadhwa 1995; Wadhwa 1997; Wilson 1997; Wong 2003) and reported all outcomes based on the protocols described in the study methods and could be meta‐analysed. Twelve studies were judged to be at high risk of bias of reporting bias (Axelrod 1973; Bennet‐Jones 1988; Churchill 1988; Cocksedge 1993; Fuchs 1990; Lo 1996; Mendoza‐Guevara 2007; Moore 1989; Nolph 1985; Ryckelynck 1987; Sharma 1971; Swartz 1991) because only one our primary outcomes cold be meta‐analysed; two studies reported outcomes incompletely so they could not be included in any of our meta‐analyses (Axelrod 1973; Sharma 1971). Reporting bias was unclear for 15 studies because only two (of our three) primary outcomes were reported or could be meta‐analysed.
Other potential sources of bias
Eight studies (Axelrod 1973; Churchill 1988; Luzar 1990; Mupirocin Study 1996; Nolph 1985; Poole‐Warren 1991; SIPROCE Study 1997; Waite 1997; Zimmerman 1991) reported receiving monetary support from pharmaceutical companies; one study received combined funding from industry and government (HONEYPOT Study 2009) and was judged to at unclear risk of bias. Four studies were judged to be at low risk bias (Bernardini 2005; Low 1980; MP3 Study 2008; Sesso 1994) and the remaining 26 studies were judged unclear.
Effects of interventions
See: Summary of findings for the main comparison Oral or topical or intraperitoneal antibiotics versus placebo/no treatment for preventing peritonitis in peritoneal dialysis patients; Summary of findings 2 Nasal antibiotics versus placebo/no treatment for preventing peritonitis in peritoneal dialysis patients; Summary of findings 3 Topical disinfectants versus standard care or other active treatment (antibiotic or other disinfectant) for preventing peritonitis in peritoneal dialysis patients; Summary of findings 4 Antifungal versus placebo/no treatment for preventing peritonitis in peritoneal dialysis patients
See: summary of findings Table for the main comparison: Oral or topical or intraperitoneal antibiotics versus placebo/no treatment for preventing peritonitis in PD patients; summary of findings Table 2: Nasal antibiotics versus no treatment for preventing peritonitis in PD patients; summary of findings Table 3: Topical disinfectants versus standard care or other active treatment (antibiotic or other disinfectant) for preventing peritonitis in PD patients; summary of findings Table 4: Antifungal versus placebo/no treatment for preventing fungal peritonitis in PD patients.
In most studies, the primary outcomes were peritonitis (number of patients), peritonitis rate, exit‐site/tunnel infection (number of patients), exit‐site/tunnel infection rate, and catheter removal or replacement (number). Many studies only included one or two of these outcomes. Other outcomes included all‐cause mortality, time to first catheter‐related infection, hospitalisation, death due to catheter‐related infection, technique failure, local pruritus/rash, and toxicity.
Oral or topical antibiotics versus placebo or no treatment
The oral antibiotic used was ofloxacin, cephalexin, rifampin or cotrimoxazole, and the topical antibiotic used was mupirocin ointment (exit site, nasal).
The use of oral or topical antibiotic prophylaxis had uncertain effects on the risk of peritonitis (Analysis 1.1 (5 studies, 395 participants): RR 0.82, 95% CI 0.57 to 1.19). There was low to moderate heterogeneity across these studies (I2 = 33%). The risk of peritonitis outcome was assessed as low quality because of unclear or high risk of bias in 3 of 5 studies and because of wide confidence intervals in all 5 studies due to small patient numbers.
The two interventions also had uncertain effects on the peritonitis rate (Analysis 1.2.1 (3 studies, 1440 patient‐months): RR 0.68, 95% CI 0.40 to 1.14), the risk of exit‐site and tunnel infection (Analysis 1.3.1 (3 studies, 191 participants): RR 0.45, 95% CI 0.19 to 1.04), exit‐site/tunnel infection rate (Analysis 1.4.1 (2 studies, 939 patient‐months): RR 0.42, 95% CI 0.17 to 1.05), risk of catheter removal or replacement (Analysis 1.5.1 (5 studies, 395 participants): RR 0.82, 95% CI 0.46 to 1.46), and all‐cause mortality (Analysis 1.6.1 (4 studies, 201 participants): RR 0.88, 95% CI 0.41 to 1.89), with no significant heterogeneity across studies for any of these analyses (I2 = 0%).
The risk of exit‐site/tunnel infection outcome was assessed as low quality because of unclear or high risk of bias in all 3 studies and because of wide confidence intervals in all 3 studies due to small patient numbers. The risk of catheter removal/replacement outcome was also assessed as low quality because of unclear or high risk of bias in 3 of 5 studies and because of wide confidence intervals in all 5 studies due to small patient numbers.
Oral or topical antibiotics versus other antibiotic
The use of antibiotic ointment prophylaxis (either sodium fusidate (exit site plus nasal) or mupirocin (exit site)) was compared with another antibiotic (oral ofloxacin, oral rifampin or gentamicin cream (exit site)) in four studies.
The interventions had uncertain effects on the risk of peritonitis (Analysis 2.1 (4 studies, 314 participants): RR 1.28, 95% CI 0.89 to 1.84). There was low heterogeneity across these studies (I2 = 9%). Similarly, topical antibiotic prophylaxis (either mupirocin ointment (exit site), sodium fusidate ointment (exit site plus nasal) or mupirocin cream (exit site)) compared with other antibiotic (either sodium fusidate ointment (exit site), oral ofloxacin or gentamicin cream (exit site)) had uncertain effects on the risk of exit‐site and tunnel infection (Analysis 2.3 (4 studies, 336 participants): RR 1.28, 95% CI 0.71 to 2.31). There was medium heterogeneity across these studies (I2 = 56%).
Nasal antibiotic prophylaxis versus placebo or no treatment
The use of nasal antibiotic prophylaxis had uncertain effects on the risk of peritonitis (Analysis 3.1 (3 studies, 338 participants): RR 0.94, 95% CI 0.67 to 1.31), the peritonitis rate (Analysis 3.2 (2 studies, 2797 patient‐months): RR 0.67, 95% CI 0.16 to 2.77), the risk of exit‐site and tunnel infection (Analysis 3.3 (3 studies, 338 participants): RR 1.34, 95% CI 0.62 to 2.87), the exit‐site and tunnel infection rate (Analysis 3.4 (2 studies, 2796 patient‐months): RR 0.91, 95% CI 0.29 to 2.92), and the number of patients with catheter removal or replacement (Analysis 3.5 (2 studies, 289 participants): RR 0.92, 95% CI 0.48 to 1.78). There was no significant heterogeneity across the studies for any of these analyses. Although in 1 study, there was a significant reduction in the exit‐site/tunnel infection rate when CAPD patients identified as S. aureus carriers (nasal) were treated with mupirocin ointment (nasal application, twice/day for 5 days, every 1 month), there were no significant differences with any of the other primary outcomes of interest (Mupirocin Study 1996).
The risk of peritonitis and the risk of exit‐site/tunnel infection outcomes were assessed as low quality because of unclear or high risk of bias in all 3 studies and because of wide confidence intervals in all 3 studies due to small patient numbers. The risk of catheter removal/replacement was assessed as low quality because of unclear to high risk of bias in the 2 studies and because of wide confidence intervals in the 2 studies due to small patient numbers.
Pre‐ or peri‐operative antibiotic prophylaxis versus placebo or no treatment or other antibiotic
Pre‐ or peri‐operative intravenous antibiotic prophylaxis compared with no treatment may reduce the risk of early peritonitis (less than one month from catheter insertion) in one study (Gadallah 2000c) but there was no difference between the interventions in three other studies using different antibiotics (Analysis 4.1 (4 studies, 379 participants). The single 3‐arm study (Gadallah 2000c) compared vancomycin with placebo, cefazolin with placebo and vancomycin with cefazolin and found the risk of peritonitis was reduced by vancomycin compared with placebo (Analysis 4.1.1 (1 study, 177 participants): RR 0.08. 95% CI 0.01 to 0.61) and by vancomycin compared with cefazolin (Analysis 4.1.6 (1 study, 178 participants): RR 0.11, 95% CI 0.01 to 0.84); there was no difference between cefazolin compared with placebo. None of the antibiotic interventions made a difference to the risk of exit‐site and tunnel infection (Analysis 4.2 (4 studies, 379 participants). When outcomes at more than one month after catheter insertion were considered, there was no difference between the interventions for the risk of peritonitis or exit‐site/tunnel infection.
Because each study used a different antibiotic intervention, it is not possible to comment on heterogeneity across the studies.
Topical disinfectants versus standard care or other active treatment (antibiotic or other disinfectant)
Eight studies reported on the use of disinfectant at the exit site versus standard care or other active treatment. As the test for subgroup differences was not significant for any of our outcomes the total summary estimates are reported here.
Overall topical disinfectants versus standard care or other active treatment had uncertain effects on the risk of peritonitis (Analysis 5.1 (6 studies, 853 participants): RR 0.83, 95% CI 0.65 to 1.06). exit‐site/tunnel infection (Analysis 5.2 (8 studies, 973 participants): RR 1.00, 95% CI 0.75 to 1.33), catheter removal or replacement (Analysis 5.4 (7 studies, 852 participants): RR 0.89, 95% CI 0.57 to 1.38), and all‐cause mortality (Analysis 5.5 (4 studies, 697 participants): RR 0.88, 95% CI 0.53 to 1.44), with no significant heterogeneity across studies for any of these analyses.
The risk of peritonitis outcome was assessed as low quality because of unclear allocation concealment and blinding in four of six studies and imprecision due to the small number of patients and events in five of six studies. The risk of exit‐site/tunnel infection outcome was assessed as low quality because of unclear allocation concealment and blinding in six of eight studies and imprecision due to the small number of patients and events in seven of eight studies. The risk of catheter removal/replacement outcome was assessed as low quality because of unclear allocation concealment and blinding in five of seven studies and imprecision due to the small number of patients and events in six of seven studies.
Other interventions
Seven studies reported on other interventions designed to reduce PD‐related infections. There was no difference in the peritonitis rate with other interventions.
-
Germicidal chamber for connection devices or soaking of the connector in antiseptic prior to bag exchange versus none (Analysis 6.1 (2 studies, 1855 patient‐months): RR 1.05, 95% CI 0.74 to 1.51)
-
Staphypan Berna antistaphylococcal vaccine (Analysis 9.1 (1 study, 1099 patient‐months): RR 1.11, 95% CI 0.77 to 1.59). Staphypan Berna compared with placebo was also shown to make no difference to the exit‐site and tunnel infection rate (Analysis 9.2 (1 study, 1107 patient‐months): RR 0.98, 95% CI 0.65 to 1.48).
Three studies (140 participants) reported on the use of different dressing systems. There was no difference between the comparisons for the number of patients with one or more episodes of exit‐site/tunnel infection (Analysis 7.1) or the exit‐site/tunnel infection rate (Analysis 7.2 (1 study, 679 patient‐months).
There was no difference between use of a silver ring on the PD catheter versus none for the risk of peritonitis (Analysis 8.1 (1 study, 195 participants): RR 0.90, 95% CI 0.49 to 1.66), risk of exit‐site/tunnel infection (Analysis 8.2 (1 study, 195 participants): RR 1.26, 95% CI 0.84 to 1.90) or risk of catheter removal/replacement (Analysis 8.3 (1 study, 195 participants): RR 1.26, 95% CI 0.35 to 4.56).
