Radiothérapie versus chirurgie effractive versus chirurgie endolaryngée (avec ou sans laser) pour le carcinome épidermoïde du larynx au stade précoce
Résumé scientifique
Contexte
Ceci est une mise à jour d'une revue Cochrane publiée pour la première fois dans la Bibliothèque Cochrane dans le numéro 2, 2002 et précédemment mise à jour en 2004, 2007 et 2010.
La radiothérapie, la chirurgie effractive et l'exérèse endolaryngée (avec ou sans laser) constituent toutes des modalités de traitement acceptées pour le cancer glottique à un stade précoce. Les séries de cas suggèrent qu'elles confèrent un bénéfice de survie similaire, mais l'avantage de la radiothérapie et de la chirurgie endolaryngée est la préservation de la voix. La tendance observée ces dernières années est à l'abandon de la chirurgie ouverte, mais la radiothérapie et la chirurgie endolaryngée sont toujours à l'égalité puisque les deux modalités de traitement offrent une préservation laryngée avec des taux de survie similaires. Les avis sur le meilleur traitement diffèrent selon les disciplines et les pays.
Objectifs
Comparer l'efficacité de la chirurgie effractive, de l'exérèse endolaryngée (avec ou sans laser) et de la radiothérapie dans la prise en charge du cancer du larynx glottique au stade précoce.
Stratégie de recherche documentaire
Nous avons effectué des recherches dans le registre des essais du groupe Cochrane sur l'otorhinolaryngologie, dans le registre Cochrane des essais contrôlés (CENTRAL 2014, numéro 8), ainsi que dans PubMed, EMBASE, CINAHL, Web of Science, Cambridge Scientific Abstracts, ICTRP et d'autres sources afin de trouver des essais publiés et non publiés. La recherche la plus récente a été effectuée le 18 septembre 2014.
Critères de sélection
Essais contrôlés randomisés comparant la chirurgie effractive, la résection endolaryngée (avec ou sans laser) et la radiothérapie.
Recueil et analyse des données
Nous avons utilisé les procédures méthodologiques standard prévues par la Collaboration Cochrane.
Résultats principaux
Nous n'avons identifié qu'un essai contrôlé randomisé, ayant comparé la chirurgie effractive et la radiothérapie chez 234 patients souffrant d'un cancer du larynx glottique à un stade précoce. Le risque global de biais de cette étude était élevé.
Pour les tumeurs T1, la survie à cinq ans était de 91,7 % suite à la radiothérapie et de 100 % après la chirurgie, et pour les tumeurs T2, de 88,8 % après la radiothérapie et de 97,4 % après la chirurgie. Il n'y avait aucune différence significative dans la survie entre les deux groupes.
Pour les tumeurs T1, le taux de survie à cinq ans sans maladie était de 71,1 % après la radiothérapie et de 100,0 % après une intervention chirurgicale, et pour les tumeurs T2, de 60,1 % après radiothérapie et de 78,7 % après la chirurgie. Seule la dernière comparaison était statistiquement significative (P = 0,036 valeur), mais la signification statistique n'aurait pas été atteinte avec un test bilatéral.
Aucune donnée n'était disponible sur les effets indésirables, la qualité de vie, les critères vocaux ou les coûts.
Nous n'avons identifié aucun essai contrôlé randomisé comprenant la chirurgie endolaryngée. Un certain nombre d'essais comparant la résection endolaryngéé et la radiothérapie ont terminé tôt à cause de la difficulté à recruter des participants. Un essai contrôlé randomisé est toujours en cours.
Conclusions des auteurs
Il y a seulement un essai contrôlé randomisé comparant la chirurgie ouverte et la radiothérapie, mais son interprétation est limitée en raison de préoccupations au sujet de l'adéquation des régimes de traitement et de lacunes dans le compte‐rendu de la conception et de l'analyse de l'étude.
Résumé simplifié
Comparaison de la radiothérapie, de la chirurgie ouverte et de la chirurgie endolaryngée (avec ou sans laser) pour le cancer du larynx au stade précoce
Contexte
Le cancer du larynx débute généralement dans la glotte (au niveau des cordes vocales), comme un cancer épidermoïde (cancer dans les membranes). La plupart des malades survivent à ces cancers lorsqu'ils sont traités de manière précoce (avant que le cancer se propage dans le larynx et les zones contiguës). Les options comprennent la radiothérapie, la chirurgie ouverte en passant par le cou ou, plus fréquemment aujourd'hui, l'exérèse endolaryngée, dans laquelle l'accès à la gorge se fait par la bouche, parfois avec un laser.
