Orthodontic treatment for prominent upper front teeth (Class II malocclusion) in children and adolescents
Abstract
Background
Prominent upper front teeth are a common problem affecting about a quarter of 12‐year‐old children in the UK. The condition develops when permanent teeth erupt. These teeth are more likely to be injured and their appearance can cause significant distress. Children are often referred to an orthodontist for treatment with dental braces to reduce the prominence of their teeth. If a child is referred at a young age, the orthodontist is faced with the dilemma of whether to treat the patient early or to wait and provide treatment in adolescence.
Objectives
To assess the effects of orthodontic treatment for prominent upper front teeth initiated when children are seven to 11 years old ('early treatment' in two phases) compared to in adolescence at around 12 to 16 years old ('late treatment' in one phase); to assess the effects of late treatment compared to no treatment; and to assess the effects of different types of orthodontic braces.
Search methods
Cochrane Oral Health’s Information Specialist searched the following databases: Cochrane Oral Health’s Trials Register (to 27 September 2017), the Cochrane Central Register of Controlled Trials (CENTRAL) (the Cochrane Library, 2017, Issue 8), MEDLINE Ovid (1946 to 27 September 2017), and Embase Ovid (1980 to 27 September 2017). The US National Institutes of Health Ongoing Trials Registry (ClinicalTrials.gov) and the World Health Organization International Clinical Trials Registry Platform were searched for ongoing trials. No restrictions were placed on the language or date of publication when searching the electronic databases.
Selection criteria
Randomised controlled trials of orthodontic treatments to correct prominent upper front teeth (Class II malocclusion) in children and adolescents. We included trials that compared early treatment in children (two‐phase) with any type of orthodontic braces (removable, fixed, functional) or head‐braces versus late treatment in adolescents (one‐phase) with any type of orthodontic braces or head‐braces, and trials that compared any type of orthodontic braces or head‐braces versus no treatment or another type of orthodontic brace or appliance (where treatment started at a similar age in the intervention groups).
We excluded trials involving participants with a cleft lip or palate, or other craniofacial deformity/syndrome, and trials that recruited patients who had previously received surgical treatment for their Class II malocclusion.
Data collection and analysis
Review authors screened the search results, extracted data and assessed risk of bias independently. We used odds ratios (ORs) and 95% confidence intervals (CIs) for dichotomous outcomes, and mean differences (MDs) and 95% CIs for continuous outcomes. We used the fixed‐effect model for meta‐analyses including two or three studies and the random‐effects model for more than three studies.
Main results
We included 27 RCTs based on data from 1251 participants.
Three trials compared early treatment with a functional appliance versus late treatment for overjet, ANB and incisal trauma. After phase one of early treatment (i.e. before the other group had received any intervention), there was a reduction in overjet and ANB reduction favouring treatment with a functional appliance; however, when both groups had completed treatment, there was no difference between groups in final overjet (MD 0.21, 95% CI −0.10 to 0.51, P = 0.18; 343 participants) (low‐quality evidence) or ANB (MD −0.02, 95% CI −0.47 to 0.43; 347 participants) (moderate‐quality evidence). Early treatment with functional appliances reduced the incidence of incisal trauma compared to late treatment (OR 0.56, 95% CI 0.33 to 0.95; 332 participants) (moderate‐quality evidence). The difference in the incidence of incisal trauma was clinically important with 30% (51/171) of participants reporting new trauma in the late treatment group compared to only 19% (31/161) of participants who had received early treatment.
Two trials compared early treatment using headgear versus late treatment. After phase one of early treatment, headgear had reduced overjet and ANB; however, when both groups had completed treatment, there was no evidence of a difference between groups in overjet (MD −0.22, 95% CI −0.56 to 0.12; 238 participants) (low‐quality evidence) or ANB (MD −0.27, 95% CI −0.80 to 0.26; 231 participants) (low‐quality evidence). Early (two‐phase) treatment with headgear reduced the incidence of incisal trauma (OR 0.45, 95% CI 0.25 to 0.80; 237 participants) (low‐quality evidence), with almost half the incidence of new incisal trauma (24/117) compared to the late treatment group (44/120).
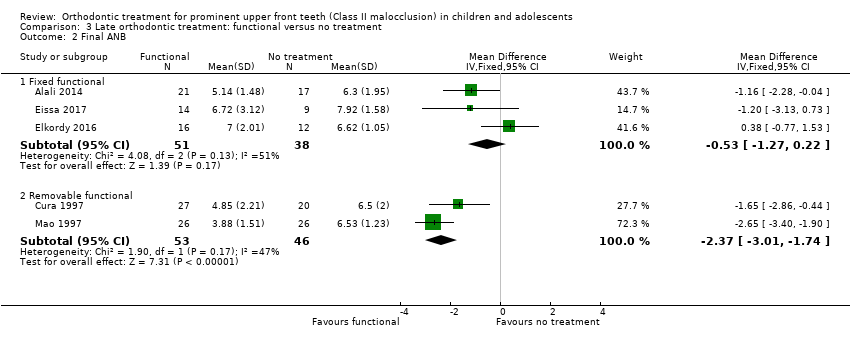
Seven trials compared late treatment with functional appliances versus no treatment. There was a reduction in final overjet with both fixed functional appliances (MD −5.46 mm, 95% CI −6.63 to −4.28; 2 trials, 61 participants) and removable functional appliances (MD −4.62, 95% CI ‐5.33 to ‐3.92; 3 trials, 122 participants) (low‐quality evidence). There was no evidence of a difference in final ANB between fixed functional appliances and no treatment (MD −0.53°, 95% CI −1.27 to −0.22; 3 trials, 89 participants) (low‐quality evidence), but removable functional appliances seemed to reduce ANB compared to no treatment (MD −2.37°, 95% CI ‐3.01 to ‐1.74; 2 trials, 99 participants) (low‐quality evidence).
Six trials compared orthodontic treatment for adolescents with Twin Block versus other appliances and found no difference in overjet (0.08 mm, 95% CI −0.60 to 0.76; 4 trials, 259 participants) (low‐quality evidence). The reduction in ANB favoured treatment with a Twin Block (−0.56°, 95% CI −0.96 to −0.16; 6 trials, 320 participants) (low‐quality evidence).
Three trials compared orthodontic treatment for adolescents with removable functional appliances versus fixed functional appliances and found a reduction in overjet in favour of fixed appliances (0.74, 95% CI 0.15 to 1.33; two trials, 154 participants) (low‐quality evidence), and a reduction in ANB in favour of removable appliances (−1.04°, 95% CI −1.60 to −0.49; 3 trials, 185 participants) (low‐quality evidence).
Authors' conclusions
Evidence of low to moderate quality suggests that providing early orthodontic treatment for children with prominent upper front teeth is more effective for reducing the incidence of incisal trauma than providing one course of orthodontic treatment in adolescence. There appear to be no other advantages of providing early treatment when compared to late treatment. Low‐quality evidence suggests that, compared to no treatment, late treatment in adolescence with functional appliances, is effective for reducing the prominence of upper front teeth.
PICOs
Plain language summary
Orthodontic treatment for prominent upper front teeth in children
Review question
This review, carried out by authors working with Cochrane Oral Health , has been produced to assess the effects of orthodontic treatment (treatment by dentists who specialise in the growth, function and position of teeth and jaws) for prominent upper front teeth in children. The review looks at whether this treatment is best initiated at seven to 11 years old (early treatment in two phases), or in adolescence, at around age 12 to 16 years (late treatment in one phase). The use of different types of braces was also assessed.
Background
Prominent (or sticking out) upper front teeth are a common problem in children around the world. For example, this condition affects about a quarter of 12‐year‐old children in the UK. The correction of this condition is one of the most common treatments performed by orthodontists (dentists who specialise in the growth, function and position of teeth and jaws). This condition develops when the child's permanent teeth erupt. Children are often referred to an orthodontist, for treatment with dental braces, to reduce the prominence of the teeth. Prominent upper front teeth are more likely to be injured and their appearance can cause significant distress.
If a child is referred at a young age, the orthodontist is faced with the dilemma of whether to treat the patient early or to wait until the child is older and provide treatment in adolescence.
In 'early treatment', treatment is given in two phases: first at an early age (seven to 11 years old) and again in adolescence (around 12 to 16 years old). In 'late treatment' (one phase), there is only one course of treatment in adolescence.
As well as the timing of treatment, this review also looked at the different types of braces used: removable, fixed, functional, or head‐braces.
Study characteristics
This review is based on 27 studies including 1251 participants. Participants were children and adolescents aged under 16 years who had prominent upper front teeth (Class II Division 1 malocclusion). The evidence in this review is up to date as of 27 September 2017.
Key results
The evidence suggests that providing orthodontic early treatment to children with prominent upper front teeth reduces the incidence of damage to upper incisor teeth significantly (middle four teeth at the top) as compared to treatment that is provided in one phase in adolescence. There are no other advantages of providing a two‐phase treatment (i.e. between age seven to 11 years and again in adolescence) compared to treatment in one phase in adolescence.
The evidence also suggests that providing treatment with functional appliances for adolescents with prominent upper front teeth, significantly reduces their prominence when compared to adolescents who did not receive any treatment. The studies did not suggest that any particular appliance was better than any other for reducing teeth prominence.
Quality of the evidence
The overall quality of the evidence is low for most comparisons and outcomes, therefore further research is needed and may change the findings.
