Programas de entrenamiento grupales para padres para mejorar su salud psicosocial
Resumen
Antecedentes
La salud psicosocial de los padres puede tener un efecto significativo sobre la relación entre padres e hijos, con consecuencias en la salud psicológica posterior del niño. Se ha demostrado que los programas de crianza tienen un impacto sobre la adaptación emocional y conductual de los niños, pero hasta la fecha, no se han realizado revisiones de su impacto sobre el bienestar psicosocial de los padres.
Objetivos
Evaluar si los programas de crianza grupales son efectivos para mejorar el bienestar psicosocial de los padres (por ejemplo, ansiedad, depresión, culpa, confianza).
Métodos de búsqueda
El 5 de diciembre de 2011 se realizaron búsquedas en las siguientes bases de datos: CENTRAL (2011, número 4), MEDLINE (desde 1950 hasta noviembre de 2011), EMBASE (desde 1980 hasta la semana 48 de 2011), BIOSIS (desde 1970 hasta el 2 de diciembre de 2011), CINAHL (desde 1982 hasta noviembre de 2011), PsycINFO (desde 1970 hasta la semana cinco de noviembre de 2011), ERIC (desde 1966 hasta noviembre de 2011), Sociological Abstracts (desde 1952 hasta noviembre de 2011), Social Science Citation Index (desde 1970 hasta el de 2 diciembre de 2011), metaRegister of Controlled Trials (5 de diciembre de 2011), NSPCC Library (5 de diciembre de 2011). El 10 de noviembre de 2012 se realizaron búsquedas en ASSIA (desde 1980 hasta la actualidad) y la última búsqueda en el National Research Register fue en el 2005.
Criterios de selección
Se incluyeron ensayos controlados aleatorios que compararon un programa de crianza grupal con una condición control y que utilizaron al menos una medida estandarizada de la salud psicosocial de los padres. Las condiciones control podrían ser lista de espera, ningún tratamiento, tratamiento habitual o placebo.
Obtención y análisis de los datos
Al menos dos revisores extrajeron los datos y evaluaron el riesgo de sesgo en cada estudio de forma independiente. Los estudios se examinaron para obtener cualquier información sobre los efectos adversos. Cuando faltó información en los informes de los ensayos, se estableció contacto con los autores. El efecto del tratamiento se estandarizó para cada resultado de cada estudio al dividir la diferencia de medias de las puntuaciones posteriores a la intervención entre los grupos de intervención y control mediante la desviación estándar agrupada.
Resultados principales
Se incluyeron 48 estudios con 4937 participantes que abarcaron tres tipos de programas: conductuales, cognitivo conductuales y multimodales. En general, se encontró que los programas de crianza grupales provocaron mejorías a corto plazo estadísticamente significativas en la depresión (diferencia de medias estandarizada [DME] ‐0,17; intervalo de confianza [IC] del 95%: ‐0,28 a ‐0,07), la ansiedad (DME ‐0,22; IC del 95%: ‐0,43 a ‐0,01), el estrés (DME ‐0,29; IC del 95%: ‐0,42 a ‐0,15 ), la ira (DME ‐0,60; IC del 95%: ‐1,00 a ‐0,20), la culpa (DME ‐0,79; IC del 95%: ‐1,18 a ‐0,41), la confianza (DME ‐0,34; IC del 95%: ‐0,51 a ‐0,17) y la satisfacción en cuanto a la relación con la pareja (DME ‐0,28; IC del 95%: ‐0,47 a ‐0,09). Sin embargo, solo el estrés y la confianza permanecieron estadísticamente significativos a los seis meses de seguimiento y ninguno fue significativo un año más tarde. No hubo pruebas de efectos sobre la autoestima (DME ‐0,01; IC del 95%: ‐0,45 a 0,42). Ninguno de los ensayos informó sobre la agresión ni los efectos adversos.
Los datos limitados centrados explícitamente en los resultados de los padres mostraron una mejoría a corto plazo estadísticamente significativa en el estrés de los padres (DME ‐0,43; IC del 95%: ‐0,79 a ‐0,06). No fue posible combinar los datos de otros resultados y los resultados de los estudios individuales no fueron concluyentes en cuanto a los efectos sobre los síntomas depresivos, la confianza ni la satisfacción con la pareja.
Conclusiones de los autores
Los hallazgos de esta revisión apoyan el uso de los programas de crianza para mejorar el bienestar psicosocial de los padres a corto plazo. Se podría necesitar aporte adicional para asegurar que se mantengan estos resultados. Se necesitan más estudios de investigación que consideren explícitamente los efectos beneficiosos para los padres y que examinen la efectividad comparativa de diferentes tipos de programas junto con los mecanismos por los cuales dichos programas producen mejorías en el funcionamiento psicosocial de los padres.
Resumen en términos sencillos
Entrenamiento para los padres para mejorar su salud psicosocial
La salud psicosocial de los padres puede tener un efecto significativo sobre la relación entre padres e hijos, con consecuencias en la salud psicológica posterior del niño. Algunos programas de crianza intentan mejorar aspectos del bienestar de los padres y esta revisión analizó específicamente si los programas de crianza grupales son efectivos para mejorar cualquier aspecto de la salud psicosocial de los padres (por ejemplo, ansiedad, depresión, culpa, confianza).
Se efectuaron búsquedas en bases de datos electrónicas para obtener ensayos controlados aleatorios en los cuales los participantes se habían asignado a un grupo experimental o control y que informaran resultados de al menos una medida científicamente estandarizada de la salud psicosocial de los padres.
Se incluyeron 48 estudios con 4937 participantes que abarcaron tres tipos de programas: conductuales, cognitivo conductuales y multimodales. En general, los resultados indicaron mejorías a corto plazo estadísticamente significativas en los padres con respecto a la depresión, la ansiedad, el estrés, la ira, la culpa, la confianza y la satisfacción en cuanto a la relación con la pareja. Sin embargo, solo el estrés y la confianza permanecieron estadísticamente significativos a los seis meses de seguimiento y ninguno fue significativo un año más tarde. No hubo pruebas de efectividad en cuanto a la autoestima en cualquier punto temporal. Ninguno de los estudios informó sobre la agresión ni los resultados adversos.
Sólo cuatro estudios informaron los resultados de los padres de forma separada. Estos datos limitados mostraron una mejoría a corto plazo estadísticamente significativa en el estrés de los padres, pero no indicaron si los programas de crianza fueron útiles en cuanto a la mejoría de los síntomas depresivos, la confianza ni la satisfacción con la pareja.
Esta revisión muestra pruebas de los efectos beneficiosos a corto plazo de los programas de crianza sobre la depresión, la ansiedad, el estrés, la ira, la culpa, la confianza y la satisfacción en cuanto a la relación con la pareja. Los hallazgos indican que se podría necesitar aporte adicional para ayudar a los padres a mantener estos efectos beneficiosos. Sin embargo, se necesitan más estudios de investigación que consideren explícitamente los efectos beneficiosos para los padres y que proporcionen pruebas de la efectividad comparativa de diferentes tipos de programas e identifiquen los mecanismos involucrados para producir un cambio.
Authors' conclusions
Background
Description of the condition
Parental psychosocial functioning is a significant factor influencing a range of aspects of children's development and wellbeing (see below). It consists of a wide range of components but those most frequently researched in terms of their impact on the wellbeing of children include parental mental health (that is depression and anxiety, parental confidence and parental conflict). The available evidence relates to infancy and toddlerhood, and to mid‐childhood and adolescence.
1. Infant and toddlerhood
The postnatal period has been identified as being of particular importance in terms of the infant's need for affectively attuned parenting (Jaffe 2001) and for parental reflective functioning (Fonagy 1997), both of which are now thought to be central to the infant's capacity to develop a secure attachment to the primary caregiver (Van IJzendoorn 1995; Grienenberger 2005). Parental psychosocial functioning can impact on the parent's capacity to provide this type of parenting. For example, one study found that depressed mothers were less sensitively attuned to their infants, less affirming and more negating of infant experience compared with parents not experiencing postnatal depression (Murray 1992); and that these infants had poorer cognitive outcomes at 18 months (Murray 1996), performed less well on object concept tasks, were more insecurely attached to their mothers and showed more behavioural difficulties (Murray 1996). Boys of postnatally depressed mothers may also score lower on standardised tests of intellectual attainment (Sharp 1995). A clinical diagnosis of postnatal depression is associated with a fourfold increase in risk of psychiatric diagnosis at age 11 years (Pawlby 2008). Recent research has also identified that the impact of postnatal depression on insecure child attachment may be moderated by maternal attachment state of mind (McMahon 2006). The chronicity of the depression appears to be a significant predictor, with depression lasting throughout the first 12 months being associated with poorer cognitive and psychomotor development for both boys and girls compared with no evidence of impact for brief periods of depression (Cornish 2008).
Recent research shows that paternal postnatal depression can have an effect that is similar in magnitude to that of maternal depression. Ramchandani 2008 showed that boys of fathers who were depressed during the postnatal period had an increased risk of conduct problems at age 3.5 years, and that boys of fathers who were depressed during both the prenatal and postnatal periods had the highest risks of subsequent psychopathology at 3.5 years and psychiatric diagnosis at seven years of age (Ramchandani 2008).
Neurodevelopmental research suggests that postnatal depression impacts the child's developing neurological system (Schore 2005). For example, one study found that infants of depressed mothers exhibited reduced left frontal electroencephalogram (EEG) activity (Dawson 1997). Parent‐infant interaction can also impact on the infant's stress regulatory system, one study showing that exposure to stress during the early postnatal period that was not mediated by sensitive parental caregiving had an impact on the infant's hypothalamic‐pituitary‐adrenocorticol (HPA) system (Gunnar 1994), which plays a major role in both the production and regulation of glucocorticoid cortisol in response to such stress.
Maternal anxiety during the postnatal period is also associated with poorer outcomes. For example, Beebe 2011 found that maternal anxiety biased the interaction toward interactive contingencies that were both heightened (vigilant) in some modalities and lowered (withdrawn) in others, as opposed to being in the 'mid‐range', which has been identified as optimal for later development, including secure attachment (Beebe 2011).
2. Mid‐childhood and adolescence
There is also evidence to show a significant impact of parental psychosocial functioning on older children. A review of longitudinal studies found that by the age of 20 years, children of affectively ill parents have a 40% chance of experiencing an episode of major depression and are more likely to exhibit general difficulties in functioning, including increased guilt and interpersonal difficulties such as problems with attachment (Beardslee 1998). More recently, maternal psychological distress has been identified as being a risk factor for conduct and emotional problems. Parry‐Langdon 2008 found that higher scores on the General Health Questionnaire (GHQ‐12) were an independent risk factor for conduct disorder (odds ratio (OR) 2.2) and for child emotional problems (OR 2.2). This OR increased to 3.5 for both emotional and behavioural problems where maternal scores on the GHQ‐12 were initially low and then subsequently increased.
One longitudinal study that focused on parental conflict found that adolescents' perceptions of typical interparental conflict directly predicted increases in depressive symptoms (particularly for girls) and aggressive behaviours (particularly for boys) over a period of a year, and that this was not mediated by parental style or quality (McGuinn 2004). This study found a significant impact on the wellbeing of adolescents who witnessed even 'normative' marital discord. Another aspect of parental psychosocial functioning is parental confidence, which has been shown to be strongly associated with parent‐child interactions that are characterised by inconsistency, guilt, detachment and anxiety (Martin 2000). One meta‐analysis also found that paternal depression was significantly related to internalising and externalising psychopathology in children, and to father‐child conflict (Kane 2004).
It is suggested that the mechanism linking parental psychosocial functioning and child outcomes is the impact of such functioning on parenting behaviours, and Waylen 2010 found that worsening parental mental health was associated with reduced parenting capacity. Similarly, Wilson 2010 found a significant deleterious impact of paternal depression on both positive and negative parenting behaviours. One longitudinal study also suggested a more complex pathway in which parental depressive symptoms were associated 12 months later with increased insecurity in adult close relationships and interparental conflict (Shelton 2008). This study showed that such conflict had a negative impact on children's appraisals of parents, which was in turn was associated with children's internalising and externalising problems (Shelton 2008).
Overall, this evidence suggests that parental psychosocial functioning can impact on the parents' capacity to provide affectively attuned interaction during infancy and toddlerhood, and an impact on older children as a result of the consequences of compromised parental psychosocial functioning for parenting behaviours and marital adjustment.There is, therefore, considerable potential for interventions aimed at promoting the psychosocial wellbeing of parents to reduce the disruption to the child's emotional, educational and social adjustment, and thereby to promote the mental health of future generations.
Description of the intervention
Parenting programmes are underpinned by a range of theoretical approaches (including behavioural, cognitive‐behavioural, family systems, Adlerian) and can involve the use of a range of techniques in their delivery including discussion, role play, watching video vignettes and homework. Behavioural parenting programmes are based on social learning principles and teach parents how to use a range of basic behavioural strategies for managing children’s behaviour, and some of these programmes involve the use of videotape modelling. Cognitive parenting programmes are aimed at helping parents to identify and change distorted patterns of belief or thought that may be influencing their behaviour, and cognitive‐behavioural programmes combine elements of both types of strategy. Other types of programme often combine some of these strategies. For example, Adlerian programmes focus on the use of 'natural and logical consequences' and 'reflective listening' strategies.
Parenting programmes are typically offered to parents over the course of eight to 12 weeks, for about one to two hours each week. They can be delivered on a one‐to‐one basis or to groups of parents and are provided in a number of settings, ranging from hospital or social work clinics to community‐based settings such as general practitioner (GP) surgeries, schools and churches. They typically involve the use of a manualised and standardised programme or curriculum, and are aimed at increasing the knowledge, skills and understanding of parents.
Recent evidence shows that parenting programmes can improve the emotional and behavioural adjustment of children under three years (Barlow 2010) and of children aged three to 10 years with conduct and behaviour problems (Dretze 2005). A review of studies focused on teenage parents found that parenting programmes improved parental responsiveness to the child and parent‐child interaction (Barlow 2011). Reviews of qualitative evidence point to a range of benefits of taking part in a group with other parents (Kane 2003).
How the intervention might work
The mechanism by which parenting programmes may impact on parental psychosocial wellbeing is thought to be twofold. Firstly, parenting programmes are, on the whole, strengths‐based, and are aimed at enhancing parental capacity and changing parenting attitudes and practices in a non‐judgemental and supportive manner, with the overall aim of improving child emotional and behavioural adjustment. For example, Patterson’s coercion theory (Patterson 1992) demonstrates the way in which parents are increasingly disempowered as a result of a process of escalation in which parents who 'give in' to child demands are increasingly likely to need more coercive strategies on the next occasion. The process in which problems escalate and parents feel increasingly disempowered may explain in part why parents experience stress and depression directly related to the parenting role.The potential impact of parenting programmes on parental psychosocial functioning may be due to the way in which such programmes help parents to address significant issues in terms of their child's wellbeing, and increase their skills and capacity to support their child's physical and emotional development (for example, Dretze 2005; Barlow 2011).
Secondly, many parenting programmes, particularly those that are underpinned by a cognitive or cognitive‐behavioural approach, may also provide parents with strategies that are directly aimed at improving parental psychological functioning. Any improvements that occur may be a result of the parents' application of such strategies to themselves instead of, or in addition to, the use of strategies focused on improving child behaviour.
Research also suggests that parenting programmes can improve other aspects of parental psychosocial functioning such as marital relations and parenting stress (Todres 1993). Factors such as marital conflict and parental stress can have a direct impact on children, in addition to being mediators of other parental problems (for example, poor mental health). Improvements in marital conflict and parental stress will, as such, have beneficial consequences in terms of children's later development.
Thus, although a number of studies have shown that parenting programmes can have an impact on aspects of maternal mental health and wellbeing, including reducing anxiety (Morawska 2009) and depression (Pisterman 1992a), it is not currently clear whether such improvements reflect the impact of strategies directly targeting parental mental health or whether they occur as an indirect result of the parent's improved ability to manage their children's behaviour and of improvements in family functioning more generally.
Therefore, although the causal mechanism is not entirely clear, parenting programmes appear to have considerable potential to impact one or more aspects of parental psychosocial functioning. It should be noted, however, that although parents who are experiencing anxiety and depression unrelated to the parenting role may also have a compromised ability to function as a parent, with consequences in terms of their children's wellbeing. The needs of such parents are not addressed by the current review, which does not include programmes provided to parents with clinical mental health or psychiatric problems.
Why it is important to do this review
The aim of this review is to evaluate the effectiveness of group‐based parenting programmes in improving the psychosocial health of parents, by appraising and collating evidence from existing studies that have used rigorous methodological designs and a range of standardised outcome instruments. The results will inform the broader debate concerning the role and effectiveness of parenting programmes.
Objectives
To update an existing review examining the effectiveness of group‐based parenting programmes in improving parental psychosocial health (for example, anxiety, depressive symptoms, self‐esteem).