Caractéristiques des études
Cette revue d'essais n'a identifié qu'un seul essai portant sur 234 patients atteints de cancer glottique à un stade précoce, ayant comparé la radiothérapie à la chirurgie ouverte. Il s'agissait d'un essai contrôlé randomisé multicentrique mené dans l'ancienne Union soviétique, en Hongrie et en Tchécoslovaquie. Les patients ont été suivis pendant cinq ans et les taux sans récidive et de survie ont été mesurés.
Principaux résultats
Les résultats de cet essai ont montré qu'il n'y avait pas de différence significative dans la survie entre les patients traités par radiothérapie ou chirurgie ouverte.
D'autres données provenant d'essais comparant la radiothérapie et la chirurgie endolaryngée sont nécessaires pour déterminer la meilleure façon de traiter le cancer du larynx à un stade précoce, mais un certain nombre d'études ont été abandonnées en raison de difficultés à recruter des participants. Un essai est toujours en cours.
Nous avons trouvé que les preuves étaient insuffisantes pour déterminer la forme de traitement qui pourrait être plus favorable aux malades souffrant d'un cancer du larynx à un stade précoce.
Qualité des preuves
L'étude incluse est de faible qualité. Les preuves incluses dans cette revue sont à jour en septembre 2014.
Authors' conclusions
Background
This is an update of a Cochrane review first published in The Cochrane Library in Issue 2, 2002 and previously updated in 2004, 2007 and 2010.
Description of the condition
Over 150,000 new cases of laryngeal cancer are diagnosed each year (GLOBOCAN 2012); the highest rates are observed in Southern and Eastern Europe (Parkin 1997). Men are more likely to develop laryngeal cancer than women. Smoking and alcohol are proven risk factors and the temporal decline in incidence of this cancer in some populations is consistent with a decline in the consumption of tobacco (Coleman 1993).
Laryngeal cancers most commonly arise from the glottis, i.e. the true vocal cord, and are usually squamous cell carcinomas. Three‐quarters of these patients present early, i.e. without vocal cord fixation, nodal involvement or extension beyond the larynx (Groome 2001; Joslin 1995; Robin 1989; Shah 1997). Reported five‐year survival rates following treatment of these early tumours, adjusted for deaths from other causes, frequently exceed 85% (Groome 2001; Joslin 1995; Robin 1989; Shah 1997).
Description of the intervention
Radiotherapy, open surgery and endolaryngeal excision are all accepted modalities of treatment for early‐stage glottic cancer (T1‐T2, N0). Radiotherapy utilises ionising radiation to initiate double‐stranded breaks of nuclear DNA leading to loss of the cells' reproductive ability and eventually to cell death. Radiotherapy offers laryngeal preservation, however it is a prolonged treatment course and may be associated with unpleasant adverse effects including oral mucositis, dysphagia, radiation skin burns and xerostomia. Open laryngeal surgery involves an open neck wound with partial or total surgical resection of the larynx with insertion of an indwelling voice prosthesis to allow speech in cases of total laryngectomy, although total laryngectomy is rarely indicated for early‐stage cancers. Endolaryngeal surgery is minimally invasive in comparison and involves resection of the tumour via the transoral route with or without the use of laser, with the advantages of preservation of voice and laryngeal function.
Why it is important to do this review
When this review was originally written in 2002, early laryngeal tumours were largely treated with open surgery or radiotherapy, with results of case series demonstrating similar survival rates. Radiotherapy offers the advantage of voice preservation over open surgery, therefore it was previously the generally preferred treatment modality (Groome 2001; Mendenhall 1994; O'Sullivan 1994; Shah 1997; Stalpers 1989). However, open surgery remained an option, particularly in populations without access to specialist centres for radiotherapy.