Authors' conclusions
Summary of findings
| Early treatment (two‐phase: phase one in childhood and phase two in adolescence) versus late treatment (one‐phase in adolescence) with functional appliance | ||||||
| Patient or population: children and/or adolescents (age ≤ 16 years) receiving orthodontic treatment to correct prominent upper front teeth Intervention: early treatment with functional appliance Comparison: late treatment with functional appliance | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | Number of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Late treatment with functional appliance | Early treatment with functional appliance | |||||
| Overjet (mm) (smaller value better) Follow‐up at end of orthodontic treatment | Mean final overjet ranged across control groups from 2.6 mm to 4.3 mm | Mean final overjet 0.21 mm more (0.10 mm less to 0.51 mm more) | 343 (3) | ⊕⊕ low2 3 | The functional appliance reduced overjet compared to no treatment at the end of the first phase of early treatment (MD −4.17, −4.61 to −3.73; 432 participants). | |
| Incidence of incisal trauma Follow‐up at end of orthodontic treatment | 298 per 10001 | 192 per 1000 (123 to 288) | OR 0.56 (0.33 to 0.95) | 332 (3) | ⊕⊕⊕ moderate2 | |
| ANB (°) Follow‐up at end of orthodontic treatment | Mean final ANB ranged across control groups from 3.7° to 4.0° | Mean final ANB 0.02° less (0.47° less to 0.43° more) | 347 (3) | ⊕⊕⊕ moderate2 | The functional appliance improved ANB at the end of the first phase of early treatment when compared with no treatment (MD −0.89, −1.38 to −0.40; 419 participants). | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI) | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Based on average in control groups | ||||||
| Early treatment (two‐phase: phase 1 in childhood and phase 2 in adolescence) with headgear appliance versus late treatment (one‐phase in adolescence) with headgear | ||||||
| Patient or population: children and/or adolescents (age ≤ 16 years) receiving orthodontic treatment to correct prominent upper front teeth Intervention: early treatment with headgear Comparison: late treatment with headgear | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Late treatment with headgear | Early treatment with headgear | |||||
| Overjet (mm) (smaller value better) Follow‐up at end of orthodontic treatment | Mean final overjet ranged across control groups from 2.4 mm to 3.48 mm | Mean final overjet in the 2‐phase treatment group was 0.22 mm less (0.56 mm less to 0.12 mm more) | 238 (2) | ⊕⊕ low2 | Headgear reduced overjet compared to no treatment at the end of the first phase of early treatment (MD −1.07, −1.63 to −0.51; 278 participants). | |
| Incidence of incisal trauma Follow‐up at end of orthodontic treatment | 367 per 10001 | 207 per 1000 (126 to 317) | OR 0.45 (0.25 to 0.80) | 237 (2) | ⊕⊕ low2 | |
| ANB (°) Follow‐up at end of orthodontic treatment | Mean final ANB ranged across control groups from 3.3° to 4.0° | Mean final ANB 0.27° less (0.80° less to 0.26° more) | 231 (2) | ⊕⊕ low2 | Headgear improved ANB compared to no treatment at the end of the first phase of early treatment (MD −0.72, −1.18 to −0.27; 277 participants). | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI) | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Based on average in control groups | ||||||
| Late treatment (one‐phase in adolescence) with functional appliance versus no treatment for prominent upper front teeth (Class II malocclusion) | ||||||
| Patient or population: adolescents (age between 12 and 16 years) receiving orthodontic treatment to correct prominent upper front teeth | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | Number of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| No treatment | Late treatment with functional appliances | |||||
| Fixed functional appliances | ||||||
| Overjet (mm) (smaller value better) Follow‐up at end of orthodontic treatment | Mean final overjet ranged from 7.47 to 10.56 mm | Mean final overjet was 5.46 mm lower | 61 | ⊕⊕⊝⊝ | ||
| Incidence of incisal trauma | Not measured | |||||
| ANB (°) Follow‐up at end of orthodontic treatment | Mean final ANB ranged from 6.30° to 7.92° | Mean final ANB was 0.53° lower | 89 | ⊕⊕⊝⊝ | ||
| Removable functional appliances | ||||||
| Overjet (mm) (smaller value better) Follow‐up at end of orthodontic treatment | Mean final overjet ranged from 7.8 to 9.9 mm | Mean final overjet was 4.62 mm lower (5.33 lower to 3.92 lower) | 122 | ⊕⊕⊝⊝ | ||
| Incidence of incisal trauma | Not measured | |||||
| ANB (°) Follow‐up at end of orthodontic treatment | Mean final ANB ranged from 6.5° to 6.53° | Mean final ANB was 2.37° lower | 99 | ⊕⊕⊝⊝ | ||
| 1 Downgraded one level as both studies were at unclear risk of bias and one level because of very high heterogeneity (I² = 95%) 2 Downgraded one level as the three studies were at unclear risk of bias and one level for moderate heterogeneity (I² = 51%) 3 Downgraded two levels as both studies were at high risk of bias | ||||||
| Late treatment (one‐phase in adolescence): comparison among different types of appliances used for treatment of prominent upper front teeth (Class II malocclusion) | ||||||
| Patient or population: adolescents (age between 12 and 16 years) receiving orthodontic treatment to correct prominent upper front teeth | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | № of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Different types of appliances | Twin Block | |||||
| Overjet (mm) (smaller value better) Follow‐up at end of orthodontic treatment | Mean final overjet ranged from 2.68 mm to 4.40 mm | Mean final overjet was 0.08 mm higher | 259 | ⊕⊕⊝⊝ | ||
| Incidence of Incisal trauma | Not measured | |||||
| ANB (°) Follow‐up at end of orthodontic treatment | Mean final ANB ranged from 3.63° to 5.00° | Mean final ANB was −0.56° lower | 320 | ⊕⊕⊝⊝ | ||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI) | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded as 2 of 4 studies were at high risk of bias 2 Dowgraded due to heterogeneity (heterogeneity: Tau² = 0.25; Chi² = 6.61, df = 3 (P = 0.09); I² = 55%) 3 Downgraded as 3 of 6 studies were at high risk of bias 4 Downgraded as the interventions in the comparison groups were not similar | ||||||
| Late treatment in adolescence (one‐phase): comparison among different types of appliances used for treatment of prominent upper front teeth (Class II malocclusion) | ||||||
| Patient or population: adolescents (age between 12 and 16 years) receiving orthodontic treatment to correct prominent upper front teeth Intervention: Removable funtional appliance | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | Number of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Fixed functional appliance | Removable functional appliance | |||||
| Overjet (mm) (smaller value better) Follow‐up at end of orthodontic treatment | Mean final overjet ranged from 0.95 mm to 3.53 mm | Mean final overjet was 0.74 mm higher (0.15 lower to 1.33 higher) | 154 | ⊕⊕⊝⊝ | ||
| Incidence of Incisal trauma | Not measured | |||||
| ANB (°) Follow‐up at end of orthodontic treatment | Mean final ANB ranged from 4.40° to 5.88° | Mean final ANB was 1.04° lower | 185 | ⊕⊕⊝⊝ | ||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI) | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded due to inconsistency (interventions were not similar between studies) 2 Downgraded twice as both studies were at high risk of bias 3 Downgraded due to inconsistency (interventions were not similar between studies) 4 Downgraded twice as 3 trials were at high risk of bias | ||||||
Background
Description of the condition
Orthodontics is the branch of dentistry concerned with the growth of the jaws and face, the development of the teeth and the way the teeth and jaws bite together. It also involves treatment of the teeth and jaws when they are irregular or bite in an abnormal way or both. There are many reasons why the teeth may not bite together correctly. These include the position of the teeth, jaws, lips, tongue, or cheeks; or may be due to heredity, a habit or the way people breathe. The need for orthodontic treatment can be decided by looking at the effect any particular tooth position has on the life expectancy of the teeth, or the effect that the appearance of the teeth has on how people feel about themselves, or both (Shaw 1991).
Prominent upper front teeth (Class II malocclusion) may be due to any combination of the jaw, tooth and lip position. The upper jaw (maxilla) can be too far forward or, more usually, the lower jaw (mandible) is too far back. The upper front teeth (incisors) may stick out if the lower lip catches behind them or due to a habit (e.g. thumb sucking). This gives the patient an appearance that may be a target for teasing (Shaw 1980) and bullying (Seehra 2011), which impacts on quality of life (Johal 2007; Silva 2016). When front teeth stick out (more than 3 mm to 5 mm), they are two to three times more likely to be injured (Frujeri 2014; Nguyen 1999). Prominent upper front teeth (Class II malocclusion) is one of the most common problems seen by orthodontists and affects about a quarter of 12‐year‐old children in the UK (Holmes 1992). However, there are racial differences: prominent upper front teeth (Class II malocclusion) are most common in whites of Northern European origin and least common in black and oriental races and some Scandinavian populations (El‐Mangoury 1990; Proffit 1993; Silva 2001).
Description of the intervention
Several dental brace (orthodontic) treatments have been suggested to correct prominent upper front teeth (Class II malocclusions). Some treatments aim to move the upper front teeth backwards (with or without the extraction of teeth) whilst others aim to modify the growth of the upper or lower jaw or both to reduce the prominence of the upper front teeth. Treatment can involve the use of one or more types of orthodontic brace.
How the intervention might work
Some braces apply a force directly to the teeth and can either be removed from the mouth or fixed to the teeth, with special glue, during treatment. Other types of brace are attached, via the teeth, to devices (headgear) that allow a force to be applied to the teeth and jaws from the back of the head. Treatment is usually carried out either early (early treatment), when a mixture of baby and adult teeth are present (around seven to 11 years of age) or later (adolescent treatment) when all the adult teeth have come into the mouth (around 12 to 16 years of age). In severe cases and some adults, orthodontic treatment may need to be combined with jaw surgery to correct the position of one or both jaws.
Why it is important to do this review
Cochrane Oral Health undertook an extensive prioritisation exercise in 2014 to identify a core portfolio of titles that were the most clinically important ones to maintain in the Cochrane Library (Worthington 2015). This review was identified as a priority title by the orthodontic expert panel (Cochrane OHG priority review portfolio).
The correction of prominent upper front teeth is one of the most common treatments performed by orthodontists. Even though we have several brace types to correct prominent upper front teeth, new braces are being introduced in the market to overcome the drawbacks of previous ones and there is a need to establish the relative effectiveness of the different braces that can be used. It is very important that we identify the most effective type of brace to give the best available treatment.
Objectives
To assess the effects of orthodontic treatment for prominent upper front teeth initiated when children are seven to 11 years old ('early treatment' in two phases) compared to in adolescence when they are around 12 to 16 years old ('late treatment' in one phase); to assess the effects of late treatment compared to no treatment; and to assess the effects of different types of orthodontic braces.
Methods
Criteria for considering studies for this review
Types of studies
All randomised controlled trials of orthodontic treatments to correct prominent upper front teeth (Class II, Division 1 malocclusion).
Types of participants
Children (seven to 11 years old) and adolescents (usually 12 to 16 years old) receiving orthodontic treatment to correct prominent upper front teeth (Class II malocclusion).
We excluded trials including participants with a cleft lip or palate or both, or other craniofacial deformity/syndrome. We also excluded trials that recruited patients who had previously received surgical treatment for their Class II malocclusion.
Types of interventions
-
Early treatment (two‐phase) in childhood with any type of orthodontic brace (removable, fixed, functional) or head‐brace compared with late treatment in adolescence (in one phase) with any type of orthodontic brace (removable, fixed, functional) or head‐brace.
-
Any type of orthodontic brace (removable, fixed, functional) or head‐brace compared with no treatment or another type of orthodontic brace or appliance. For this comparison, treatment should have been started in children of similar ages in both groups.
Types of outcome measures
We recorded clinically important outcomes at the most common endpoints that were reported. If we identified harms, these were recorded and reported in descriptive terms.
Primary outcomes
-
Prominence of the upper front teeth (overjet measured in millimetres or by any index of malocclusion).
Secondary outcomes
-
Relationship between upper and lower jaws measured, for example, by ANB angle.
-
Self‐esteem and patient satisfaction.
-
Any injury to the upper front teeth (i.e. incisal trauma).
-
Jaw joint problems.
-
Number of attendances required to complete treatment.
-
Harms such as health of the gums, damage to the teeth (e.g. tooth decay).
-
Standard of orthodontic treatment.
Search methods for identification of studies
Electronic searches
Cochrane Oral Health’s Information Specialist conducted systematic searches of the following databases for randomised controlled trials and controlled clinical trials. There were no language, publication year or publication status restrictions.
-
Cochrane Oral Health’s Trials Register (searched 27 September 2017) (Appendix 1).
-
Cochrane Central Register of Controlled Trials (CENTRAL; 2017, Issue 8) in the Cochrane Library (searched 27 September 2017) (Appendix 2).
-
MEDLINE Ovid (1946 to 27 September 2017) (Appendix 3).
-
Embase Ovid (1980 to 27 September 2017) (Appendix 4).
Subject strategies were modelled on the search strategy designed for MEDLINE Ovid. Where appropriate, they were combined with subject strategy adaptations of the Highly Sensitive Search Strategy designed by Cochrane for identifying randomised controlled trials and controlled clinical trials as described in the Cochrane Handbook for Systematic Reviews of Interventions, Chapter 6 (Lefebvre 2011).
Searching other resources
The following trial registries were searched for ongoing studies:
-
US National Institutes of Health Ongoing Trials Register (ClinicalTrials.gov; searched 29 September 2017) (Appendix 5).
-
World Health Organization International Clinical Trials Registry Platform (apps.who.int/trialsearch; searched 29 September 2017) (Appendix 6).
We handsearched the following journals.
-
Seminars in Orthodontics (from 1995 to December 2006).
-
Clinical Orthodontics and Research (from 1998 to December 2001).
-
Orthodontics & Craniofacial Research (from 2001 to December 2006).
-
Australian Orthodontic Journal (from 1956 to December 2006).
We checked the bibliographies of the clinical trials that we identified for references to trials published outside the handsearched journals, including personal references. We contacted the first named authors of all trial reports in an attempt to identify unpublished studies and to obtain any further information about the trials.
We searched the reference lists of included studies and relevant systematic reviews for further studies.
We did not perform a separate search for adverse effects of interventions used, we considered adverse effects described in included studies only.
Data collection and analysis
Selection of studies
Two review authors (KB and BT or BT and JH), independently and in duplicate, assessed the eligibility of all reports that were identified by the search strategy as being potentially relevant to the review. They were not blinded to author(s), institution or site of publication. Disagreements were resolved by discussion or following clarification from authors.
Data extraction and management
Two review authors (KB and BT or BT and JH) extracted data (independently and in duplicate) using a specially designed data extraction form. We recorded the year of publication, interventions assessed, outcomes, sample size and age of subjects. We grouped the outcome data into those measured at the end of treatment provided for young children and at the end of treatment provided for adolescent children.
Assessment of risk of bias in included studies
This was conducted using the recommended approach for assessing risk of bias in studies included in Cochrane Reviews (Higgins 2011). We used the two‐part tool, addressing six specific domains (namely sequence generation; allocation concealment; blinding of outcome assessors; incomplete outcome data; selective outcome reporting; and other bias). Each domain included one specific entry in a 'Risk of bias' table. Within each entry, the first part of the tool involved describing what was reported to have happened in the study. The second part of the tool involved assigning a judgement relating to the risk of bias for that entry, either 'low risk', 'high risk' or, where there was insufficient information on which to base a judgement, 'unclear risk'.