Antifungal prophylaxis versus placebo or no treatment
The use of antifungal agents (oral fluconazole or oral nystatin) compared with no antifungal agent being given when a patient receives a course of antibiotics for bacterial peritonitis were reported in 2 studies. The antifungal intervention may reduce the risk of fungal peritonitis (Analysis 10.1 (2 studies, 817 participants): RR 0.28, 95% CI 0.12 to 0.63). There was low heterogeneity across the two studies for this analysis. The risk of fungal peritonitis outcome was assessed as low quality because of unclear risk of bias in 1 study and high risk of bias in 1 study and imprecision due to the small number of events and patient numbers. One study of oral nystatin in PD patients who were receiving treatment for bacterial peritonitis showed a significant reduction in the rate of fungal peritonitis due to Candida spp. with nystatin prophylaxis (Analysis 10.2 (1 study, 6864 patient‐months): RR 0.31, 95% CI 0.10 to 0.95).
Adverse effects
For the comparisons which included oral or topical antibiotics versus placebo/no treatment, two studies (86 participants) provided some information on adverse effects of therapy. They were reported in relation to the use of oral rifampin and sodium fusidate ointment (nasal and exit site). More patients reported adverse effects with oral rifampin therapy but the results did not achieve significance. Heterogeneity could not be determined (Analysis 1.8).
For the studies which included oral or topical antibiotics versus other antibiotic, three studies (419 participants) reported on adverse effects of therapy. The antibiotics used were applied daily/routinely to the exit site and included Polysporin triple ointment, gentamicin cream and cyclic oral rifampin against mupirocin ointment or cream. There were fewer patients who reported adverse effects with mupirocin but the result was not significantly different; nausea (Analysis 2.8.1 (1 study, 82 participants): RR 0.09, 95% CI 0.01 to 1.59); pruritus (Analysis 2.8.2 (2 studies, 337 participants): RR 0.65, 95% CI 0.29 to 1.49).
Three studies (289 participants) compared nasal antibiotics against placebo/no treatment and two of them reported information on adverse effects of therapy. The antibiotics used included mupirocin ointment (nasal) and sodium fusidate ointment (nasal and exit site) versus placebo ointment (nasal) or placebo tablets. More patients reported adverse effects with the antibiotic treatments (headache, diarrhoea, nausea, vomiting, pruritus, nasal irritation/rhinitis) but the results did not achieve significance. Heterogeneity could not be determined (Analysis 3.7).
For the studies which included topical disinfectant versus standard care or other active treatment at the exit site, four studies reported on adverse effects of therapy. The interventions that these reports related to were sodium hypochlorite solution, antibacterial honey and povidone iodine dry powder spray against povidone iodine solution, mupirocin ointment (nasal) or alcohol wipes. More patients reported adverse effects with use of the former agents and a statistically significant increase in pruritus occurred with topical disinfectants versus standard care (Analysis 5.7 (4 studies, 609 participants): RR 2.80, 95% CI 1.21 to 6.48; I2 = 44%). There was low heterogeneity of results.
Antibiotic resistance was not adequately reported in the included studies (Table 3).
| Outcome analysed | Number of studies | Number of patients | RR (95% CI) |
| Oral antibiotic prophylaxis | |||
| Pruritus | 1 | 64 | 3.00 (0.13 to 71.00) |
| Diarrhoea | 1 | 64 | 0.09 (0.01 to 1.58) |
| Nausea | 1 | 64 | 9.00 (0.50 to 160.59) |
| Allergy | 1 | 64 | 5.00 (0.25 to 100.20) |
| Nasal antibiotic prophylaxis | |||
| Nasal irritation | 1 | 15 | 2.10 (0.10 to 44.40) |
| Rhinitis | 1 | 267 | 0.74 (0.27 to 2.09) |
| Headache | 1 | 267 | 0.99 (0.14 to 6.94) |
| Diarrhoea | 1 | 267 | 1.65 (0.40 to 6.78) |
| Nausea | 1 | 267 | 0.99 (0.14 to 6.94) |
| Vomiting | 1 | 267 | 2.98 (0.61 to 14.94) |
| Pruritus | 1 | 267 | 1.49 (0.25 to 8.77) |
| Topical disinfectants | |||
| Technique failure | 1 | 149 | 0.19 (0.01 to 3.83) |
| Pruritus | 1 | 149 | 10.29 (0.58 to 182.92) |
Outcomes sought but not reported
Very few studies reported on peritonitis relapse, development of antibiotic resistance (topical use), hospitalisation due to PD‐related infections or peritonitis, time to first peritonitis episode, technique failure (transfer from PD to haemodialysis/transplant due to peritonitis), or death due to peritonitis.
Discussion
Summary of main results
We identified 39 studies that compared antimicrobial agents with placebo/no treatment or other antimicrobial agent or standard care in CKD patients on PD. A range of antimicrobial agents were found and studies using antibiotic prophylaxis showed wide variability regarding the dose and duration of the interventions trialled. The duration of studies ranged from 1 month to 8 years. The quality of the evidence for all of the findings listed below was low.
Key findings are as follows.
-
The use of oral or topical antibiotic had uncertain effects on the risk of exit‐site/tunnel infection and the risk of peritonitis.
-
The topical administration of antibiotic ointment to the anterior nares of PD patients (sodium fusidate or mupirocin ointment) had uncertain effects on the risk of exit‐site/tunnel infection and the risk of peritonitis.
-
Pre/peri‐operative intravenous vancomycin may reduce the risk of early peritonitis in the first few weeks (< 1 month) following Tenckhoff catheter insertion but has an uncertain effect on the risk of exit‐site/tunnel infection. The comparisons using other antibiotics (i.e. IV gentamicin; IV cefazolin plus gentamicin; IV cefuroxime plus cefuroxime intraperitoneal) did not reduce the risk of peritonitis or exit‐site/tunnel infection.
-
The use of topical disinfectant had uncertain effects on the risk of exit‐site/tunnel infection and the risk of peritonitis.
-
Oral antifungal prophylaxis (fluconazole or nystatin) with each antibiotic course given to a PD patient may reduce the risk of fungal peritonitis.
-
No intervention reduced the risk of catheter removal or replacement.
Oral or topical antibiotics versus placebo/no treatment, oral or topical antibiotics versus other antibiotic, nasal antibiotics versus placebo/no treatment, pre/peri‐operative prophylaxis versus placebo/no treatment or other antibiotic, topical disinfectants versus standard care or other active treatment, germicidal chamber versus none, or silver ring system on catheter versus none had an effect on all‐cause mortality. Neither oral or topical antibiotics versus other antibiotic nor topical disinfectants versus standard care or other active treatment had an effect on the risk of technique failure.
Heterogeneity among the studies was low except for the interventions oral or topical antibiotics versus placebo/no treatment and oral or topical antibiotics versus other antibiotic. Heterogeneity in the former comparison for the risk of peritonitis was 33% and was likely related to the variety of antibiotics used, the frequency of administration (daily, monthly, every three months), the route of administration (oral, topical) and the population studied (adults in Brazil, Canada, USA, Hong Kong). Heterogeneity in the latter comparison for the risk of exit‐site/tunnel infection was 56% and was probably related to the range of antibiotics used, the frequency of administration (twice daily, daily, every 2 days, weekly), the route of administration (oral, topical) and the population studied (adults in the Philippines, Brazil, Hong Kong, USA).
Overall completeness and applicability of evidence
Twelve studies reported all three primary outcomes of interest and could be meta‐analysed (peritonitis, exit‐site/tunnel infection, catheter removal/replacement), 15 studies reported two primary outcomes of interest, and 12 studies reported on one primary outcome of interest; two studies reported all primary outcomes in a way that could not be meta‐analysed (Axelrod 1973; Sharma 1971). Our meta‐analyses identified that use of oral or topical antibiotics had uncertain effects on the risk of exit‐site/tunnel infection and the risk of peritonitis and did not appear to affect the exit‐site/tunnel infection rate, peritonitis rate, or the risk of catheter removal/replacement. It is unclear if the use of nasal mupirocin in identified nasal carriers of S. aureus reduces the risk of exit‐site/tunnel infection or peritonitis. The use of pre/peri‐operative IV antibiotics at PD catheter insertion may reduce the occurrence of early peritonitis (within 1 month of insertion) with vancomycin being the most effective antibiotic to use. The RR of 0.08 for the outcome of early peritonitis could be classified as clinically important, should it be confirmed with future studies. The use of topical disinfectant had uncertain effects on the risk of exit‐site/tunnel infection and the risk of peritonitis. The co‐administration of antifungal agents with an antibiotic course appears to reduce the risk of fungal peritonitis developing in a PD patient. The risk ratio of 0.28 for the outcome of fungal peritonitis could prove to be clinically important, should it be confirmed with future studies.
No RCT was found which had the comparison of routine courses of intranasal mupirocin versus daily exit‐site mupirocin. Likewise, no RCT was found which compared S. aureus nasal carriage eradication at the time of PD catheter insertion versus no eradication of S. aureus nasal carriage. In addition, some outcomes were either not addressed (development of antibiotic resistance with topical use) or not often addressed (peritonitis relapse, hospitalisation rates due to PD‐related infections or peritonitis, technique failure due to peritonitis). It should also be mentioned that for most comparisons there are only a few studies and small numbers of patients.
Quality of the evidence
Our review included 39 studies that involved 4374 patients; all were either on PD (CAPD, CCPD or APD) or were having surgery to insert the Tenckhoff catheter prior to commencing PD. Two studies had paediatric populations, two studies had a mix of adults and children, with the remainder having only adult patients. We found the quality of evidence for all outcomes to be of low quality mainly due to unclear or high risk of bias in a majority of studies and imprecise results because of small patient numbers and events. This means that further research is likely to have an important impact on our confidence in the estimates of effect and is likely to change those estimates.
