| Exercise compared to no treatment for dysmenorrhoea |
| Patient or population: young women with suspected primary dysmenorrhoea
Setting: school, university or outpatient setting
Intervention: exercise
Comparison: no treatment |
| Menstrual pain intensity,
measured by various outcome measures including VAS, MPQ and NRS at the end of the intervention
Lower scores indicate less intense menstrual pain | The mean menstrual pain intensity was 6.76 | SMD 1.86 lower
(2.06 lower to 1.66 lower) | ‐ | 632
(9 RCTs) | ⊕⊕⊝⊝
Lowab | Exercise may provide a large reduction in menstrual pain intensity compared to no treatment. |
| Adverse events | 0 per 1000 | 0 per 1000
(0 to 0) | Not estimable | 36
(1 RCT) | ⊕⊝⊝⊝
Very lowcd | Due to the very low‐quality evidence, we are uncertain whether there is any difference in risk for adverse events between exercise and no treatment control. |
| Overall menstrual symptoms ,
measured by the MMDQ at the end of the intervention.
Lower scores indicates lower menstrual symptom severity | The mean overall menstrual symptoms was 99 | MD 33.16 lower
(40.45 lower to 25.87 lower) | ‐ | 120
(1 RCT) | ⊕⊝⊝⊝
Very lowef | Due to the very low‐quality evidence, we are uncertain whether exercise reduces overall menstrual symptoms compared to a no treatment control. |
| Use of rescue analgesic medication ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | No studies reported on this outcome. |
| Restriction of daily life activities ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | No studies reported on this outcome. |
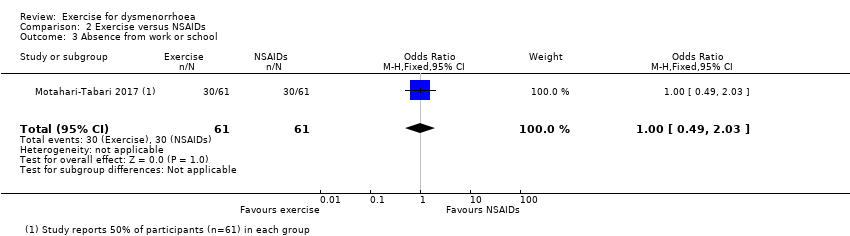
| Absence from work or school ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | No studies reported on this outcome. |
| Quality of life,
assessed with: physical and mental component summary scores measured by the SF‐12 at the end of the intervention Higher scores indicate higher quality of life | Mean postintervention score for the mental component in the no treatment group was 37.6 Mean postintervention score for the physical component in the no treatment group was 44.4 | Mental component: MD 4.40 higher
(1.59 higher to 7.21 higher) Physical component: MD 3.40 higher
(1.68 lower to 8.48 higher) | ‐ | 55
(1 RCT) | ⊕⊝⊝⊝
Very lowgh | Due to the very low‐quality evidence, we are uncertain whether exercise improves quality of life compared to a no treatment control. |
| *The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI).
CI: confidence interval; MD: mean difference; MMDQ: Moos Menstrual Distress Questionnaire; MPQ: McGil Pain Questionnaire; NRS: numeric rating scale; RCT: randomised controlled trial; SF‐12: 12‐Item Short Form Health Survey; SMD: standardised mean difference; VAS: visual analogue scale |
| GRADE Working Group grades of evidence
High quality: further research is very unlikely to change our confidence in the estimate of effect.
Moderate quality: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate.
Low quality: further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate.
Very low quality: we are very uncertain about the estimate. |