The risk of bias assessments were undertaken independently and in duplicate by two review authors (KB and BT or BT and JH) as part of the data extraction process with assistance from Cochrane Oral Health when necessary.
After taking into account the additional information provided by the authors of the trials, we grouped studies into the following categories.
-
Low risk of bias (plausible bias unlikely to seriously alter the results) if all key domains were assessed as low.
-
Unclear risk of bias (plausible bias that raises some doubt about the results) if one or more key domains were assessed as unclear.
-
High risk of bias (plausible bias that seriously weakens confidence in the results) if one or more key domains were assessed to be at high risk of bias.
A 'Risk of bias' table was completed for each included study and results were presented graphically.
Measures of treatment effect
For dichotomous outcomes, we expressed the estimates of effect of an intervention as odds ratios together with 95% confidence intervals (CIs). For continuous outcomes, we used mean differences, together with 95% CIs, to summarise the data for each group.
Assessment of heterogeneity
The significance of any discrepancies in the estimates of the treatment effects from the different trials was assessed by means of Cochrane's test for heterogeneity and the I² statistic, which describes the percentage total variation across studies that is due to heterogeneity rather than chance.
Data synthesis
We performed meta‐analysis only if there were studies with similar comparisons that reported the same outcome measures. We combined odds ratios for dichotomous data, and mean differences for continuous data, using random‐effects models if there were four or more studies in the meta‐analysis, and fixed‐effect models if there were up to three studies.
Subgroup analysis and investigation of heterogeneity
We assessed clinical heterogeneity by examining the types of participants and interventions for all outcomes in each study.
Sensitivity analysis
We had planned to undertake sensitivity analyses to examine the effect of the study risk of bias assessment on the overall estimates of effect. In addition, we planned to examine the effect of including unpublished literature, but there were insufficient trials to undertake this.
Summarising findings
We created 'Summary of findings' (SoF) tables to record results of the main outcomes (overjet, incisal trauma and ANB) for the main comparisons: early treatment using a functional appliance versus late treatment; early treatment using headgear versus late treatment; late treatment with functional appliances versus no treatment; late treatment with different appliances (two tables). We assessed the quality of the evidence using GRADE.
Results
Description of studies
Results of the search
The initial review was published in 2007. Searches to date (September 2017) have identified a total of 2319 records (910 after duplicates removed), of which we assessed 181 records in full text. Of these 181 records, we excluded 104 articles and we considered a further 14 irrelevant. Twenty‐seven trials (published in 63 papers) met the inclusion criteria. See Figure 1.

Study flow diagram
Included studies
See Characteristics of included studies table for details of included studies.
Characteristics of the trial settings and investigators
Of the 27 included trials, seven were conducted in the United Kingdom (Banks 2004; Lee 2007; London 1998; Thiruvenkatachari 2010; UK (11‐14) 2003; UK (Mixed) 2009; Yaqoob 2012); three were carried out in North America (Florida 1998; Ghafari 1998; North Carolina 2004); two were conducted in China (Mao 1997; Jin 2015); one in New Zealand (New Zealand 2000); one in Australia (Bilgiç 2011); four in Turkey (Aras 2017a; Aras 2017b; Cura 1997; Baysal 2014); two in Iran (Jamilian 2011; Showkatbakhsh 2011); two in Syria (Alali 2014; Burhan 2015); one in Brazil (Cevidanes 2003); one in Italy (Martina 2013); two in Egypt (Eissa 2017; Elkordy 2016); and one in Sweden (Cirgić 2016). All trials had a parallel‐group design. Five were multicentre studies (Banks 2004; Thiruvenkatachari 2010; UK (11‐14) 2003; UK (Mixed) 2009; Cirgić 2016). Eleven of the trials had more than one publication. Seven of the trials received external funding. The providers and assessors were dental staff.
Characteristics of the participants
For the 27 trials included in the review, the results are based on data from 1251 participants who presented with prominent upper front teeth (Class II Division 1 malocclusion). The number of participants in each treatment or control group ranged from 12 to 105.
Four trials provided treatment for children aged between 7 and 11 years old (Florida 1998; Ghafari 1998; North Carolina 2004; UK (Mixed) 2009). One trial provided treatment for children who were 7 to 14 years old (Cirgić 2016). Two trials provided treatment for children aged between 8 and 11 years (Mao 1997; Showkatbakhsh 2011). Three trials provided treatment for children aged between 9 and 13 years old (Cevidanes 2003; Jamilian 2011; Martina 2013). One trial provided treatment for children who were 10 to 13 years old (New Zealand 2000). Twenty provided treatment for children who were 10 to 15 years old (Alali 2014; Aras 2017a; Aras 2017b; Banks 2004; Baysal 2014; Burhan 2015; Bilgiç 2011; Cura 1997; Eissa 2017; Elkordy 2016; Jin 2015; Lee 2007; London 1998; Thiruvenkatachari 2010; UK (11‐14) 2003; Yaqoob 2012).
Two of the trials had an active recruitment strategy that involved screening school children and providing incentives, such as reduced fees for participation (Florida 1998; North Carolina 2004).
The percentage of participants lost to follow‐up varied from 0% to 26%.
Characteristics of the intervention
All of the trials provided a clear description of the treatment protocols.
We classified the interventions for the treatment of Class II malocclusion as follows.
Early treatment (two‐phase) for Class II Division 1 malocclusion
-
There were three trials that compared early treatment (two‐phase) with late treatment (one‐phase) (Florida 1998; North Carolina 2004; UK (Mixed) 2009).
-
Three trials compared two different types of appliances for early treatment (Florida 1998; Ghafari 1998; North Carolina 2004).
In this group of trials, treatment of Class II division 1 malocclusion started when participants were aged nine years and comprised two treatment phases. In phase one, participants were randomised to receive one of two types of appliance or to a control group that received no early treatment. When phase one of the trials was completed, participants who had early treatment had a second phase of treatment, and participants who were in the no treatment group had one single phase of adolescent treatment. Outcome measures were compared between those who had received both early and late treatment and those who received late treatment only.
Late treatment in adolescence (one‐phase) for Class II Division 1 malocclusion
-
Nine trials compared functional appliances with no treatment (Alali 2014; Baysal 2014; Cevidanes 2003; Cura 1997; Eissa 2017; Elkordy 2016; Mao 1997; Martina 2013; New Zealand 2000). As Baysal 2014 did not randomise participants to the 'no treatment' arm, we did not include their results for the functional versus no treatment comparison.
-
Eighteen trials compared different types of appliances.
-
-
Twin Block appliances were compared with other types of appliances in eight trials (Baysal 2014; Burhan 2015; Jamilian 2011; Jin 2015; Lee 2007; London 1998; Thiruvenkatachari 2010; UK (11‐14) 2003).
-
Twin Block appliances were compared with various modifications to twin blocks in two trials (Banks 2004; Yaqoob 2012).
-
Andresen activator was compared with a prefabricated functional appliance in one trial (Cirgic 2016).
-
Forsus Fatigue Resistance Device was compared to Forsus Fatigue Resistance Device and mini‐implants in two trials (Eissa 2017; Elkordy 2016).
-
R‐appliance was compared with Anterior Inclined Bite Plate in one trial (Showkatbakhsh 2011).
-
Removable functional appliances were compared to fixed functional appliances in three trials (Baysal 2014; Bilgiç 2011; UK (11‐14) 2003).
-
Forsus Fatigue Resistance Device was compared with intermaxillary elastics in one trial (Aras 2017b).
-
Functional mandibular advancer was compared for stepwise versus single step advancement (Aras 2017a).
-
Harvold Activator was compared with Frankel function regulator (New Zealand 2000)
-
Outcome measures in the included studies
The primary outcome measure was the prominence of the upper front teeth (overjet measured in millimetres or by any index of malocclusion), and this was included in all studies. We also measured the relationship between upper and lower jaws (ANB angle measured in degrees), self‐esteem and patient satisfaction (measured using reported questionnaires), any injury to the upper front teeth, jaw joint problems, number of attendances required to complete treatment, harms to gums, damage to the teeth and the standard of orthodontic treatment (measured using PAR scores ‒ Peer Assessment Rating index). The majority of the studies presented results for late orthodontic treatment in adolescence. Three trials reported on final overjet, final ANB, final PAR score and incidence of new incisal trauma for early treatment (Florida 1998; North Carolina 2004; UK (Mixed) 2009). One trial reported self‐concept in early treatment (UK (Mixed) 2009).
Excluded studies
We excluded 104 studies. The main reasons for exclusion were as follows. See Characteristics of excluded studies table for further details.
-
85 were not RCTs;
-
4 had only abstracts and did not have sufficient information to determine whether they met the inclusion criteria of the review;
-
4 did not involve treatment of people with a Class II Division 1 malocclusion (or they were only a small proportion of participants);
-
4 included Class II division 2 participants;
-
5 included adults;
-
1 had no information on overjet and ANB;
-
1 was imaging study of TMJ.
Risk of bias in included studies
Allocation
Sequence generation
In 16 studies (Aras 2017a; Aras 2017b; Banks 2004; Baysal 2014; Burhan 2015; Eissa 2017; Elkordy 2016; Jamilian 2011; Jin 2015; Martina 2013; North Carolina 2004; Showkatbakhsh 2011; Thiruvenkatachari 2010; UK (11‐14) 2003; UK (Mixed) 2009; Yaqoob 2012), the method of random sequence generation was clearly described and these studies were assessed as being at low risk of bias for this domain. Ten of these studies used minimisation software as a method of sequence generation (Aras 2017a; Aras 2017b; Banks 2004; Burhan 2015; Eissa 2017; Elkordy 2016; Martina 2013; Thiruvenkatachari 2010; UK (11‐14) 2003; UK (Mixed) 2009). One study used stratified block randomisation (Yaqoob 2012), four studies used random number tables (Baysal 2014; Jamilian 2011; Jin 2015; Showkatbakhsh 2011) and one used Proc plan in SAS (North Carolina 2004). Nine studies did not report on the method of random sequence generation and were judged at unclear risk of bias (Alali 2014; Cevidanes 2003; Cirgić 2016; Cura 1997; Ghafari 1998; Lee 2007; London 1998; Mao 1997; New Zealand 2000) . Two studies were judged to be at high risk of bias (Bilgiç 2011; Florida 1998). Florida 1998 reported an inadequate method of randomisation, filling up the partially filled blocks in stratified block randomisation due to slow rate of entry. Bilgiç 2011 reported that participants were selected and matched between groups according to the inclusion criteria. Additionally, they did not report the method of random sequence generation.
Allocation concealment
In eight studies (Banks 2004; Eissa 2017; Elkordy 2016; Martina 2013; Thiruvenkatachari 2010; UK (11‐14) 2003; UK (Mixed) 2009; Yaqoob 2012), allocation concealment was clearly described and therefore these studies were judged at low risk of bias for this domain. Eighteen studies did not report any information about allocation concealment and were assessed as being at unclear risk of bias for this domain (Aras 2017a; Aras 2017b; Alali 2014; Baysal 2014; Bilgiç 2011; Burhan 2015; Cevidanes 2003; Cirgić 2016; Cura 1997; Florida 1998; Ghafari 1998; Jamilian 2011; Jin 2015; Lee 2007; London 1998; Mao 1997; North Carolina 2004; Showkatbakhsh 2011). One study reported that randomisation was matched in triads according to age and sex and randomly assigned to the three intervention groups (New Zealand 2000). It is possible that allocation could be predictable within the triad time. As a result, we felt that this study was at high risk of bias for this domain (New Zealand 2000).
Blinding
Blind assessment of all outcomes was reported in 13 studies and these were assessed as at low risk of bias (Aras 2017a; Aras 2017b; Alali 2014; Banks 2004; Burhan 2015; Cevidanes 2003; Elkordy 2016; Florida 1998; Jamilian 2011; Martina 2013; UK (11‐14) 2003; UK (Mixed) 2009; Yaqoob 2012). Blind outcome assessment was not reported in 10 studies and they were judged at unclear risk of bias (Bilgiç 2011; Cura 1997; Eissa 2017; Ghafari 1998; Jin 2015; Lee 2007; London 1998; Mao 1997; New Zealand 2000; Showkatbakhsh 2011). An additional study reported clinical measures only and blinding was not possible. This was judged to be at unclear risk of bias (Thiruvenkatachari 2010). Three studies stated that the assessors were not blinded and were judged at high risk of bias (Baysal 2014; Cirgić 2016; North Carolina 2004).