In recent years endolaryngeal surgery (with or without laser) has grown in popularity (DAHNO 2012), and there has been an observed trend away from open surgery as a result. Endolaryngeal surgery offers survival rates that are similar to radiotherapy and has an advantage over open surgery in preservation of voice and laryngeal function. A number of systematic reviews of non‐randomised studies have been undertaken (Abdurehim 2011; Feng 2011; Higgins 2009; Spielmann 2010), all of which have failed to demonstrate a significant difference between survival rates after radiotherapy or endolaryngeal surgery. Voice outcomes may also be similar following radiotherapy and endolaryngeal surgery (Cohen 2006; Hirano 1985; Keilmann 1996; McGuirt 1994; Sittel 1998), thus creating a position of equipoise between these two treatment modalities.
Endolaryngeal resection requires access to specialist surgeons with appropriate experience and expertise, however recent years have seen an apparent increase in the use of this modality of treatment (Hoffman 2006). For example, in England and Wales it has been reported that patients are as likely to receive transoral laser‐assisted microsurgical resection as they are to receive radiotherapy (Bradley 2009; DAHNO 2012), although there remains a geographical discrepancy as some UK centres still do not offer transoral laser surgery (DAHNO 2012).
If recurrence does occur, the options for further treatment after endolaryngeal surgery not only include open surgery but also further endolaryngeal resection and radiotherapy, whereas locoregional failure after radiotherapy can only be treated with major open surgical intervention (Goh 1996; Jensen 1994; Smee 2000). Additionally, as endolaryngeal resection is often a day‐case procedure, some clinicians believe that treatment costs will be less than for radiotherapy (Brandenburg 2001; Goor 2007); this is supported by a recent cost‐utility analysis (Higgins 2011).
Therapeutic conflicts in the management of early laryngeal cancers are sustained by the belief that randomised controlled trials have not been and could not be undertaken (Goh 1996). We have undertaken a systematic review to identify any randomised controlled trials comparing open surgery, radiotherapy and endolaryngeal excision in patients with early glottic cancer.
Objectives
To compare the effectiveness of open surgery, endolaryngeal excision (with or without laser) and radiotherapy in the management of early glottic laryngeal cancer.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled trials that compared open surgery, endolaryngeal resection and/or radiotherapy. We did not consider trials which compared different radiotherapeutic techniques. We also excluded trials which were primarily a comparison of treatments for advanced laryngeal cancer. We only included trials with a radiotherapy arm when patients were predominantly recruited from 1980 onwards, because of concerns that regimens prior to that date may have been sub‐optimal.
Types of participants
The study population was limited to patients diagnosed with early squamous cell carcinoma of the glottic larynx following laryngoscopy and biopsy. Early‐stage tumours were defined as carcinoma in situ (Tis) or invasive cancers confined to the vocal cords or with supraglottic or subglottic extension without cord fixation or nodal metastases (T1‐T2, N0) (Sobin 1997).
Types of interventions
Open surgery, endolaryngeal excision (with or without laser) and/or radiotherapy.
Types of outcome measures
Primary outcomes
We compared different modalities of treatment using the following primary outcome measure:
-
Mortality ‐ survival at five years.
Secondary outcomes
-
Morbidity ‐ post‐treatment complications (bleeding, mucositis, swallowing dysfunction, weight loss), immediate and delayed.
-
Voice quality ‐ at one year.
-
Recurrence of disease ‐ at five years.
-
Quality of life ‐ at one year.
-
Cost.
Search methods for identification of studies
We conducted systematic searches for randomised controlled trials. There were no language, publication year or publication status restrictions. The date of the most recent search was 18 September 2014, following previous searches in November 2013, February 2013, 2012, 2009, 2007, 2006, 2003 and 2000.
Electronic searches
We searched the following databases from their inception for published, unpublished and ongoing trials: the Cochrane Ear, Nose and Throat Disorders Group Trials Register; the Cochrane Central Register of Controlled Trials (CENTRAL 2014, Issue 8); PubMed; EMBASE; CINAHL; LILACS; KoreaMed; IndMed; PakMediNet; CAB Abstracts; Web of Science; ClinicalTrials.gov; ICTRP; Google Scholar and Google. In searches prior to 2013, we also searched BIOSIS Previews 1926 to 2012, ISRCTN and CNKI.