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled trials (RCTs) and quasi‐randomised controlled trials in which participants had been randomly allocated to an experimental or a control group, the latter being a waiting‐list, no treatment, treatment as usual (normal service provision) or a placebo control group.
Quasi‐randomised controlled trials are defined as trials where allocation was done on the basis of a pseudo‐random sequence, for example, odd or even hospital number, date of birth or alternation (Higgins 2008).
We did not include studies comparing two different therapeutic modalities (that is, without a control group).
Types of participants
We included studies that targeted adult (rather than teenage) parents (including mothers, fathers, grandparents, foster parents, adoptive parents or guardians) from either population or clinical samples (that is, with or without child behavioural problems) with parental responsibility for the day‐to‐day care of children, and who were eligible to take part in a parent training programme aimed at helping them to address some aspect of parental functioning (for example, attitudes and behaviour).
We included studies of parenting programmes delivered to all parents, not just those at risk of poor psychosocial health and child behavioural problems. Although we are addressing the impact of parenting programmes on aspects of parental psychosocial functioning such as anxiety and depression, we excluded studies that explicitly targeted and thereby focused solely on parents with a diagnosed psychiatric disorder, for example, clinical depression. This reflects the fact that parenting programmes are primarily provided to address children's social, emotional and behavioural functioning, and although parents with clinical psychiatric conditions may benefit from a parenting programme, these would not typically be provided as the primary source of treatment. Parents with clinical psychiatric conditions should be the focus of a separate review.
We included studies of parents who had children with a disability if the intervention was aimed at supporting or changing parenting and the study also measured parental psychosocial health.
We excluded studies that focused solely on child outcomes, preparation of parents for parenthood or that were directed at pregnant or parenting teenagers (below the age of 20 years).
Types of interventions
We included parenting programmes meeting the following criteria:
-
group‐based format;
-
standardised or manualised programme;
-
any theoretical framework including behavioural, cognitive and cognitive‐behavioural (please see Description of the intervention);
-
developed largely with the intention of helping parents to manage children's behaviour and improve family functioning and relationships.
We excluded programmes:
-
provided to parents on an individual or self‐administered basis;
-
that involved direct work with children;
-
that involved other types of service provision, such as home visits;
-
in studies that included only measures of parental attitudes (for example, Parental Attitude Test) or of family functioning (for example, McMaster Family Assessment Device) because, although these may reflect the family's functioning as a group, they are not direct measures of parental psychosocial health.
Types of outcome measures
Primary outcomes
Outcomes measured using standardised instruments including the measures detailed below.
Depressive symptoms
Parental depressive symptoms measured, for example, through improvement in scores on the Beck Depression Inventory (BDI) (Beck 1961) or similar standardised instrument.
Anxiety symptoms
Parental anxiety measured, for example, through improvement in scores on the Beck Anxiety Inventory (BAI) (Beck 1988) or similar standardised instrument.
Stress
Parental stress measured, for example, through improvement in scores on the Parenting Stress Index (PSI) (Abidin 1983) or similar standardised instrument.
Self‐esteem
Parental self‐esteem measured, for example, through improvement in scores on the Rosenberg Self‐Esteem scale (RSE) (Rosenberg 1965) or similar standardised instrument.
Anger
Parental anger measured, for example, through improvement in scores on the Brief Anger‐Aggression Questionnaire (BAAQ) (Maiuro 1987) or similar standardised instrument.
Aggression
Parental aggression measured, for example, through improvement in scores on the Brief Anger‐Aggression Questionnaire (BAAQ) (Maiuro 1987) or similar standardised instrument.
Guilt
Parental guilt measured, for example, through improvement in scores on the Situation of Guilt Scale or similar (SGS) (Klass 1987) or similar standardised instrument.
Secondary outcomes
Confidence
Parental confidence measured through improvement in scores on the Parent Sense of Competence Scale (PSC) (Johnston 1989) or similar standardised instrument.
Partner satisfaction
Marital or partner satisfaction measured through improvement in scores on the Dyadic Adjustment Scale (DAS) (Spanier 1976) or similar standardised instrument.
Adverse effects
Any adverse effects relating to parental psychosocial health including, for example, increase in tension between parents.
Search methods for identification of studies
Electronic searches
The previous version of this review was based on searches run in 2002. This update is based on searches run in 2008, 2010 and 2011. We added the metaRegister of Controlled Trials to search for completed and ongoing trials. We could not update the searches in SPECTR or the National Research Register because they had ceased to exist by 2008. Since the previous version of the review, Sociological Abstracts replaced Sociofile and PsycINFO replaced PsycLIT. During the update, ERIC and Sociological Abstracts moved to new search platforms and the original search strategies were adapted accordingly. All search strategies used for this update are reported in Appendix 1.
We searched the following electronic databases.
-
Cochrane Central Register of Controled Trials (CENTRAL), part of the Cochrane Library (2011, Issue 4), last searched 5 December 2011.
-
MEDLINE (Ovid) 1950 to November 2011, last searched 5 December 2011.
-
EMBASE (Ovid) 1980 to 2011 Week 48, last searched 5 December 2011.
-
CINAHL (EBSCO) 1982 to current, last searched 5 December 2011.
-
BIOSIS 1970 to 2 December 2011, last searched 5 December 2011.
-
PsycINFO 1970 to week 5 November 2011, last searched 5 December 2011.
-
Sociological Abstracts (Proquest), 1952 to current, last searched 5 December 2011.
-
Sociological Abstracts (CSA), 1963 to current, last searched March 2010.
-
Social Science Citation Index, 1956 to 2 December 2011, last searched 5 December 2011.
-
ASSIA 1980 to current, last searched 10 November 2011.
-
ERIC (via www.eric.ed.gov), 1966 to current, last searched 7 December 2011.
-
ERIC (via OVID), 1966 to current, last searched March 2010.
Searching other resources
-
NSPCC library database (last searched 5 December 2011).
-
metaRegister of Controlled Trials (last searched 5 December 2011).
-
Reference lists of articles identified through database searches were examined for further relevant studies. We also examined bibliographies of systematic and non‐systematic review articles to identify relevant studies.
Data collection and analysis
Selection of studies
For the first published versions of this review (Barlow 2001; Barlow 2003), we identified titles and abstracts of studies through searches of electronic databases and reviewed the results to determine whether the studies that appeared relevant met the inclusion criteria. For the original review Esther Coren (EC) identified titles and abstracts and these were screened by EC and JB. Two review authors (EC and JB) independently assessed full copies of papers that appeared to meet the inclusion criteria. We resolved uncertainties concerning the appropriateness of studies for inclusion in the review through consultation with a third review author, Sarah Stewart‐Brown (SS‐B). For the update of the review, Nadja Smailagic (NS) and Nick Huband (NH) carried out the eligibility assessments in consultation with JB and Cathy Bennett (CB). JB had overall responsibility for the inclusion or exclusion of studies in this review.
Data extraction and management
Two review authors extracted data independently (JB and EC or SS‐B; later NS and NH) using a data extraction form and entered the data into Review Manager 5 (RevMan) (RevMan 2011). Where data were not available in the published trial reports, we contacted trial investigators to supply missing information.
Some of the standardised measures used in the studies included in this review are reversed, such that a high score is considered to represent an improvement in outcome. We investigated whether the study investigators had used any methods to correct for this, for example, by reversing the direction of the scale by multiplying the mean values by ‐1 or by subtracting the mean from the maximum possible for the scale, to ensure that all the scales pointed in the same direction. For data entry into RevMan, we consistently multiplied the mean values by ‐1 for those scales where a higher score implies lower disease severity, unless this correction had already been made in the published report. Where there was ambiguity about the method of correction, we contacted the study investigators for further information.
Timing of outcome assessment
We extracted data for the following time points:
-
post‐intervention assessment, immediately post‐intervention (up to one month following the delivery of the intervention);
-
short‐term follow‐up assessment, two to six months post‐intervention;
-
long‐term follow‐up assessment, more than six months post‐intervention.
Assessment of risk of bias in included studies
For each included study, three review authors (NH, NS and HJ) independently completed the Cochrane Collaboration’s tool for assessing risk of bias (Higgins 2008, Section 8.5.1). Any disagreement was resolved in consultation with a third review author (CB). We assessed the degree to which:
-
the allocation sequence was adequately generated (‘sequence generation’);
-
the allocation was adequately concealed (‘allocation concealment’);
-
knowledge of the allocated interventions was adequately prevented during the study (‘blinding’);
-
incomplete outcome data were adequately addressed;
-
reports of the study were free of suggestion of selective outcome reporting;
-
the study was apparently free of other problems that could put it at high risk of bias.
Each domain was allocated one of three possible categories for each of the included studies: low risk of bias, high risk of bias, or 'unclear risk' where the risk of bias was uncertain or unknown.
The first published version of this review used a quality assessment method that we elected not to use in this updated review, instead following guidance from the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2008) concerning the assessment of risk of bias.
Measures of treatment effect
For continuous data that were reported using standardised scales, we calculated a standardised mean difference (effect size) by subtracting the mean post‐intervention scores for the intervention and control groups and dividing by the pooled standard deviation.
Unit of analysis issues
Cluster‐randomised trials
The randomisation of clusters can result in an overestimate of the precision of the results (with a higher risk of a Type I error) where their use has not been compensated for in the analysis. Some meta‐analyses involved combining data from cluster‐randomised trials with data from individually‐randomised trials. Five of the included studies were cluster‐randomised (Wolfson 1992; Gross 2003; Hiscock 2008; Gross 2009; Hanisch 2010). The impact of the cluster RCTs was explored using a sensitivity analysis (see Sensitivity analysis, below) and we made no adjustments to the data.
Cross‐over trials
None of the included studies involved cross‐over randomisation.
Multi‐arm trials
Eleven studies utilised more than one intervention group (Sirbu 1978; Webster Stratton 1988; Spaccerelli 1992; Blakemore 1993; Cunningham 1995; Greaves 1997; Taylor 1998; Gross 2003; Gallart 2005; Gutierrez 2007; Larsson 2009). None of the interventions in these studies were sufficiently similar to be combined to create a single pair‐wise comparison, therefore for studies where there was more than one active intervention and only one control group, we selected the intervention that most closely matched our inclusion criteria and excluded the others. In only one study (Gutierrez 2007) was it possible to include both intervention arms in the study without double counting, as a result of the use of a second control group. Gutierrez 2007 compared two parenting programmes: the 1‐2‐3 Magic Program (classified as behavioural parenting program in our review) and the STEP program (Adlerian, assigned to 'other' types of parenting in our review) against attention placebo (where parents received lectures on topics of interest unrelated to parenting) or a wait‐list control condition. In our analyses we compared the behavioural parenting program with the wait‐list control group and the STEP program with the attention placebo group.
Dealing with missing data
We assessed missing data and dropouts for each included study and we report the number of participants who were included in the final analysis as a proportion of all participants in each study. We provide reasons for missing data in the 'Risk of bias' tables of the 'Characteristics of included studies' section.
We attempted to contact the trial investigators to request missing data and information.
Assessment of heterogeneity
We assessed the extent of between‐trial differences and the consistency of results of meta‐analyses in three ways. We assessed the extent to which there were between‐study differences, including the extent to which there were variations in the population group or clinical intervention, or both. We combined studies only if the between‐study differences were minor.
We assessed heterogeneity using the I2 statistic. The importance of the observed value of I2 is dependent on the magnitude and direction of effects and strength of evidence for heterogeneity (for example, P value from the Chi2 test, or a confidence interval for I2) (Higgins 2008), and we interpreted I2 > 50% as evidence of substantial heterogeneity. We also performed the Chi2 test of heterogeneity (where a significance level less than 0.10 was interpreted as evidence of heterogeneity). We used a random‐effects model as the standard approach and identified significant heterogeneity using subgroup analyses.
Data synthesis
The included studies used a range of standardised instruments to measure similar outcomes. For example, depression was measured using the Beck Depression Inventory, the Irritability, Depression and Anxiety Scale and the Centre for Epidemiological Studies Depression Scale. We standardised the results from these different measures by calculating the treatment effect for each outcome in each study and dividing the mean difference in post‐intervention scores for the intervention and treatment groups by the pooled standard deviation to produce an effect size. Where appropriate, we then combined the results in a meta‐analysis. The decision about whether to combine data in this way was determined by the levels of clinical and statistical heterogeneity present in the population, intervention and outcomes used in the primary studies.
We have presented the effect sizes and 95% confidence intervals for individual outcomes in individual studies using figures only and have not provided a narrative presentation of individual study results.
Subgroup analysis and investigation of heterogeneity
No subgroup analysis was undertaken because there was insufficient evidence of heterogeneity.
Sensitivity analysis
At the time of the first update of this review (2003), sensitivity analyses were conducted to assess the impact on the results of the two studies classified as quasi‐randomised. This was not repeated for the current update since both studies were reclassified as excluded. We conducted a sensitivity analysis to investigate the potential impact of cluster‐randomisation methods in five studies. We had planned an a priori sensitivity analyses for studies focusing on children with disabilities, but none of the included studies involved parents of disabled children.
Results
Description of studies
Results of the search
The updated electronic searches in January 2008, March 2010 and December 2011 produced 16,609 records. The obvious duplicates were removed by one review author (NS), who inspected the abstracts and discarded 16,477 irrelevant records. Most of articles reviewed were written in English. All studies in languages other than English had abstracts in English and we excluded all these studies on the basis of the information contained in the abstracts, apart from three German studies (Heinrichs 2006; Franz 2007; Naumann 2007), which are awaiting assessment as they need to be translated. We obtained a full text copy of 132 potential included studies and two review authors independently examined each study (NS and NH). JB and CB provided advice on any studies about which there was uncertainty.
Included studies
This updated review includes 48 studies, 28 of which were published since the previous review (Barlow 2003) that were identified using full text screening against inclusion criteria (Bradley 2003; Gross 2003; Martin 2003; Wolfe 2003; DeGarmo 2004; Farrar 2005; Feliciana 2005; Gallart 2005; Lipman 2005; Treacy 2005; Wang 2005; Chronis 2006; Gardner 2006; Fanning 2007; Fantuzzo 2007; Gutierrez 2007; Hutchings 2007; Matsumoto 2007; Turner 2007; van den Hoofdakker 2007; Hiscock 2008; Gross 2009; Larsson 2009; Morawska 2009; Niccols 2009; Hanisch 2010; Joachim 2010; Matsumoto 2010). Two review authors (NS and NH) independently re‐examined the 26 studies included in the previous version of the review against the inclusion criteria and retained 20 of them in this review. Six previously included studies (Van Wyk 1983; Scott 1987; Anastopoulos 1993; Mullin 1994; Sheeber 1994; Zimmerman 1996) were excluded in this update because they did not meet the more rigorous inclusion criteria being applied (see Excluded studies for further details).
We have provided further details about the included studies in the Characteristics of included studies table.
Design
All 48 included studies were randomised controlled trials.
Most studies were two‐condition comparisons of group‐based parenting programmes against a control group (n = 37). Eleven studies utilised more than one intervention group (Sirbu 1978; Webster Stratton 1988; Spaccerelli 1992; Blakemore 1993; Cunningham 1995; Greaves 1997; Taylor 1998; Gross 2003; Gallart 2005; Gutierrez 2007; Larsson 2009). Gutierrez 2007 compared two parent education programmes (behavioural‐based and Adlerian) against two control groups, 'attention placebo' or a wait‐list control condition. In our analyses of data from this trial, we compared the behavioural parenting programme with the wait‐list control group and the Adlerian programme with the attention placebo group.
Seven studies used a no‐treatment control group (Gammon 1991; Schultz 1993; Gross 1995; Greaves 1997; Patterson 2002; DeGarmo 2004; Hanisch 2010); three studies used a treatment‐as‐usual control group (Fantuzzo 2007; van den Hoofdakker 2007; Hiscock 2008), and three studies used an attention placebo control group (Sirbu 1978; Farrar 2005; Gutierrez 2007). In Farrar 2005 the attention placebo group received information about choosing developmentally appropriate books for their pre‐school children; in Gutierrez 2007, which had two control conditions, participants in the 'attention placebo' group were either presented lectures on topics of interest to them, but unrelated to parenting, or assigned to a wait‐list control group. In Sirbu 1978, the attention placebo group did not utilise any materials or have a professional leader, and the sessions were unstructured. The remaining 35 studies used only a wait‐list control group.
Cluster‐randomised studies