Incomplete outcome data
Trials of orthodontic treatment for Class II division 1 malocclusion typically last for at least five or more years and consequently there is a high rate of attrition, some of which is related to the orthodontic treatment offered, and some due to factors such as families moving to a different area. Attrition rates in the studies included in this review ranged from 6% to 28% of participants initially randomised to treatments. In assessing risk of attrition bias, we looked at the overall rate of attrition in the study, the relative loss for each arm of each study and the reasons given to explain these.
We assessed 11 studies as being at low risk of attrition bias (Aras 2017a; Aras 2017b; Baysal 2014; Bilgiç 2011; Burhan 2015; Jamilian 2011; Jin 2015; Lee 2007; Showkatbakhsh 2011; UK (Mixed) 2009; Yaqoob 2012). UK (Mixed) 2009 had high overall attrition (19%) but the reasons given and the numbers were similar in each treatment arm and we considered that attrition bias was unlikely. Yaqoob 2012 had low overall attrition (6%) and reasons and numbers were similar in each treatment arm.
A further eight studies were assessed as being at unclear risk of attrition bias (Alali 2014; Cirgić 2016; Cevidanes 2003; Eissa 2017; Elkordy 2016; Mao 1997; North Carolina 2004; Thiruvenkatachari 2010). In two of these studies (Cevidanes 2003; North Carolina 2004), the overall rate of attrition was 10% to 19%, but there was incomplete information on the rates and reasons for participants being excluded from the analysis in each treatment group within the study. In Alali 2014 the overall rate of attrition was 13% but there were more dropouts in the treatment (four participants, 16%) than in the control group (one participant, 5%). Mao 1997 provided no information about the number of participants included in the outcome evaluation. The study by Thiruvenkatachari 2010 was stopped early and had more than twice as many participants lost from the Twin Block treatment group compared to the Dynamax group. One study reported 46% attrition rate for one of the outcomes measured (Cirgić 2016). Cirgić 2016 also presented an imbalance between the treated groups with 43 participants analysed in one group and 62 in the other group. One study reported uneven dropout rates between groups and was therefore judged as unclear risk (Eissa 2017). In Elkordy 2016 there was no loss in the treated groups, but there was a loss of 20% in the control group.
We assessed the remaining eight studies as being at high risk of attrition bias (Banks 2004; Cura 1997; Florida 1998; Ghafari 1998; London 1998; Martina 2013; New Zealand 2000; UK (11‐14) 2003). Seven of these studies had more than 20% attrition and a significant difference in the rate and reason for participants being excluded from the analysis in each arm of the study (Banks 2004; Cura 1997; Florida 1998; Ghafari 1998; London 1998; Martina 2013; New Zealand 2000). UK (11‐14) 2003 had a lower overall attrition rate of 15% but the dropout rate was significantly different between groups.
Selective reporting
Twenty‐four studies reported all of the outcomes specified in the methodology and were judged at low risk of reporting bias (Alali 2014; Aras 2017a; Aras 2017b; Banks 2004; Baysal 2014; Bilgiç 2011; Burhan 2015; Cirgić 2016; Cura 1997; Eissa 2017; Elkordy 2016; Florida 1998; Ghafari 1998; Jamilian 2011; Jin 2015; Lee 2007; London 1998; Martina 2013; New Zealand 2000; North Carolina 2004; Thiruvenkatachari 2010; UK (11‐14) 2003; UK (Mixed) 2009; Yaqoob 2012). One study reported only on a few cephalometric measurements and no clinical measurements so was judged to be at unclear risk of bias (Showkatbakhsh 2011). One study used a complicated reporting method from which data could not be extracted for meta‐analysis and this study was judged at unclear risk of reporting bias (Cevidanes 2003). The study by Mao 1997 had reported data, but these were not clear and data could not be extracted for meta‐analysis, so this study was also assessed at unclear risk of reporting bias.
Other potential sources of bias
There was no other potential source of bias identified in 18 studies and these were judged to be at low risk of bias (Aras 2017a; Alali 2014; Banks 2004; Baysal 2014; Bilgiç 2011; Burhan 2015; Eissa 2017; Florida 1998; Ghafari 1998; Jamilian 2011; Jin 2015; Martina 2013; New Zealand 2000; North Carolina 2004; Showkatbakhsh 2011; UK (11‐14) 2003; UK (Mixed) 2009; Yaqoob 2012).
Five studies were judged as being at unclear risk of other bias (Cevidanes 2003; Cirgić 2016; Elkordy 2016; Lee 2007; London 1998). One study did not report baseline characteristics of the groups (Cevidanes 2003). One study did not present the age of participants at baseline (Cirgić 2016). The sample of one study had only females (Elkordy 2016). One study had differences in age at baseline between randomised groups. Although this was not statistically significant (which may be due to small numbers in each group), this study was assessed as at unclear risk of other bias (London 1998). Two studies found a higher incidence of appliance breakages in the Dynamax group than in the Twin Block group (Lee 2007; Thiruvenkatachari 2010). Cirgić 2016 stopped recruitment midway and therefore had uneven numbers between groups.
Four studies were assessed at high risk of other bias (Aras 2017b; Cura 1997; Mao 1997; Thiruvenkatachari 2010). Cura 1997 and Aras 2017b had gender imbalance at baseline between groups, which may have led to a bias due to the different responses of boys and girls to orthodontic treatment. Mao 1997 did not report data clearly and also had gender imbalance between groups at baseline (Bionator group 18 males, six females and untreated group nine males and 17 females). One study stopped prematurely due to excessive adverse events and a statistically significant difference between groups at the first interim analysis and so was assessed to be at high risk of bias (Thiruvenkatachari 2010).
Overall risk of bias
In summary, 15 studies were considered to be at high risk of bias in at least one domain and were therefore assessed to be at high risk of bias overall (Aras 2017b; Banks 2004; Baysal 2014; Bilgiç 2011; Cirgić 2016; Cura 1997; Florida 1998; Ghafari 1998; London 1998; Mao 1997; Martina 2013; New Zealand 2000; North Carolina 2004; Thiruvenkatachari 2010; UK (11‐14) 2003); two studies were considered to be at low overall risk of bias (UK (Mixed) 2009; Yaqoob 2012); and 10 studies at unclear overall risk of bias (Aras 2017a; Alali 2014; Burhan 2015; Cevidanes 2003; Eissa 2017; Elkordy 2016; Jamilian 2011; Jin 2015; Lee 2007; Showkatbakhsh 2011) (Figure 2).
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Effects of interventions
See: Summary of findings for the main comparison Early treatment (two‐phase: phase one in childhood and phase two in adolescence) versus late treatment (one‐phase in adolescence) with functional appliance; Summary of findings 2 Early treatment (two‐phase: phase 1 in childhood and phase 2 in adolescence) with headgear appliance versus late treatment (one‐phase in adolescence) with headgear; Summary of findings 3 Late treatment (one‐phase in adolescence) with functional appliance versus no treatment for prominent upper front teeth (Class II malocclusion); Summary of findings 4 Late treatment (one‐phase in adolescence): comparison among different types of appliances used for treatment of prominent upper front teeth (Class II malocclusion); Summary of findings 5 Late treatment (one‐phase in adolescence): comparison among different types of appliances used for treatment of prominent upper front teeth (Class II malocclusion)
We divided the trials into two main groups.
-
Early orthodontic treatment for Class II Division 1 malocclusion.
-
-
Comparison 1: early treatment (two‐phase: phase one in childhood (7 to 11 years) and phase two in adolescence (12 to 16 years)) versus late treatment (one‐phase in adolescence).
-
Outcomes at the end of phase one (Comparisons 1.1 to 1.4).
-
Outcomes at the end of phase two (Comparisons 1.5 to 1.8).
-
-
Comparison 2: early orthodontic treatment (two‐phase): different types of appliances.
-
Outcomes at the end of phase one (Comparisons 2.1 and 2.2).
-
Outcomes at the end of phase two (Comparisons 2.3 and 2.4).
-
-
-
Late orthodontic treatment in adolescence (one‐phase) for Class II Division 1 malocclusion.
-
-
Comparison 3: late treatment in adolescence with functional appliances versus no treatment (Comparison 3.1).
-
Comparison 4: different types of appliances used for late treatment in adolescence (Comparisons 4.1 to 4.10).
-
Four studies were not included in meta‐analysis (Cevidanes 2003; Ghafari 1998; Lee 2007; Thiruvenkatachari 2010).
Cevidanes 2003 looked at the effects of functional appliances (Frankel appliance) on the temporomandibular joint. This study did not carry out any dental measurements and therefore had no data to contribute to the meta‐analysis.
Ghafari 1998 did not publish data at the end of the study. Partial presentation of data in several interim publications could not be included in the analysis.
Lee 2007 reported medians and interquartile range and these non‐parametric data could not be used in the meta‐analysis. However, this study reported that there was no difference in overjet change between Twin Block and Dynamax appliances.
Thiruvenkatachari 2010 stopped this trial early due to harms. The incidence of adverse events with the Dynamax appliance (82%) was significantly greater than the Twin Block appliance (12%) (P value < 0.001) and the Twin Block appliance was more effective for overjet reduction. However, insufficient data were available to be used in the meta‐analysis.
Early orthodontic treatment (two‐phase) for Class II division 1 malocclusion
Early treatment (two‐phase) versus late treatment in adolescence (one‐phase)
Outcomes at the end of phase one
Treatment with functional appliance
Three trials (two at high risk of bias, one at low risk of bias) compared early treatment (two‐phase) using a functional appliance, with late treatment in adolescence (one‐phase) (Florida 1998; North Carolina 2004; UK (Mixed) 2009). Data were available comparing outcomes at the end of phase one for the early treatment group with observation only in the late treatment group. The meta‐analysis showed that there was a statistically significant difference in the overjet in favour of the treated group at the end of phase one (mean difference (MD) −4.17 mm, 95% confidence interval (CI) −4.61 to −3.73, Chi² = 117.02, 2 degrees of freedom (df), P value < 0.00001, I² = 98%; three studies, 432 participants) (Analysis 1.1).
When we evaluated the effect of treatment on final ANB, we found that there was a statistically significant mean difference between the treatment and control groups in favour of functional appliance treatment (MD −0.89°; 95% CI −1.38° to −0.40°, Chi² = 9.17, 2 df, P value = 0.0004, I² = 78%; three studies, 419 participants).
There was also a statistically significant effect on the PAR score in favour of early treatment (MD −10.52, 95% CI −12.32 to −8.71, Chi² = 52.23, 2 df, P value < 0.00001, I² = 98%; two studies, 249 participants) (Analysis 1.1).
Early treatment did not show any significant difference in self‐concept score (MD −3.63, 95% CI −7.66 to 0.40, P value = 0.08; one study, 135 participants) (Analysis 1.1); and incidence of new incisal trauma at the end of phase 1 (odds ratio (OR) 0.72, 95% CI 0.35 to 1.49, P value = 0.38; two trials, 281 participants) (Analysis 1.2) when compared with untreated control group participants.
Treatment with headgear
Two trials, both at high risk of bias, compared early treatment (two‐phase), using headgear, with late treatment in adolescence (one‐phase) (Florida 1998; North Carolina 2004). The comparison of the effect of treatment with headgear at the end of phase one (early treatment group), compared with observation (late treatment group), revealed a statistically significant effect of headgear treatment, in the reduction of the overjet (MD −1.07 mm, 95% CI −1.63 mm to −0.51 mm, Chi² = 0.05, 1 df, P value = 0.0002, I² = 0%; 278 participants) (Analysis 1.3). Similarly, headgear resulted in a statistically significant reduction of −0.72° (95% CI −1.18° to −0.27°, Chi² = 0.34, 1 df, P value = 0.002, I² = 0%; 277 participants) in final ANB (Analysis 1.3). However, there was no statistically significant difference in new incisal trauma (OR 0.76, 95% CI 0.37 to 1.54, Chi² = 0.66, 1 df, P value = 0.44, I² = 0%) between the two groups (Analysis 1.4).