Of the 39 included studies, four were available only as abstracts; 19 reported adequate sequence generation, and 12 had adequate allocation concealment. Hence, allocation concealment was either unclear or inadequate in two‐thirds of the studies. Studies that do not have adequate allocation concealment are felt to be at increased risk of bias (Moher 1998; Schulz 1995). Eight studies reported adequate blinding of patients and personnel, and 10 studies reported adequate blinding of outcome assessment. Therefore, blinding methodology was either unclear or inadequate in three‐quarters of the studies. We found that 22 studies provided complete data reporting, and 12 reported all primary outcomes. Seven studies reported receiving some form of sponsorship from pharmaceutical companies, four studies reported complete or partial funding from an institute or government organisation, one study received funding from both pharmaceutical and a government organisation, and 27 studies did not report any funding source. In this review, we did not observe a difference between studies that were sponsored by pharmaceutical companies and those that were not. Of the eight pharma‐sponsored/pharma plus government funded studies, five had adequate allocation concealment; of the four studies with partial or full funding from an institute/government organisation, three reported adequate allocation concealment; and of the 27 studies that did not report a funding source, only four demonstrated adequate allocation concealment. Likewise, in terms of selective outcome reporting, two of the eight pharma‐sponsored/pharma plus government funded studies reported all of our primary outcomes; three of the four institute/ government‐sponsored studies reported all our primary outcomes; and seven of the 27 studies without a declared funding source included all our primary outcomes.
For the comparison of oral or topical antibiotics versus placebo/no treatment, the variable quality of relevant studies and the small patient numbers, meant the quality of evidence was rated as low for the outcomes of peritonitis, exit‐site/tunnel infection and catheter removal/replacement (summary of findings Table for the main comparison). For the comparison of nasal antibiotics versus placebo/no treatment, the variable quality of relevant studies and the small patient numbers, reduced the quality of evidence to low for the outcomes of peritonitis, exit‐site/tunnel infection and catheter removal/replacement (summary of findings Table 2). With the comparison of topical disinfectants versus standard care or other active treatment, the unclear allocation in several studies and imprecision due to small patient numbers and events in several studies, meant the quality of evidence was rated as low for the outcomes of peritonitis, exit‐site/tunnel infection and catheter removal/replacement (summary of findings Table 3).
With the comparison of antifungal prophylaxis versus placebo/no treatment, the quality of evidence for the outcome of fungal peritonitis was considered to be low because of high risk of bias in one study and modest patient numbers and the limited number of studies reporting this outcome (summary of findings Table 4).
Potential biases in the review process
Four of the 39 included studies were available only as abstracts but this was not considered a major source of bias. Since the original version of this review was published, the literature search has been run several times (up to 4 October 2016), to increase the chance that all eligible studies published before that time have been included. Although the Cochrane Kidney and Transplant Specialised Register includes references of reports of studies identified by handsearching resources including conference proceedings, it is a possibility that relevant studies may have been added since our last search of the register. Some outcomes were reported in only a few studies, which increased the risk of the non‐randomised selection of patients for the intervention or control group in a study. For example, the outcome of fungal peritonitis was reported in two studies (817 patients), with one study finding a significant difference between the fungal prophylaxis and control groups, while the second study did not have this finding. In addition, adverse effects were reported in only five studies.
Agreements and disagreements with other studies or reviews
A systematic review was performed as part of the HONEYPOT Study 2009 and was published in 2014 (Johnson 2014). The authors systematically reviewed studies of topical antimicrobial prophylaxis for prevention of infections in PD. Nine studies were identified using a search strategy that included electronic searches of MEDLINE (through Ovid) and the Cochrane Central Register of Controlled Trials. Our review included all of the studies included by Johnson 2014, as well as two studies not reported in that review (Chu 2008; Danguilan 2003). This review concluded that the evidence from the nine studies was inconclusive for nasal mupirocin, exit‐site mupirocin and exit‐site gentamicin prophylaxis. In the present review, we reached a similar conclusion, with some individual studies making a significant difference to the risk of exit‐site/tunnel infection or the exit‐site/tunnel infection rate but not having an effect on the other outcomes of peritonitis, catheter removal/replacement and technique failure.
The Renal Association (UK) guidelines currently recommend that "topical antibiotic administration be used to reduce the frequency of S. aureus and Gram‐negative exit‐site infection and peritonitis" (Woodrow 2010). The suggested antibiotics are mupirocin ointment or gentamicin cream (the latter for patients with a known history of Pseudomonas infections). The ISPD position statement on exit‐site care to prevent peritonitis (Piraino 2011) states that "antibiotic protocols against S. aureus are effective in reducing the risk of S. aureus catheter infections" and that "all PD patients should use topical antibiotic either at the catheter exit‐site or intranasally or both". The Kidney Health Australia‐Caring for Australasians with Renal Impairment (KHA‐CARI) guidelines (Walker 2014) recommend that "prophylactic therapy using mupirocin ointment be used, especially for S. aureus carriage (intranasally or at the exit site) to decrease the risk of S. aureus catheter exit‐site/tunnel infections and peritonitis" and suggest that the "PD catheter exit site be cleaned daily and a topical antimicrobial agent (either mupirocin or gentamicin) be applied". This review found that the use of oral antibiotic or mupirocin ointment (at the exit site) may reduce the risk of exit‐site/tunnel infection and the risk of peritonitis but was not seen to reduce the exit‐site/tunnel infection rate, the peritonitis rate or the number of patients with catheter removal/replacement. The head‐to‐head comparison of application of mupirocin ointment or cream against gentamicin cream is based on two studies and shows that there is no difference between the effectiveness of mupirocin and gentamicin in terms of preventing exit‐site/tunnel infection and peritonitis. It is unclear if the nasal application of mupirocin reduces the risk of exit‐site/tunnel infection or the risk of peritonitis.
The Renal Association (UK) guidelines state it is "recommended that initial catheter insertion be accompanied by antibiotic prophylaxis" and refer to the RCT evidence supporting the use of vancomycin (Figueiredo 2010; Woodrow 2010). The ISPD position statement says that "prophylactic antibiotics administered at the time of insertion decrease the infection risk. A first‐generation cephalosporin or vancomycin can be used, but suggested each program should weigh the potential benefit against the risk of vancomycin use (development of resistant organisms)" (Piraino 2011). The KHA‐CARI guidelines say it is "recommended that intravenous antibiotic prophylaxis be used prior to PD catheter insertion to reduce the risk of early peritonitis" and "vancomycin, cephalosporins and gentamicin have demonstrated effectiveness in reducing the risk of peritonitis" (Walker 2014). The inclusion of first generation cephalosporins is based on extrapolations from the results of pre‐operative antibiotic studies in patients without chronic kidney disease. However, our study indicates that the evidence supporting the use of first generation cephalosporins in PD patients undergoing Tenckhoff catheter insertion is scant. In the present review, we identified four RCTs of different pre‐operative antibiotic prophylaxis regimens, including parenteral gentamicin, vancomycin, cephazolin and cefuroxime, with only two evaluating a first generation cephalosporin. One small study involving 50 PD patients found that cephazolin and gentamicin were no better than no treatment (Lye 1992). The largest of the studies (265 patients) showed that cephazolin was inferior to vancomycin in preventing post‐operative catheter‐associated infections (7% versus 1%, respectively; P < 0.05) (Gadallah 2000c). However, the recommendation to use a first generation cephalosporin or vancomycin is understandable because of the risk of selecting for resistant organisms such as vancomycin‐resistant enterococci and S. aureus (HICPAC 1995) and the development of Clostridium difficile colitis (Figueiredo 2010). The postoperative incidence of peritonitis in the control arms of three of the evaluated studies were high, ranging from 14% to 46% (Bennet‐Jones 1988; Gadallah 2000c; Wikdahl 1997) and the applicability of these data to PD units with lower infection rates following PD catheter insertion is unclear.
The ISPD position statement suggests "most episodes of fungal peritonitis are preceded by courses of antibiotics" and "fungal prophylaxis during antibiotic therapy may prevent some cases of Candida peritonitis in programs that have high rates of fungal peritonitis" (Piraino 2011). The KHA‐CARI guidelines recommend "oral antifungal prophylaxis should be considered when antibiotics are administered to patients undergoing PD to reduce the risk of developing fungal peritonitis" (Walker 2014). This review indicates that fluconazole reduced the risk of fungal peritonitis following antibiotic treatment and that nystatin reduced the rate of Candida peritonitis in PD patients. The authors of the fluconazole study (Restrepo 2010) noted that a growing number of Candida strains were resistant to fluconazole during their study, and this would limit its use.
The ISPD no longer recommends that the exit site be regularly disinfected with antibacterial soap or a medical antiseptic to keep the exit site clean and reduce the numbers of resident bacteria. The current position statement states that "water and antibacterial soap are recommended by many centres. Use of an antiseptic to clean the exit site is preferred in some programs, but the agent must be non‐cytotoxic" (Piraino 2011). The four studies in this review which compared the use of disinfectant against standard care did not show any benefit with the use of disinfectant (povidone‐iodine 10% ointment; povidone‐iodine 2.5% dry powder spray; povidone‐iodine 20g/L solution; sodium hypochlorite 10% solution) compared with standard care (povidone‐iodine 10% solution; alcohol chlorhexidine hand wash and use of alcohol wipes; non‐disinfectant soap and water; pH neutral soap and water). Three of the studies did not report on adverse effects of the interventions and one study observed that skin rashes/pruritus occurred in 6% of patients following use of the povidone‐iodine dry powder spray (Wilson 1997). The three studies in this review which looked at the use of disinfectant versus antibiotic or other disinfectant also did not show any benefit with the use of disinfectant (sodium hypochlorite 10% solution; sodium hypochlorite 5% solution; antibacterial honey 10 mg) compared with antibiotic (2% mupirocin ointment) or other disinfectant (povidone iodine 10% solution). Adverse effects were reported in each of these studies. Sodium hypochlorite solution was associated with more irritation around the exit site than povidone iodine solution (Wadhwa 1995; Wadhwa 1997) and 5.9% of patients using antibacterial honey at the exit site in HONEYPOT Study 2009 reported local reaction as the reason for withdrawing from the study whereas no patients in the control group reported this adverse effect.