We modelled subject strategies for databases on the search strategy designed for CENTRAL. Where appropriate, we combined subject strategies with adaptations of the highly sensitive search strategy designed by The Cochrane Collaboration for identifying randomised controlled trials and controlled clinical trials (as described in theCochrane Handbook for Systematic Reviews of Interventions Version 5.1.0, Box 6.4.b. (Handbook 2011)). Search strategies for major databases including CENTRAL are provided in Appendix 1.
Searching other resources
We scanned the reference lists of retrieved review articles to identify other trials and wrote to a number of researchers who had published in this area. We handsearched the Proceedings of the 2nd World Congress on Laryngeal Cancer and the 5th International Conference for Head and Neck Cancer for abstracts of, and references to, other relevant studies.
Data collection and analysis
Selection of studies
One author performed the searches and two authors reviewed the abstracts. We requested and translated manuscripts of potentially relevant studies whenever necessary. Laura Warner (LW) and Paola Dey (PD) reviewed relevant manuscripts to identify reports of randomised controlled trials comparing the interventions of interest in patients with early‐stage laryngeal cancer. When randomised controlled trials were identified we obscured information which could identify the journal of publication, authors' names and their affiliation before the manuscripts were independently assessed by two further authors (Kenneth McKenzie (KMacK) and Richard Wight (RW)) to determine eligibility for inclusion in the review and methodological quality.
Data extraction and management
Two authors used a data extraction form adapted from the proforma designed by the Cochrane Musculoskeletal Injuries Group to extract data and assess risk of bias. PD contacted the authors of the included trial for additional information.
Assessment of risk of bias in included studies
LW and PD undertook assessment of the risk of bias of the included trials independently, with the following taken into consideration, as guided by theCochrane Handbook for Systematic Reviews of Interventions (Handbook 2011):
-
sequence generation;
-
allocation concealment;
-
blinding;
-
incomplete outcome data;
-
selective outcome reporting; and
-
other sources of bias.
We used the Cochrane 'Risk of bias' tool in RevMan 5.3 (RevMan 2014), which involves describing each of these domains as reported in the trial and then assigning a judgement about the adequacy of each entry: 'low', 'high' or 'unclear' risk of bias. We reported these judgements in a 'Risk of bias' table.
Data synthesis
If there are sufficient data available from trials of comparable interventions and outcomes in future updates of this review, we will pool data in a meta‐analysis for each outcome for the following comparisons:
-
radiotherapy with surgery;
-
surgery with transoral laser surgery;
-
radiotherapy with transoral laser surgery.
We will assess statistical heterogeneity using the I2 statistic. We will use Peto odds ratios with 95% confidence intervals to summarise five‐year overall and disease‐free survival and other dichotomous variables. We will use standardised mean differences (SMD) when pooling continuous data from comparable measures. If data are available, we may undertake subgroup analysis for different tumour stages.
Results
Description of studies
Results of the search
The most recent update search in September 2014 identified 450 records, the previous search in November 2013 identified 469 records and the search in February 2013 identified 1010 records, however no new published randomised controlled trials were identified (Figure 1). In the 2014 update, we also confirmed that one study remains ongoing (Saedi 2007) (see Characteristics of ongoing studies). Other trials which we had previously identified as ongoing have either now been abandoned (Abdurehim 2009; EaStER 2006), or there was no response from the authors when contacted (Coman 2003). The EaStER feasibility randomised trial comparing the effectiveness of radiotherapy and endoscopic excision (with or without laser) is closed and recruited only 17 patients to the trial, however the patients were reported as being followed up, so the status is unknown (EaStER 2006) (see Characteristics of studies awaiting classification).
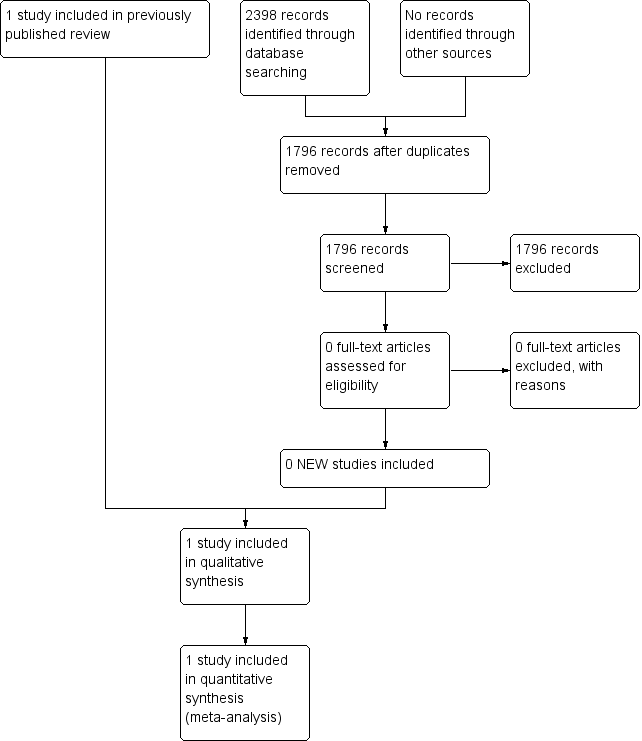
Study flow diagram.
A total of 962 abstracts had been reviewed following the update searches covering the period 2000 to October 2009. The original searches for the review identified 455 abstracts. From the combined searches we identified four possible randomised controlled trials comparing surgery and radiotherapy. We excluded three of these, with reasons (Hintz 1979; Li 1993; Yin 2000), and we included one trial in the review (Ogoltsova 1990). We identified no randomised controlled trials including endolaryngeal surgery.
Included studies
See Characteristics of included studies.
Only one trial recruited a substantial number of patients with glottic cancer; this was a multicentre randomised controlled trial undertaken in Eastern Europe, that is the former Soviet Union, Hungary and Czechoslovakia (Ogoltsova 1990). Patients were recruited from 1979 and randomised to open surgery, radiotherapy or a combination of radiotherapy and chemotherapy after stratification by anatomical site (glottis or supraglottis) and tumour stage (T1 or T2). Two hundred and sixty‐nine patients were evaluated, of whom 234 had glottic laryngeal cancer. Patients were followed up for five years and recurrence‐free and survival rates were reported.
Excluded studies
See Characteristics of excluded studies.
Hintz et al reported the results of a randomised controlled trial involving 108 head and neck patients. We excluded this trial because of the small number of eligible patients who were recruited between 1971 and 1976. Seventy‐five patients were available for analysis of whom only 24 had early stage glottic cancer; staging was retrospective. Patients were not stratified by site or stage before randomisation and of eight patients with T2 glottic cancer only one received surgery. Analysis was not on an intention‐to‐treat basis. The authors suggest that radiotherapy dosimetry may have been sub‐optimal (Hintz 1979).
We excluded one trial immediately after translation; this randomised controlled trial reported on the efficacy of preoperative radiotherapy and only 14 patients with early glottic laryngeal cancer were randomised to surgery alone (Li 1993).
We excluded a further trial because it assessed the effectiveness of postoperative radiotherapy, and the stage of disease was not clearly defined (Yin 2000).
Abdurehim 2009, which we had previously identified as an ongoing study, has now been abandoned due to difficulty recruiting patients.
Risk of bias in included studies
We had a number of concerns about the methodology of the included study (Ogoltsova 1990), and we originally gave it a 'grade C' quality rating. At the 2014 update, using the Cochrane 'Risk of bias' tool, we judged it to be at high risk of bias.
Allocation
Randomisation was by consecutive numbers, which were implemented in each co‐operative centre by "converters", but it is not clear whether the randomisation schedule was concealed from the investigators. The total number of patients randomised to each treatment arm is not provided and data are not available on the baseline characteristics of treatment groups at study entry. The number of patients evaluated in each group is unbalanced; 76 were allocated surgery but 129 allocated radiotherapy. A further 64 evaluable patients were allocated combination therapy, that is radiotherapy and chemotherapy; these patients are not further considered in this review. There is no evidence that the trial was designed with 2:1 allocation, but the authors do admit that follow‐up was poor and therefore the imbalance may be due to differential follow‐up.
Blinding
Outcomes were not assessed blind and no detail is provided on how and when outcome assessment was performed.
Incomplete outcome data
There were difficulties with the completion of follow‐up and loss of patients to follow‐up during the study is mentioned.
Selective reporting
The number of patients with glottic cancer evaluated in each arm is not provided. The number of patients in each arm available for outcome evaluation at specified time points is not available.
Other potential sources of bias
The method of diagnosis and preoperative staging is not detailed, but the investigators suggest that patients had been inadequately staged before treatment. The authors were concerned that surgical interventions had not been standardised and that radiotherapy regimens may be sub‐optimal; patients received gamma irradiation suggesting the use of cobalt units and neither treatment volume nor technique are reported.
Survival is compared using a Mantel‐Haenszel test and the Chi² statistic at 1 degree of freedom is reported at the one‐sided 5% significance level.
Effects of interventions
One study is included in the review (Ogoltsova 1990).
Primary outcome
Mortality ‐ survival at five years
Five‐year survival rates are presented for each tumour stage (T1 and T2) for patients with glottic cancer. The number of events and the number of patients at risk in each arm at each specified time point are not presented. For T1 tumours, the five‐year survival was 91.7% following radiotherapy and 100% following surgery and for T2 tumours, 88.8% following radiotherapy and 97.4% following surgery. There were no significant differences in survival between the two groups.
Secondary outcomes
Morbidity ‐ post‐treatment complications (bleeding, mucositis, swallowing dysfunction, weight loss), immediate and delayed
No data were available for this outcome.
Voice quality ‐ at one year
No data were available for this outcome.
Recurrence of disease ‐ at five years
Five‐year locoregional recurrence rates are presented for each tumour stage for patients with glottic cancer. Again the number of events and the number of patients at risk in each arm at each specified time point are not presented. There is some inconsistency in the text regarding the number of locoregional recurrences in the whole group. For T1 tumours, the five‐year disease‐free survival rate was 71.1% following radiotherapy and 100.0% following surgery, and for the T2 tumours, 60.1% following radiotherapy and 78.7% following surgery. Only the latter comparison is statistically significant (Chi 1.8, P value = 0.036), but statistical significance would not have been achieved with a two‐sided test.
Quality of life ‐ at one year
No data were available for this outcome.
Cost
No data were available for this outcome.
Discussion
Summary of main results
There is no good evidence available from randomised controlled trials to guide treatment choice for patients with early‐stage glottic cancer.
Quality of the evidence
Interpretation of the findings of the only randomised controlled trial that recruited substantial numbers of patients to a comparison between radiotherapy and open surgery is limited by concerns about the adequacy of treatment regimens and deficiencies in the reporting of the study design and analysis. In this trial, open surgical outcomes were better than might be expected from data derived from case series whilst radiotherapy outcomes were worse. The trial investigators admitted that patients were inadequately staged prior to therapy, and radiotherapy may have been sub‐optimal. In addition, follow‐up was poor and differences between groups may be biased by differential follow‐up.
There are no published randomised controlled trials comparing the effectiveness of endolaryngeal resection with either radiotherapy or open surgery and difficulties in recruiting and randomising patients with early laryngeal cancers has been noted by authors of abandoned studies. The difficulties in recruiting to the EaStER trial are addressed in a paper by Hamilton et al, who describe a difference in surgeons' and recruiters' opinions of optimum treatment of carcinoma in situ and those tumours involving the anterior commissure. Additionally, the recruiters felt that there was non‐equivalence of the treatment process as endolaryngeal surgery was often considered by patients and clinicians to be more convenient compared to radiotherapy and therefore consent to randomisation was not given (Hamilton 2013).
Potential biases in the review process
At the 2014 update, using the Cochrane 'Risk of bias' method, we judged the included study to be at high risk of bias (Ogoltsova 1990).
Agreements and disagreements with other studies or reviews
Our recent search has identified five systematic reviews comparing endolaryngeal surgery and radiotherapy published since 2009 (Abdurehim 2011; Feng 2011; Higgins 2009; Spielmann 2010; Yoo 2013). None identified any randomised trials and they varied in staging criteria, types of study (comparative only or case series and comparative studies) and outcomes for study inclusion. Those including comparative studies only suggest similar oncological and functional outcomes (Abdurehim 2011; Feng 2011; Spielmann 2010; Yoo 2013).
Several studies have reported use of concomitant chemoradiotherapy in the treatment of T2 laryngeal cancers (Niibe 2007; Ohguri 2008). The results show promising local control rates, particularly when combined with debulking transoral laser surgery. In years to come concomitant chemoradiotherapy may gain popularity as it offers organ preservation with improved local control rates. The efficacy of this new approach will need to be further elucidated.