Outcomes at the end of phase two
Treatment with functional appliance
Three trials (two at high risk of bias, one at low risk of bias) compared early treatment (two‐phase) with a functional appliance versus late treatment in adolescence (Florida 1998; North Carolina 2004; UK (Mixed) 2009). When we evaluated the effects of a course of treatment for children (one‐phase) with a functional appliance and at the end of all orthodontic treatment during adolescence (one‐phase), we found that there were no statistically significant differences in final overjet (MD 0.21 mm, 95% CI −0.10 mm to 0.51 mm, Chi² = 5.23, 2 df, P value = 0.18, I² = 62%; 343 participants) (Analysis 1.5), final ANB (MD −0.02°; 95% CI −0.47° to 0.43°, Chi² = 2.62, 2 df , P value = 0.92, I² = 24%; 347 participants) (Analysis 1.5), PAR score (MD 0.62, 95% CI −0.66 to 1.91, Chi² = 6.43, 2 df, P value = 0.34, I² = 69%; 360 participants) (Analysis 1.5), or self‐concept score (MD −0.83, 95% CI −3.97 to 2.31, P value = 0.60; one study, 132 participants). However, the incidence of new incisal trauma showed a statistically significant difference, in favour of early functional appliance treatment in childhood (two‐phase) (OR 0.56, 95% CI 0.33 to 0.95, Chi² = 1.98, 2 df, P value = 0.03, I² = 0%; 332 participants) (Analysis 1.6) compared with late orthodontic treatment during adolescence (one‐phase). The reduction in the incidence of new incisal trauma by the end of phase two was clinically significant with 30% (51/171) of participants reporting new trauma incidence in the late treatment group compared to only 19% (31/161) in the early treatment group.
Treatment with headgear when younger
Two trials, both at high risk of bias, compared early treatment (two‐phase), using headgear, with late treatment in adolescence (one‐phase) (Florida 1998; North Carolina 2004). There were no statistically significant effects of an early course of headgear treatment in childhood followed by treatment in adolescence with respect to final overjet (MD −0.22 mm, 95% CI −0.56 mm to 0.12 mm, Chi² = 1.27, 1 df, P value = 0.20, I² = 21%; 238 participants) (Analysis 1.7), final ANB (MD −0.27°, 95% CI −0.80° to 0.26°, Chi² = 0.10, 1 df, P value = 0.32, I² = 0%; 231 participants) (Analysis 1.7), or PAR score (MD −1.55, 95% CI −3.70 to 0.60, Chi² = 0.39, 1 df, P value = 0.16, I² = 0%; 177 participants) (Analysis 1.7) compared with one phase of treatment in adolescence. However, the incidence of new incisal trauma showed a statistically significant reduction in the earlier treatment (two‐phase) group (OR 0.45, 95% CI 0.25 to 0.80, Chi² = 1.15, 1 df, P value = 0.007, I² = 13%; 237 participants) (Analysis 1.8). The group who had late treatment in adolescence (one‐phase) suffered twice the incidence of new incisal trauma (44/120) as compared to the group who had early headgear treatment (two‐phase) in childhood (24/117).
Early orthodontic treatment in children (two‐phase): different types of appliances
Outcomes at the end of phase one
Two trials, at high risk of bias, compared the use of different types of appliances (headgear and functional appliance) for early treatment (two‐phase) (Florida 1998; North Carolina 2004). When we compared the effects of treatment with headgear or functional appliances in children, we found statistically significant differences with respect to final overjet (MD 0.75 mm, 95% CI 0.21 mm to 1.29 mm, Chi² = 12.54, 1 df, P value = 0.006, I² = 92%; 271 participants) (Analysis 2.1) in favour of functional appliances, but no difference in final ANB (MD −0.04°, 95% CI −0.49° to 0.41°, Chi² = 0.03, 1 df, P value = 0.85, I² = 0%; 271 participants) (Analysis 2.1), or new incisal trauma (OR 1.02, 95% CI 0.48 to 2.17, Chi² = 0.22, 1 df, P value = 0.95, I² = 0%; 282 participants) (Analysis 2.2).
Outcomes at the end of phase two
An evaluation of the effect of treatment between headgear and functional appliance in children followed by treatment in adolescence revealed no significant difference in final overjet (MD −0.21 mm, 95% CI −0.57 mm to 0.15 mm, Chi² = 0.01, 1 df, P value = 0.26, I² = 0%; 225 participants) (Analysis 2.3), final ANB (MD −0.17°, 95% CI −0.67° to 0.34°, Chi² = 1.58, 1 df, P value = 0.52, I² = 37%; 222 participants) (Analysis 2.3), PAR score (MD −0.81, 95% CI −2.21 to 0.58, Chi² = 0.09, 1 df, P value = 0.25, I² = 0%; 224 participants) (Analysis 2.3), or the incidence of incisal trauma (OR 0.78, 95% CI 0.42 to 1.47, Chi² = 0.08, 1 df, P value = 0.45, I² = 0%; 226 participants) (Analysis 2.4) (Florida 1998; North Carolina 2004).
Late orthodontic treatment in adolescence (one‐phase) for Class II Division 1 malocclusion
Late orthodontic treatment: functional appliance versus no treatment
Seven trials compared the use of functional appliances against no treatment. We decided, after considering the clinical and statistical heterogeneity, to analyse the trials according to the type of functional appliance: fixed or removable. Three trials evaluated fixed functional appliances (Alali 2014; Eissa 2017; Elkordy 2016), all of which were assessed as being at unclear risk of bias overall. The other four trials evaluated removable functional appliances and we assessed these trials as being at high risk of bias overall (Cura 1997; Mao 1997; Martina 2013; New Zealand 2000). The overall quality of the evidence was low.
There was evidence of a reduction in overjet with both removable functional appliances (MD −4.62, 95% CI ‐5.33 to ‐3.92, P < 0.00001; three trials, 122 participants) and fixed functional appliance (MD −5.46, 95% CI −6.63 to −4.28, P < 0.00001; two trials, 61 participants) when compared with no treatment (Analysis 3.1).
There was no evidence of a clear difference between use of the fixed appliance and no treatment for final ANB (MD −0.53, 95% CI −1.27 to −0.22, P = 0.17; three trials, 89 participants) (Analysis 3.2). However, the removable functional appliance reduced ANB significantly compared to no treatment (MD −2.37°, 95% CI ‐3.01 to ‐1.74, P < 0.00001; two trials, 99 participants) (Analysis 3.2).
Late orthodontic treatment: different types of appliances
Twin Block functional appliance versus other functional appliances
Four trials evaluated overjet (Burhan 2015; Jamilian 2011; London 1998; UK (11‐14) 2003). Two of them were at unclear risk of bias (Burhan 2015; Jamilian 2011); and two at high risk of bias (London 1998; UK (11‐14) 2003). There was no statistically significant effect of the type of appliance on final overjet (MD 0.08 mm, 95% CI −0.60 to 0.76, P = 0.83; 259 participants) (Analysis 4.1). Six trials evaluated ANB (Baysal 2014; Burhan 2015; Jamilian 2011; Jin 2015; London 1998; UK (11‐14) 2003). Three of them were at high risk of bias (Baysal 2014; London 1998; UK (11‐14) 2003); and three at unclear risk of bias (Burhan 2015; Jamilian 2011; Jin 2015). There was a statistically significant reduction in ANB with the Twin Block when compared to other functional appliances (MD −0.56°, 95% CI −0.96 to −0.16, P = 0.006; 320 participants) (Analysis 4.1).
Twin Block functional appliance versus other modifications of Twin Block appliances
Two trials compared a Twin Block functional appliance versus other modifications of Twin Block appliances; one trial was at high risk of bias and one at low risk of bias (Banks 2004; Yaqoob 2012). There were no statistically significant differences between the Twin Block designs with respect to final overjet (MD −0.23 mm, 95% CI −0.67 mm to 0.22 mm, Chi² = 2.59, 1 df, P value = 0.11, I² = 61%; 196 participants) (Analysis 4.2).
Activator functional appliance versus prefabricated myobrace appliance (PFA)
The results in this section are based on a single trial at high risk of bias (Cirgić 2016). There was no statistically significant difference between the two groups with respect to final overjet (MD 0.60 mm, 95% CI −1.63 to 0.43, P value = 0.25; 97 participants) (Analysis 4.3).
Activator functional appliance versus fixed functional (FORSUS FRD EZ) appliances
The results in this section are based on one trial (24 participants) at high risk of bias (Bilgiç 2011). Reduction in overjet favoured the FORSUS appliance (MD 2.19 mm, 95% CI 0.58 mm to 3.80 mm, P value = 0.008) (Analysis 4.4); but final ANB favoured the Activator group (MD −1.74°, 95% CI −3.28° to −0.20°, P value = 0.03) (Analysis 4.4).
Fixed functional (FORSUS FRD) versus fixed functional with mini‐implants (FMI)
Two trials, both at unclear risk of bias (Elkordy 2016; Eissa 2017), evaluated this comparison and found no significant difference between the two groups with respect to final overjet (MD ‐0.36, 95% CI ‐1.07 to 0.35, P value = 0.32; one trial, 29 participants) and final ANB (MD 0.22, 95% CI ‐0.86 to 1.30, P value = 0.69; two trials, 60 participants) (Analysis 4.5).
There was no difference between the groups in patient satisfaction (OR 0.18, 95% CI 0.01 to 3.97, P value = 0.27; one trial, 32 participants) (Analysis 4.6).
R‐appliance versus anterior inclined bite plate (AIBP)
A single trial at unclear risk of bias showed no statistically significant difference between the two groups with respect to final ANB (MD −0.30°, 95% CI −0.99° to 0.39°, P value = 0.40; 50 participants) (Showkatbakhsh 2011) (Analysis 4.7).
Removable functional versus fixed functional
Three trials at high risk of bias compared orthodontic treatment for adolescents with removable functional appliances to fixed functional appliances (Baysal 2014; Bilgiç 2011; UK (11‐14) 2003). There was a statistically significant difference between the groups in overjet (MD 0.74, 95% CI 0.15 to 1.33, P = 0.01; two trials, 154 participants) in favour of fixed functional appliances (Analysis 4.8). However, a statistically significant difference in final ANB of −1.04° (95% CI −1.60 to −0.49, P = 0.0002; three trials, 185 participants) was found in favour of removable functional appliances (Analysis 4.8).
Fixed functional (FORSUS FRD) versus intermaxillary elastics
The results in this section are based on one trial at high risk of bias (Aras 2017b). The results showed no statistically significant difference for final overjet (MD 0.28, 95% CI ‐0.35 to 0.91, P = 0.39; 28 participants) or final ANB (MD ‐0.90, 95% CI ‐1.96 to 0.61, P = 0.10; 28 participants) (Analysis 4.9).
FMA stepwise (SWG) versus FMA single step (SSG)
The results are based on a single trial at unclear risk of bias (Aras 2017a). There was no statistically significant difference for final overjet (MD 0.23, 95% CI ‐0.26 to 0.72, P = 0.36; 34 participants), but the results favoured stepwise advancement for final ANB value (MD ‐0.69, 95% CI ‐1.19 to ‐0.19, P = 0.007; 34 participants) (Analysis 4.10).
Harvold Activator versus Frankel function regulator
The results are based on a single trial at high risk of bias (New Zealand 2000). There was a statistically significant difference in the overjet change favouring Harvold Activator when compared with Frankel function regulator (MD ‐2.23, 95% CI ‐5.37 to 0.49, P = 0.02; 25 participants) (Analysis 4.11).
Discussion
Summary of main results
Early treatment (two‐phase) versus late treatment in adolescence (one‐phase)
We have found evidence that orthodontic treatment provided to 7 to 11 year olds with prominent upper front teeth results in a statistically significant reduction in incisor prominence. This effect occurs if the child received treatment with a functional appliance or headgear. This treatment also resulted in some changes in the relationship of the upper and lower jaws. However, while these changes or differences at the end of phase one were statistically significant, the quality of evidence for this comparison is low.
When we considered the final outcome of treatment at the end of a second phase of treatment in adolescence, we found that the treatment was effective, in that incisor prominence had been reduced. There were no differences in treatment outcome between the group who had received treatment at a younger age or treatment in adolescence for any variable other than the incidence of new incisal trauma. The results showed a significant reduction in incisor trauma in the early treatment (two‐phase) group as compared to the late treatment (one‐phase) group. The quality of the evidence for this comparison is low to moderate.