Study flow diagram.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Comparison 1 Oral or topical antibiotics versus placebo/no treatment, Outcome 1 Peritonitis (number of patients with one or more episodes).

Comparison 1 Oral or topical antibiotics versus placebo/no treatment, Outcome 2 Peritonitis rate (episodes/total patient‐months on PD).

Comparison 1 Oral or topical antibiotics versus placebo/no treatment, Outcome 3 Exit‐site/tunnel infection (number of patients with one or more episodes).

Comparison 1 Oral or topical antibiotics versus placebo/no treatment, Outcome 4 Exit‐site/tunnel infection rate (episodes/total patient‐months on PD).

Comparison 1 Oral or topical antibiotics versus placebo/no treatment, Outcome 5 Catheter removal or replacement (number of patients).

Comparison 1 Oral or topical antibiotics versus placebo/no treatment, Outcome 6 Mortality (all‐cause).
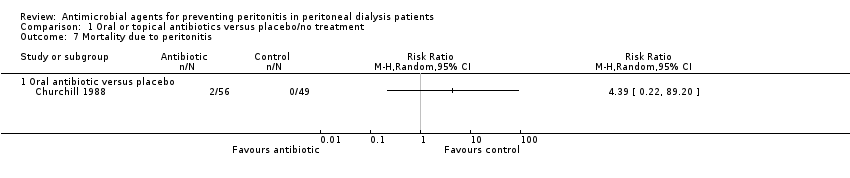
Comparison 1 Oral or topical antibiotics versus placebo/no treatment, Outcome 7 Mortality due to peritonitis.

Comparison 1 Oral or topical antibiotics versus placebo/no treatment, Outcome 8 Adverse effects.
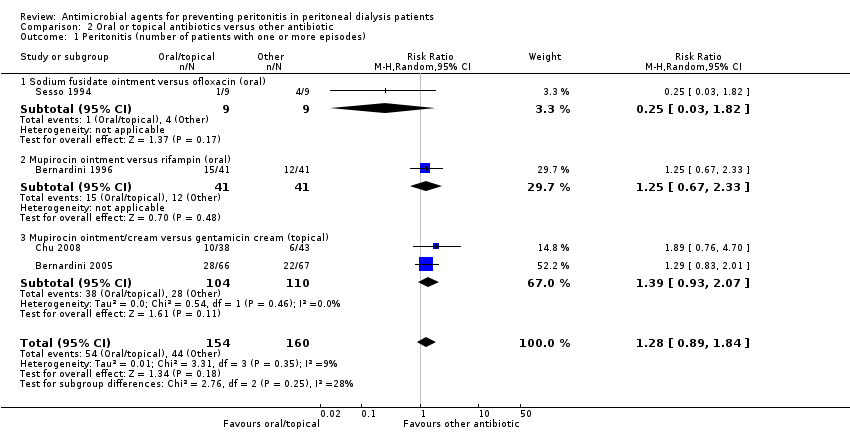
Comparison 2 Oral or topical antibiotics versus other antibiotic, Outcome 1 Peritonitis (number of patients with one or more episodes).

Comparison 2 Oral or topical antibiotics versus other antibiotic, Outcome 2 Peritonitis rate (episodes/total patient‐months on PD).