Five studies were cluster‐randomised trials (Wolfson 1992; Gross 2003; Hiscock 2008; Gross 2009; Hanisch 2010). Gross 2003 used day centres as the unit of allocation; in total seven day centres were randomly assigned to one of the three conditions: ‘parent training plus teacher condition’ (n = 4); ‘teacher training condition’ (n = 4), and ‘control condition’ (n = 3). The control centres received no intervention for at least one year, after which new parents were recruited and the centres were transferred to the ‘parent training condition’ (n = 3). Hanisch 2010 used kindergartens as the unit of allocation: 58 kindergartens were randomised to the intervention group (n = 32) or to the control group (n = 26). Hiscock 2008 used primary‐care nursing centres as the unit of allocation: 40 centres were randomly assigned to the intervention group (n = 18) or to the control group (n = 22). Wolfson 1992 employed randomisation by childbirth class: 25 childbirth classes were randomised but no further details were given.
Sensitivity analysis
The randomisation of clusters can result in an overestimate of the precision of the results (with a higher risk of a Type I error) where their use has not been compensated for in the analysis. We therefore conducted a sensitivity analysis to investigate cluster effects. For this, we assumed the intracluster correlation to be 0.2, which is much bigger than normally expected. For two of the five cluster‐RCTs (Wolfson 1992; Hiscock 2008), we only had information about the number of clusters at randomisation and we therefore assumed a worst case scenario using the maximal possible cluster size, taking into account the dropouts during the study. Based on these assumptions, we assessed that the results of the meta‐analyses were robust to any clustering effects for most outcomes.
In the worst case scenario there is potential for the confidence interval to widen, depending on the weight of the clustered studies in the meta‐analysis. In cases where the effect size is borderline non‐significant (for example, analysis 1.1.2), there is potential for the meta‐analysis to become borderline significant after the adjustment. Conversely, there is potential for previous significance to be overcome following the adjustment.
In all analyses involving cluster‐corrected standard errors, the adjusted effect sizes were equivalent to the unadjusted effect sizes. In addition, in all cases the statistical conclusions were unchanged from the uncorrected to the corrected analyses.
Sample sizes
There was considerable variation in sample size between studies. Altogether the 49 included studies initially randomised 4937 participants, with sample sizes ranging from 22 to 733 (mean 102.9; median 60). Five large trials (Irvine 1999; Gross 2003; DeGarmo 2004; Hiscock 2008; Gross 2009) randomised a total of 1830 participants, with sample sizes ranging from 238 to 733 (mean 366; median 292). A further 11 studies (Webster Stratton 1988; Spaccerelli 1992; Cunningham 1995; Taylor 1998; Patterson 2002; Bradley 2003; Lipman 2005; Fantuzzo 2007; Hutchings 2007; Larsson 2009; Hanisch 2010) randomised 1481 participants, with sample sizes ranging from 110 to 198 (mean 134.6; median 126). The remaining 32 studies involved 1626 participants, with sample sizes ranging from 22 to 96 (mean 50.8; median 51).
Seven studies (Sirbu 1978; Gammon 1991; Spaccerelli 1992; Pisterman 1992b; Blakemore 1993; Schultz 1993; Bradley 2003) did not provide sufficient data to calculate effect sizes. The remaining 41 studies included in total 3416 participants with sample sizes ranging from 16 to 671 (mean 83.3; median 82).
Setting
Twenty‐two studies were conducted in the USA, 10 in Australia, seven in Canada and three in the UK. The remaining studies were conducted in China, Germany, Japan, the Netherlands and New Zealand. Most studies (n = 32) were single‐centre trials.
In 41 studies, participants were recruited from community settings by a variety of methods including flyers, emails and advertisements directed at parents of young children, or self‐referral (Sirbu 1978; Gammon 1991; Spaccerelli 1992; Wolfson 1992; Blakemore 1993; Nixon 1993; Schultz 1993; Gross 1995; Joyce 1995; Odom 1996; Greaves 1997; Taylor 1998; Webster Stratton 1988; Irvine 1999; McGillicuddy 2001; Nicholson 2002; Bradley 2003; Gross 2003; Martin 2003; Wolfe 2003; DeGarmo 2004; Farrar 2005; Feliciana 2005; Gallart 2005; Lipman 2005; Wang 2005; Chronis 2006; Gardner 2006; Fanning 2007; Fantuzzo 2007; Gutierrez 2007; Hutchings 2007; Matsumoto 2007; Turner 2007; Hiscock 2008; Gross 2009; Morawska 2009; Niccols 2009; Hanisch 2010; Joachim 2010; Matsumoto 2010); in one study from a primary care setting (Patterson 2002); in three studies from outpatient settings including an outpatient mental health clinic (van den Hoofdakker 2007), child psychiatric outpatients departments (Larsson 2009) and from a university‐based research clinic (Treacy 2005); in three studies parents were recruited from both community and outpatient settings (Pisterman 1992a; Pisterman 1992b; Cunningham 1995).
The intervention was delivered in outpatient clinics (including research clinics and paediatric outpatient departments) in seven studies (Pisterman 1992a; Pisterman 1992b; Blakemore 1993; Taylor 1998; Treacy 2005; van den Hoofdakker 2007; Larsson 2009); in primary care in one study (Patterson 2002); and in the community in the remaining studies.
Participants
An inclusion criterion for this updated review was that participants were parents with responsibility for the day‐to‐day care of children. In 19 studies, both mothers and fathers were recruited (Webster Stratton 1988; Wolfson 1992; Pisterman 1992a; Pisterman 1992b; Blakemore 1993; Nixon 1993; Schultz 1993; Gross 1995; Taylor 1998; Irvine 1999; McGillicuddy 2001; Wang 2005; Fanning 2007; Hutchings 2007; Matsumoto 2007; van den Hoofdakker 2007; Larsson 2009; Hanisch 2010; Matsumoto 2010). Thirteen studies recruited mothers only (Sirbu 1978; Gammon 1991; Odom 1996; Greaves 1997; Wolfe 2003; DeGarmo 2004; Farrar 2005; Feliciana 2005; Lipman 2005; Chronis 2006; Gutierrez 2007; Hiscock 2008; Niccols 2009). Either the mother or the father was recruited in 12 studies (Spaccerelli 1992; Cunningham 1995; Joyce 1995; Patterson 2002; Bradley 2003; Martin 2003; Gallart 2005; Gardner 2006; Fantuzzo 2007; Turner 2007; Morawska 2009; Joachim 2010). Four studies recruited not only biological parents but also grandparents, foster parents, step parents and relatives (Nicholson 2002; Gross 2003; Treacy 2005; Gross 2009). The studies included in this review were largely directed at mothers, and the trial investigators reported results that were mainly derived from the mothers.
Interventions
We provide a description by category of the structure and content of the parenting programmes that were evaluated in the included studies in 'Additional Table 1'. We have grouped the interventions into five categories according to the basic theoretical premise underpinning the programme (for example, behavioural and cognitive‐behavioural programmes) or, where there was a sufficient number of studies, according to the brand of the programme (Incredible Years and Triple‐P parenting programmes). A small group of programmes were unclassifiable (other and non‐branded multimodal programmes). For the purpose of analysis we categorised the studies as below.
| Study ID | Aim | Content/delivery |
| Behavioural only | ||
| To evaluate the effects of a brief parenting programme on positive and negative parenting behaviours. | Brief behavioural parenting program consisted of three weekly 2‐hour group meetings with booster session 4 weeks after the third session. The intervention included video material (1‐2‐3 Magic) on managing difficult child behaviours, handouts and mutual support/problem solving work. | |
| To examine the efficacy of a large group‐based parenting programme as a means of increasing the accessibility of such programmes to parents of children with disruptive behaviour; to determine whether parenting programme improve parental sense of competence and decrease depressive symptoms. | Coping modelling problem‐solving parenting programme comprised 11‐12 weekly sessions, involving the formulation of solutions through the observation of videotapes, discussion, modelling and role play. Homework reviewed each week. | |
| To evaluate changes in parent management and subsequently changes in child behaviour and maternal affects over time. | Parent Management Training (PMT) was a series of parent group meetings and discussion (14 weekly sessions). Interventionists made midweek telephone calls to encourage the participation. The program included a 30‐minute video, and covered 5 theoretically based effective parenting practices (appropriate discipline, skill encouragement, monitoring, problem solving, and positive reinforcement). Individual catch‐up sessions offered to replace missed sessions; 10% participants had at least one individual session. | |
|
| To evaluate the effectiveness of a parenting programme and assess the impact of telephone contact sessions in developing positive relationships, in encouraging desirable behaviour, in teaching new skills and behaviours, and in managing misbehaviour. | The full Group Triple‐P program comprised four weekly 2‐hour group sessions and four weekly follow‐up telephone calls. The programmes standard Facilitators Kit (leaders manual, AV materials, participants workbook) was used, plus a video (Every Parents Survival Guide). The modified Group Triple‐P program is the standard programme delivered as four weekly 2‐hour group sessions but without the four follow‐up telephone contacts. |
| Gutierrez 2007 (behavioural) | To evaluate the efficacy of two parenting programmes in reducing perceived parental stress | Behaviourally‐based parenting programme (BPP)1‐2‐3 Magic Parenting Program included components on parents reactions to their child's misbehaviour, using time‐out, dealing with testing and manipulation, positive reinforcement, and preventing relapses. see below for description of Adlerian parenting program. Compared two active parenting interventions with an attention placebo program and a wait‐list control group. Each programme consists of eight 2‐hours‐weekly sessions, delivered in Spanish. |
| To evaluate the effects of a parenting programme on child behaviour, parenting practices, parent‐child interaction, and parent quality of life | Prevention Programme for Externalising Problem behaviour (PEP) consisted of ten weekly sessions (80‐120 minutes each).
The first three sessions focused on defining individual problem situations, introducing unspecific basic strategies. The next three sessions thought participants the classical key strategies of behaviour modification. Sessions 7 to 10 consolidated these strategies by working on common difficult parenting situations. Individual homework assessments and telephone supervision were provided. | |
| To assess the effectiveness of a parenting programme in preventing early childhood behavioural problems
| The Universal parenting programme comprised of three structured sessions, covering normal development and behaviour, strategies to increase desired behaviour, and strategies to reduce unwanted behaviour. First session (child at 8 months) consisted of handouts; second and third sessions (child at 12 and 15 months) were 2‐hour group sessions. Training incorporated didactic teaching, written information, role play and video vignettes of appropriate parenting responses to childhood behaviours. | |
| To assess the effectiveness of a brief parent training in preventing behaviour problems on shopping trips.
| Brief, two‐hour, topic‐specific parent discussion group based on the Triple P‐Positive Parenting Program. Intervention entitled Hassle‐free Shopping was for parents looking for specific advice on how to manage their child's behaviour in the supermarket and how to prevent behaviour problems on shopping trips. | |
| To evaluate the effectiveness of a parenting programme provided by non‐mental health providers who are more likely to be available in small communities.
| Adolescent Transition Program was a stepwise, skill‐based curriculum designed to teach parenting skills. Content included: positive reinforcement, parental monitoring, limit‐setting, parent‐child communication, and problem solving. | |
| To evaluate the effects of a parent training in managing parents successfully functioning at work, at home, and in their parenting role.
| Work Place Triple‐P program (WPTP) consisted of four sessions (2 hours each), and four additional individual telephone consultations (15 to 30 minutes each). It was designed specifically for delivering in the workplace and involved i) teaching parents 17 core positive parenting and child management strategy; ii) planning activities routine for times such as getting ready for work and arrival home from work; iii) active training methods such as video modelling, rehearsal, practice, feedback and goal setting Parents received copy of a workbook that included exercises for completion both in‐session and between sessions. | |
| To evaluate the efficacy and acceptability of a parenting programme with Japanese parents in learning and practicing positive parenting skills
| Triple P‐Positive Parenting Program comprised of five sessions (2‐hours each), and three telephone consultation sessions (20‐30 minutes each). Active skills training methods were used to facilitate the development of a self‐regulatory framework for parents, involving modelling, role‐plays, feedback and the use of specific homework. All sessions conducted in Japanese by a Japanese accredited Triple P trainer. | |
| To evaluate the efficacy and acceptability of a parenting programme with Japanese parents in Japanese society in learning and practicing positive parenting skills
| Triple P‐Positive Parenting Program comprised of five sessions (2‐hours each), and three telephone consultation sessions (20‐30 minutes each). Active skills training methods were used to facilitate the development of a self‐regulatory framework for parents, involving modelling, role‐plays, feedback and the use of specific homework. All sessions conducted in Japanese by a Japanese accredited Triple P trainer. | |
| To assess the efficacy of a parenting program in enhancing parenting skills, and subsequently in improving the behavioural and emotional adjustment of their gifted child.
| Gifted and Talented Group Triple P programme (based on the Group Triple P intervention) consisted of five weekly sessions (2 hours each), followed by three weekly telephone consultations (15‐minutes each), and a final 2 hours group session. The program involved teaching parents core child management skills: i) promoting children's development, ii) managing misbehaviour, and iii) planned activities and routines | |
| To evaluate the effectiveness of a parenting programme in preventing challenging behaviour of their child. | COPEing with toddler behaviour comprised eight weekly group sessions (2 hours each) and focused on parenting styles and strategies in preventing challenging behaviour for children in late infancy/toddlerhood. | |
| To determine whether parent training would improve a mother's knowledge about ADHD and her feelings of competence and self‐esteem in using problem‐solving strategies. | Educational programme comprised five weekly sessions (60‐90 minutes each), including information on the pathology of ADHD, its impact on family, the effects of stimulant medication, the meaning and development of a child's behaviour, enhancing positive mother‐child attention, time‐out, positive reinforcement, and the use of problem‐solving strategies. | |
| To assess the effects of a parenting programme on parenting stress and sense of competence in parents of children with ADHD.
| Parent training programme comprised twelve weekly sessions, including information on ADHD and instruction involving role‐play, modelling and homework assignments. Compliance training component differed slightly for Study 1 and Study 2. Reading material and manuals provided for participants. | |
|
| To evaluate whether a parent mediated behaviour intervention could ameliorate ADHD related deficits and behavioural problems.
| Attention‐training treatment programme comprised twelve weekly sessions, including educational material and information about ADHD, compliance training (behaviour management) and attention training. Teaching methods includes modelling, role‐play, and individual feedback to videotaped interactions. |
| To investigate the effectiveness of a behavioural parenting programme. To examine whether lecture/written materials/combination were differentially effective in teaching behavioural principles. | Behavioural parenting programme comprised five weekly sessions (2 hours each) and a This intervention was used in Group 1. Group 2 received the same programme but without the text. Group 3 received the text only plus the exercises. Group 4 were a non‐intervention control group.
| |
| To assess the impact of a culturally sensitive adaptation of parenting programme on parental skills, parental stress, anxiety and depression. | Triple‐P Positive Parenting Program, culturally adapted, comprised eight sessions: i) one group introduction session, giving an overview of the program and establishing rapport within the groups (1.5‐2 hours); ii) four group sessions (2‐2.5 hours each); iii) two home‐based consultations (30‐40 minutes each); and iv) one final group session (1.5‐2 hours). The intervention covers modelling, rehearsal, practice, feedback and goal setting, considering needs of Australian Indigenous families. | |
| To investigate the effectiveness of parenting training as adjunct to routine clinical care in enhancing parenting skills. | Behavioural Parenting Training (BPT) comprised twelve sessions (2 hours each). The program covers the following parenting skills: i) structuring the environment, ii) setting rules, iii) giving instructions, iv) anticipating misbehaviours, v) communicating, vi) reinforcing positive behaviour, vii) ignoring, viii) employing punishment, and ix) implementing token system. As a part of homework assignment, for each session parents read a chapter of a book written for this program (van der Veen‐Mulders et al, 2001); they also practice parental skills during each session, and wrote the reports. | |
| To evaluate the effects of a parenting program on the interactive skills of parents of children with autism. | Educational parenting program comprised four weekly sessions (4 hours each), supported by home visits (4 hours in total). Training program included lectures, handouts, live modelling and group discussion, which was supported by individual home visits. The purpose of the individual home visits was to observe the parent/child interaction in the natural environment and assist parents in applying the intervention strategies thought during group training. | |
| To evaluate the effectiveness of a parenting programme in promoting healthy, self‐sufficient sleep in infants; to test the hypothesis that parent training would reduce both stress and response to child wakefulness. | Behavioural parenting training comprised two prenatal sessions and two post‐natal sessions (1‐1/2 hours each). Content included information on infant sleep and methods to assist in establishing early good sleep habits. Handouts, questions and answers, group discussion and problem‐solving strategy used. Diaries and daily practice records completed and discussed.
| |
| Cognitive‐Behavioural Parenting Programme | ||
|
| To evaluate the effectiveness of a parenting programme in enhancing the self‐directedness of children with ADHD and responsibility for their own behaviour.
| Behaviour management parenting programme consisted of 12 weekly 2‐hour sessions delivered using a lecture format. Follow‐up (maintenance) sessions at 3‐ and 6‐months. Optional school consultation time offered. Topics included the re‐framing of ADHD, behaviour management based on the use of various techniques, the grief cycle, communication skills, listening, acknowledging feelings, self‐esteem, and anger‐management. |
| To examine whether a parenting programme improve maternal functioning in terms of depressive symptoms, anxiety, self‐esteem, perceived stress and cognitions about child behaviour. | Maternal Stress and Coping Group Program was a modified version of the Coping With Depression Course Program (CWDCP), which increases its relevance for mothers of children with ADHD. It comprised twelve weekly sessions, including four treatment models: i) relaxing training, ii) increasing pleasurable activities, iii) cognitive restructuring, and iv) increasing social skills/assertiveness training. Homework exercises that involved practising behavioural skills were completed. | |