Treatment provided in adolescence (one‐phase)
We found seven studies that measured the effect of treatment with a functional appliance versus an untreated control. Heterogeneity was high, and we analysed fixed and removable appliances separately. We found significant reductions in final overjet with fixed and removable functional appliances (Analysis 3.1). There was evidence for a reduction in final ANB with removable functional appliances. The quality of the evidence was low for both outcomes.
We also found that several studies compared the effect of the Twin Block functional appliance against other functional appliances, for example the Bionator and Herbst appliances. We found that while there was a statistically significant difference in skeletal changes (ANB) in favour of Twin Block. The quality of the evidence was low.
There were three trials that compared orthodontic treatment for adolescents with removable functional appliances to fixed functional appliances. Although a statistically significant reduction in ANB was found in favour of removable functional appliances, and a statistically significant reduction in overjet was found in favour of fixed functional appliances, the changes were so small that they may not be of clinical importance. Additionally, the quality of the evidence was low for both.
Overall completeness and applicability of evidence
One important finding from this review was that while we identified 27 RCTs, they had been published in 63 different papers. Furthermore, several of the investigators had not only reported outcomes at the end of early treatment, but they had produced several papers that were confined to analysis of subsets of participants, to form interim reports or 'updates'. While they may have had good reasons to follow this publication strategy, in terms of having to compete for the renewal of grant funding, this did result in difficulty interpreting the results of these studies. We approached this problem by identifying the most relevant outcomes and data points and then produced composite data extraction for these studies. We would like to suggest that studies are not reported until they are completed. The registration of trials will go some way to addressing some of these issues, where each trial has a unique identity number that will appear on all publications.
In this review we have analysed data at the end of phase one and phase two in studies that evaluated the effect of early treatment. This is because these trials were carried out to evaluate the effectiveness of early treatment provided when the children were 7 to 11 years old. These studies were then extended to the completion of all orthodontic treatment and included in this review. It could be suggested that we should only report the final findings of these trials. However, we feel that the 'early' treatment studies should be included to illustrate that there were some short‐term benefits: for example, reduction in overjet and possible increase in self‐esteem. Nevertheless, these findings do not detract from the overall conclusions that early treatment is of limited benefit.
Finally, there was great variation in the outcome measures that were adopted by the investigators. This was particularly marked with the use of cephalometric analyses and is not surprising when we consider that there are many different types of analysis. We would suggest that uniformly applied cephalometric analyses are used when future studies are planned, so that adequate comparisons between trials can be achieved.
Quality of the evidence
We found 27 RCTs evaluating orthodontic treatment of people with prominent upper front teeth (Class II malocclusion). The overall quality of evidence in this review was low (summary of findings Table for the main comparison; summary of findings Table 2; summary of findings Table 3; summary of findings Table 4; summary of findings Table 5), with only two trials assessed as being at low risk of bias (UK (Mixed) 2009; Yaqoob 2012). There were three two‐phase studies that contributed data to this review (Florida 1998; North Carolina 2004; UK (Mixed) 2009). It is important to mention that carrying out a trial of a two‐phase study (treatment for young children followed by treatment in adolescence) is much more difficult and potentially more prone to bias than a one‐phase study. However, in this review, the two‐phase studies were of better quality than most of the one‐phase studies.
It is important to point out that one study did not report a complete data set. Although six different articles were published, none of them included a complete data set and did not give reasons for not doing so (Ghafari 1998).
It is interesting to note that one study was prematurely stopped due to harms (Thiruvenkatachari 2010). The study compared the Twin Block and the Dynamax appliances and showed a statistically significant overjet reduction in the Twin Block group at the end of the first interim analysis. The study also reported significantly greater incidence of harms with the Dynamax appliance.
Potential biases in the review process
A potential bias could be reporting bias. We avoided this by carrying out a broad search with no restrictions on language or publication status.
Another potential bias in the review could be our categorisation based on terminology of 'early' and 'late' treatment. In the protocol, we defined early treatment as treatment initiated between 7 and 11 years of age and late treatment as treatment initiated between 12 and 16 years of age. Some studies were difficult to categorise as they had recruited participants between 9 and 12 years of age (see Characteristics of included studies section). As the 'early' and 'late' terminologies are accepted globally, we considered two‐phase studies as early treatment and one‐phase studies as late treatment.
Agreements and disagreements with other studies or reviews
There are several systematic reviews that have been performed on the effects of functional appliances for patients with increased overjet (Antonarakis 2007; Barnett 2008; Cozza 2006; Flores‐Mir 2007; Perillo 2012; Ehsani 2015; Koretsi 2015; Zymperdikas 2016; Yang 2016; Pacha 2016). Antonarakis 2007 reported that functional appliances show a statistically significant reduction in overjet and ANB value when compared with untreated controls. However, the authors have included prospective and retrospective studies and did not separate early and late treatment. This makes it difficult to compare with the present review. Similarly, Barnett 2008, Cozza 2006, Flores‐Mir 2007, Perillo 2012, Ehsani 2015, Koretsi 2015, Zymperdikas 2016, Yang 2016, and Pacha 2016 included non‐randomised studies. Cozza 2006 evaluated the effects of functional appliances on mandibular length and did not report on other dental measurements. Barnett 2008, Flores‐Mir 2007 and Yang 2016 were confined to the Herbst appliance, whereas Perillo 2012 evaluated the Frankel appliance and Ehsani 2015 studied Twin‐Block. Koretsi 2015 compared removable functional appliances versus untreated Class II; Zymperdikas 2016 compared fixed functional appliances versus untreated Class II; and Pacha 2016 compared fixed versus removable functional appliances. This makes it impossible to compare the results with the present review.
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
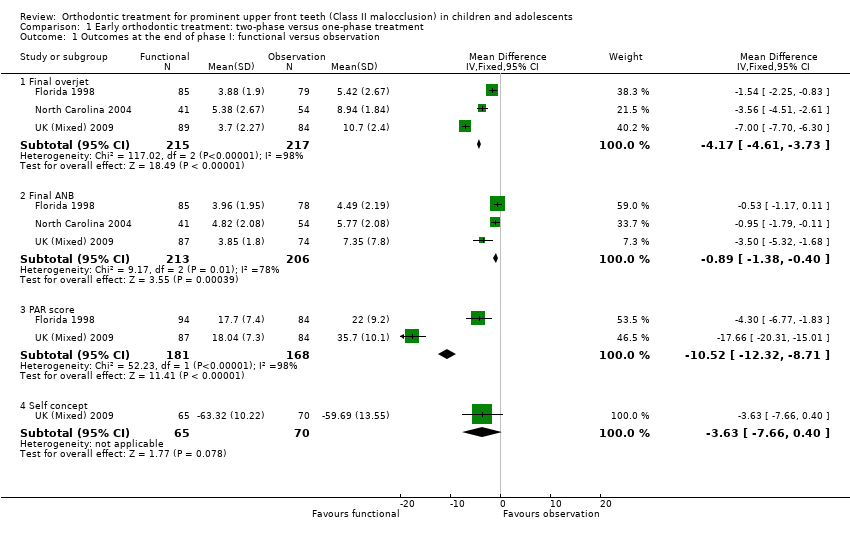
Comparison 1 Early orthodontic treatment: two‐phase versus one‐phase treatment, Outcome 1 Outcomes at the end of phase I: functional versus observation.
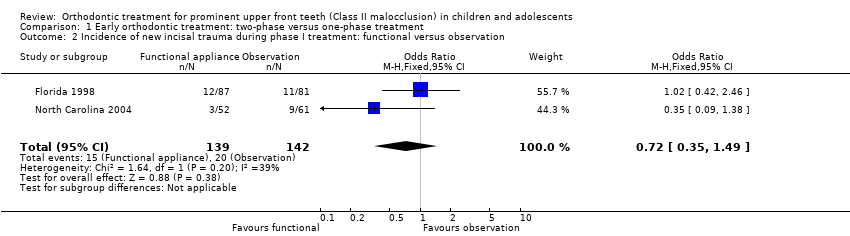
Comparison 1 Early orthodontic treatment: two‐phase versus one‐phase treatment, Outcome 2 Incidence of new incisal trauma during phase I treatment: functional versus observation.
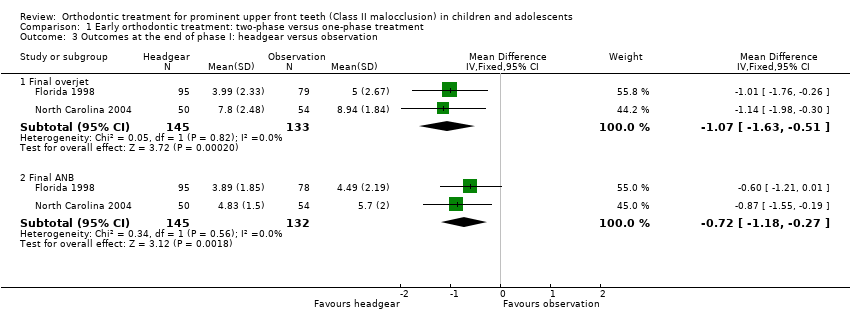
Comparison 1 Early orthodontic treatment: two‐phase versus one‐phase treatment, Outcome 3 Outcomes at the end of phase I: headgear versus observation.
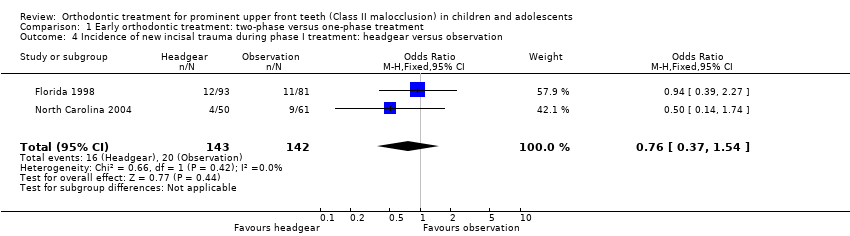
Comparison 1 Early orthodontic treatment: two‐phase versus one‐phase treatment, Outcome 4 Incidence of new incisal trauma during phase I treatment: headgear versus observation.

Comparison 1 Early orthodontic treatment: two‐phase versus one‐phase treatment, Outcome 5 Outcomes at the end of phase II: functional (2‐phase) versus adolescent (1‐phase) treatment.

Comparison 1 Early orthodontic treatment: two‐phase versus one‐phase treatment, Outcome 6 Incidence of new incisal trauma by the end of phase II treatment: functional (2‐phase) versus adolescent (1‐phase) treatment.

Comparison 1 Early orthodontic treatment: two‐phase versus one‐phase treatment, Outcome 7 Outcomes at the end of phase II: headgear (2‐phase) versus adolescent (1‐phase) treatment.

Comparison 1 Early orthodontic treatment: two‐phase versus one‐phase treatment, Outcome 8 Incidence of new incisal trauma by the end of phase II treatment: headgear (2‐phase) versus adolescent (1‐phase) treatment.

Comparison 2 Early orthodontic treatment: two‐phase appliance 1 (headgear) versus appliance 2 (functional), Outcome 1 Outcomes at the end of phase I: headgear versus functional.

Comparison 2 Early orthodontic treatment: two‐phase appliance 1 (headgear) versus appliance 2 (functional), Outcome 2 Incidence of new incisal trauma during phase I treatment: headgear versus functional.
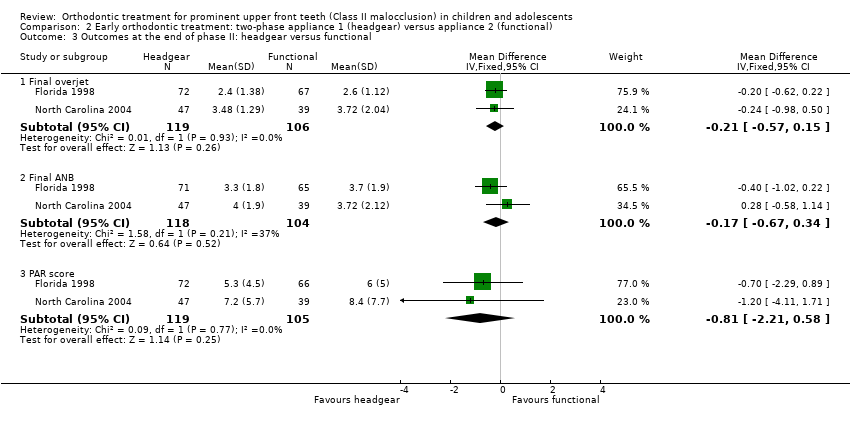
Comparison 2 Early orthodontic treatment: two‐phase appliance 1 (headgear) versus appliance 2 (functional), Outcome 3 Outcomes at the end of phase II: headgear versus functional.