Comparison 2 Oral or topical antibiotics versus other antibiotic, Outcome 3 Exit‐site/tunnel infection (number of patients with one or more episodes).
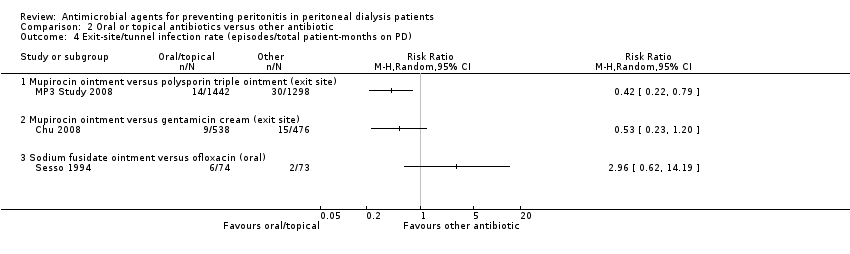
Comparison 2 Oral or topical antibiotics versus other antibiotic, Outcome 4 Exit‐site/tunnel infection rate (episodes/total patient‐months on PD).
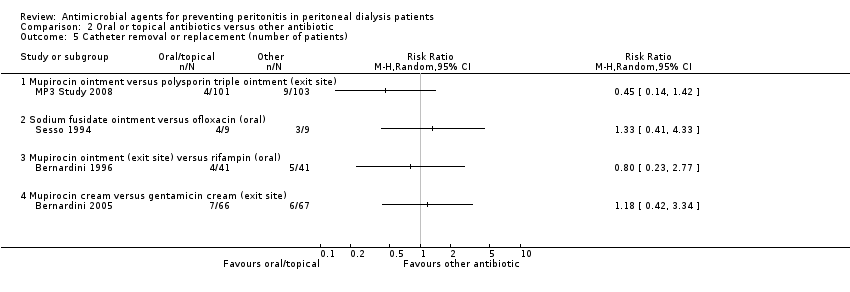
Comparison 2 Oral or topical antibiotics versus other antibiotic, Outcome 5 Catheter removal or replacement (number of patients).
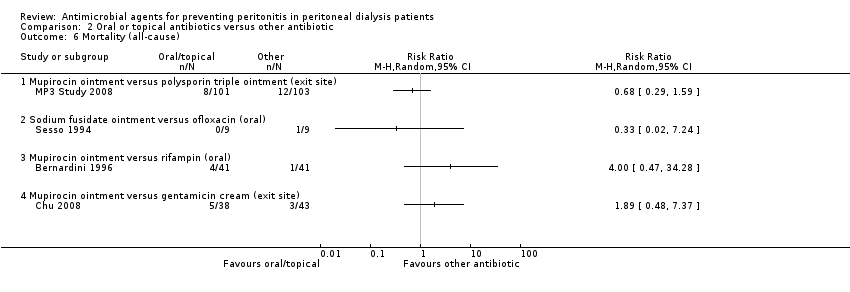
Comparison 2 Oral or topical antibiotics versus other antibiotic, Outcome 6 Mortality (all‐cause).

Comparison 2 Oral or topical antibiotics versus other antibiotic, Outcome 7 Technique failure.

Comparison 2 Oral or topical antibiotics versus other antibiotic, Outcome 8 Adverse effects.
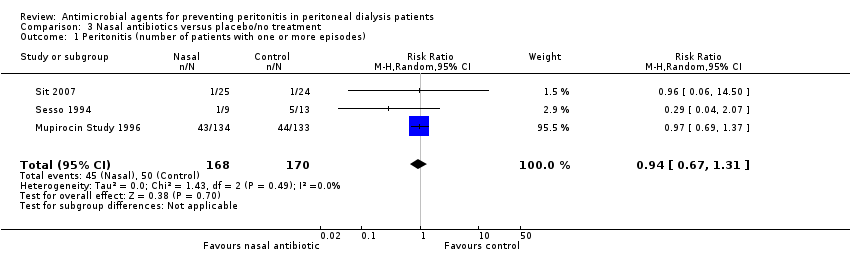
Comparison 3 Nasal antibiotics versus placebo/no treatment, Outcome 1 Peritonitis (number of patients with one or more episodes).
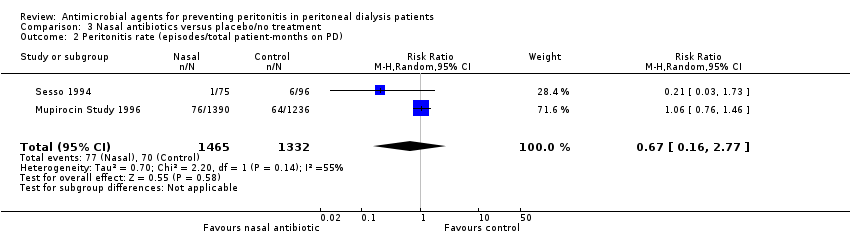
Comparison 3 Nasal antibiotics versus placebo/no treatment, Outcome 2 Peritonitis rate (episodes/total patient‐months on PD).

Comparison 3 Nasal antibiotics versus placebo/no treatment, Outcome 3 Exit site and tunnel infection (number of patients with one or more episodes).
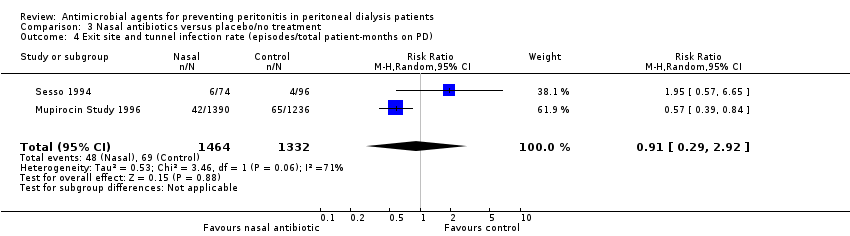
Comparison 3 Nasal antibiotics versus placebo/no treatment, Outcome 4 Exit site and tunnel infection rate (episodes/total patient‐months on PD).
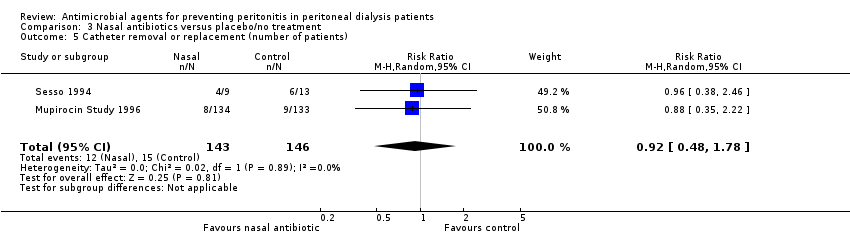
Comparison 3 Nasal antibiotics versus placebo/no treatment, Outcome 5 Catheter removal or replacement (number of patients).
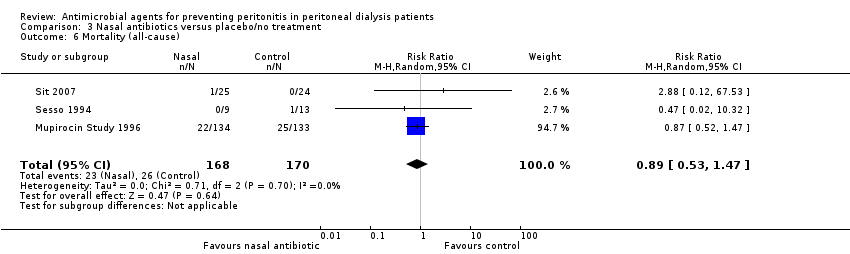
Comparison 3 Nasal antibiotics versus placebo/no treatment, Outcome 6 Mortality (all‐cause).

Comparison 3 Nasal antibiotics versus placebo/no treatment, Outcome 7 Adverse effects.

Comparison 4 Pre/peri‐operative prophylaxis versus placebo/no treatment or other antibiotic, Outcome 1 Peritonitis (number of patients with one or more episodes).

Comparison 4 Pre/peri‐operative prophylaxis versus placebo/no treatment or other antibiotic, Outcome 2 Exit site/tunnel infection (number of patients with one or more episodes).
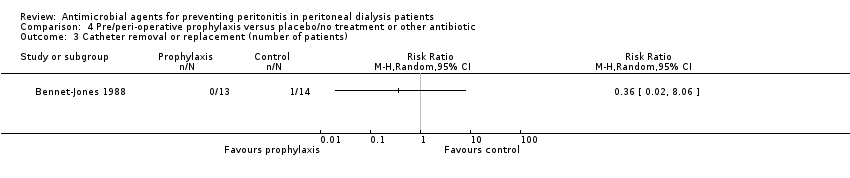
Comparison 4 Pre/peri‐operative prophylaxis versus placebo/no treatment or other antibiotic, Outcome 3 Catheter removal or replacement (number of patients).

Comparison 4 Pre/peri‐operative prophylaxis versus placebo/no treatment or other antibiotic, Outcome 4 Mortality (all‐cause).

Comparison 5 Topical disinfectants versus standard care or other active treatment (antibiotic or other disinfectant), Outcome 1 Peritonitis (number of patients with one or more episodes).