| To examine the effectiveness of a parenting programme in promoting coping skills in parents of children with developmental disabilities. | Coping Skills Training Programme consisted of ten 2‐hour weekly sessions, involving cognitive restructuring, interpersonal skills training, problem solving and individual goal attainment. | |
| To examine the effectiveness of a parenting programme in reducing child conduct problem, in enhancing positive parenting skills and confidence, and in decreasing parental depression
| Webster‐Stratton Incredible Years intervention comprised a video‐based 14‐week group programme which teaches behavioural principles for managing behaviours using a collaborative, practical problem‐solving approach. Topics included parent‐child play praise, incentives, limit‐setting, problem‐solving and discipline. Each week parents practice tasks at home. Telephone calls made to encourage progress. | |
| To evaluate the effectiveness of a parenting programme in promoting positive parent‐child relationships; to promote parental self‐efficacy. | Parent and Children Series (PACS) training programme for promoting positive parent‐child relationship consisted of 10‐weekly sessions, using manual, written materials and videos. Topics included: how to play with a child, use of praise, limit setting, use of time‐out. Video‐tape vignettes used to model skills and stimulate discussion. Weekly homework assignments used. | |
| To evaluate the relative effectiveness of a parenting programme on parenting competence (higher parenting self‐efficacy, less reliance on coercive discipline strategies, and more positive parent behaviour) | Webster‐Stratton Incredible Years BASIC Programme comprised 12 weekly sessions (2 hours each). Topics covered included child‐directed play, helping young children to learn, using praise and rewards, effective limit setting, handling misbehaviour and problem solving. Home work assignments were also used. The course was taught using video vignettes which were appropriate for toddlers. | |
| To evaluate the effectiveness of a parenting programme in improving parenting competence and child behaviour. | Chicago Parent Programme (CPP) comprised 12 weekly sessions, employing videotaped vignettes and group discussion. The topics covered the concept of child‐centred time, helping young children to learn, using praise and rewards, effective limit setting, handling misbehaviour and problem solving. | |
| To assess the effectiveness of a parenting programme in reducing parental stress in parents of children with disabilities. | Rational‐Emotive Parent Education programme comprised eight weekly sessions. Content focused on core irrational beliefs and links with stress response. Programme thought the disputation of these beliefs and their replacement with rational beliefs. Teaching based on a didactic approach and included homework, completion of worksheets, and the distribution of a prepared summary sheet. | |
| To evaluate the effectiveness of a parenting programme as a preventative intervention for parents with children considered to be at risk of developing conduct disorder | Webster‐Stratton Incredible Years Basic parenting programme comprised twelve weekly sessions (2 to 2.5 hours each) and promoted positive parenting, using a collaborative approach (for example: role play, modelling, discussion, etc). | |
| To evaluate the effectiveness of a parenting programme in reducing levels of parent irrationality, negative emotions, and to assess whether the change in irrationality is correlated with changes in emotionality. | Rational‐Emotive based Parent Education programme comprised nine weekly sessions Content focused on identifying and disputing parental irrational beliefs that lead to emotional stress; the reinforcement of rational beliefs; rational problem‐solving; teaching children rational personality traits.
| |
| To examine the efficacy of a parenting programme in reducing child conducts problems.
| Webster‐Stratton Incredible Years Basic parenting programme consisted of twelve to fourteen weekly sessions (2 hours each), focusing on positive disciplinary strategies, effective parenting skills, strategies coping with stress, and ways to strengthen children's social skills. Video vignettes for discussion, role play, rehearsals and home work assessments used. | |
| To evaluate the effects of a community group‐based parenting programme on vulnerable single mothers in improving maternal wellbeing (mood, self‐esteem and social support) and parenting. | Social support and education parenting programme consisted of 10 weekly group sessions (1.5 hours each). The program covered two thematic areas: i) child related area (for example: child development and behaviour, behaviour management, school involvement, child welfare agencies), and maternal area (for example: social isolation, stress and coping, personal care and development, relationships, grief). Cognitive behavioural techniques and structured counselling were provided. | |
| To examine the effectiveness of a coping skill training programme for parents of substance‐abusing adolescents
| Behavioural‐analytic parenting programme comprised eight weekly sessions (2 hours each). Aims were to teach participants more effective skills for coping with problems resulting from their adolescent's substance abuse. | |
| To examine the effectiveness of a parenting programme with at‐risk parents of young children. | Psycho‐educational programme STAR (Stop Think Ask Respond) comprised 10 weekly sessions (1.5 hours each), employing 'segments' in which parents learned thoughtful ways to respond to children, how to have realistic expectations of children, and how to implement positive parenting and discipline strategies. | |
| To examine the effect of a short‐term intervention to reduce self‐blame and guilt in parents of children with severe disabilities.
| Cognitive‐behavioural parenting programme comprised five weekly sessions (2 hours each). Content delivered using a lecture format. Homework assigned each week consisted of monitoring automatic thoughts, cognitive distortions, negative feelings, and attempts at cognitive restructuring. Sessions focused on the cognitive distortions that contribute to self‐blame and guilt in families of children with disabilities, and techniques to deal with such distortions. | |
|
| To assess effects of a parenting programme delivered by health visitors in primary care in improving mental health of children and parents | Webster Stratton parenting programme comprised 10 weekly sessions (2 hours each). The sessions included video vignettes of parent‐child interactions, group discussion, role play, rehearsal of parenting techniques, and home practice. |
| To evaluate the additional benefit of providing a problem‐solving parenting intervention in improving parental and child behaviour. | Problem‐solving skills parenting training comprised 6 units (1 hour each), focusing on aspects of problem‐solving including: problem definition, goal setting, alternative solutions, and decision‐making. This training was used as a supplement to a 10‐hour Parent and Children Series (PACS) programme based on the work of Webster‐Stratton. Topics included how to play with a child, use of praise, limit setting, use of time‐out. Video‐tape vignettes used to model skills and stimulate discussion. Written materials and homework assignments used. | |
| To evaluate the effectiveness of parent training in reducing parental psychosocial difficulties and conduct problems in children. | Parent and Children Series (PACS) treatment intervention consisted of 11‐14 weekly sessions (2 ¼ each), using manual, written materials and videos. | |
| To compare different treatment modes in reducing parental stress and improving child behaviour.
| GDVM: Group‐based video‐tape modelling parenting skills followed by discussion. IVM: Weekly in‐clinic sessions for approximately 1‐hour viewing of self‐administered videotape without therapist or discussion. GD: Weekly therapist‐led discussion sessions covering same topics as other groups. All modes of delivery comprised 10‐12 weekly sessions (2 hours each). Content, sequencing and number of sessions constant between groups. Topics covered play skills, praises, rewards, discipline and problem‐solving approaches | |
| Other or multimodal | ||
| To investigate the feasibility, implementation, and potential effects of a parenting programme on positive changes in parenting stress and child behaviour. | Success in Parenting Preschoolers (SIP) programme consisted of 8 weekly group sessions, each lasted 2 hours. The programme included both language facilitation techniques and behaviour management strategies. The parents viewed 100 instructional pages, watched four video vignettes, and received weekly session outlines, handouts, and home reminder magnets highlighting specific parenting skills presented during that weekly session. Additional weekly phone sessions were provided. All group sessions were videotaped. | |
| To evaluate the effectiveness of a community‐based intervention on enhancing pro‐social interaction and psychological wellbeing of urban, Head Start parents.
| The COPE (Community Outreach through Parent Empowerment) intervention has two components: (a) informal support groups, and (b) implementation of the Parent as Change Agent for Self module. Involved 10 group‐training sessions (each ˜3 hrs) focusing on the relationship between stress and social support. The 10 sessions had two main purposes: to identify major categories of stressful events for urban, African‐American Head Start parents, and to consider and discuss the ways in which friendships and various connections within the community can mitigate these stressors. | |
| To examine the effect of a parenting intervention on parental stress scores. | A brief cognitively‐based group parenting training is a 30‐minute single‐session, which targeted mothers perception of a preschool‐age child. The session focused on shifting parent perception of the child. Parents learned about the connection between thoughts, feelings and behaviours. Duration of the training was in total 1.5 hours with questionnaire completion. Sessions were audio‐taped. Attention‐placebo control group received information regarding [use of] developmentally appropriate books for preschool age children during 30 minutes. The session (1.5 hours) involved questionnaire completion. | |
| To examine the effects of a parenting programme on maternal sense of competency and stress | Active Parenting Programme was an educational programme and consisted of sessions (11/2 hours each). Content focused on understanding children's behaviour and misbehaviour, responsible parenting, effective communication and discipline, and developing responsibility in children. The training format used a variety of teaching techniques including lecture, videos, group discussion, and role‐play. | |
| Gutierrez 2007 (Adlerian) | To evaluate the efficacy of two parenting programmes in reducing perceived parental stress | Adlerian‐based parenting programme (APP) is the Systematic Training for Effective Parenting (STEP) program which included components on understanding yourself and your child, beliefs and feelings, encouraging your child and yourself, listening and talking to your child and problem solving. Each programme consists of eight 2 hour weekly sessions, delivered in Spanish. |
| To evaluate the effectiveness of a parenting programme in empowering parents to strengthen family resources. | Model based on a three‐tiered approach to developing personal coping and social support. Designed to strengthen interpersonal, intrapersonal and social resources by means of group work, discussion and didactic input. Topics included: family dynamics, loss and grief, communication and conflict resolution, networking and resource utilisation, stress management and relaxation skills. | |
| To assess the effectiveness of a parenting programme in reducing parenting stress, and in improving parental mood, family functioning, parenting style, locus of control, and perceived social support of children with ADHD. | Parent Stress Management (PSM) training program comprised nine weekly sessions (2 hour each). The program covered: Session 1: Orientation to the program and understanding stress; Session 2: Education about ADHD; Session 3: Rights and reasons; Session 4: Problem‐solving skills; Session 5: Cognitive restructuring; Session 6: Communication skills; Session 7: Self‐care skills; Session 8: Parenting skills; Session 9: Wrap‐up session. | |
| To evaluate the effects of a parenting programme in enhancing parent adaptive behaviour through emphasis on parental self‐reflection, social support and the emotional roots of children's misbehaviour and parenting stress. | Study 1 ‐ Counselling and social support parent programme. Listening to Children (LTC) parent training comprised eight weekly sessions (2.5 hours each) and was based on re‐evaluation counselling. It focused on the three core themes: recognising the effects of parents own childhood experience, spending special time with children, and understanding and handling children's emotions and upsets. Each session involved in‐class activities, reading assignments, and homework projects built around those themes. |
i) Behavioural parenting programmes
Twenty‐two studies evaluated the effectiveness of a behavioural parenting programme (Sirbu 1978; Wolfson 1992; Pisterman 1992a; Pisterman 1992b; Blakemore 1993; Cunningham 1995; Odom 1996; Irvine 1999; DeGarmo 2004; Wang 2005; Gutierrez 2007; van den Hoofdakker 2007; Hiscock 2008; Niccols 2009; Hanisch 2010; Martin 2003; Gallart 2005; Matsumoto 2007; Turner 2007; Morawska 2009; Joachim 2010; Matsumoto 2010). This category included programmes which are primarily behavioural in orientation and that are based on social learning principles. These programmes teach parents how to use a range of basic behavioural strategies for managing children’s behaviour. Triple‐P programmes are included in this category.
ii) Cognitive‐behavioural parenting programmes
Nineteen studies evaluated the effectiveness of a cognitive‐behavioural parenting programme (Webster Stratton 1988; Gammon 1991; Spaccerelli 1992; Blakemore 1993; Nixon 1993; Gross 1995; Joyce 1995; Greaves 1997; Taylor 1998; McGillicuddy 2001; Nicholson 2002; Patterson 2002; Gross 2003; Lipman 2005; Chronis 2006; Gardner 2006; Hutchings 2007; Gross 2009; Larsson 2009). These programmes combined the basic behavioural type strategies with cognitive strategies aimed at helping parents to identify and change distorted patterns of belief or thought that may be influencing their behaviour. Webster‐Stratton Incredible Years programmes were included in this category.
iii) Other and multimodal
It was not possible to classify the interventions from eight studies (Schultz 1993; Wolfe 2003; Farrar 2005; Feliciana 2005; Treacy 2005; Fanning 2007; Fantuzzo 2007; Gutierrez 2007) based on the information provided. See Table 1 for further information about these programmes.
Duration of the intervention
We have described the duration of the intervention as 'standard' in 36 studies (8 to 14 sessions), 'brief' in 10 studies (1 to 6 sessions) and 'long' in two studies (16 weeks or more).
Outcomes
All outcomes were parent‐report and involved the use of a variety of standardised instruments. We assessed outcomes at three time points: immediately post‐intervention (up to one month following the delivery of the intervention), short‐term follow‐up (two to six months post‐intervention) and long‐term follow‐up (more than six months post‐intervention).
Primary outcome measures
Depressive symptoms
Twenty‐nine studies assessed the impact of a parent training programme on parental depressive symptoms. Nine studies used the Beck Depression Inventory (Nixon 1993; Cunningham 1995; Taylor 1998; Irvine 1999; McGillicuddy 2001; Treacy 2005; Chronis 2006; Gardner 2006; Hutchings 2007); nine studies used the Depression Anxiety Stress Scale (Martin 2003; Gallart 2005; Matsumoto 2007; Turner 2007; Hiscock 2008; Morawska 2009; Hanisch 2010; Joachim 2010; Matsumoto 2010); six studies used the Center for Epidemiological Studies Depression scale (Gross 1995; Gross 2003; DeGarmo 2004; Lipman 2005; Gross 2009; Niccols 2009); three studies used the Parent Stress Index (Pisterman 1992a; Greaves 1997; Feliciana 2005); Patterson 2002 used the General Health Questionnaire; and Bradley 2003 used the Irritability Depression Anxiety Scale.
Anxiety symptoms
Thirteen studies measured parental anxiety. Most studies (n = 8) used the Depression Anxiety Stress Scale (Martin 2003; Gallart 2005; Matsumoto 2007; Hiscock 2008; Morawska 2009; Hanisch 2010; Joachim 2010; Matsumoto 2010); one study used the State‐Trait Anxiety Inventory (Joyce 1995); one study (McGillicuddy 2001) used the Brief Symptom Inventory; one (Patterson 2002) used the General Health Questionnaire; and one (Chronis 2006) used the Beck Anxiety Inventory.
Stress
Almost three‐quarters (n = 36) of included studies assessed parental stress using nine scales. Seventeen studies used the Parenting Stress Index (Webster Stratton 1988; Spaccerelli 1992; Pisterman 1992a; Pisterman 1992b; Blakemore 1993; Gross 1995; Greaves 1997; Nicholson 2002; Patterson 2002; Wolfe 2003; Feliciana 2005; Treacy 2005; Wang 2005; Gutierrez 2007; Hutchings 2007; van den Hoofdakker 2007; Larsson 2009); nine studies used the Depression Anxiety Stress Scale (Martin 2003; Gallart 2005; Matsumoto 2007; Turner 2007; Hiscock 2008; Morawska 2009; Hanisch 2010; Joachim 2010; Matsumoto 2010); two studies used the Every Day Stress Index (Gross 2003; Gross 2009); two studies used the modified Uplifts and Hassles Scale (Wolfson 1992; Fantuzzo 2007); and six studies (Sirbu 1978; Gammon 1991; Bradley 2003; Farrar 2005; Chronis 2006; Fanning 2007) used the Brief Symptom Inventory, Perceived Stress Scale, Parental Stress Scale, Confidence Rating Questionnaire, Profile of Mood State and Stress Satisfaction Questionnaire, respectively.
Self‐esteem
Three studies (Patterson 2002; Lipman 2005; Chronis 2006) assessed parental self‐esteem using the Rosenberg Self‐Esteem Scale (Rosenberg 1965).
Anger
Three studies assessed parental anger using the Berger Feeling Scale (Joyce 1995; Greaves 1997) and the State‐Trait Anger Inventory (McGillicuddy 2001).
Aggression
None of the included studies assessed aggression.
Guilt
Three studies measured guilt using the Berger Feeling Scale (Joyce 1995; Greaves 1997) and Situational Guilt Scale (Nixon 1993).
Secondary outcome measures
Confidence
One‐third (n = 16) of included studies assessed parental confidence and used seven scales or subscales to measure this outcome. Four studies used the Parenting Sense of Competence Scale (Cunningham 1995; Odom 1996; Feliciana 2005; Gardner 2006); four studies used the Problem Setting and Behaviour Checklist (Martin 2003; Matsumoto 2007; Morawska 2009; Matsumoto 2010); three studies used the Toddler Care Questionnaire (Gross 1995; Gross 2003; Gross 2009); two studies used the Parent Stress Index (Pisterman 1992a; Pisterman 1992b); and three studies (Wolfson 1992; Farrar 2005; Joachim 2010) used the Kansas Parent satisfaction Scale, Parenting Task Checklist and Parental Efficacy measures, respectively.
Partner satisfaction
Eight included studies reported partner satisfaction and used five scales to measure this. Three studies (Matsumoto 2007; Morawska 2009; Matsumoto 2010) used the Relationship Quality Index; two studies (Taylor 1998; Chronis 2006) used the Dyadic Adjustment Scale; one study (Pisterman 1992a) used the Parenting Stress Index; one study (Schultz 1993) used the Marital Adjustment Inventory; and one study used the Locke‐Wallace Marital Adjustment Scale (Treacy 2005).
Adverse effects
None of the included studies set out to report any adverse effects and none reported any adverse effects.
Excluded studies