Comparison 2 Early orthodontic treatment: two‐phase appliance 1 (headgear) versus appliance 2 (functional), Outcome 4 Incidence of new incisal trauma by the end of phase II treatment: headgear versus functional appliance.
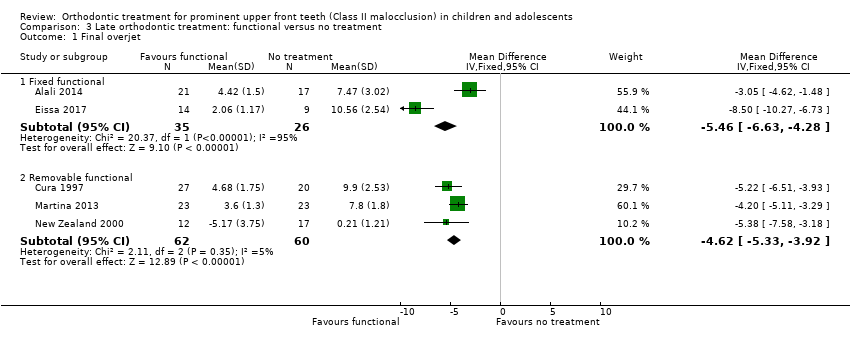
Comparison 3 Late orthodontic treatment: functional versus no treatment, Outcome 1 Final overjet.
Comparison 3 Late orthodontic treatment: functional versus no treatment, Outcome 2 Final ANB.
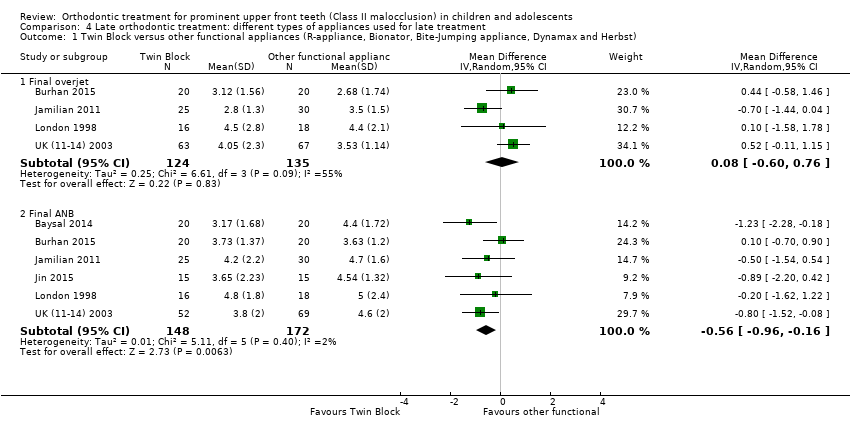
Comparison 4 Late orthodontic treatment: different types of appliances used for late treatment, Outcome 1 Twin Block versus other functional appliances (R‐appliance, Bionator, Bite‐Jumping appliance, Dynamax and Herbst).

Comparison 4 Late orthodontic treatment: different types of appliances used for late treatment, Outcome 2 Twin Block conventional versus other Twin Block modifications.

Comparison 4 Late orthodontic treatment: different types of appliances used for late treatment, Outcome 3 Functional (Activator) versus prefabricated functional myobrace appliance (PFA).

Comparison 4 Late orthodontic treatment: different types of appliances used for late treatment, Outcome 4 Functional (Activator) versus fixed functional (FORSUS FRD EZ).

Comparison 4 Late orthodontic treatment: different types of appliances used for late treatment, Outcome 5 Fixed functional (FORSUS FRD) versus fixed functional with mini‐implants (FMI).
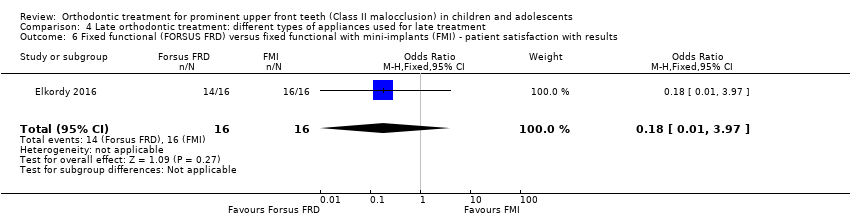
Comparison 4 Late orthodontic treatment: different types of appliances used for late treatment, Outcome 6 Fixed functional (FORSUS FRD) versus fixed functional with mini‐implants (FMI) ‐ patient satisfaction with results.
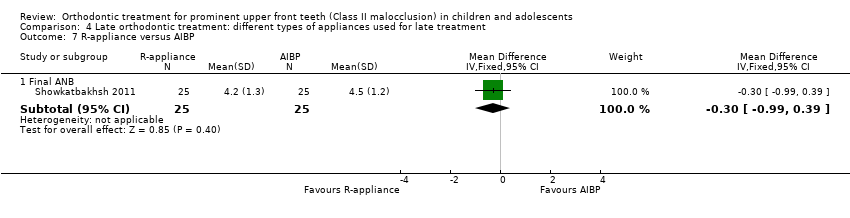
Comparison 4 Late orthodontic treatment: different types of appliances used for late treatment, Outcome 7 R‐appliance versus AIBP.
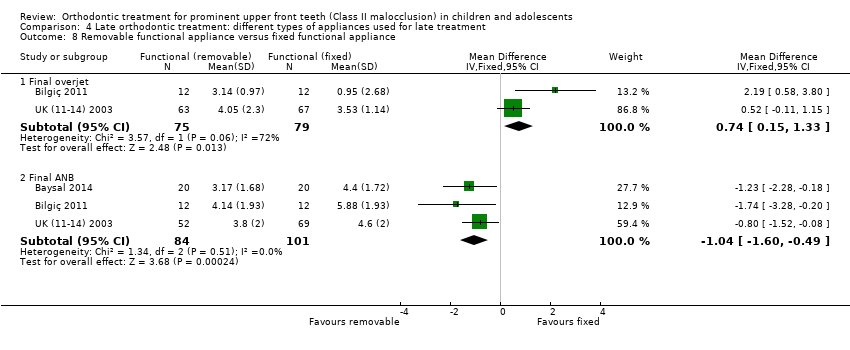
Comparison 4 Late orthodontic treatment: different types of appliances used for late treatment, Outcome 8 Removable functional appliance versus fixed functional appliance.
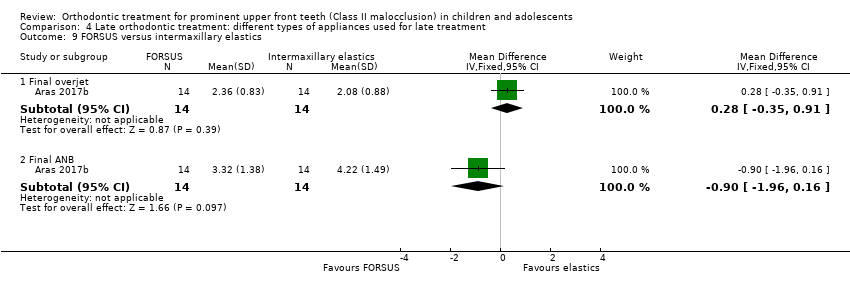
Comparison 4 Late orthodontic treatment: different types of appliances used for late treatment, Outcome 9 FORSUS versus intermaxillary elastics.
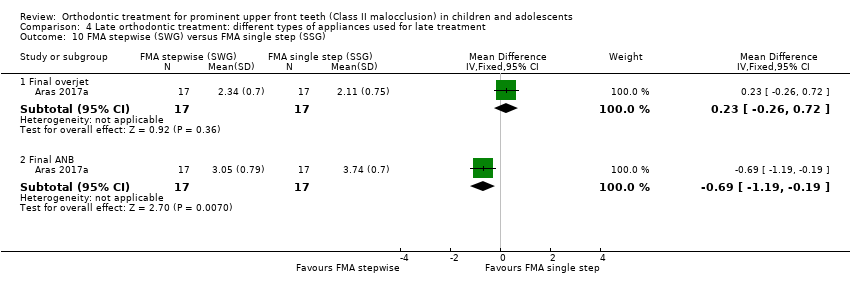
Comparison 4 Late orthodontic treatment: different types of appliances used for late treatment, Outcome 10 FMA stepwise (SWG) versus FMA single step (SSG).

Comparison 4 Late orthodontic treatment: different types of appliances used for late treatment, Outcome 11 Harvold Activator versus Frankel function regulator.