Comparison 5 Topical disinfectants versus standard care or other active treatment (antibiotic or other disinfectant), Outcome 2 Exit site/tunnel infection (number of patients with one or more episodes).
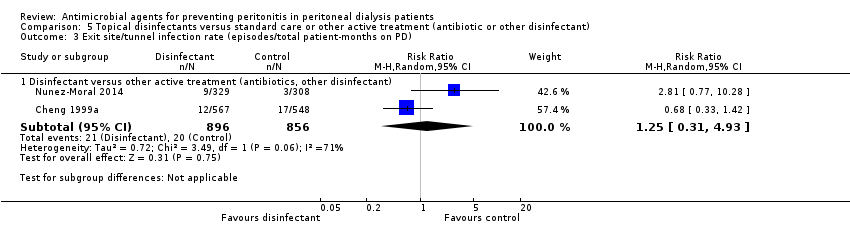
Comparison 5 Topical disinfectants versus standard care or other active treatment (antibiotic or other disinfectant), Outcome 3 Exit site/tunnel infection rate (episodes/total patient‐months on PD).

Comparison 5 Topical disinfectants versus standard care or other active treatment (antibiotic or other disinfectant), Outcome 4 Catheter removal or replacement (number of patients).
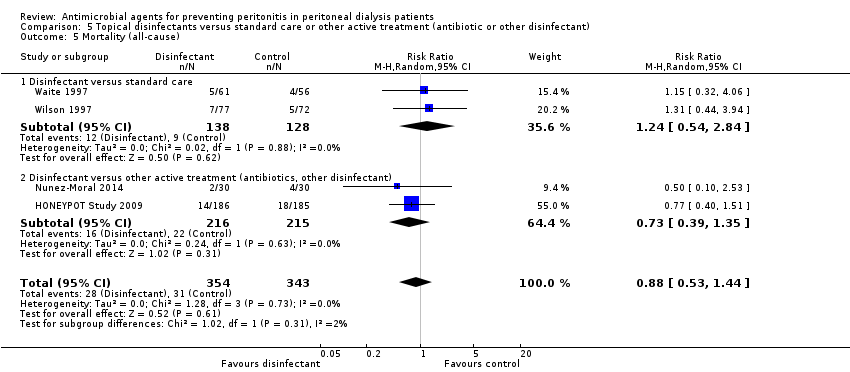
Comparison 5 Topical disinfectants versus standard care or other active treatment (antibiotic or other disinfectant), Outcome 5 Mortality (all‐cause).

Comparison 5 Topical disinfectants versus standard care or other active treatment (antibiotic or other disinfectant), Outcome 6 Technique failure.
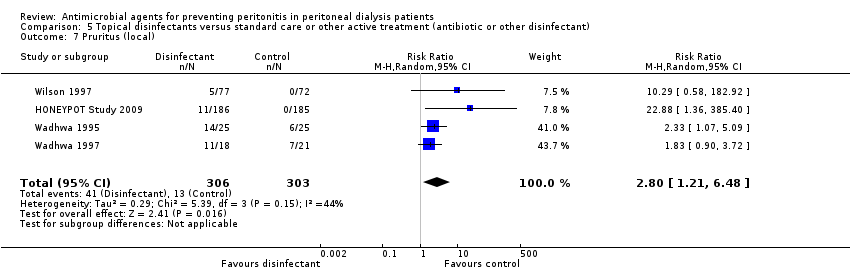
Comparison 5 Topical disinfectants versus standard care or other active treatment (antibiotic or other disinfectant), Outcome 7 Pruritus (local).
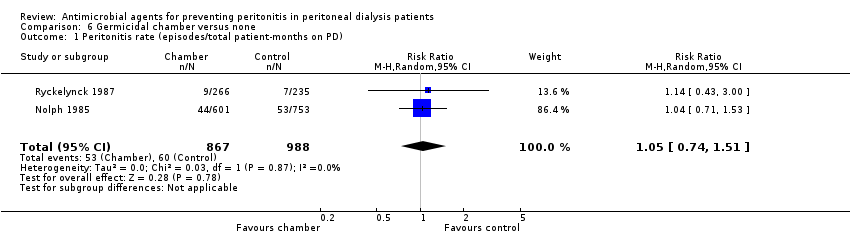
Comparison 6 Germicidal chamber versus none, Outcome 1 Peritonitis rate (episodes/total patient‐months on PD).

Comparison 6 Germicidal chamber versus none, Outcome 2 Mortality (all‐cause).

Comparison 7 Dressing systems (any), Outcome 1 Exit site/tunnel infection (number of patients with one or more episodes).

Comparison 7 Dressing systems (any), Outcome 2 Exit site/tunnel infection rate (episodes/total patient‐months on PD).

Comparison 8 Silver ring system on catheter versus none, Outcome 1 Peritonitis (number of patients with one or more episodes).

Comparison 8 Silver ring system on catheter versus none, Outcome 2 Exit site/tunnel infection (number of patients with one or more episodes).
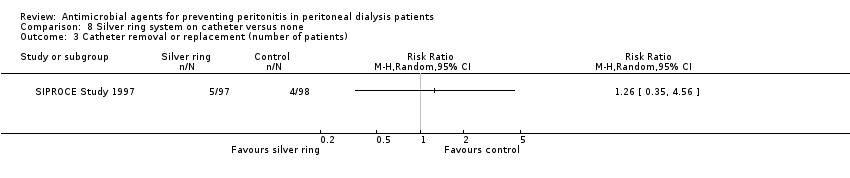
Comparison 8 Silver ring system on catheter versus none, Outcome 3 Catheter removal or replacement (number of patients).

Comparison 8 Silver ring system on catheter versus none, Outcome 4 Mortality (all‐cause).

Comparison 9 Antistaphylococcal vaccine (Staphypan) versus placebo, Outcome 1 Peritonitis rate (episodes/total patient‐months on PD).

Comparison 9 Antistaphylococcal vaccine (Staphypan) versus placebo, Outcome 2 Exit site/tunnel infection rate (episodes/total patient‐months on PD).

Comparison 10 Antifungal versus placebo/no treatment, Outcome 1 Fungal peritonitis (number of patients with one or more episodes).

Comparison 10 Antifungal versus placebo/no treatment, Outcome 2 Fungal peritonitis rate (episodes/total patient‐months on PD).
| Oral or topical or intraperitoneal antibiotics versus placebo/no treatment for preventing peritonitis in peritoneal dialysis patients | ||||||
| Patient or population: patients with CKD on peritoneal dialysis | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Oral or topical or intraperitoneal antibiotics versus placebo/no treatment | |||||
| Peritonitis (number of patients with one or more episodes) | Study population | RR 0.82 | 395 (5) | ⊕⊕⊝⊝ | ||
| 360 per 1000 | 295 per 1000 | |||||
| Moderate | ||||||
| 385 per 1000 | 316 per 1000 | |||||
| Exit‐site/tunnel infection (number of patients with one or more episodes) | Study population | RR 0.45 | 191 (3) | ⊕⊕⊝⊝ | ||
| 176 per 1000 | 79 per 1000 | |||||
| Moderate | ||||||
| 231 per 1000 | 104 per 1000 | |||||
| Catheter removal or replacement (number of patients) | Study population | RR 0.82 | 395 (5) | ⊕⊕⊝⊝ | ||
| 115 per 1000 | 94 per 1000 | |||||
| Moderate | ||||||
| 156 per 1000 | 128 per 1000 | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Unclear or high risk of bias in 3 of 5 studies Abbreviations: CKD ‐ chronic kidney disease; GRADE ‐ Grading of Recommendations Assessment, Development and Evaluation | ||||||
| Nasal antibiotics versus no treatment for preventing peritonitis in peritoneal dialysis patients | ||||||
| Patient or population: patients with CKD on peritoneal dialysis | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No. of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Nasal antibiotics versus placebo/no treatment | |||||
| Peritonitis (number of patients with one or more episodes) | Study population | RR 0.94 | 338 (3) | ⊕⊕⊝⊝ | ||
| 294 per 1000 | 276 per 1000 | |||||
| Moderate | ||||||
| 331 per 1000 | 311 per 1000 | |||||
| Exit‐site/ tunnel infection (number of patients with one or more episodes) | Study population | RR 1.34 | 338 (3) | ⊕⊕⊝⊝ | ||
| 165 per 1000 | 221 per 1000 | |||||
| Moderate | ||||||
| 188 per 1000 | 252 per 1000 | |||||
| Catheter removal or replacement (number of patients) | Study population | RR 0.92 | 289 (2) | ⊕⊕⊝⊝ | ||
| 103 per 1000 | 95 per 1000 | |||||
| Moderate | ||||||
| 265 per 1000 | 244 per 1000 | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio | ||||||
| GRADE Working Group grades of evidence | ||||||
| ¹ Unclear risk of bias for allocation concealment in largest study (Mupirocin Study 1996) Abbreviations: CKD ‐ chronic kidney disease; GRADE ‐ Grading of Recommendations Assessment, Development and Evaluation | ||||||
| Topical disinfectants versus standard care or other active treatment (antibiotic or other disinfectant) for preventing peritonitis in peritoneal dialysis patients | ||||||
| Patient or population: patients with CKD on peritoneal dialysis | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No. of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Topical disinfectants versus standard care or other active treatment (antibiotic or other disinfectant) | |||||
| Peritonitis (number of patients with one or more episodes) | Study population | RR 0.83 | 853 (6) | ⊕⊕⊝⊝ | ||
| 235 per 1000 | 195 per 1000 | |||||
| Moderate | ||||||
| 152 per 1000 | 126 per 1000 | |||||
| Exit‐site/tunnel infection (number of patients with one or more episodes) | Study population | RR 0.97 | 913 (7) | ⊕⊕⊝⊝ | ||
| 238 per 1000 | 230 per 1000 | |||||
| Moderate | ||||||
| 222 per 1000 | 215 per 1000 | |||||
| Catheter removal or replacement (number of patients) | Study population | RR 0.89 | 792 (6) | ⊕⊕⊝⊝ | ||
| 97 per 1000 | 86 per 1000 | |||||
| Moderate | ||||||
| 93 per 1000 | 83 per 1000 | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Unclear allocation in several studies Abbreviations: CKD ‐ chronic kidney disease; GRADE ‐ Grading of Recommendations Assessment, Development and Evaluation | ||||||
| Antifungal versus placebo/no treatment for preventing fungal peritonitis in peritoneal dialysis patients | ||||||
| Patient or population: patients with CKD on peritoneal dialysis | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No. of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Antifungal versus placebo/no treatment | |||||
| Fungal peritonitis (number of patients with one or more episodes) | Study population | RR 0.28 | 817 (2) | ⊕⊕⊝⊝ | ||
| 64 per 1000 | 18 per 1000 | |||||
| Moderate | ||||||
| 64 per 1000 | 18 per 1000 | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 High risk of bias in one study (Lo 1996) Abbreviations: CKD ‐ chronic kidney disease; GRADE ‐ Grading of Recommendations Assessment, Development and Evaluation | ||||||
| Guideline | Country | Year | Recommendation |
| Kidney‐Disease Outcomes Quality Initiative | United States of America | NA | No guideline |
| The Renal Association | United Kingdom | April 2008 July 2010 | Guideline 3.1 ‐ PD Access: Implantation Protocol
Guideline 5.1.4 ‐ PD Infectious Complications: Prevention Strategies
Guideline 5.1.5 ‐ PD Infectious Complications: Prevention Strategies
Guideline 5.1.6 ‐ PD Infectious Complications: Prevention Strategies
|
| Canadian Society of Nephrology | Canada | NA | No guideline |
| European Renal Best Practice | Europe | NA | No guideline |
| International Society for Peritoneal Dialysis | NA | July 2010 November 2011 | Guideline 3.1: Implantation Protocol (1A)
Position Statement: Catheter Placement to Prevent Catheter Infections and the Related Peritonitis Episodes
Position Statement: Exit‐Site Care to Prevent Peritonitis
Position Statement: Prevention of Fungal Peritonitis
|
| Kidney Health Australia‐Caring for Australasians with Renal Impairment | Australia/ New Zealand | February 2014 | Guideline 6. Prophylactic Antibiotics for Insertion of PD Catheters
Guideline 8. Treatment of Peritoneal Dialysis‐Associated Fungal Peritonitis
Guideline 10. Prophylaxis for Exit‐site/Tunnel Infections Using Mupirocin
|
| MRSA ‐ methicillin‐resistant S. aureus; NA ‐ not applicable; PD ‐ peritoneal dialysis | |||
| Comparisons in 2004 review | Comparisons in 2017 review |
| Oral antibiotics versus none | Oral or topical antibiotics versus placebo/no treatment |
| Nasal antibiotics versus none | Oral or topical antibiotics versus other antibiotic |
| Peri‐operative IV prophylaxis versus none | Nasal antibiotics versus no treatment |
| Peri‐operative IV prophylaxis head‐to‐head | Pre/peri‐operative IV prophylaxis versus none or head‐to‐head |
| Topical disinfectants versus none | Topical disinfectants versus standard care or other active treatment (antibiotic or other disinfectant) |
| Germicidal chamber versus none | Germicidal chamber versus none |
| Antistaphylococcal vaccine (Staphypan) versus placebo | Dressing systems (any) |
| Antibiotic prophylaxis head‐to‐head agents | Silver ring system on catheter versus none |
| ‐‐ | Antistaphylococcal vaccine (Staphypan) versus placebo |
| ‐‐ | Antifungal versus placebo/no treatment |
| Outcome analysed | Number of studies | Number of patients | RR (95% CI) |
| Oral antibiotic prophylaxis | |||
| Pruritus | 1 | 64 | 3.00 (0.13 to 71.00) |
| Diarrhoea | 1 | 64 | 0.09 (0.01 to 1.58) |
| Nausea | 1 | 64 | 9.00 (0.50 to 160.59) |
| Allergy | 1 | 64 | 5.00 (0.25 to 100.20) |
| Nasal antibiotic prophylaxis | |||
| Nasal irritation | 1 | 15 | 2.10 (0.10 to 44.40) |
| Rhinitis | 1 | 267 | 0.74 (0.27 to 2.09) |
| Headache | 1 | 267 | 0.99 (0.14 to 6.94) |
| Diarrhoea | 1 | 267 | 1.65 (0.40 to 6.78) |
| Nausea | 1 | 267 | 0.99 (0.14 to 6.94) |
| Vomiting | 1 | 267 | 2.98 (0.61 to 14.94) |
| Pruritus | 1 | 267 | 1.49 (0.25 to 8.77) |
| Topical disinfectants | |||
| Technique failure | 1 | 149 | 0.19 (0.01 to 3.83) |
| Pruritus | 1 | 149 | 10.29 (0.58 to 182.92) |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Peritonitis (number of patients with one or more episodes) Show forest plot | 5 | 395 | Risk Ratio (M‐H, Random, 95% CI) | 0.82 [0.57, 1.19] |
| 1.1 Oral antibiotic versus placebo | 4 | 241 | Risk Ratio (M‐H, Random, 95% CI) | 0.87 [0.58, 1.32] |
| 1.2 Mupirocin ointment versus standard care | 1 | 154 | Risk Ratio (M‐H, Random, 95% CI) | 0.55 [0.22, 1.40] |
| 2 Peritonitis rate (episodes/total patient‐months on PD) Show forest plot | 3 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 2.1 Any systemic antibiotic versus placebo/no treatment (excluding nystatin) | 3 | 1440 | Risk Ratio (M‐H, Random, 95% CI) | 0.68 [0.40, 1.14] |
| 3 Exit‐site/tunnel infection (number of patients with one or more episodes) Show forest plot | 3 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 3.1 Any systemic antibiotic versus placebo/no treatment | 3 | 191 | Risk Ratio (M‐H, Random, 95% CI) | 0.45 [0.19, 1.04] |
| 4 Exit‐site/tunnel infection rate (episodes/total patient‐months on PD) Show forest plot | 2 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 4.1 Any systemic antibiotic versus placebo/no treatment | 2 | 939 | Risk Ratio (M‐H, Random, 95% CI) | 0.42 [0.17, 1.05] |
| 5 Catheter removal or replacement (number of patients) Show forest plot | 5 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 5.1 Any systemic antibiotic versus placebo/no treatment | 5 | 395 | Risk Ratio (M‐H, Random, 95% CI) | 0.82 [0.46, 1.46] |
| 6 Mortality (all‐cause) Show forest plot | 4 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 6.1 Any systemic antibiotic versus placebo/no treatment | 4 | 201 | Risk Ratio (M‐H, Random, 95% CI) | 0.88 [0.41, 1.89] |
| 7 Mortality due to peritonitis Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 7.1 Oral antibiotic versus placebo | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8 Adverse effects Show forest plot | 2 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 8.1 Diarrhoea | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.2 Nausea | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.3 Pruritus (generalised) | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.4 Nasal irritation | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.5 Allergy | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Peritonitis (number of patients with one or more episodes) Show forest plot | 4 | 314 | Risk Ratio (M‐H, Random, 95% CI) | 1.28 [0.89, 1.84] |
| 1.1 Sodium fusidate ointment versus ofloxacin (oral) | 1 | 18 | Risk Ratio (M‐H, Random, 95% CI) | 0.25 [0.03, 1.82] |
| 1.2 Mupirocin ointment versus rifampin (oral) | 1 | 82 | Risk Ratio (M‐H, Random, 95% CI) | 1.25 [0.67, 2.33] |
| 1.3 Mupirocin ointment/cream versus gentamicin cream (topical) | 2 | 214 | Risk Ratio (M‐H, Random, 95% CI) | 1.39 [0.93, 2.07] |