In this updated review, 121 studies (85 new and 36 from the earlier review) did not meet all the inclusion criteria. We excluded studies from the review if random allocation was not used (n = 14), if participants or the control group did not meet the inclusion criteria (n = 28), if the intervention was not group‐based (n = 34), if the study did not focus on parental psychosocial health (n = 54), if the study involved direct work with children (n = 9) or was a summary of another study (n = 5), and if standardised outcome measures were not used (3). We excluded 23 studies because of more than one reason mentioned above. Six excluded studies were listed as included studies in a previous version of the review but are now excluded (Van Wyk 1983; Scott 1987; Anastopoulos 1993; Mullin 1994; Sheeber 1994; Zimmerman 1996). We excluded Anastopoulos 1993, Scott 1987, Sheeber 1994 and Mullin 1994 on the basis that they did not meet the definition of a randomised or quasi‐randomised trial (Higgins 2008). Anastopoulos 1993 and Mullin 1994 were described as 'quasi‐experimental', but on inspection they were pre and post‐test studies and no attempt was made to randomly assign the participants to groups. Scott 1987 allocated by group alternation. Sheeber 1994 was a partially randomised trial. We excluded Van Wyk 1983, which reported changes in personality outcomes only, because it did not focus on parental mental health or parenting. Zimmerman 1996 did not focus on parental psychosocial health; the study investigated the influence of parenting skills strategies on family functioning. We have given the reasons for the exclusion of the 121 excluded studies in the Characteristics of excluded studies table.
Risk of bias in included studies
The 'Risk of bias' table provides a summary of our assessment of the risk of bias for the 48 included studies (see Characteristics of included studies and Figure 1). Each risk of bias table provides a decision about the adequacy of the study in relation to the criterion, summarised as 'low risk of bias'; 'high risk of bias' and 'unclear risk of bias’ (Higgins 2008). We attempted to contact the investigators where insufficient information was provided and we succeeded in obtaining further information for 22 studies.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study
Allocation
The method of sequence generation was adequate in 24 studies: 18 studies used allocation based on random numbers that were computer‐generated or derived from a table (Cunningham 1995; Gross 1995; Irvine 1999; McGillicuddy 2001; Nicholson 2002; Gross 2003; DeGarmo 2004; Farrar 2005; Lipman 2005; Gardner 2006; Hutchings 2007; Turner 2007; van den Hoofdakker 2007; Hiscock 2008; Gross 2009; Morawska 2009; Niccols 2009; Joachim 2010); four studies used allocation by drawing lots from a hat (Webster Stratton 1988; Odom 1996; Gallart 2005; Hanisch 2010); two studies allocated participants by throwing a dice or coin flipping (Patterson 2002; Wang 2005). We classified adequacy of sequence generation as ‘unclear’ in the 24 remaining studies.
We assessed that allocation was adequately concealed in 14 studies (Webster Stratton 1988; Cunningham 1995; Gross 1995; Odom 1996; Irvine 1999; McGillicuddy 2001; Patterson 2002; Farrar 2005; Lipman 2005; Gardner 2006; Turner 2007; van den Hoofdakker 2007; Hiscock 2008; Niccols 2009). Six studies (Nicholson 2002; Gross 2003; Gallart 2005; Wang 2005; Gross 2009; Morawska 2009) reported that allocation was not adequately concealed. We classified adequacy of allocation sequence as ‘unclear’ in the 28 remaining studies.
Blinding
We judged that it would not be possible to fully blind participants in studies of the type included in this review. We found no indication of any specific additional measures taken to reduce the risk of bias in the majority of included studies (n = 45). Farrar 2005 reported that one assessor was assigned to each group in order to ensure that participants did not have contact with members of the other group. Gallart 2005 reported that participants were kept blind to the fact that there were two different formats of the programme. Sirbu 1978 attempted to ensure that participants were unaware of the type of intervention they were receiving. However, review authors judged that those specific measures were not sufficient to reduce the risk of bias.
Trial investigators reported that outcome assessors were blind to the allocation status of participants in 15 studies (Blakemore 1993; Cunningham 1995; Gross 1995; Odom 1996; Webster Stratton 1988; Irvine 1999; McGillicuddy 2001; Patterson 2002; DeGarmo 2004; Gardner 2006; Fanning 2007; Fantuzzo 2007; Turner 2007; Hiscock 2008; Niccols 2009). In eight studies, outcome assessors were either not blinded or blinding was compromised during the trial (Taylor 1998; Farrar 2005; Gallart 2005; Lipman 2005; Wang 2005; Matsumoto 2007; Morawska 2009; Hanisch 2010). We classified the blinding of outcome assessors as ‘unclear’ in the remaining 25 studies.
Incomplete outcome data
We judged that most of the studies (n = 32) adequately addressed incomplete outcome data; eight of those studies (Blakemore 1993; Greaves 1997; McGillicuddy 2001; Nicholson 2002; Wolfe 2003; Feliciana 2005; Fantuzzo 2007; Matsumoto 2007) reported that none of the participants dropped out and the study data were collected on all participants at each data collection point; four studies (Gross 1995; Gross 2003; Martin 2003; Larsson 2009) did not adequately address incomplete outcome data; the remaining 12 studies were classified as ‘unclear’.
Selective reporting
Most studies (n = 44) appeared to have included all expected outcomes and were free of selective reporting. Four studies were not free of selective reporting: Bradley 2003 did not report endpoint and follow‐up data for depressive symptoms from the BSI subscale; Gross 2009 stated that three outcomes (depressive symptoms, stress and confidence) were not included in the paper because of length and their lack of association with the outcome variables; Turner 2007 did not report scores for the anxiety scale of the DASS; Wolfe 2003 did not report endpoint and follow‐up data for the parent‐child dysfunctional interaction subscale of the PSI.
Other potential sources of bias
While the use of randomisation should in theory ensure that any possible confounders are equally distributed between the arms of the trial, the randomisation of small numbers of respondents may result in an unequal distribution of confounding factors. It is therefore important that the distribution of known potential confounders is: (i) compared between the different study groups at the outset, or (ii) adjusted for at the analysis stage.
Spaccerelli 1992 used two newly developed measures, which also raised the possibility of bias. Hutchings 2007 reported a competing interest as both author and provider of occasional parent training courses. The remaining 46 studies appeared to be free of other bias.
Effects of interventions
In the text below, an I2 value for heterogeneity was only reported if it exceeded 50% or if the P value from the Chi2 test was < 0.05. Numbers given are the total number of participants randomised. Where it has been possible to calculate an effect size, we have reported these with 95% confidence intervals (CI). Where we calculated and reported effect sizes, a minus sign indicates that the results favour the intervention group. Where the calculated effect size is statistically significant (P < 0.05), we state whether the result favours the intervention or control condition.
In terms of effect sizes, values > 0.70 have been treated as large; those between 0.40 and 0.70 as moderate; values < 0.40 and > 0.10 have been treated as small; and values < 0.10 have been treated as no evidence of effectiveness (Higgins 2008, Section 12.6.2).
We have summarised the results below under headings corresponding to the seven primary and the three secondary outcomes outlined in the section entitled Types of outcome measures. For each outcome, we have presented the results according to the timing of the outcome assessment. Three categories of outcome assessment were used: post‐intervention (up to four weeks after the end of the intervention), short‐term follow‐up (two to six months post‐intervention), and long‐term follow‐up (more than six months post‐intervention). Under each heading, results of subgroup analyses (to compare types of intervention) are included where these were conducted. For clarity, results of two further subgroup analyses (impact of paternal‐only outcomes; impact of duration of intervention) are summarised in a separate section.
Primary outcomes
Depressive symptoms
Post‐intervention
Meta‐analysis of data from 22 studies revealed a statistically significant difference between intervention and control conditions, favouring the intervention (SMD ‐0.17, CI ‐0.28 to ‐0.07, P = 0.001, n = 1591, I2 = 7%, Analysis 1.1.1). This result was broadly consistent with the meta‐analysis of 11 studies reported in the previous version of this review (SMD ‐0.26) (Barlow 2003).
Short‐term follow‐up
Meta‐analysis of data from 13 studies indicated no statistically significant difference between intervention and control conditions at short‐term follow‐up (Analysis 1.1.2). In the previous version of this review, meta‐analysis of six studies similarly failed to achieve statistical significance (95% CI ‐0.40 to 0.002) (Barlow 2003).
Long‐term follow‐up
Meta‐analysis of data from seven studies revealed no statistically significant difference between intervention and control conditions at long‐term follow‐up (Analysis 1.1.3).
Anxiety symptoms
Post‐intervention
Meta‐analysis of data from nine studies revealed a statistically significant difference between intervention and control conditions favouring the intervention (SMD ‐0.22, CI ‐0.43 to ‐0.01, P = 0.04, n = 464, I2 = 22%, Analysis 1.2.1). The previous version of this review did not report an analysis for anxiety symptoms alone, although a statistically significant effect favouring the intervention was identified for the combined outcome of anxiety and stress (SMD ‐0.4, 95% CI ‐0.6 to ‐0.2) (Barlow 2003).
Short‐term follow‐up
Meta‐analysis of data from three studies indicated no statistically significant difference between intervention and control conditions at short‐term follow‐up (Analysis 1.2.2).
Long‐term follow‐up
Meta‐analysis of data from two studies at long‐term follow‐up indicated no statistically significant difference between intervention and control conditions (Analysis 1.2.3).
Stress
Post‐intervention
Meta‐analysis of data from 25 studies, which included data from both arms (behavioural versus wait‐list control, Adlerian parent training versus attention placebo control) and both control conditions for Gutierrez 2007, revealed a statistically significant difference between intervention and control conditions favouring the intervention (SMD ‐0.29, 95% CI ‐0.42 to ‐0.15, P < 0.0001, n = 1567, Analysis 1.3.1) but with evidence of significant heterogeneity (I2 = 35%; P = 0.04). The previous version of this review did not report an analysis for stress symptoms alone, although a statistically significant effect was found for the combined outcome of anxiety and stress, again favouring the intervention (SMD ‐0.4, 95% CI ‐0.6 to ‐0.2, 10 studies).
Short‐term follow‐up
Meta‐analysis of data from 12 studies again indicated a statistically significant difference between intervention and control conditions favouring the intervention (SMD ‐0.22, 95% CI ‐0.42 to ‐0.01, P = 0.04, n = 1680, Analysis 1.3.2) but with evidence of statistically significant heterogeneity (I2 = 69%; P < 0.0001). One possible reason for the large I2 value is that the impact of parent training on stress scores varied with the modality of the intervention (see below).
Long‐term follow‐up
Meta‐analysis of data from four studies at long‐term follow‐up indicated no statistically significant difference between intervention and control conditions (Analysis 1.3.3).
Self‐esteem
Post‐intervention
Meta‐analysis of data from two studies at post‐intervention indicated no statistically significant difference between intervention and control conditions (Analysis 1.4.1).
Short‐term follow‐up
Meta‐analysis of data from two studies at short‐term follow‐up indicated no statistically significant difference between intervention and control conditions (Analysis 1.4.2).
Long‐term follow‐up
Meta‐analysis of data from two studies at long‐term follow‐up indicated no statistically significant difference between intervention and control conditions (Analysis 1.4.3).
Anger
Post‐intervention
Meta‐analysis of data from three studies revealed a statistically significant difference between intervention and control conditions favouring the intervention (SMD ‐0.60, 95% CI ‐1.00 to ‐0.20, P = 0.004, n = 107, I2 = 0%, Analysis 1.5.1).
Short‐ and long‐term follow‐up
Anger was not reported in any study at short‐ or long‐term follow‐up.
Aggression
No study reported aggression.
Guilt
Post‐intervention
Meta‐analysis of data from three studies showed a statistically significant difference between intervention and control conditions favouring the intervention (SMD ‐0.79, 95% CI ‐1.18 to ‐0.41, P < 0.0001, n = 119, I2 = 0%, Analysis 1.6.1).
Short‐ and long‐term follow‐up
No study reported guilt at short‐ or long‐term follow‐up.
Secondary outcomes
Confidence
Post‐intervention
Meta‐analysis of data from 14 studies revealed a statistically significant difference between intervention and control conditions favouring the intervention (SMD ‐0.34, 95% CI ‐0.51 to ‐0.17, P < 0.0001, n = 1001, I2 = 36%, Analysis 1.7.1).
Short‐term follow‐up
Meta‐analysis of data from seven studies revealed a statistically significant difference between intervention and control conditions favouring the intervention (SMD ‐0.32, 95% CI ‐0.63 to ‐0.01, P = 0.04, n = 636, Analysis 1.7.2) but with evidence of significant heterogeneity (I2 = 68%; P = 0.005).
Long‐term follow‐up
Meta‐analysis of data from two studies at long‐term follow‐up indicated no statistically significant difference between intervention and control conditions (Analysis 1.7.3).
Partner satisfaction
Post‐intervention
Meta‐analysis of data from nine studies revealed a moderate, statistically significant difference between intervention and control conditions favouring the intervention (SMD ‐0.28, 95% CI ‐0.47 to ‐0.09, P = 0.005, n = 432, I2 = 0%, Analysis 1.8.1). This was consistent with the meta‐analysis of four studies reported in the previous version of this review (Barlow 2003), which produced an SMD of ‐0.4.
Short‐term follow‐up
At short‐term follow up, results of analysis of data from a single study indicated no statistically significant difference between intervention and control conditions (Analysis 1.8.2).
Long‐term follow‐up
No study reported partner satisfaction at short‐ or long‐term follow‐up.
Adverse effects
No study reported adverse effects.
Paternal outcome measures
Only four studies reported outcome data from fathers separately. These data were available for four outcomes (depressive symptoms, stress, confidence, and partner satisfaction) but with meta‐analysis possible for the outcome of stress only. Meta‐analysis of data from four studies for paternal stress at post‐intervention revealed a statistically significant difference between intervention and control conditions favouring the intervention (SMD ‐0.43, 95% CI ‐0.79 to ‐0.06, P = 0.02, n = 123, I2 = 0%, Analysis 2.42.1). This effect size is larger than the overall figure (for mothers and for both parental figures) obtained in Analysis 1.3.1 (SMD ‐0.29). Examining data from individual studies revealed no statistically significant effect from paternal‐only data for depressive symptoms, confidence or partner satisfaction (Analysis 2.40.1; Analysis 2.41.1; Analysis 2.43.1; Analysis 2.44.1).
Discussion
Summary of main results
This updated review includes a total of 48 studies. Eight meta‐analyses were conducted evaluating the immediate post‐intervention impact and four evaluating the short‐term (six months) and long‐term (one year or more) impact of behavioural (n = 22), cognitive‐behavioural (n = 19) and non‐classifiable or multimodal (n = 8) parenting programmes on a range of aspects of parental psychosocial wellbeing. The results indicate that parenting programmes were effective immediately post‐intervention in producing statistically significant improvements in a number of aspects of parental psychosocial functioning including depression (SMD ‐0.17, 95% CI ‐0.28 to ‐0.07); anxiety (SMD ‐0.22, 95% CI ‐0.43 to ‐0.01); stress (SMD ‐0.29, 95% CI ‐0.42 to ‐0.15); anger (SMD ‐0.60, 95% CI ‐1.00 to ‐0.20); guilt (SMD ‐0.79, 95% CI ‐1.18 to ‐0.41); confidence (SMD ‐0.34, 95% CI ‐0.51 to ‐0.17), and satisfaction with the partner relationship (SMD ‐0.28, 95% CI ‐0.47 to ‐0.09). There was, however, evidence of significant statistical heterogeneity for the meta‐analyses of stress outcomes post‐intervention and for parental confidence at short‐term follow‐up.
Although the results suggest that stress (SMD ‐0.22, 95% CI ‐0.42 to ‐0.01) and confidence (SMD ‐0.32, 95% CI ‐0.63 to ‐0.01) continued to be statistically significant at six month follow‐up, none of the outcomes measured remained statistically significant at one year. This finding strongly points to the need for parents to receive 'top ups' or post‐intervention support to help them to maintain the short‐term benefits.
There were only sufficient data from fathers to conduct one meta‐analysis. This showed a statistically significant short‐term improvement in paternal stress (SMD ‐0.43, 95% CI ‐0.79 to ‐0.06). The deleterious consequences of compromised paternal psychosocial functioning has now been clearly recognised (for example, Kane 2004; Ramchandani 2008), and the need to support fathers has been highlighted at policy level (Department of Health 2009). This finding points to the need for further research focusing explicitly on the impact of such programmes on the psychosocial functioning of fathers.
Overall completeness and applicability of evidence
These data provide a comprehensive picture about the impact of the key types of parenting programme (for example, behavioural and cognitive‐behavioural) on parental psychosocial functioning.
The studies were conducted in a wide range of settings and countries including the USA, Australia, Canada, UK, China, Germany, Japan, the Netherlands and New Zealand.
Only a small number of studies examined the effectiveness of parenting programmes in terms of the psychosocial functioning of fathers, and this is a serious omission given that fathers now play a significant role in childcare, and research suggests that their psychosocial functioning is key to the wellbeing of children (see Background).
Quality of the evidence
The overall quality of the included studies is summarised in Figure 1. Many studies were unclear about important quality criteria, including allocation concealment, sequence generation and blinding. We examined the included studies for evidence of other potential biases, including that of conflict of interest, which was implicated in one study only (Hutchings 2007) where the study author also delivered the intervention. A number of the included studies (in particular the Webster‐Stratton and Triple‐P programmes) involved the programme developer in the evaluation.
Potential biases in the review process
In the original review we estimated the standardised mean difference by calculating the treatment effect for each outcome in each study by dividing the mean difference in post‐intervention scores for the intervention and treatment groups by the pooled standard deviation. To promote consistency we have continued with this method. It should be noted, however, that random allocation does not guarantee equality of means between groups at pre‐test, and also that post‐test standard deviation (SD) may be inflated by a differential response to intervention, and may underestimate the effect size attributable to the intervention.
Agreements and disagreements with other studies or reviews
These findings are consistent with the earlier review (Barlow 2003) of the effectiveness of parent training programmes in improving the psychosocial wellbeing of parents. However, the significant addition of new studies has enabled us to reach a number of new conclusions in terms of the evidence about effectiveness being limited to standard (10 to 12 week) parent training programmes and in the short term only. This is largely consistent with the findings of reviews that examine the impact of parenting programmes on children's behaviour, which is again mostly limited to evidence of short‐term benefits (Dretze 2005; Barlow 2011).

Risk of bias summary: review authors' judgements about each risk of bias item for each included study

Comparison 1 Meta analysis: any parent training programme versus control (parental outcomes), Outcome 1 Depressive symptoms.

Comparison 1 Meta analysis: any parent training programme versus control (parental outcomes), Outcome 2 Anxiety symptoms.

Comparison 1 Meta analysis: any parent training programme versus control (parental outcomes), Outcome 3 Stress.
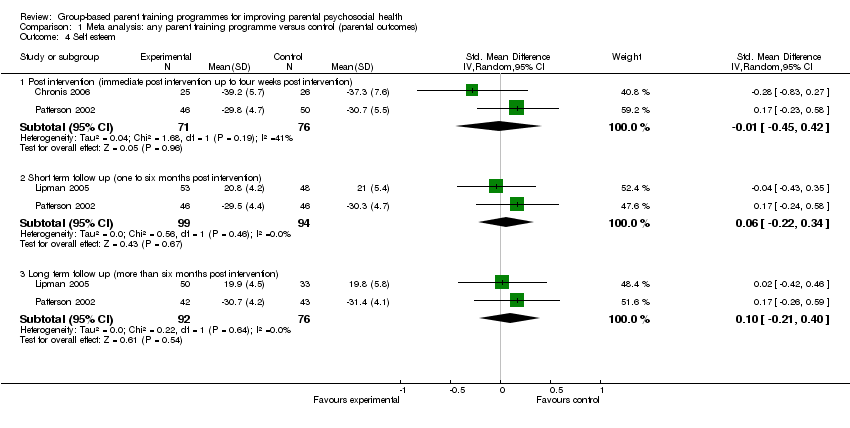
Comparison 1 Meta analysis: any parent training programme versus control (parental outcomes), Outcome 4 Self esteem.
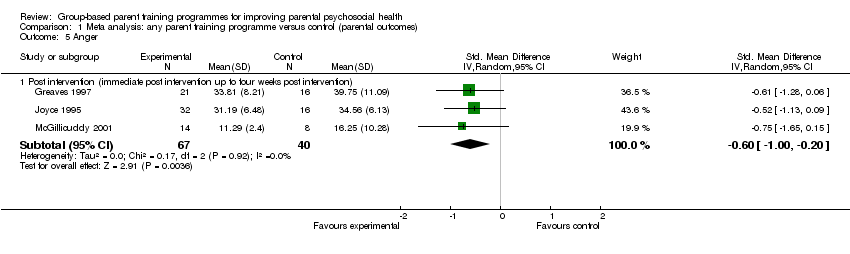
Comparison 1 Meta analysis: any parent training programme versus control (parental outcomes), Outcome 5 Anger.

Comparison 1 Meta analysis: any parent training programme versus control (parental outcomes), Outcome 6 Guilt.

Comparison 1 Meta analysis: any parent training programme versus control (parental outcomes), Outcome 7 Confidence.

Comparison 1 Meta analysis: any parent training programme versus control (parental outcomes), Outcome 8 Partner satisfaction.

Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 1 Parental outcomes: depressive symptoms (Beck Depression Inventory).
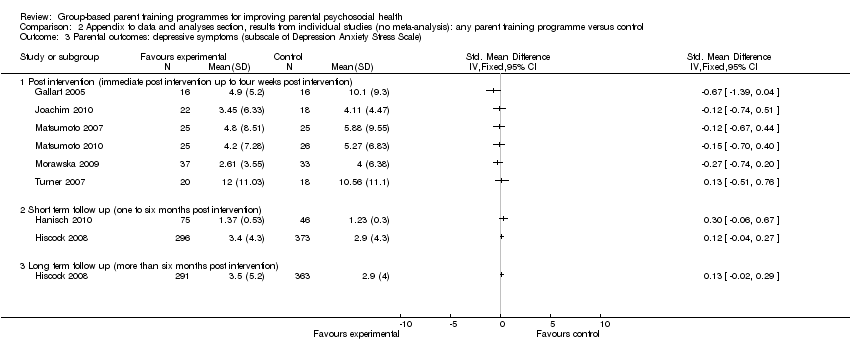
Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 3 Parental outcomes: depressive symptoms (subscale of Depression Anxiety Stress Scale).

Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 4 Parental outcomes: depressive symptoms (Centre for Epidem. Studies Depression Scale).

Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 5 Parental outcomes: depressive symptoms (subscale of Parenting Stress Index).
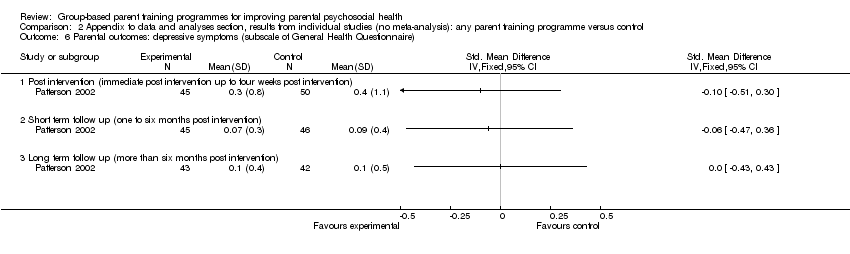
Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 6 Parental outcomes: depressive symptoms (subscale of General Health Questionnaire).
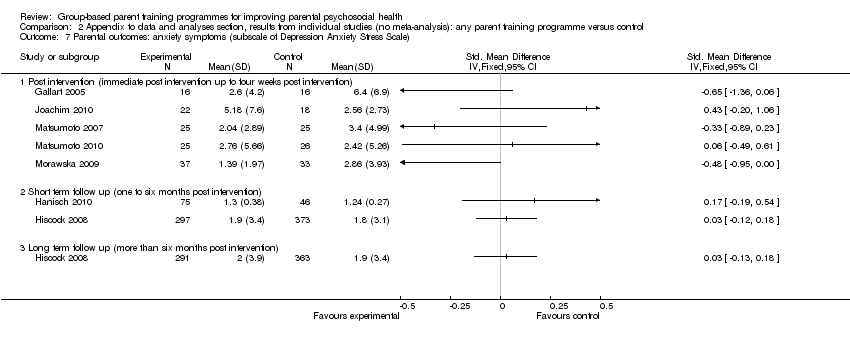
Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 7 Parental outcomes: anxiety symptoms (subscale of Depression Anxiety Stress Scale).

Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 9 Parental outcomes: anxiety symptoms (subscale of General Health Questionnaire).
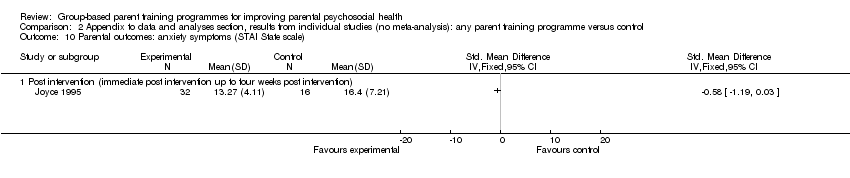
Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 10 Parental outcomes: anxiety symptoms (STAI State scale).
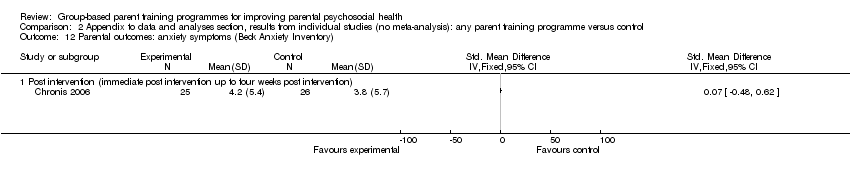
Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 12 Parental outcomes: anxiety symptoms (Beck Anxiety Inventory).

Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 13 Parental outcomes: anxiety symptoms (Brief Symptom Inventory).

Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 14 Parental outcomes: stress (Perceived Stress Scale).

Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 15 Parental outcomes: stress (Parenting Stress Index: overall score).

Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 16 Parental outcomes: stress (Parenting Stress Index: parent domain score).

Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 17 Parental outcomes: stress (Parenting Stress Index ‐ short form: overall score).

Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 18 Parental outcomes: stress (Parenting Stress Index ‐ short form: distress subscale).

Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 19 Parental outcomes: stress (Everyday Stress Index).

Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 20 Parental outcomes: stress (Ability & Confidence Rating Questionnaire).

Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 21 Parental outcomes: stress (Parental Stress Scale).
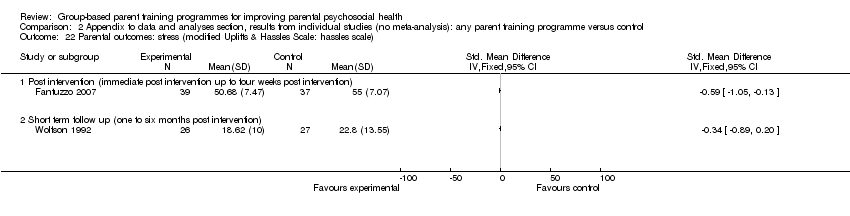
Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 22 Parental outcomes: stress (modified Uplifts & Hassles Scale: hassles scale).
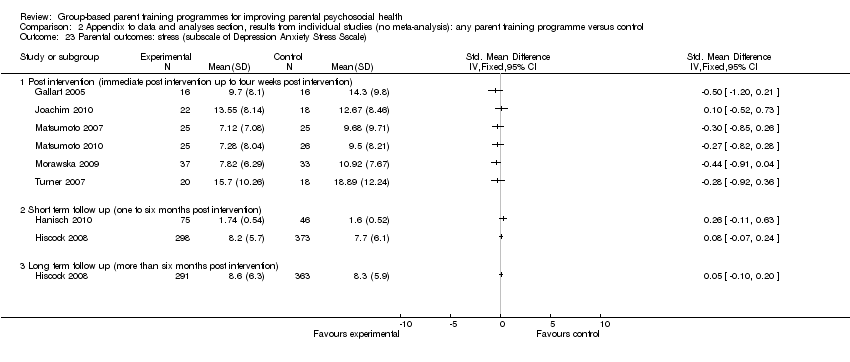
Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 23 Parental outcomes: stress (subscale of Depression Anxiety Stress Sscale).
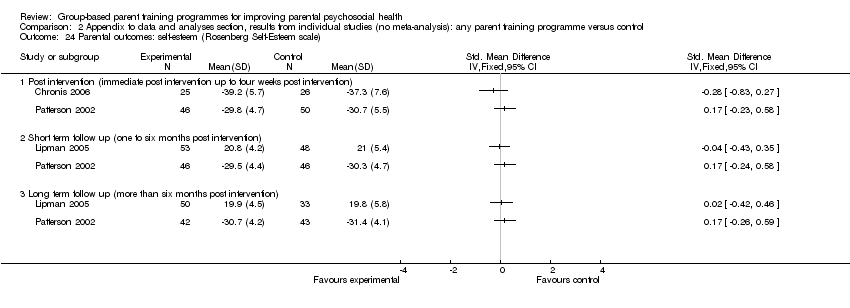
Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 24 Parental outcomes: self‐esteem (Rosenberg Self‐Esteem scale).

Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 25 Parental outcomes: anger (subscale of Berger's Feeling Scale).

Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 26 Parental outcomes: anger (State‐Trait Anger Expression Inventory scale).

Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 27 Parental outcomes: guilt (subscale of Berger's Feeling Scale).

Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 28 Parental outcomes: guilt (Situation Guilt Scale).
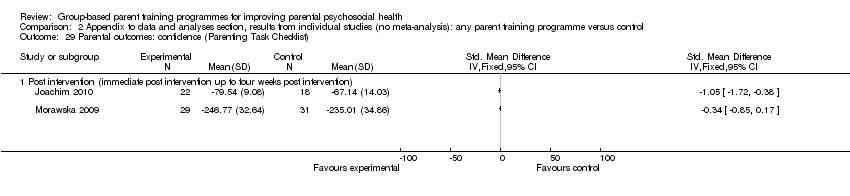
Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 29 Parental outcomes: confidence (Parenting Task Checklist).

Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 30 Parental outcomes: confidence (Parental Efficacy measure).

Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 31 Parental outcomes: confidence (Parenting Stress Index).
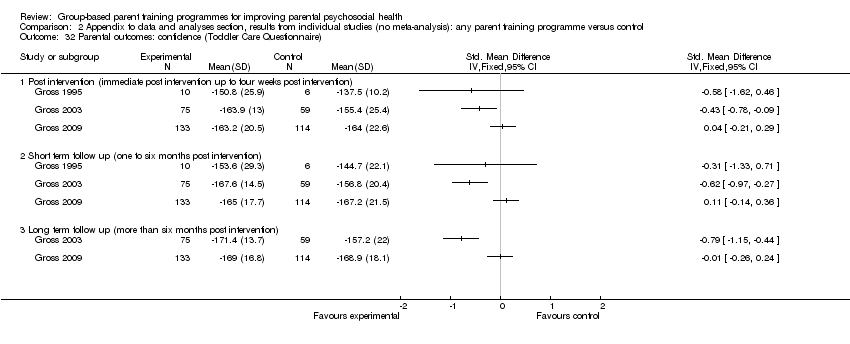
Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 32 Parental outcomes: confidence (Toddler Care Questionnaire).

Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 33 Parental outcomes: confidence (Parenting Sense of Competence Scale: total score).

Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 34 Parental outcomes: confidence (Problem Setting & Behaviour Checklist).

Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 35 Parental outcomes: confidence (Kansas Parental Satisfaction Scale: satisfaction in parental role).

Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 36 Parental outcomes: partner satisfaction (Dyadic Adjustment Scale).

Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 37 Parental outcomes: partner satisfaction (Locke‐Wallace Marital Adjustment Test).

Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 38 Parental outcomes: partner satisfaction (Parenting Stress Index).

Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 39 Parental outcomes: partner satisfaction (Relation Quality Index).

Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 40 Father outcomes: depressive symptoms (Beck Depression Inventory).

Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 41 Father outcomes: depressive symptoms (Center for Epidemiological Studies Depression Scale.

Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 42 Father outcomes: stress (Parenting Stress Index: parent domain subscale).

Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 43 Father outcomes: confidence (Toddler Care Questionnaire: overall scores).
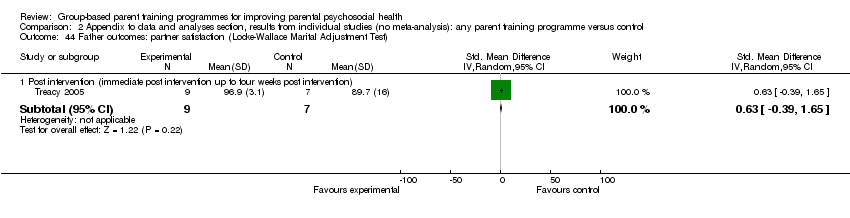
Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 44 Father outcomes: partner satisfaction (Locke‐Wallace Marital Adjustment Test).
| Study ID | Aim | Content/delivery |
| Behavioural only | ||
| To evaluate the effects of a brief parenting programme on positive and negative parenting behaviours. | Brief behavioural parenting program consisted of three weekly 2‐hour group meetings with booster session 4 weeks after the third session. The intervention included video material (1‐2‐3 Magic) on managing difficult child behaviours, handouts and mutual support/problem solving work. | |
| To examine the efficacy of a large group‐based parenting programme as a means of increasing the accessibility of such programmes to parents of children with disruptive behaviour; to determine whether parenting programme improve parental sense of competence and decrease depressive symptoms. | Coping modelling problem‐solving parenting programme comprised 11‐12 weekly sessions, involving the formulation of solutions through the observation of videotapes, discussion, modelling and role play. Homework reviewed each week. | |
| To evaluate changes in parent management and subsequently changes in child behaviour and maternal affects over time. | Parent Management Training (PMT) was a series of parent group meetings and discussion (14 weekly sessions). Interventionists made midweek telephone calls to encourage the participation. The program included a 30‐minute video, and covered 5 theoretically based effective parenting practices (appropriate discipline, skill encouragement, monitoring, problem solving, and positive reinforcement). Individual catch‐up sessions offered to replace missed sessions; 10% participants had at least one individual session. | |
|
| To evaluate the effectiveness of a parenting programme and assess the impact of telephone contact sessions in developing positive relationships, in encouraging desirable behaviour, in teaching new skills and behaviours, and in managing misbehaviour. | The full Group Triple‐P program comprised four weekly 2‐hour group sessions and four weekly follow‐up telephone calls. The programmes standard Facilitators Kit (leaders manual, AV materials, participants workbook) was used, plus a video (Every Parents Survival Guide). The modified Group Triple‐P program is the standard programme delivered as four weekly 2‐hour group sessions but without the four follow‐up telephone contacts. |
| Gutierrez 2007 (behavioural) | To evaluate the efficacy of two parenting programmes in reducing perceived parental stress | Behaviourally‐based parenting programme (BPP)1‐2‐3 Magic Parenting Program included components on parents reactions to their child's misbehaviour, using time‐out, dealing with testing and manipulation, positive reinforcement, and preventing relapses. see below for description of Adlerian parenting program. Compared two active parenting interventions with an attention placebo program and a wait‐list control group. Each programme consists of eight 2‐hours‐weekly sessions, delivered in Spanish. |
| To evaluate the effects of a parenting programme on child behaviour, parenting practices, parent‐child interaction, and parent quality of life | Prevention Programme for Externalising Problem behaviour (PEP) consisted of ten weekly sessions (80‐120 minutes each).
The first three sessions focused on defining individual problem situations, introducing unspecific basic strategies. The next three sessions thought participants the classical key strategies of behaviour modification. Sessions 7 to 10 consolidated these strategies by working on common difficult parenting situations. Individual homework assessments and telephone supervision were provided. | |
| To assess the effectiveness of a parenting programme in preventing early childhood behavioural problems
| The Universal parenting programme comprised of three structured sessions, covering normal development and behaviour, strategies to increase desired behaviour, and strategies to reduce unwanted behaviour. First session (child at 8 months) consisted of handouts; second and third sessions (child at 12 and 15 months) were 2‐hour group sessions. Training incorporated didactic teaching, written information, role play and video vignettes of appropriate parenting responses to childhood behaviours. | |
| To assess the effectiveness of a brief parent training in preventing behaviour problems on shopping trips.
| Brief, two‐hour, topic‐specific parent discussion group based on the Triple P‐Positive Parenting Program. Intervention entitled Hassle‐free Shopping was for parents looking for specific advice on how to manage their child's behaviour in the supermarket and how to prevent behaviour problems on shopping trips. | |
| To evaluate the effectiveness of a parenting programme provided by non‐mental health providers who are more likely to be available in small communities.
| Adolescent Transition Program was a stepwise, skill‐based curriculum designed to teach parenting skills. Content included: positive reinforcement, parental monitoring, limit‐setting, parent‐child communication, and problem solving. | |
| To evaluate the effects of a parent training in managing parents successfully functioning at work, at home, and in their parenting role.
| Work Place Triple‐P program (WPTP) consisted of four sessions (2 hours each), and four additional individual telephone consultations (15 to 30 minutes each). It was designed specifically for delivering in the workplace and involved i) teaching parents 17 core positive parenting and child management strategy; ii) planning activities routine for times such as getting ready for work and arrival home from work; iii) active training methods such as video modelling, rehearsal, practice, feedback and goal setting Parents received copy of a workbook that included exercises for completion both in‐session and between sessions. | |
| To evaluate the efficacy and acceptability of a parenting programme with Japanese parents in learning and practicing positive parenting skills
| Triple P‐Positive Parenting Program comprised of five sessions (2‐hours each), and three telephone consultation sessions (20‐30 minutes each). Active skills training methods were used to facilitate the development of a self‐regulatory framework for parents, involving modelling, role‐plays, feedback and the use of specific homework. All sessions conducted in Japanese by a Japanese accredited Triple P trainer. | |
| To evaluate the efficacy and acceptability of a parenting programme with Japanese parents in Japanese society in learning and practicing positive parenting skills
| Triple P‐Positive Parenting Program comprised of five sessions (2‐hours each), and three telephone consultation sessions (20‐30 minutes each). Active skills training methods were used to facilitate the development of a self‐regulatory framework for parents, involving modelling, role‐plays, feedback and the use of specific homework. All sessions conducted in Japanese by a Japanese accredited Triple P trainer. | |
| To assess the efficacy of a parenting program in enhancing parenting skills, and subsequently in improving the behavioural and emotional adjustment of their gifted child.
| Gifted and Talented Group Triple P programme (based on the Group Triple P intervention) consisted of five weekly sessions (2 hours each), followed by three weekly telephone consultations (15‐minutes each), and a final 2 hours group session. The program involved teaching parents core child management skills: i) promoting children's development, ii) managing misbehaviour, and iii) planned activities and routines | |
| To evaluate the effectiveness of a parenting programme in preventing challenging behaviour of their child. | COPEing with toddler behaviour comprised eight weekly group sessions (2 hours each) and focused on parenting styles and strategies in preventing challenging behaviour for children in late infancy/toddlerhood. | |
| To determine whether parent training would improve a mother's knowledge about ADHD and her feelings of competence and self‐esteem in using problem‐solving strategies. | Educational programme comprised five weekly sessions (60‐90 minutes each), including information on the pathology of ADHD, its impact on family, the effects of stimulant medication, the meaning and development of a child's behaviour, enhancing positive mother‐child attention, time‐out, positive reinforcement, and the use of problem‐solving strategies. | |
| To assess the effects of a parenting programme on parenting stress and sense of competence in parents of children with ADHD.
| Parent training programme comprised twelve weekly sessions, including information on ADHD and instruction involving role‐play, modelling and homework assignments. Compliance training component differed slightly for Study 1 and Study 2. Reading material and manuals provided for participants. | |
|
| To evaluate whether a parent mediated behaviour intervention could ameliorate ADHD related deficits and behavioural problems.
| Attention‐training treatment programme comprised twelve weekly sessions, including educational material and information about ADHD, compliance training (behaviour management) and attention training. Teaching methods includes modelling, role‐play, and individual feedback to videotaped interactions. |
| To investigate the effectiveness of a behavioural parenting programme. To examine whether lecture/written materials/combination were differentially effective in teaching behavioural principles. | Behavioural parenting programme comprised five weekly sessions (2 hours each) and a This intervention was used in Group 1. Group 2 received the same programme but without the text. Group 3 received the text only plus the exercises. Group 4 were a non‐intervention control group.
| |
| To assess the impact of a culturally sensitive adaptation of parenting programme on parental skills, parental stress, anxiety and depression. | Triple‐P Positive Parenting Program, culturally adapted, comprised eight sessions: i) one group introduction session, giving an overview of the program and establishing rapport within the groups (1.5‐2 hours); ii) four group sessions (2‐2.5 hours each); iii) two home‐based consultations (30‐40 minutes each); and iv) one final group session (1.5‐2 hours). The intervention covers modelling, rehearsal, practice, feedback and goal setting, considering needs of Australian Indigenous families. | |
| To investigate the effectiveness of parenting training as adjunct to routine clinical care in enhancing parenting skills. | Behavioural Parenting Training (BPT) comprised twelve sessions (2 hours each). The program covers the following parenting skills: i) structuring the environment, ii) setting rules, iii) giving instructions, iv) anticipating misbehaviours, v) communicating, vi) reinforcing positive behaviour, vii) ignoring, viii) employing punishment, and ix) implementing token system. As a part of homework assignment, for each session parents read a chapter of a book written for this program (van der Veen‐Mulders et al, 2001); they also practice parental skills during each session, and wrote the reports. | |
| To evaluate the effects of a parenting program on the interactive skills of parents of children with autism. | Educational parenting program comprised four weekly sessions (4 hours each), supported by home visits (4 hours in total). Training program included lectures, handouts, live modelling and group discussion, which was supported by individual home visits. The purpose of the individual home visits was to observe the parent/child interaction in the natural environment and assist parents in applying the intervention strategies thought during group training. | |
| To evaluate the effectiveness of a parenting programme in promoting healthy, self‐sufficient sleep in infants; to test the hypothesis that parent training would reduce both stress and response to child wakefulness. | Behavioural parenting training comprised two prenatal sessions and two post‐natal sessions (1‐1/2 hours each). Content included information on infant sleep and methods to assist in establishing early good sleep habits. Handouts, questions and answers, group discussion and problem‐solving strategy used. Diaries and daily practice records completed and discussed.
| |
| Cognitive‐Behavioural Parenting Programme | ||
|
| To evaluate the effectiveness of a parenting programme in enhancing the self‐directedness of children with ADHD and responsibility for their own behaviour.
| Behaviour management parenting programme consisted of 12 weekly 2‐hour sessions delivered using a lecture format. Follow‐up (maintenance) sessions at 3‐ and 6‐months. Optional school consultation time offered. Topics included the re‐framing of ADHD, behaviour management based on the use of various techniques, the grief cycle, communication skills, listening, acknowledging feelings, self‐esteem, and anger‐management. |
| To examine whether a parenting programme improve maternal functioning in terms of depressive symptoms, anxiety, self‐esteem, perceived stress and cognitions about child behaviour. | Maternal Stress and Coping Group Program was a modified version of the Coping With Depression Course Program (CWDCP), which increases its relevance for mothers of children with ADHD. It comprised twelve weekly sessions, including four treatment models: i) relaxing training, ii) increasing pleasurable activities, iii) cognitive restructuring, and iv) increasing social skills/assertiveness training. Homework exercises that involved practising behavioural skills were completed. | |
| To examine the effectiveness of a parenting programme in promoting coping skills in parents of children with developmental disabilities. | Coping Skills Training Programme consisted of ten 2‐hour weekly sessions, involving cognitive restructuring, interpersonal skills training, problem solving and individual goal attainment. | |
| To examine the effectiveness of a parenting programme in reducing child conduct problem, in enhancing positive parenting skills and confidence, and in decreasing parental depression
| Webster‐Stratton Incredible Years intervention comprised a video‐based 14‐week group programme which teaches behavioural principles for managing behaviours using a collaborative, practical problem‐solving approach. Topics included parent‐child play praise, incentives, limit‐setting, problem‐solving and discipline. Each week parents practice tasks at home. Telephone calls made to encourage progress. | |
| To evaluate the effectiveness of a parenting programme in promoting positive parent‐child relationships; to promote parental self‐efficacy. | Parent and Children Series (PACS) training programme for promoting positive parent‐child relationship consisted of 10‐weekly sessions, using manual, written materials and videos. Topics included: how to play with a child, use of praise, limit setting, use of time‐out. Video‐tape vignettes used to model skills and stimulate discussion. Weekly homework assignments used. | |
| To evaluate the relative effectiveness of a parenting programme on parenting competence (higher parenting self‐efficacy, less reliance on coercive discipline strategies, and more positive parent behaviour) | Webster‐Stratton Incredible Years BASIC Programme comprised 12 weekly sessions (2 hours each). Topics covered included child‐directed play, helping young children to learn, using praise and rewards, effective limit setting, handling misbehaviour and problem solving. Home work assignments were also used. The course was taught using video vignettes which were appropriate for toddlers. | |
| To evaluate the effectiveness of a parenting programme in improving parenting competence and child behaviour. | Chicago Parent Programme (CPP) comprised 12 weekly sessions, employing videotaped vignettes and group discussion. The topics covered the concept of child‐centred time, helping young children to learn, using praise and rewards, effective limit setting, handling misbehaviour and problem solving. | |
| To assess the effectiveness of a parenting programme in reducing parental stress in parents of children with disabilities. | Rational‐Emotive Parent Education programme comprised eight weekly sessions. Content focused on core irrational beliefs and links with stress response. Programme thought the disputation of these beliefs and their replacement with rational beliefs. Teaching based on a didactic approach and included homework, completion of worksheets, and the distribution of a prepared summary sheet. | |
| To evaluate the effectiveness of a parenting programme as a preventative intervention for parents with children considered to be at risk of developing conduct disorder | Webster‐Stratton Incredible Years Basic parenting programme comprised twelve weekly sessions (2 to 2.5 hours each) and promoted positive parenting, using a collaborative approach (for example: role play, modelling, discussion, etc). | |
| To evaluate the effectiveness of a parenting programme in reducing levels of parent irrationality, negative emotions, and to assess whether the change in irrationality is correlated with changes in emotionality. | Rational‐Emotive based Parent Education programme comprised nine weekly sessions Content focused on identifying and disputing parental irrational beliefs that lead to emotional stress; the reinforcement of rational beliefs; rational problem‐solving; teaching children rational personality traits.
| |
| To examine the efficacy of a parenting programme in reducing child conducts problems.
| Webster‐Stratton Incredible Years Basic parenting programme consisted of twelve to fourteen weekly sessions (2 hours each), focusing on positive disciplinary strategies, effective parenting skills, strategies coping with stress, and ways to strengthen children's social skills. Video vignettes for discussion, role play, rehearsals and home work assessments used. | |
| To evaluate the effects of a community group‐based parenting programme on vulnerable single mothers in improving maternal wellbeing (mood, self‐esteem and social support) and parenting. | Social support and education parenting programme consisted of 10 weekly group sessions (1.5 hours each). The program covered two thematic areas: i) child related area (for example: child development and behaviour, behaviour management, school involvement, child welfare agencies), and maternal area (for example: social isolation, stress and coping, personal care and development, relationships, grief). Cognitive behavioural techniques and structured counselling were provided. | |
| To examine the effectiveness of a coping skill training programme for parents of substance‐abusing adolescents
| Behavioural‐analytic parenting programme comprised eight weekly sessions (2 hours each). Aims were to teach participants more effective skills for coping with problems resulting from their adolescent's substance abuse. | |
| To examine the effectiveness of a parenting programme with at‐risk parents of young children. | Psycho‐educational programme STAR (Stop Think Ask Respond) comprised 10 weekly sessions (1.5 hours each), employing 'segments' in which parents learned thoughtful ways to respond to children, how to have realistic expectations of children, and how to implement positive parenting and discipline strategies. | |
| To examine the effect of a short‐term intervention to reduce self‐blame and guilt in parents of children with severe disabilities.
| Cognitive‐behavioural parenting programme comprised five weekly sessions (2 hours each). Content delivered using a lecture format. Homework assigned each week consisted of monitoring automatic thoughts, cognitive distortions, negative feelings, and attempts at cognitive restructuring. Sessions focused on the cognitive distortions that contribute to self‐blame and guilt in families of children with disabilities, and techniques to deal with such distortions. | |
|
| To assess effects of a parenting programme delivered by health visitors in primary care in improving mental health of children and parents | Webster Stratton parenting programme comprised 10 weekly sessions (2 hours each). The sessions included video vignettes of parent‐child interactions, group discussion, role play, rehearsal of parenting techniques, and home practice. |
| To evaluate the additional benefit of providing a problem‐solving parenting intervention in improving parental and child behaviour. | Problem‐solving skills parenting training comprised 6 units (1 hour each), focusing on aspects of problem‐solving including: problem definition, goal setting, alternative solutions, and decision‐making. This training was used as a supplement to a 10‐hour Parent and Children Series (PACS) programme based on the work of Webster‐Stratton. Topics included how to play with a child, use of praise, limit setting, use of time‐out. Video‐tape vignettes used to model skills and stimulate discussion. Written materials and homework assignments used. | |
| To evaluate the effectiveness of parent training in reducing parental psychosocial difficulties and conduct problems in children. | Parent and Children Series (PACS) treatment intervention consisted of 11‐14 weekly sessions (2 ¼ each), using manual, written materials and videos. | |
| To compare different treatment modes in reducing parental stress and improving child behaviour.
| GDVM: Group‐based video‐tape modelling parenting skills followed by discussion. IVM: Weekly in‐clinic sessions for approximately 1‐hour viewing of self‐administered videotape without therapist or discussion. GD: Weekly therapist‐led discussion sessions covering same topics as other groups. All modes of delivery comprised 10‐12 weekly sessions (2 hours each). Content, sequencing and number of sessions constant between groups. Topics covered play skills, praises, rewards, discipline and problem‐solving approaches | |
| Other or multimodal | ||
| To investigate the feasibility, implementation, and potential effects of a parenting programme on positive changes in parenting stress and child behaviour. | Success in Parenting Preschoolers (SIP) programme consisted of 8 weekly group sessions, each lasted 2 hours. The programme included both language facilitation techniques and behaviour management strategies. The parents viewed 100 instructional pages, watched four video vignettes, and received weekly session outlines, handouts, and home reminder magnets highlighting specific parenting skills presented during that weekly session. Additional weekly phone sessions were provided. All group sessions were videotaped. | |
| To evaluate the effectiveness of a community‐based intervention on enhancing pro‐social interaction and psychological wellbeing of urban, Head Start parents.
| The COPE (Community Outreach through Parent Empowerment) intervention has two components: (a) informal support groups, and (b) implementation of the Parent as Change Agent for Self module. Involved 10 group‐training sessions (each ˜3 hrs) focusing on the relationship between stress and social support. The 10 sessions had two main purposes: to identify major categories of stressful events for urban, African‐American Head Start parents, and to consider and discuss the ways in which friendships and various connections within the community can mitigate these stressors. | |
| To examine the effect of a parenting intervention on parental stress scores. | A brief cognitively‐based group parenting training is a 30‐minute single‐session, which targeted mothers perception of a preschool‐age child. The session focused on shifting parent perception of the child. Parents learned about the connection between thoughts, feelings and behaviours. Duration of the training was in total 1.5 hours with questionnaire completion. Sessions were audio‐taped. Attention‐placebo control group received information regarding [use of] developmentally appropriate books for preschool age children during 30 minutes. The session (1.5 hours) involved questionnaire completion. | |
| To examine the effects of a parenting programme on maternal sense of competency and stress | Active Parenting Programme was an educational programme and consisted of sessions (11/2 hours each). Content focused on understanding children's behaviour and misbehaviour, responsible parenting, effective communication and discipline, and developing responsibility in children. The training format used a variety of teaching techniques including lecture, videos, group discussion, and role‐play. | |
| Gutierrez 2007 (Adlerian) | To evaluate the efficacy of two parenting programmes in reducing perceived parental stress | Adlerian‐based parenting programme (APP) is the Systematic Training for Effective Parenting (STEP) program which included components on understanding yourself and your child, beliefs and feelings, encouraging your child and yourself, listening and talking to your child and problem solving. Each programme consists of eight 2 hour weekly sessions, delivered in Spanish. |
| To evaluate the effectiveness of a parenting programme in empowering parents to strengthen family resources. | Model based on a three‐tiered approach to developing personal coping and social support. Designed to strengthen interpersonal, intrapersonal and social resources by means of group work, discussion and didactic input. Topics included: family dynamics, loss and grief, communication and conflict resolution, networking and resource utilisation, stress management and relaxation skills. | |
| To assess the effectiveness of a parenting programme in reducing parenting stress, and in improving parental mood, family functioning, parenting style, locus of control, and perceived social support of children with ADHD. | Parent Stress Management (PSM) training program comprised nine weekly sessions (2 hour each). The program covered: Session 1: Orientation to the program and understanding stress; Session 2: Education about ADHD; Session 3: Rights and reasons; Session 4: Problem‐solving skills; Session 5: Cognitive restructuring; Session 6: Communication skills; Session 7: Self‐care skills; Session 8: Parenting skills; Session 9: Wrap‐up session. | |
| To evaluate the effects of a parenting programme in enhancing parent adaptive behaviour through emphasis on parental self‐reflection, social support and the emotional roots of children's misbehaviour and parenting stress. | Study 1 ‐ Counselling and social support parent programme. Listening to Children (LTC) parent training comprised eight weekly sessions (2.5 hours each) and was based on re‐evaluation counselling. It focused on the three core themes: recognising the effects of parents own childhood experience, spending special time with children, and understanding and handling children's emotions and upsets. Each session involved in‐class activities, reading assignments, and homework projects built around those themes. |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Depressive symptoms Show forest plot | 27 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 Post intervention (immediate post intervention up to four weeks post intervention) | 22 | 1591 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.17 [‐0.28, ‐0.07] |
| 1.2 Short term follow up (one to six months post intervention) | 13 | 2104 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.10 [‐0.22, 0.03] |
| 1.3 Long term follow up (more than six months post intervention) | 7 | 1491 | Std. Mean Difference (IV, Random, 95% CI) | 0.02 [‐0.10, 0.13] |
| 2 Anxiety symptoms Show forest plot | 11 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 Post intervention (immediate post intervention up to four weeks post intervention) | 9 | 464 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.22 [‐0.43, ‐0.01] |
| 2.2 Short term follow up (one to six months post intervention) | 3 | 882 | Std. Mean Difference (IV, Random, 95% CI) | 0.05 [‐0.08, 0.19] |
| 2.3 Long term follow up (more than six months post intervention) | 2 | 739 | Std. Mean Difference (IV, Random, 95% CI) | 0.02 [‐0.13, 0.16] |
| 3 Stress Show forest plot | 29 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.1 Post intervention (immediate post intervention up to four weeks post intervention) | 25 | 1567 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.29 [‐0.42, ‐0.15] |
| 3.2 Short term follow up (one to six months post intervention) | 12 | 1680 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.22 [‐0.42, ‐0.01] |
| 3.3 Long term follow up (more than six months post intervention) | 4 | 1121 | Std. Mean Difference (IV, Random, 95% CI) | 0.02 [‐0.10, 0.13] |
| 4 Self esteem Show forest plot | 3 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 4.1 Post intervention (immediate post intervention up to four weeks post intervention) | 2 | 147 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.01 [‐0.45, 0.42] |
| 4.2 Short term follow up (one to six months post intervention) | 2 | 193 | Std. Mean Difference (IV, Random, 95% CI) | 0.06 [‐0.22, 0.34] |
| 4.3 Long term follow up (more than six months post intervention) | 2 | 168 | Std. Mean Difference (IV, Random, 95% CI) | 0.10 [‐0.21, 0.40] |
| 5 Anger Show forest plot | 3 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 5.1 Post intervention (immediate post intervention up to four weeks post intervention) | 3 | 107 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.60 [‐1.00, ‐0.20] |
| 6 Guilt Show forest plot | 3 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 6.1 Post intervention (immediate post intervention up to four weeks post intervention) | 3 | 119 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.79 [‐1.18, ‐0.41] |
| 7 Confidence Show forest plot | 15 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 7.1 Post intervention (immediate post intervention up to four weeks post intervention) | 14 | 1001 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.34 [‐0.51, ‐0.17] |
| 7.2 Short term follow up (one to six months post intervention) | 7 | 636 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.32 [‐0.63, ‐0.01] |
| 7.3 Long term follow up (more than six months post intervention) | 2 | 381 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.39 [‐1.16, 0.38] |
| 8 Partner satisfaction Show forest plot | 9 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 8.1 Post intervention (immediate post intervention up to four weeks post intervention) | 9 | 432 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.28 [‐0.47, ‐0.09] |
| 8.2 Short term follow up (one to six months post intervention) | 1 | 46 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.33 [‐0.91, 0.25] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Parental outcomes: depressive symptoms (Beck Depression Inventory) Show forest plot | 9 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.1 Post intervention (immediate post intervention up to four weeks post intervention) | 8 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Short term follow up (one to six months post intervention) | 3 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 Long term follow up (more than six months post intervention) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Parental outcomes: depressive symptoms (subscale of Irritability Depression & Anxiety Scale) | 0 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2.1 Post intervention (immediate post intervention up to four weeks post intervention) | 0 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Parental outcomes: depressive symptoms (subscale of Depression Anxiety Stress Scale) Show forest plot | 8 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3.1 Post intervention (immediate post intervention up to four weeks post intervention) | 6 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Short term follow up (one to six months post intervention) | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.3 Long term follow up (more than six months post intervention) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Parental outcomes: depressive symptoms (Centre for Epidem. Studies Depression Scale) Show forest plot | 6 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4.1 Post intervention (immediate post intervention up to four weeks post intervention) | 4 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 Short term follow up (one to six months post intervention) | 6 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.3 Long term follow up (more than six months post intervention) | 4 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Parental outcomes: depressive symptoms (subscale of Parenting Stress Index) Show forest plot | 3 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 5.1 Post intervention (immediate post intervention up to four weeks post intervention) | 3 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.2 Short term follow up (one to six months post intervention) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Parental outcomes: depressive symptoms (subscale of General Health Questionnaire) Show forest plot | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 6.1 Post intervention (immediate post intervention up to four weeks post intervention) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.2 Short term follow up (one to six months post intervention) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.3 Long term follow up (more than six months post intervention) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Parental outcomes: anxiety symptoms (subscale of Depression Anxiety Stress Scale) Show forest plot | 7 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 7.1 Post intervention (immediate post intervention up to four weeks post intervention) | 5 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.2 Short term follow up (one to six months post intervention) | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.3 Long term follow up (more than six months post intervention) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8 Parental outcomes: anxiety symptoms (subscale of Irritability, Depression and Anxiety Scale) | 0 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 8.1 Post intervention (immediate post intervention up to four weeks post intervention) | 0 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 9 Parental outcomes: anxiety symptoms (subscale of General Health Questionnaire) Show forest plot | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 9.1 Post intervention (immediate post intervention up to four weeks post intervention) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 9.2 Short term follow up (one to six months post intervention) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 9.3 Long term follow up (more than six months post intervention) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 10 Parental outcomes: anxiety symptoms (STAI State scale) Show forest plot | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 10.1 Post intervention (immediate post intervention up to four weeks post intervention) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 11 Parental outcomes: anxiety symptoms (STAI Trait scale) | 0 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 11.1 Post intervention (immediate post intervention up to four weeks post intervention) | 0 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 11.2 Short term follow up (one to six months post intervention) | 0 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 12 Parental outcomes: anxiety symptoms (Beck Anxiety Inventory) Show forest plot | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 12.1 Post intervention (immediate post intervention up to four weeks post intervention) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 13 Parental outcomes: anxiety symptoms (Brief Symptom Inventory) Show forest plot | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 13.1 Post intervention (immediate post intervention up to four weeks post intervention) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 14 Parental outcomes: stress (Perceived Stress Scale) Show forest plot | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 14.1 Post intervention (immediate post intervention up to four weeks post intervention) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 15 Parental outcomes: stress (Parenting Stress Index: overall score) Show forest plot | 3 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 15.1 Post intervention (immediate post intervention up to four weeks post intervention) | 3 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 15.2 Short term follow up (one to six months post intervention) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 15.3 Long term follow up (more than six months post intervention) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 16 Parental outcomes: stress (Parenting Stress Index: parent domain score) Show forest plot | 6 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 16.1 Post intervention (immediate post intervention up to four weeks post interven | 6 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 16.2 Short term follow up (one to six months post intervention) | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 17 Parental outcomes: stress (Parenting Stress Index ‐ short form: overall score) Show forest plot | 4 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 17.1 Post intervention (immediate post intervention up to four weeks post intervention) | 3 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 17.2 Short term follow up (one to six months post intervention) | 3 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 18 Parental outcomes: stress (Parenting Stress Index ‐ short form: distress subscale) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 18.1 Post intervention (immediate post intervention up to four weeks post intervention) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 19 Parental outcomes: stress (Everyday Stress Index) Show forest plot | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 19.1 Post intervention (immediate post intervention up to four weeks post intervention) | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 19.2 Short term follow up (one to six months post intervention) | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 19.3 Long term follow up (more than six months post intervention) | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 20 Parental outcomes: stress (Ability & Confidence Rating Questionnaire) Show forest plot | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 20.1 Post intervention (immediate post intervention up to four weeks post intervention) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 21 Parental outcomes: stress (Parental Stress Scale) Show forest plot | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 21.1 Post intervention (immediate post intervention up to four weeks post intervention) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 21.2 Short term follow up (one to six months post intervention) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 22 Parental outcomes: stress (modified Uplifts & Hassles Scale: hassles scale) Show forest plot | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 22.1 Post intervention (immediate post intervention up to four weeks post intervention) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 22.2 Short term follow up (one to six months post intervention) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 23 Parental outcomes: stress (subscale of Depression Anxiety Stress Sscale) Show forest plot | 8 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 23.1 Post intervention (immediate post intervention up to four weeks post intervention) | 6 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 23.2 Short term follow up (one to six months post intervention) | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 23.3 Long term follow up (more than six months post intervention) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 24 Parental outcomes: self‐esteem (Rosenberg Self‐Esteem scale) Show forest plot | 3 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 24.1 Post intervention (immediate post intervention up to four weeks post intervention) | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 24.2 Short term follow up (one to six months post intervention) | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 24.3 Long term follow up (more than six months post intervention) | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 25 Parental outcomes: anger (subscale of Berger's Feeling Scale) Show forest plot | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 25.1 Post intervention (immediate post intervention up to four weeks post intervention) | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 26 Parental outcomes: anger (State‐Trait Anger Expression Inventory scale) Show forest plot | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 26.1 Post intervention (immediate post intervention up to four weeks post intervention) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 27 Parental outcomes: guilt (subscale of Berger's Feeling Scale) Show forest plot | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 27.1 Post intervention (immediate post intervention up to four weeks post intervention) | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 28 Parental outcomes: guilt (Situation Guilt Scale) Show forest plot | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 28.1 Post intervention (immediate post intervention up to four weeks post intervention) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 29 Parental outcomes: confidence (Parenting Task Checklist) Show forest plot | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 29.1 Post intervention (immediate post intervention up to four weeks post intervention) | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 30 Parental outcomes: confidence (Parental Efficacy measure) Show forest plot | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 30.1 Short term follow up (one to six months post intervention) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 31 Parental outcomes: confidence (Parenting Stress Index) Show forest plot | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 31.1 Post intervention (immediate post intervention up to four weeks post intervention) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 31.2 Short term follow up (one to six months post intervention) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 32 Parental outcomes: confidence (Toddler Care Questionnaire) Show forest plot | 3 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 32.1 Post intervention (immediate post intervention up to four weeks post intervention) | 3 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 32.2 Short term follow up (one to six months post intervention) | 3 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 32.3 Long term follow up (more than six months post intervention) | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 33 Parental outcomes: confidence (Parenting Sense of Competence Scale: total score) Show forest plot | 4 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 33.1 Post intervention (immediate post intervention up to four weeks post intervention) | 4 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 33.2 Short term follow up (one to six months post intervention) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 34 Parental outcomes: confidence (Problem Setting & Behaviour Checklist) Show forest plot | 3 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 34.1 Post intervention (immediate post intervention up to four weeks post intervention) | 3 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 35 Parental outcomes: confidence (Kansas Parental Satisfaction Scale: satisfaction in parental role) Show forest plot | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 35.1 Post intervention (immediate post intervention up to four weeks post intervention) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 35.2 Short term follow up (one to six months post intervention) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 36 Parental outcomes: partner satisfaction (Dyadic Adjustment Scale) Show forest plot | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 36.1 Post intervention (immediate post intervention up to four weeks post intervention) | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 37 Parental outcomes: partner satisfaction (Locke‐Wallace Marital Adjustment Test) Show forest plot | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 37.1 Post intervention (immediate post intervention up to four weeks post intervention) | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 38 Parental outcomes: partner satisfaction (Parenting Stress Index) Show forest plot | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 38.1 Post intervention (immediate post intervention up to four weeks post intervention) | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 38.2 Short term follow up (one to six months post intervention) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 39 Parental outcomes: partner satisfaction (Relation Quality Index) Show forest plot | 3 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 39.1 Post intervention (immediate post intervention up to four weeks post intervention) | 3 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 40 Father outcomes: depressive symptoms (Beck Depression Inventory) Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 40.1 Post intervention (immediate post intervention up to four weeks post intervention) | 1 | 18 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.53 [‐1.48, 0.42] |
| 41 Father outcomes: depressive symptoms (Center for Epidemiological Studies Depression Scale Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 41.1 Post intervention (immediate post intervention up to four weeks post intervention) | 1 | 16 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.39 [‐1.41, 0.64] |
| 41.2 Short term follow up (one to six months post intervention) | 1 | 16 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.63 [‐1.67, 0.42] |
| 42 Father outcomes: stress (Parenting Stress Index: parent domain subscale) Show forest plot | 4 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 42.1 Post intervention (immediate post intervention up to four weeks post intervention) | 4 | 123 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.43 [‐0.79, ‐0.06] |
| 42.2 Short term follow up (one to six months post intervention) | 1 | 16 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.24 [‐1.25, 0.78] |
| 43 Father outcomes: confidence (Toddler Care Questionnaire: overall scores) Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 43.1 Post intervention (immediate post intervention up to four weeks post intervention) | 1 | 17 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.07 [‐1.06, 0.93] |
| 43.2 Short term follow up (one to six months post intervention) | 1 | 17 | Std. Mean Difference (IV, Random, 95% CI) | 0.68 [‐0.35, 1.70] |
| 44 Father outcomes: partner satisfaction (Locke‐Wallace Marital Adjustment Test) Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 44.1 Post intervention (immediate post intervention up to four weeks post intervention) | 1 | 16 | Std. Mean Difference (IV, Random, 95% CI) | 0.63 [‐0.39, 1.65] |