| Early treatment (two‐phase: phase one in childhood and phase two in adolescence) versus late treatment (one‐phase in adolescence) with functional appliance | ||||||
| Patient or population: children and/or adolescents (age ≤ 16 years) receiving orthodontic treatment to correct prominent upper front teeth Intervention: early treatment with functional appliance Comparison: late treatment with functional appliance | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | Number of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Late treatment with functional appliance | Early treatment with functional appliance | |||||
| Overjet (mm) (smaller value better) Follow‐up at end of orthodontic treatment | Mean final overjet ranged across control groups from 2.6 mm to 4.3 mm | Mean final overjet 0.21 mm more (0.10 mm less to 0.51 mm more) | 343 (3) | ⊕⊕ low2 3 | The functional appliance reduced overjet compared to no treatment at the end of the first phase of early treatment (MD −4.17, −4.61 to −3.73; 432 participants). | |
| Incidence of incisal trauma Follow‐up at end of orthodontic treatment | 298 per 10001 | 192 per 1000 (123 to 288) | OR 0.56 (0.33 to 0.95) | 332 (3) | ⊕⊕⊕ moderate2 | |
| ANB (°) Follow‐up at end of orthodontic treatment | Mean final ANB ranged across control groups from 3.7° to 4.0° | Mean final ANB 0.02° less (0.47° less to 0.43° more) | 347 (3) | ⊕⊕⊕ moderate2 | The functional appliance improved ANB at the end of the first phase of early treatment when compared with no treatment (MD −0.89, −1.38 to −0.40; 419 participants). | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI) | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Based on average in control groups | ||||||
| Early treatment (two‐phase: phase 1 in childhood and phase 2 in adolescence) with headgear appliance versus late treatment (one‐phase in adolescence) with headgear | ||||||
| Patient or population: children and/or adolescents (age ≤ 16 years) receiving orthodontic treatment to correct prominent upper front teeth Intervention: early treatment with headgear Comparison: late treatment with headgear | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Late treatment with headgear | Early treatment with headgear | |||||
| Overjet (mm) (smaller value better) Follow‐up at end of orthodontic treatment | Mean final overjet ranged across control groups from 2.4 mm to 3.48 mm | Mean final overjet in the 2‐phase treatment group was 0.22 mm less (0.56 mm less to 0.12 mm more) | 238 (2) | ⊕⊕ low2 | Headgear reduced overjet compared to no treatment at the end of the first phase of early treatment (MD −1.07, −1.63 to −0.51; 278 participants). | |
| Incidence of incisal trauma Follow‐up at end of orthodontic treatment | 367 per 10001 | 207 per 1000 (126 to 317) | OR 0.45 (0.25 to 0.80) | 237 (2) | ⊕⊕ low2 | |
| ANB (°) Follow‐up at end of orthodontic treatment | Mean final ANB ranged across control groups from 3.3° to 4.0° | Mean final ANB 0.27° less (0.80° less to 0.26° more) | 231 (2) | ⊕⊕ low2 | Headgear improved ANB compared to no treatment at the end of the first phase of early treatment (MD −0.72, −1.18 to −0.27; 277 participants). | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI) | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Based on average in control groups | ||||||
| Late treatment (one‐phase in adolescence) with functional appliance versus no treatment for prominent upper front teeth (Class II malocclusion) | ||||||
| Patient or population: adolescents (age between 12 and 16 years) receiving orthodontic treatment to correct prominent upper front teeth | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | Number of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| No treatment | Late treatment with functional appliances | |||||
| Fixed functional appliances | ||||||
| Overjet (mm) (smaller value better) Follow‐up at end of orthodontic treatment | Mean final overjet ranged from 7.47 to 10.56 mm | Mean final overjet was 5.46 mm lower | 61 | ⊕⊕⊝⊝ | ||
| Incidence of incisal trauma | Not measured | |||||
| ANB (°) Follow‐up at end of orthodontic treatment | Mean final ANB ranged from 6.30° to 7.92° | Mean final ANB was 0.53° lower | 89 | ⊕⊕⊝⊝ | ||
| Removable functional appliances | ||||||
| Overjet (mm) (smaller value better) Follow‐up at end of orthodontic treatment | Mean final overjet ranged from 7.8 to 9.9 mm | Mean final overjet was 4.62 mm lower (5.33 lower to 3.92 lower) | 122 | ⊕⊕⊝⊝ | ||
| Incidence of incisal trauma | Not measured | |||||
| ANB (°) Follow‐up at end of orthodontic treatment | Mean final ANB ranged from 6.5° to 6.53° | Mean final ANB was 2.37° lower | 99 | ⊕⊕⊝⊝ | ||
| 1 Downgraded one level as both studies were at unclear risk of bias and one level because of very high heterogeneity (I² = 95%) 2 Downgraded one level as the three studies were at unclear risk of bias and one level for moderate heterogeneity (I² = 51%) 3 Downgraded two levels as both studies were at high risk of bias | ||||||
| Late treatment (one‐phase in adolescence): comparison among different types of appliances used for treatment of prominent upper front teeth (Class II malocclusion) | ||||||
| Patient or population: adolescents (age between 12 and 16 years) receiving orthodontic treatment to correct prominent upper front teeth | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | № of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Different types of appliances | Twin Block | |||||
| Overjet (mm) (smaller value better) Follow‐up at end of orthodontic treatment | Mean final overjet ranged from 2.68 mm to 4.40 mm | Mean final overjet was 0.08 mm higher | 259 | ⊕⊕⊝⊝ | ||
| Incidence of Incisal trauma | Not measured | |||||
| ANB (°) Follow‐up at end of orthodontic treatment | Mean final ANB ranged from 3.63° to 5.00° | Mean final ANB was −0.56° lower | 320 | ⊕⊕⊝⊝ | ||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI) | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded as 2 of 4 studies were at high risk of bias 2 Dowgraded due to heterogeneity (heterogeneity: Tau² = 0.25; Chi² = 6.61, df = 3 (P = 0.09); I² = 55%) 3 Downgraded as 3 of 6 studies were at high risk of bias 4 Downgraded as the interventions in the comparison groups were not similar | ||||||
| Late treatment in adolescence (one‐phase): comparison among different types of appliances used for treatment of prominent upper front teeth (Class II malocclusion) | ||||||
| Patient or population: adolescents (age between 12 and 16 years) receiving orthodontic treatment to correct prominent upper front teeth Intervention: Removable funtional appliance | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | Number of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Fixed functional appliance | Removable functional appliance | |||||
| Overjet (mm) (smaller value better) Follow‐up at end of orthodontic treatment | Mean final overjet ranged from 0.95 mm to 3.53 mm | Mean final overjet was 0.74 mm higher (0.15 lower to 1.33 higher) | 154 | ⊕⊕⊝⊝ | ||
| Incidence of Incisal trauma | Not measured | |||||
| ANB (°) Follow‐up at end of orthodontic treatment | Mean final ANB ranged from 4.40° to 5.88° | Mean final ANB was 1.04° lower | 185 | ⊕⊕⊝⊝ | ||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI) | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded due to inconsistency (interventions were not similar between studies) 2 Downgraded twice as both studies were at high risk of bias 3 Downgraded due to inconsistency (interventions were not similar between studies) 4 Downgraded twice as 3 trials were at high risk of bias | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Outcomes at the end of phase I: functional versus observation Show forest plot | 3 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 Final overjet | 3 | 432 | Mean Difference (IV, Fixed, 95% CI) | ‐4.17 [‐4.61, ‐3.73] |
| 1.2 Final ANB | 3 | 419 | Mean Difference (IV, Fixed, 95% CI) | ‐0.89 [‐1.38, ‐0.40] |
| 1.3 PAR score | 2 | 349 | Mean Difference (IV, Fixed, 95% CI) | ‐10.52 [‐12.32, ‐8.71] |
| 1.4 Self concept | 1 | 135 | Mean Difference (IV, Fixed, 95% CI) | ‐3.63 [‐7.66, 0.40] |
| 2 Incidence of new incisal trauma during phase I treatment: functional versus observation Show forest plot | 2 | 281 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.72 [0.35, 1.49] |
| 3 Outcomes at the end of phase I: headgear versus observation Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 3.1 Final overjet | 2 | 278 | Mean Difference (IV, Fixed, 95% CI) | ‐1.07 [‐1.63, ‐0.51] |
| 3.2 Final ANB | 2 | 277 | Mean Difference (IV, Fixed, 95% CI) | ‐0.72 [‐1.18, ‐0.27] |
| 4 Incidence of new incisal trauma during phase I treatment: headgear versus observation Show forest plot | 2 | 285 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.76 [0.37, 1.54] |
| 5 Outcomes at the end of phase II: functional (2‐phase) versus adolescent (1‐phase) treatment Show forest plot | 3 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 5.1 Final overjet | 3 | 343 | Mean Difference (IV, Fixed, 95% CI) | 0.21 [‐0.10, 0.51] |
| 5.2 Final ANB | 3 | 347 | Mean Difference (IV, Fixed, 95% CI) | ‐0.02 [‐0.47, 0.43] |
| 5.3 PAR score | 3 | 360 | Mean Difference (IV, Fixed, 95% CI) | 0.62 [‐0.66, 1.91] |
| 5.4 Self concept | 1 | 132 | Mean Difference (IV, Fixed, 95% CI) | ‐0.83 [‐3.97, 2.31] |
| 6 Incidence of new incisal trauma by the end of phase II treatment: functional (2‐phase) versus adolescent (1‐phase) treatment Show forest plot | 3 | 332 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.56 [0.33, 0.95] |
| 7 Outcomes at the end of phase II: headgear (2‐phase) versus adolescent (1‐phase) treatment Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 7.1 Final overjet | 2 | 238 | Mean Difference (IV, Fixed, 95% CI) | ‐0.22 [‐0.56, 0.12] |
| 7.2 Final ANB | 2 | 231 | Mean Difference (IV, Fixed, 95% CI) | ‐0.27 [‐0.80, 0.26] |
| 7.3 PAR score | 2 | 177 | Mean Difference (IV, Fixed, 95% CI) | ‐1.55 [‐3.70, 0.60] |
| 8 Incidence of new incisal trauma by the end of phase II treatment: headgear (2‐phase) versus adolescent (1‐phase) treatment Show forest plot | 2 | 237 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.45 [0.25, 0.80] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Outcomes at the end of phase I: headgear versus functional Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 Final overjet | 2 | 271 | Mean Difference (IV, Fixed, 95% CI) | 0.75 [0.21, 1.29] |
| 1.2 Final ANB | 2 | 271 | Mean Difference (IV, Fixed, 95% CI) | ‐0.04 [‐0.49, 0.41] |
| 2 Incidence of new incisal trauma during phase I treatment: headgear versus functional Show forest plot | 2 | 282 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.48, 2.17] |
| 3 Outcomes at the end of phase II: headgear versus functional Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 3.1 Final overjet | 2 | 225 | Mean Difference (IV, Fixed, 95% CI) | ‐0.21 [‐0.57, 0.15] |
| 3.2 Final ANB | 2 | 222 | Mean Difference (IV, Fixed, 95% CI) | ‐0.17 [‐0.67, 0.34] |
| 3.3 PAR score | 2 | 224 | Mean Difference (IV, Fixed, 95% CI) | ‐0.81 [‐2.21, 0.58] |
| 4 Incidence of new incisal trauma by the end of phase II treatment: headgear versus functional appliance Show forest plot | 2 | 226 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.78 [0.42, 1.47] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Final overjet Show forest plot | 5 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 Fixed functional | 2 | 61 | Mean Difference (IV, Fixed, 95% CI) | ‐5.46 [‐6.63, ‐4.28] |
| 1.2 Removable functional | 3 | 122 | Mean Difference (IV, Fixed, 95% CI) | ‐4.62 [‐5.33, ‐3.92] |
| 2 Final ANB Show forest plot | 5 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.1 Fixed functional | 3 | 89 | Mean Difference (IV, Fixed, 95% CI) | ‐0.53 [‐1.27, 0.22] |
| 2.2 Removable functional | 2 | 99 | Mean Difference (IV, Fixed, 95% CI) | ‐2.37 [‐3.01, ‐1.74] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Twin Block versus other functional appliances (R‐appliance, Bionator, Bite‐Jumping appliance, Dynamax and Herbst) Show forest plot | 6 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 Final overjet | 4 | 259 | Mean Difference (IV, Random, 95% CI) | 0.08 [‐0.60, 0.76] |
| 1.2 Final ANB | 6 | 320 | Mean Difference (IV, Random, 95% CI) | ‐0.56 [‐0.96, ‐0.16] |
| 2 Twin Block conventional versus other Twin Block modifications Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.1 Final overjet | 2 | 196 | Mean Difference (IV, Fixed, 95% CI) | ‐0.23 [‐0.67, 0.22] |
| 3 Functional (Activator) versus prefabricated functional myobrace appliance (PFA) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 3.1 Final overjet | 1 | 97 | Mean Difference (IV, Fixed, 95% CI) | ‐0.60 [‐1.63, 0.43] |
| 4 Functional (Activator) versus fixed functional (FORSUS FRD EZ) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 4.1 Final overjet | 1 | 24 | Mean Difference (IV, Fixed, 95% CI) | 2.19 [0.58, 3.80] |
| 4.2 Final ANB | 1 | 24 | Mean Difference (IV, Fixed, 95% CI) | ‐1.74 [‐3.28, ‐0.20] |
| 5 Fixed functional (FORSUS FRD) versus fixed functional with mini‐implants (FMI) Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 5.1 Final overjet | 1 | 29 | Mean Difference (IV, Fixed, 95% CI) | ‐0.36 [‐1.07, 0.35] |
| 5.2 Final ANB | 2 | 60 | Mean Difference (IV, Fixed, 95% CI) | 0.22 [‐0.86, 1.30] |
| 6 Fixed functional (FORSUS FRD) versus fixed functional with mini‐implants (FMI) ‐ patient satisfaction with results Show forest plot | 1 | 32 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.18 [0.01, 3.97] |
| 7 R‐appliance versus AIBP Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 7.1 Final ANB | 1 | 50 | Mean Difference (IV, Fixed, 95% CI) | ‐0.30 [‐0.99, 0.39] |
| 8 Removable functional appliance versus fixed functional appliance Show forest plot | 3 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 8.1 Final overjet | 2 | 154 | Mean Difference (IV, Fixed, 95% CI) | 0.74 [0.15, 1.33] |
| 8.2 Final ANB | 3 | 185 | Mean Difference (IV, Fixed, 95% CI) | ‐1.04 [‐1.60, ‐0.49] |
| 9 FORSUS versus intermaxillary elastics Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 9.1 Final overjet | 1 | 28 | Mean Difference (IV, Fixed, 95% CI) | 0.28 [‐0.35, 0.91] |
| 9.2 Final ANB | 1 | 28 | Mean Difference (IV, Fixed, 95% CI) | ‐0.90 [‐1.96, 0.16] |
| 10 FMA stepwise (SWG) versus FMA single step (SSG) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 10.1 Final overjet | 1 | 34 | Mean Difference (IV, Fixed, 95% CI) | 0.23 [‐0.26, 0.72] |
| 10.2 Final ANB | 1 | 34 | Mean Difference (IV, Fixed, 95% CI) | ‐0.69 [‐1.19, ‐0.19] |
| 11 Harvold Activator versus Frankel function regulator Show forest plot | 1 | 25 | Mean Difference (IV, Fixed, 95% CI) | ‐2.93 [‐5.37, ‐0.49] |
| 11.1 Overjet change | 1 | 25 | Mean Difference (IV, Fixed, 95% CI) | ‐2.93 [‐5.37, ‐0.49] |