| 2 Peritonitis rate (episodes/total patient‐months on PD) Show forest plot | 5 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2.1 Mupirocin ointment versus polysporin triple ointment (exit site) | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Sodium fusidate ointment versus ofloxacin (oral) | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 Mupirocin ointment versus neomycin sulphate ointment (nasal) | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.4 Mupirocin ointment versus rifampin (oral) | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.5 Mupirocin ointment versus gentamicin cream (exit site) | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Exit‐site/tunnel infection (number of patients with one or more episodes) Show forest plot | 4 | 336 | Risk Ratio (M‐H, Random, 95% CI) | 1.28 [0.71, 2.31] |
| 3.1 Mupirocin ointment versus sodium fusidate ointment (topical) | 1 | 100 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.42, 1.95] |
| 3.2 Sodium fusidate ointment versus ofloxacin (oral) | 1 | 22 | Risk Ratio (M‐H, Random, 95% CI) | 2.41 [0.76, 7.62] |
| 3.3 Mupirocin ointment/cream versus gentamicin cream (topical) | 2 | 214 | Risk Ratio (M‐H, Random, 95% CI) | 1.19 [0.41, 3.46] |
| 4 Exit‐site/tunnel infection rate (episodes/total patient‐months on PD) Show forest plot | 3 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 4.1 Mupirocin ointment versus polysporin triple ointment (exit site) | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 Mupirocin ointment versus gentamicin cream (exit site) | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.3 Sodium fusidate ointment versus ofloxacin (oral) | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Catheter removal or replacement (number of patients) Show forest plot | 4 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 5.1 Mupirocin ointment versus polysporin triple ointment (exit site) | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.2 Sodium fusidate ointment versus ofloxacin (oral) | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.3 Mupirocin ointment (exit site) versus rifampin (oral) | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.4 Mupirocin cream versus gentamicin cream (exit site) | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Mortality (all‐cause) Show forest plot | 4 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 6.1 Mupirocin ointment versus polysporin triple ointment (exit site) | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.2 Sodium fusidate ointment versus ofloxacin (oral) | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.3 Mupirocin ointment versus rifampin (oral) | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.4 Mupirocin ointment versus gentamicin cream (exit site) | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Technique failure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 7.1 Mupirocin ointment versus polysporin triple ointment (exit site) | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8 Adverse effects Show forest plot | 3 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 8.1 Nausea | 1 | 82 | Risk Ratio (M‐H, Random, 95% CI) | 0.09 [0.01, 1.59] |
| 8.2 Pruritus (local) | 2 | 337 | Risk Ratio (M‐H, Random, 95% CI) | 0.65 [0.29, 1.49] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Peritonitis (number of patients with one or more episodes) Show forest plot | 3 | 338 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.67, 1.31] |
| 2 Peritonitis rate (episodes/total patient‐months on PD) Show forest plot | 2 | 2797 | Risk Ratio (M‐H, Random, 95% CI) | 0.67 [0.16, 2.77] |
| 3 Exit site and tunnel infection (number of patients with one or more episodes) Show forest plot | 3 | 338 | Risk Ratio (M‐H, Random, 95% CI) | 1.34 [0.62, 2.87] |
| 4 Exit site and tunnel infection rate (episodes/total patient‐months on PD) Show forest plot | 2 | 2796 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.29, 2.92] |
| 5 Catheter removal or replacement (number of patients) Show forest plot | 2 | 289 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.48, 1.78] |
| 6 Mortality (all‐cause) Show forest plot | 3 | 338 | Risk Ratio (M‐H, Random, 95% CI) | 0.89 [0.53, 1.47] |
| 7 Adverse effects Show forest plot | 2 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 7.1 Headache | 1 | 267 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.14, 6.94] |
| 7.2 Diarrhoea | 1 | 267 | Risk Ratio (M‐H, Random, 95% CI) | 1.65 [0.40, 6.78] |
| 7.3 Nausea | 1 | 267 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.14, 6.94] |
| 7.4 Vomiting | 1 | 267 | Risk Ratio (M‐H, Random, 95% CI) | 2.98 [0.61, 14.49] |
| 7.5 Pruritus | 1 | 267 | Risk Ratio (M‐H, Random, 95% CI) | 1.49 [0.25, 8.77] |
| 7.6 Nasal irritation/rhinitis | 2 | 289 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.30, 2.94] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Peritonitis (number of patients with one or more episodes) Show forest plot | 4 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 1.1 Vancomycin versus placebo | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Cefazolin versus placebo | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 IV gentamicin versus no antibiotics | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.4 IV cefazolin + gentamicin versus no antibiotics | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.5 IV cefuroxime + cefuroxime (intraperitoneal) versus no antibiotics | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.6 Vancomycin versus cefazolin | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Exit site/tunnel infection (number of patients with one or more episodes) Show forest plot | 4 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2.1 Vancomycin versus placebo | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Cefazolin versus placebo | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 IV gentamicin versus no antibiotics | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.4 IV cefazolin + gentamicin versus no antibiotics | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.5 IV cefuroxime + cefuroxime (intraperitoneal) versus no antibiotics | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.6 Vancomycin versus cefazolin | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Catheter removal or replacement (number of patients) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 4 Mortality (all‐cause) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Peritonitis (number of patients with one or more episodes) Show forest plot | 6 | 853 | Risk Ratio (M‐H, Random, 95% CI) | 0.83 [0.65, 1.06] |
| 1.1 Disinfectant versus standard care | 3 | 393 | Risk Ratio (M‐H, Random, 95% CI) | 0.81 [0.52, 1.26] |
| 1.2 Disinfectant versus other active treatment (antibiotics, other disinfectant) | 3 | 460 | Risk Ratio (M‐H, Random, 95% CI) | 0.84 [0.62, 1.13] |
| 2 Exit site/tunnel infection (number of patients with one or more episodes) Show forest plot | 8 | 973 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.75, 1.33] |
| 2.1 Disinfectant versus standard care | 4 | 453 | Risk Ratio (M‐H, Random, 95% CI) | 0.74 [0.45, 1.20] |
| 2.2 Disinfectant versus other active treatment (antibiotics, other disinfectant) | 4 | 520 | Risk Ratio (M‐H, Random, 95% CI) | 1.19 [0.89, 1.60] |
| 3 Exit site/tunnel infection rate (episodes/total patient‐months on PD) Show forest plot | 2 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 3.1 Disinfectant versus other active treatment (antibiotics, other disinfectant) | 2 | 1752 | Risk Ratio (M‐H, Random, 95% CI) | 1.25 [0.31, 4.93] |
| 4 Catheter removal or replacement (number of patients) Show forest plot | 7 | 852 | Risk Ratio (M‐H, Random, 95% CI) | 0.89 [0.57, 1.38] |
| 4.1 Disinfectant versus standard care | 2 | 266 | Risk Ratio (M‐H, Random, 95% CI) | 0.73 [0.34, 1.55] |
| 4.2 Disinfectant versus other active treatment (antibiotics, other disinfectant) | 5 | 586 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.57, 1.69] |
| 5 Mortality (all‐cause) Show forest plot | 4 | 697 | Risk Ratio (M‐H, Random, 95% CI) | 0.88 [0.53, 1.44] |
| 5.1 Disinfectant versus standard care | 2 | 266 | Risk Ratio (M‐H, Random, 95% CI) | 1.24 [0.54, 2.84] |
| 5.2 Disinfectant versus other active treatment (antibiotics, other disinfectant) | 2 | 431 | Risk Ratio (M‐H, Random, 95% CI) | 0.73 [0.39, 1.35] |
| 6 Technique failure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 7 Pruritus (local) Show forest plot | 4 | 609 | Risk Ratio (M‐H, Random, 95% CI) | 2.80 [1.21, 6.48] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Peritonitis rate (episodes/total patient‐months on PD) Show forest plot | 2 | 1855 | Risk Ratio (M‐H, Random, 95% CI) | 1.05 [0.74, 1.51] |
| 2 Mortality (all‐cause) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Exit site/tunnel infection (number of patients with one or more episodes) Show forest plot | 3 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 1.1 Chlorhexidine gluconate + water versus povidone‐iodine solution | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Sodium hypochlorite solution versus povidone‐iodine solution | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 Shower + gauze versus dressing pack + fixomull | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.4 Blisterfilm versus gauze | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Exit site/tunnel infection rate (episodes/total patient‐months on PD) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2.1 Shower + gauze versus dressing pack + fixomull | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Peritonitis (number of patients with one or more episodes) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Exit site/tunnel infection (number of patients with one or more episodes) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3 Catheter removal or replacement (number of patients) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 4 Mortality (all‐cause) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Peritonitis rate (episodes/total patient‐months on PD) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Exit site/tunnel infection rate (episodes/total patient‐months on PD) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Fungal peritonitis (number of patients with one or more episodes) Show forest plot | 2 | 817 | Risk Ratio (M‐H, Random, 95% CI) | 0.28 [0.12, 0.63] |
| 2 Fungal peritonitis rate (episodes/total patient‐months on PD) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |

