Interventions for recurrent corneal erosions
Abstract
Background
Recurrent corneal erosion is a common cause of disabling ocular symptoms and predisposes the cornea to infection. It may follow corneal trauma. Measures to prevent the development of recurrent corneal erosion following corneal trauma have not been firmly established. Once recurrent corneal erosion develops, simple medical therapy (standard treatment) may lead to resolution of the episode. However, some people continue to suffer when such therapy fails and repeated episodes of erosion develop. A number of treatment and prophylactic options are then available but there is no agreement as to the best option. This review version is an update to the original version published in 2007 and a previous update published in 2012.
Objectives
To assess the effectiveness and adverse effects of regimens for the prophylaxis of further recurrent corneal erosion episodes, the treatment of recurrent corneal erosion and prophylaxis of the development of recurrent corneal erosion following trauma.
Search methods
We searched CENTRAL, which contains the Cochrane Eyes and Vision Trials Register; MEDLINE; Embase; LILACS; the ISRCTN registry; ClinicalTrials.gov and the ICTRP. The date of the search was 14 December 2017.
Selection criteria
We included randomised and quasi‐randomised trials that compared a prophylactic or treatment regimen with another prophylaxis/treatment or no prophylaxis/treatment for people with recurrent corneal erosion.
Data collection and analysis
We used standard methods expected by Cochrane. Two authors independently screened search results, extracted data and assessed risk of bias in the included studies using the Cochrane tool for assessing risk of bias. We considered the following outcome measures: resolution of symptoms after treatment; recurrence after complete or partial resolution; symptoms (pain); adverse effects (corneal haze, astigmatism). We graded the certainty of the evidence using GRADE for the three most clinically relevant comparisons.
Main results
We included eight randomised and two quasi‐randomised controlled trials in the review, encompassing 505 participants. Seven studies were from Europe (Germany, Sweden and the UK), two from East Asia (Hong Kong and Japan) and one from Australia. Nine of the studies examined treatments for episodes of recurrent corneal erosions and one study considered prophylaxis to prevent development of recurrent corneal erosions after injury. Two of the nine treatment studies also enrolled participants in a study of prophylaxis to prevent further episodes of recurrent corneal erosions. The studies were poorly reported; we judged only one study low risk of bias on all domains.
Two studies compared therapeutic contact lens with topical lubrication but one of these studies was published over 30 years ago and used a therapeutic contact lens that is no longer in common use. The more recent study was a two‐centre UK study with 29 participants. It provided low‐certainty evidence on resolution of symptoms after treatment with similar number of participants in both groups experiencing resolution of symptoms at four months (risk ratio (RR) 0.97, 95% confidence interval (CI) 0.62 to 1.53). There was very low‐certainty evidence on recurrence after partial or total resolution at seven months' follow‐up (RR 1.07, 95% CI 0.07 to 15.54). There was no evidence of an important difference in pain score (score of 3 in the contact lens group and score of 2 in the topical lubrication group, low‐certainty evidence) and no adverse effects were reported. The older study, using a contact lens no longer in common use, found an increased risk of pain and complications with the contact lens compared with hypromellose drops and paraffin ointment at night.
A single‐centre, Australian study, with 33 participants, provided low‐certainty evidence of an increased risk of recurrence with phototherapeutic keratectomy compared with alcohol delamination but with wide confidence intervals, compatible with increased or decreased risk (RR 1.27, 95% CI 0.48 to 3.37). Time to recurrence was similar in both groups (6.5 and 6 months, low‐certainty evidence). On average people receiving phototherapeutic keratectomy reported less pain but confidence intervals included no difference or greater pain (mean difference (MD) ‐0.70, 95% CI ‐2.23 to 0.83, low‐certainty evidence). No adverse effects were reported.
A 48‐participant study in Hong Kong found recurrences were less common in people given diamond burr superficial keratectomy after epithelial debridement compared with sham diamond burr treatment after epithelial debridement (RR 0.07, 95% CI 0.01 to 0.50, moderate‐certainty evidence). The study did not report pain scores but adverse effects such as corneal haze (RR 0.92, 95% CI 0.06 to 13.87, low‐certainty evidence) and astigmatism (0.88 versus 0.44 dioptres, moderate‐certainty evidence) were similar between the groups.
A study comparing transepithelial versus subepithelial excimer laser ablation in 100 people found low‐certainty evidence of a small increased risk of recurrence of corneal erosion at one‐year follow‐up in people given the transepithelial compared with subepithelial technique, however, the confidence intervals were wide and compatible with increased or decreased risk (RR 1.20, 95% CI 0.58 to 2.48, low‐certainty evidence). Other outcomes were not reported.
Other treatment comparisons included in this review were only addressed by studies published two decades or more ago. The results of these studies were inconclusive: excimer laser ablation (after epithelial debridement) versus no excimer laser ablation (after epithelial debridement), epithelial debridement versus anterior stromal puncture, anterior stromal puncture versus therapeutic contact lens, oral oxytetracycline and topical prednisolone (in addition to 'standard therapy') versus oral oxytetracycline (in addition to 'standard therapy') versus 'standard therapy'.
Authors' conclusions
Well‐designed, masked, randomised controlled trials using standardised methods are needed to establish the benefits of new and existing prophylactic and treatment regimes for recurrent corneal erosion. Studies included in this review have been of insufficient size and quality to provide firm evidence to inform the development of management guidelines. International consensus is also needed to progress research efforts towards evaluation of the major effective treatments for recurrent corneal erosions.
PICO
Plain language summary
Prevention and treatment regimens for recurrent corneal erosion (corneal epithelial surface breakdown)
What is the aim of this review?
The aim of this Cochrane Review was to find what treatment works best for recurrent corneal erosions and whether they can be prevented. Cochrane researchers collected and analysed all relevant studies to answer this question and found 10 studies.
Key messages
The review shows that there is a lack of good‐quality evidence to guide treatment decisions for recurrent corneal erosions. This is an evidence gap.
What was studied in the review?
The cornea is the clear front part of the eye. Sometimes the outermost layer of cells in the cornea (epithelium) breaks down and this can lead to repeated episodes of eye pain or discomfort, sensitivity to light, watering eyes and blurred vision. This is known as recurrent corneal erosion (RCEs). These symptoms can be disabling, and RCEs can make the eye more prone to infection. RCEs can happen after eye injury but are also a consequence of eye conditions, such as corneal dystrophy.
Various treatments have been proposed and are used for RCEs. Eye drops moisten the eye (lubricants) or may contain antibiotics or steroids. Special contact lenses, known as therapeutic or bandage contact lenses, may be used. A section or layer of the cornea can be physically removed, which is known as debridement when the loose epithelium is removed, or superficial keratectomy when the epithelium and other material is removed. This can be done manually or using an 'excimer' laser (phototherapeutic). Sometimes the cornea is 'polished' afterwards using a tool called a diamond burr. This material can also be removed using alcohol (alcohol delamination). Small puncture holes, called anterior stromal punctures, may be made in the cornea with the aim of stabilising the epithelium. This can also be done with a laser.
What are the main results of the review?
Cochrane researchers found 10 relevant studies. Seven studies were from Europe (Germany, Sweden and the UK), two from East Asia (Hong Kong and Japan) and one from Australia.
Two studies compared contact lens versus lubricant; single studies looked at phototherapeutic keratectomy versus alcohol delamination; diamond burr superficial keratectomy (after epithelial debridement) compared with epithelial debridement; two different techniques of laser removal of material (transepithelial versus subepithelial excimer laser ablation); contact lens compared with anterior stromal puncture; epithelial debridement compared with anterior stromal puncture; phototherapeutic keratectomy (after epithelial debridement) compared with epithelial debridement alone; and oral tetracycline compared with both topical prednisolone and standard therapy.
Three studies (including two of the above treatment studies) compared different ways of preventing RCEs (prophylaxis). Two studies compared topical lubrication with no topical lubrication; and one study compared antibiotic ointment versus no antibiotic ointment.
In general the studies included in this review were too small to provide conclusive results. More good‐quality randomised controlled trials are needed to guide the management of recurrent corneal erosions.
How up to date is this review?
Cochrane researchers searched for studies that had been published up to December 2017.
Authors' conclusions
Summary of findings
| Therapeutic contact lens versus topical lubrication | ||||||
| Patient or population: people with recurrent corneal erosion syndrome without previous surgical intervention Settings: outpatient Intervention: therapeutic contact lens Comparison: topical lubrication | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Certainty of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Topical lubrication | Therapeutic contact lens | |||||
| Resolution of symptoms after treatment Follow‐up: 4 months | 730 per 1000 | 708 per 1000 (453 to 1000) | RR 0.97 (0.62 to 1.53) | 29 participants (1 study) | ⊕⊕⊝⊝ | |
| Recurrence after complete or partial resolution Follow‐up: 7 months | 67 per 1000 | 72 per 1000 (0 to 1000) | RR 1.07 (0.07 to 15.54) | 29 participants (1 study) | ⊕⊝⊝⊝ | Single study only followed up participants with complete resolution to screen for recurrence |
| Time to recurrence | Outcome not reported for this comparison | |||||
| Recurrences requiring further treatment | See comment | ‐ | ‐ | ‐ | ‐ | Neither study reported this outcome but one study stated that the two recurrences were minor symptoms with no obvious macroerosions. |
| Symptoms (pain score) Follow‐up: 3 months (higher score indicates more pain, unclear range of scale but probably 0 to 10) | Mean pain score with topical lubrication was 2 | Mean pain score with therapeutic contact lens was 1 higher (worse) | ‐ | 29 participants (1 study) | ⊕⊕⊝⊝ | Visual analogue scale range not specified, standard deviations not reported One other study of 24 participants reported more pain in contact lens group (RR 3.15, 95% CI 1.10, 9.06) but contact lens used is no longer in common use |
| Adverse effects: corneal haze | See comment | ‐ | ‐ | ‐ | ⊕⊝⊝⊝ | The more recent study did not report this outcome. The older study using a lens no longer in common use reported more complications with the contact lens. |
| Adverse effects: astigmatism | Outcome not reported for this comparison | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence High‐certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate‐certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low‐certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low‐certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
| 1Downgraded one level for risk of bias due to serious limitation in study design and execution (the single study has a high risk of bias due to lack of blinding of study personnel). | ||||||
| Phototherapeutic keratectomy versus alcohol delamination | ||||||
| Patient or population: people with recurrent corneal erosion syndrome without previous surgical intervention Settings: outpatient Intervention: phototherapeutic keratectomy (after epithelial debridement) Comparison: alcohol delamination and sham excimer laser (after epithelial debridement) | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Certainty of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Alcohol delamination | Phototherapeutic keratectomy | |||||
| Resolution of symptoms after treatment Follow‐up: 3 months | 590 per 1000 | 378 per 1000 (177 to 797) | RR 0.64 (0.30 to 1.35) | 33 participants (1 study) | ⊕⊕⊝⊝ | |
| Recurrence after complete or partial resolution Follow‐up: 24 months | 294 per 1000 | 373 per 1000 (141 to 991) | RR 1.27 (0.48 to 3.37) | 33 participants (1 study) | ⊕⊕⊝⊝ | All participants were followed for recurrence up to 24 months |
| Time to recurrence Follow‐up: 24 months | Mean time to recurrence in the control group was 6 months | Mean time to recurrence in the intervention group was 0.5 months longer | ‐ | 33 participants (1 study) | ⊕⊕⊝⊝ | Standard deviations not reported but difference between groups was reported to be not statistically significant |
| Recurrences requiring further treatment Follow‐up: 24 months | 176 per 1000 | 125 per 1000 (25 to 651) | RR 0.71 (0.14 to 3.70) | 33 participants (1 study) | ⊕⊝⊝⊝ | Further treatment of choice not indicated |
| Symptoms (pain score) (scale 0‐10) (lower scores indicate less pain) Follow‐up: 24 months | Mean pain score in the control group was1.7 | Mean pain score in the intervention group was 0.7 lower (2.23 lower to 0.83 higher) | ‐ | 33 participants (1 study) | ⊕⊕⊝⊝ | |
| Adverse effects: corneal haze Follow‐up: 12 months | There were no events in either group. | 33 participants (1 study) | ⊕⊝⊝⊝ | |||
| Adverse effects: astigmatism | Outcome not reported for this comparison | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence High‐certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate‐certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low‐certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low‐certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
| 1Downgraded one level for imprecision: small sample size | ||||||
| Diamond burr superficial keratectomy (after epithelial debridement) versus sham diamond burr (after epithelial debridement) | ||||||
| Patient or population: people with recurrent corneal erosion syndrome without other corneal basement membrane dystrophy Settings: outpatient Intervention: diamond burr superficial keratectomy after epithelial debridement Comparison: sham diamond burr superficial keratectomy after epithelial debridement | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Certainty of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Sham diamond burr superficial keratectomy after epithelial debridement | Diamond burr superficial keratectomy after epithelial debridement | |||||
| Resolution of symptoms after treatment | Outcome not reported for this comparison | |||||
| Recurrence after complete or partial resolution Follow‐up: 6 months | 565 per 1000 | 40 per 1000 | RR 0.07 (0.01 to 0.50) | 48 participants (1 study) | ⊕⊕⊕⊝ | Single study reported major recurrence defined as those requiring ophthalmologist assessment |
| Time to recurrence Follow‐up: 6 months | Mean time to recurrence with sham diamond burr was 2.4 months | Mean time to recurrence in the intervention group was 3.6 months longer | ‐ | 48 participants (1 study) | ⊕⊕⊝⊝ | Only one event in diamond burr group |
| Recurrences requiring further treatment | Outcome not reported for this comparison | |||||
| Symptoms (pain score) | Outcome not reported for this comparison | |||||
| Adverse effects: corneal haze Follow‐up: 6 months | 43 per 1000 | 40 per 1000 | 0.92 (0.06‐13.87) | 48 participants (1 study) | ⊕⊕⊝⊝ | Four point scale was used to grade degree of haze (absent, mild, moderate, severe). Single study reported 1 mild haze and 1 moderate in the control and intervention groups respectively. Haze was analysed as dichotomous variable. |
| Adverse effects: astigmatism (mean magnitude) measured in dioptres. Higher value is worse astigmatism. Follow‐up: 3 weeks | Mean astigmatism in the sham diamond burr group was 0.88 dioptres | Mean astigmatism in the diamond burr group was 0.44 dioptres less (better) | ‐ | 48 participants (1 study) | ⊕⊕⊕⊝ | No standard deviations available |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence High‐certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate‐certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low‐certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low‐certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
| 1 Downgraded one level for imprecision: small sample size ‐ did not reach target sample size per included power calculations. | ||||||
Background
Description of the condition
Recurrent corneal erosion is a relatively common clinical disorder that is characterised by repeated episodes of breakdown of the corneal epithelium (Brown 1976; Chandler 1945). Erosions can occur spontaneously, following superficial corneal injury, in certain corneal dystrophies (such as epithelial basement membrane (map‐dot‐fingerprint) dystrophy or lattice dystrophy), and in systemic illnesses such as epidermolysis bullosa. People with this condition experience repeated episodes of ocular discomfort and blurred vision and some may require prolonged therapy (Heyworth 1998). Abnormal formation of hemidesmosomes or anchoring filaments (cellular attachments) at the basal layer of the corneal epithelium are believed to play an important role in the pathogenesis of recurrent corneal erosion (Wood 1984). Matrix metalloproteinases (extracellular proteolytic enzymes) may have a role in degrading epithelial cell attachments (Dursun 2001). Bernauer 1996 and colleagues proposed that the lids may adhere to the cornea overnight due to thinning of the tear film. A shearing force on the corneal epithelium may then occur due to movement of the lid on waking or of the eye during rapid eye movement sleep thus producing a corneal erosion.
The incidence and prevalence of recurrent corneal erosion is not known with certainty. In a retrospective case series of 104 people with recurrent corneal erosion a history of trauma was reported in around half of them, epithelial basement membrane dystrophy in around a third of them and the majority of the remaining people had a history of both trauma and epithelial basement membrane dystrophy (Reidy 2000). The mean age of presentation has been reported as 43 years (range 14 to 77 years) with a preponderance of recurrent corneal erosion in women (Reidy 2000). Traumatic corneal abrasion, a leading precipitating cause for recurrent corneal erosion, is one of the commonest causes for attendance in eye casualty and general emergency departments (Jones 1986). The incidence of recurrent corneal erosion following traumatic corneal abrasion has been estimated at one in 150 cases (Jackson 1960).
Recurrent corneal erosion is typically diagnosed on the basis of a clinical history of repeated episodes of ocular discomfort that develops with or without a prior corneal epithelial abrasion or injury. Patients will report episodes of pain, watering of the eye, increased sensitivity to light and blurring of vision, typically on waking. These episodes are interspersed with periods where the eye is relatively quiet or completely asymptomatic. The characteristic complaint is of early morning eye pain with or without preceding trauma (Wood 1984). Symptoms result from the breakdown of the corneal epithelium. Erosions can resolve quickly and may be missed on examination.
Two types of recurrent corneal erosion have been described (Chandler 1945). In the macroform type (macroerosions) there is extensive loss of corneal epithelium accompanied by severe symptoms that may take several days to resolve. In the microform type (microerosions) there is a small area of epithelial loss; this type of erosion occurs more frequently but is milder and of shorter duration (Chandler 1945; Wood 1984). However, this terminology is not in routine clinical use and there is evidence that there is no clear distinction between these types of recurrent corneal erosion (Brown 1976).
There are no specific diagnostic tests for recurrent corneal erosion. Signs of recurrent corneal erosion are best visualised with slit‐lamp examination using a cobalt‐blue light following the instillation of topical fluorescein. A frank epithelial defect or loose epithelium will be seen (Reidy 2000). In some patients clinical signs or evidence of an underlying epithelial basement membrane disorder such as microcysts and epithelial lines may aid the diagnosis (Chandler 1945; Wood 1984). Meibomian gland dysfunction has been reported to co‐exist in people with recalcitrant recurrent corneal erosion (Hope‐Ross 1994a).
Description of the intervention
Simple medical therapy may be used, for example, ointment at night following traumatic corneal abrasion (Eke 1999).
Standard (empirical) therapy involves topical ointments, patching of the eye, dilation of the pupil and topical antibiotics, used alone or in combination (Eke 1999; Hope‐Ross 1994a; Hykin 1994). Their adverse effects or effectiveness have not been established in clinical trials. A Cochrane Review found that patching simple corneal abrasions, following trauma or a foreign body, does not improve healing rates or reduce pain (Lim 2016).
Alternative strategies, when the above do not work, include the following.
-
Removal of the loose epithelium by mechanical debridement, superficial keratectomy or excimer laser phototherapeutic keratectomy (PTK) (Maini 2002; Ohman 1998). Diamond burr polishing produces fewer recurrences compared to simple epithelial debridement (Wong 2009). Alcohol delamination (Dua 2006; Singh 2007) has been described as a safer and less invasive procedure compared to mechanical or laser debridement.
-
A therapeutic contact lens has been used for recalcitrant recurrent erosion involving the visual axis.
-
Nd:YAG laser treatment, needle anterior stromal puncture or microdiathermy have been used to promote epithelial stability via the production of subepithelial scar tissue (Geggel 1990; McLean 1986; Wood 1984).
-
Oral tetracycline 250 mg twice daily for 12 weeks or topical prednisolone 0.5% four times daily for seven days, or both (Hope‐Ross 1994), or oral doxycycline 50 mg twice daily and topical corticosteroid (either methylprednisolone 1%, prednisolone acetate 1% or fluoromethalone 0.1%) three times a day for two to three weeks (Dursun 2001) have been added to standard treatment regimens. Autologous serum eye drops three to eight times per day for three to six months have been used in patients not improving on the standard therapy or for whom antibiotic therapy has failed, or both (del Castillo 2002; Ziakas 2010).
How the intervention might work
The standard treatments are given on the basis of symptomatic relief and prophylaxis for infection. The theoretical basis of the alternative therapies is outlined below.
-
Removal of loose epithelium by mechanical debridement, superficial keratectomy or PTK. This is thought to strengthen the adhesion of the basal epithelial cells to the basement membrane (Maini 2002; Ohman 1998). Alcohol delamination is thought to be a superior method because it does not seem to disrupt the lamina lucida (Menucci 2010) and therefore has a reduced risk of excessive scarring or alteration of the optical properties of the cornea, or both.
-
A therapeutic contact lens may protect the epithelium from the shearing force of the lids but requires monitoring of the patient for microbial keratitis (Liu 1996; Williams 1985).
-
The production of subepithelial scar tissue is thought to strengthen the junction between epithelium and basement membrane. It has been observed that eyes with penetrating corneal injuries are less likely to get recurrent corneal erosion as a complication.
-
Oral tetracyclines and topical steroid regimens are thought to inhibit matrix metalloproteinases and hence reduce protein breakdown to preserve the bond between the epithelium and basement membrane.
-
Autologous serum therapy is thought to provide fibronectin, which promotes epithelial migration and anchorage.
Why it is important to do this review
Recurrent corneal erosion is a common, painful and debilitating ocular condition. However, as the many different prophylactic and treatment options available suggest, there is no agreement as to the best management. In this review we aimed to analyse evidence from randomised trials to determine the risks and benefits of prophylactic and treatment modalities available for recurrent corneal erosion. However, as different therapies have been trialled for the prophylaxis and treatment of recurrent corneal erosion episodes and for averting the occurrence of recurrent corneal erosion after a corneal injury, we analysed the studies on recurrent corneal erosion in three groups. Regimens to:
-
avert the development of recurrent corneal erosion following a traumatic corneal erosion (prophylaxis of the development of recurrent corneal erosion);
-
treat episodes of recurrent corneal erosion (treatment of recurrent corneal erosion); and
-
prevent the occurrence of further episodes once a diagnosis of recurrent corneal erosion has been made (prophylaxis of further episodes of recurrent corneal erosion).
This current review is an update to the original version published in 2007 and a previous update published in 2012. Both previous versions of the review concluded that there is a need for well‐designed, masked, randomised controlled trials using standardised methods to establish the benefits of new and existing prophylactic and treatment regimens for recurrent corneal erosion.
Objectives
To assess the effectiveness and adverse effects of regimens for the prophylaxis of further recurrent corneal erosion episodes, the treatment of recurrent corneal erosion and prophylaxis of the development of recurrent corneal erosion following trauma.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised and quasi‐randomised trials.
Types of participants
Participants in the studies were:
-
people with recurrent corneal erosion occurring spontaneously, following corneal trauma, or with evidence of epithelial basement dystrophy; or
-
people with traumatic corneal abrasions.
The diagnosis of recurrent corneal erosion was based on the typical history of eye pain and watering with increased sensitivity to light on waking. We excluded studies that included participants with any corneal dystrophy other than epithelial basement membrane dystrophy and with systemic diseases known to be associated with recurrent corneal erosion, such as epidermolysis bullosa.
Types of interventions
We included studies that compared any of the following types of prophylactic or treatment regimens: ointment (lubricant, tetracycline, hypertonic saline) at night, other topical therapy (topical prednisolone, lubricants), oral tetracycline, anterior stromal puncture, manual debridement, excimer laser ablation and therapeutic contact lenses. We also included studies that compared one of these interventions to no intervention. These regimens were employed to:
-
avert the development of recurrent corneal erosion following traumatic corneal abrasion (prophylactic regimen);
-
prevent the occurrence of further episodes once a diagnosis of recurrent corneal erosion had been made (prophylactic regimen); and
-
treat episodes of recurrent corneal erosion (treatment regimen).
Types of outcome measures
We considered the following outcome measures:
-
resolution of symptoms after treatment (number in total, total number of erosions, time to resolution);
-
recurrence after complete or partial resolution (number in total, time to recurrence, recurrences requiring further treatment);
-
symptoms (pain); and
-
adverse effects (corneal haze, astigmatism).
Outcome 1 was not relevant to the prophylaxis regimen.
Search methods for identification of studies
Electronic searches
The Cochrane Eyes and Vision Information Specialist conducted systematic searches in the following databases for randomised controlled trials and controlled clinical trials. There were no language or publication year restrictions. The date of the search was 14 December 2017.
-
Cochrane Central Register of Controlled Trials (CENTRAL; 2017, Issue 11) (which contains the Cochrane Eyes and Vision Trials Register) in the Cochrane Library (searched 14 December 2017) (Appendix 1).
-
MEDLINE Ovid (1946 to 14 December 2017) (Appendix 2).
-
Embase Ovid (1980 to 14 December 2017) (Appendix 3).
-
LILACS (1982 to 14 December 2017) (Appendix 4).
-
ISRCTN registry (www.isrctn.com/editAdvancedSearch; searched 14 December 2017) (Appendix 5).
-
US National Institutes of Health Ongoing Trials Register ClinicalTrials.gov (www.clinicaltrials.gov; searched 14 December 2017) (Appendix 6).
-
World Health Organization (WHO) International Clinical Trials Registry Platform (ICTRP)(www.who.int/ictrp; searched 14 December 2017) (Appendix 7).
Searching other resources
We used the Science Citation Index to search for studies that cited the studies included in this review. We searched the reference lists of reports of studies that were selected for inclusion. We contacted experts in the field to ask if they were aware of any other relevant published or unpublished studies.
Data collection and analysis
Selection of studies
The review authors independently checked the titles and abstracts identified from the electronic and bibliographic searches and from contact with experts. We obtained the full texts of possibly relevant papers. Each review author assessed the studies according to the inclusion criteria for this review. We resolved disagreements by discussion. We assessed selected studies for methodological quality.
Data extraction and management
The review authors independently extracted data using a form developed by Cochrane Eyes and Vision. We compared the results and resolved discrepancies. We contacted the authors of reports to obtain missing data.
Assessment of risk of bias in included studies
The review authors assessed study quality according to the Cochrane Eyes and Vision Review Development Guidelines based on Chapter 8 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011a). The review authors were not masked to the report authors and study results during the assessment. We resolved disagreements by discussion. We considered four parameters: allocation concealment and method of allocation to treatment (selection bias), masking of participants and examiners (performance bias and detection bias) and exclusions after randomisation and losses to follow‐up (attrition bias). We assessed each parameter of study quality according to the 'Risk of bias' table and judged as 'low risk', 'high risk' or 'unclear risk'. We contacted authors of studies that were unclear on any parameter for clarification of details.
Data synthesis
We calculated outcome measures of effect across studies and expressed the results as risk ratios (RR) and 95% confidence intervals (CI) for dichotomous outcomes and mean difference (MD) and 95% CI for continuous outcomes. We were unable to pool the studies as there was significant clinical heterogeneity between the studies. We have provided a descriptive summary of the results.
'Summary of findings' tables
We selected the three most clinically relevant treatment comparisons for the 'Summary of findings' tables and GRADE assessment. The comparisons selected includes:
-
Therapeutic contact lens versus topical lubrication for the treatment of recurrent corneal erosion syndrome
-
Phototherapeutic keratectomy versus alcohol delamination for the treatment of recurrent corneal erosion syndrome
-
Diamond burr superficial keratectomy (after epithelial debridement) versus sham diamond burr (after epithelial debridement) for the treatment of recurrent corneal erosion syndrome
We included the following outcomes:
-
resolution of symptoms after treatment
-
recurrence after complete or partial resolution
-
time to recurrence
-
recurrences requiring further treatment
-
symptoms (pain score)
-
adverse effects (corneal haze)
-
adverse effects (astigmatism)
We used a two‐author consensus to assess the certainty of the body of evidence in accordance to the five GRADE considerations (study limitations, consistency of effect, imprecision, indirectness, publication bias) (GRADEpro GDT 2015). We justified any decisions to downgrade or upgrade certainty of evidence through explanatory footnotes and highlighted important considerations in the 'Comments' column.
Results
Description of studies
Results of the search
The original electronic search conducted in June 2007, retrieved 1217 titles and abstracts. We obtained the full‐text copies of seven papers of possible relevance (Arbour 1997; Eke 1999; Hope‐Ross 1994; Hykin 1994; Ohman 1998; Williams 1985; Yamada 1998). These described randomised or quasi‐randomised controlled studies comparing therapies for recurrent corneal erosions. One paper was translated into English from Japanese (Yamada 1998). One study (Arbour 1997) randomised and analysed recurrent corneal erosions and traumatic erosions together. We received no response from our letter to the authors requesting subgroup data so this paper was excluded (see Characteristics of excluded studies table). A total of six studies were included in the review (see Characteristics of included studies table).
An update search in June 2012 identified 341 new records. The Cochrane Eyes and Vision Information Specialist scanned the search results and removed 320 records that were not relevant to the scope of the review. We screened the remaining 21 records and rejected a further 16 records as not eligible for inclusion in the review. We obtained full‐text copies of five reports of studies for further investigation. We excluded three studies: one study (Kasparova 2010) did not include the correct patient population and two studies (Yoon 2011; Ziakas 2010) were found not to be randomised trials (see Characteristics of excluded studies table). The studies Hutz 2010 and Wong 2009 met the inclusion criteria and were included in the review (see Characteristics of included studies table).
Updated searches conducted in December 2017 identified 836 new records (Figure 1). After removing 176 duplicates, the Cochrane Information Specialist (CIS) screened the remaining 660 records and removed 616 references that were not relevant to the scope of the review. We screened the remaining 44 records and obtained two full‐text reports of studies for further assessment. We included two studies (Ahad 2013; Chan 2014) that met the inclusion criteria (see Characteristics of included studies). We did not identify any ongoing studies from our searches of the clinical trials registries.

Study flow diagram
Included studies
We have given a summary of the included studies (Ahad 2013; Chan 2014; Eke 1999; Hope‐Ross 1994; Hutz 2010; Hykin 1994; Ohman 1998; Williams 1985; Yamada 1998; Wong 2009) below, and have presented details in the Characteristics of included studies table and a summary in Table 1.
| Study | Treatment/ prophylaxis | Country | No. of participants* | Average age | Age range | Percentage women | Intervention 1 | Intervention 2 | Comparator | Co‐intervention | Duration of treatment | |
| 1 | Treatment | UK | 29 | 39 | 21‐73 | 45% | Therapeutic contact lens Air Optix Night and Day lenses (silicon hydrogel with 24% water, CIBA vision), replaced every 30 days | Topical lubricant carbomer (celluvisc) 0.5% 4 times daily and lacrilube at night | 3 months | |||
| 2 | Treatment | Australia | 33 | 49 | NR | 45% | Phototherapeutic keratectomy epithelium removed with blade, excimer laser treatment (Zyoptix, Bausch and Lomb) | Alcohol delamination epithelium removed with blade, simulated excimer laser | Stat diclofenac (Voltaren Ophthal Eye Drops), chloramphenicol 0.5% (Chlorsig, Sigma Pharmaceuticals), prednisolone phosphate 0.5% (Minims, Bausch and Lomb), postoperative chloramphenicol and fluorometholone and therapeutic contact lens paraffin based lubricating ointment at night for 3 months following treatment participants with persistent or recurring symptoms causing discomfort were offered repeat phototherapeutic keratectomy | 3 months | ||
| 3 | Prophylaxis | UK | 42 | NR | NR | NR | Topical lubrication Lacrilube, Allergan at night | No topical lubrication | Cyclopentolate 1% drops and chloramphenicol ointment | 2 months | ||
| 4 | Treatment | UK | 30 | 45 | 27‐77 | 57% | Oral oxytetracycline 250 mg twice a day and topical prednisolone 0.5% four times a day and daily lid hygiene | Oral oxytetracycline 250 mg twice a day and daily lid hygiene | No oxytetracycline or prednisolone | Simple eye ointment. Macroerosions were treated with a single dose of cyclopentolate 1% and chloramphenicol followed by patching for 24 h and analgesia as required and paraffin (lubricating) ointment at night combined with manual debridement if the epithelium appeared wrinkled | 24 weeks for standard therapy, 12 weeks for tetracycline and 7 days for prednisolone | |
| 5 | Treatment | Germany | 100 | NR but inclusion criteria specified > 20 years | NR but inclusion criteria specified > 20 years | NR | Transepithelial excimer laser ablation (20 pulses of 193 nm) | Subepithelial excimer laser ablation (20 pulses of 193 nm). Subepithelial group also received additional contact bandages postoperatively until re‐epithelialisation | One‐off procedure | |||
| 6 | Prophylaxis study | Prophylaxis | UK | 117 | 38 | 14‐80 | 53% | Topical lubrication paraffin ointment nightly | Control hypertonic saline nightly | 3‐6 months | ||
| 6 | Treatment study | Treatment | Anterior stromal puncture purpose‐ | Therapeutic contact lens hydrogel (80% water content) soft contact lenses, left in situ for 6 weeks | If symptoms not controlled, a partial superficial keratectomy (anterior to Bowman's membrane) was performed. If this failed then the participant was withdrawn from study and total superficial keratectomy considered | 6 weeks | ||||||
| 7 | Treatment | Sweden | 56 | 45 | 21‐75 | 63% | Excimer laser ablation (after epithelial debridement) Summit ExciMed 200 central ablation of 5 microns with diameter of 6.5 mm | No excimer laser ablation (epithelial debridement alone) | Epithelial debridement using a Beaver blade or a sponge. Patch overnight. Antibiotic ointment, chloramphenicol | One‐off procedure followed by topical treatment 3 times per day for 3‐4 days | ||
| 8 | Treatment | UK | 24 | 43 | 22‐60 | 50% | Therapeutic contact lens hydrogel high water content lens (Duragel 75 plano) with chloramphenicol 2 times a day. | Topical lubrication hypromellose drops 4 times a day and paraffin ointment (oculentum simplex) nightly | 8 weeks | |||
| 9 | Treatment | China | 48 | 38 | 20‐70 | 56% | Diamond burr superficial keratectomy (after epithelial debridement) 5.0 mm diamond ball burr to polish denuded corneal surface for 30 seconds | Sham diamond burr superficial keratectomy (after epithelial debridement). Sham procedure performed without contact of corneal surface. | Epithelial debridement: loose epithelium removed using cellulose sponge. Tobramycin ointment (Tobrex; Alcon) and homatropine 4% cycloplegic eyedrops were applied followed by an eye patch overnight. Postoperatively, participants received a regimen of levofloxacin 0.5% (Cravit; Santen, Osaka, Japan) | One‐off procedure and topical treatment over 3‐4 months | ||
| 10 | Yamada 1998 prophylaxis study | Prophylaxis | Japan | 26 | 46 | 21‐71 | 35% | Antibiotic tetracycline ointment | Control hypertonic saline ointment | 6 months if no subjective symptoms, 3 months if no signs | ||
| 10 | treatment study | Treatment | Epithelial debridement | Anterior stromal puncture | Therapeutic contact lens |
NR: not reported
Design
Eight studies were randomised controlled trials (RCTs), seven single‐centre and one‐double centre. Two studies were quasi‐RCTs (allocation by alternation) (Williams 1985; Yamada 1998). The studies, described below, sought to determine measures to prevent further episodes of recurrent erosion, to treat current episodes of recurrent erosion and to avert the development of recurrent erosion following a traumatic corneal erosion. We did not find any studies that compared an intervention to no treatment. We have described the interventions examined in each study briefly here and in greater detail below (see Effects of interventions section).
Participants
Five studies were conducted in the United Kingdom, one in Sweden, one in Germany, one in Japan, one in Hong Kong and one in Australia. The number of participants randomised ranged from 24 to 100. Male and female participants ranged in age from 14 to 80 years; one study did not include data on age and sex (Eke 1999) and we did not receive any reply to a letter written to the study authors requesting this information. Inclusion criteria differed between the studies as did the treatment regimens given prior to the trial. Details on the study populations are given below (see Effects of interventions section). Nine studies included people with a diagnosis of recurrent corneal erosion and one study included people following a traumatic corneal abrasion (Eke 1999).
Risk of bias in included studies
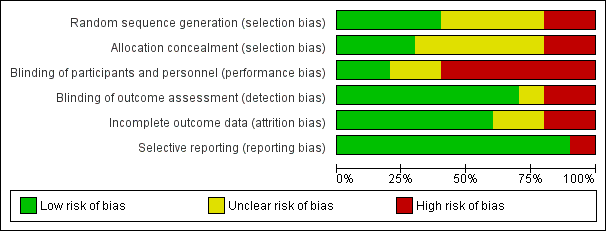
'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Random sequence generation
We assessed two studies as high risk of bias. Williams 1985 and Yamada 1998 used 'alternate patients' as the randomisation method. Four studies reported an acceptable method of generating the random sequence, either random number tables (Hope‐Ross 1994) or computer‐generated (Ahad 2013; Chan 2014; Wong 2009). The other studies did not specify their method of generating the random sequence but they described the participants as being randomly assigned to treatment.
Allocation concealment
We assessed two studies as high risk of bias (Williams 1985; Yamada 1998) as the investigators could foresee allocation of participants with 'alternate' allocation. Three studies reported adequate methods to conceal the allocation (Ahad 2013; Chan 2014; Wong 2009) using sealed, numbered containers (Ahad 2013), independent or masked investigators, or both (Chan 2014; Wong 2009). The risk of selection bias was unclear in all the other studies as insufficient information regarding allocation concealment was provided.
Blinding
Blinding (masking) of participants and personnel
We assessed six studies as high risk of performance bias (Ahad 2013; Chan 2014; Eke 1999; Hope‐Ross 1994; Hykin 1994; Williams 1985). Masking was not possible in Eke 1999 and Hykin 1994 when the groups were given 'ointment' versus 'drops'. Masking was not possible in Ahad 2013 as therapeutic contact lens use was apparent to both participants and personnel. Masking of personnel was not possible in Chan 2014 as one had to administer the phototherapeutic keratectomy. Hope‐Ross 1994 and Williams 1985 did not perform masking. The risk of performance and detection bias was unclear in Ohman 1998 and Yamada 1998 as the trial reports did not explicitly state if masking was performed.
Masking of outcome assessment
All studies but three (Ahad 2013; Chan 2014; Ohman 1998) had low risk of detection bias. Although the masking of outcomes was not necessarily reported in all studies, the outcomes measured were mostly self‐reported symptoms, thus unlikely to be affected by lack of masking of assessment.
Incomplete outcome data
We assessed two studies as high risk of attrition bias. In Chan 2014 there was high loss to follow‐up at 24 months and follow‐up was unequal between groups. In Yamada 1998 there was unequal follow‐up between groups. Two studies (Eke 1999; Hykin 1994) had an unclear risk of attrition bias as insufficent data were provided regarding loss to follow‐up. All other studies were judged to be of low risk of attrition bias as all enrolled participants were accounted for.
Selective reporting
All but one study had low risk of bias. Hutz 2010 did not report patient symptoms post‐treatment. Patient symptoms are a major outcome measure for the management of recurrent corneal erosions.
Effects of interventions
See: Summary of findings for the main comparison Therapeutic contact lens versus topical lubrication for the treatment of recurrent corneal erosion syndrome; Summary of findings 2 Phototherapeutic keratectomy versus alcohol delamination for the treatment of recurrent corneal erosion syndrome; Summary of findings 3 Diamond burr superficial keratectomy (after epithelial debridement) versus sham diamond burr (after epithelial debridement) for the treatment of recurrent corneal erosion syndrome
Treatment of recurrent corneal erosion syndrome
We have covered the following eight comparisons in this section and we have prepared 'Summary of findings' tables and assessed the three most clinically relevant comparisons using GRADE.
-
Therapeutic contact lens versus topical lubrication (Ahad 2013; Williams 1985;summary of findings Table for the main comparison)
-
Phototherapeutic keratectomy (after epithelial debridement) versus alcohol delamination and sham excimer laser (after epithelial debridement) (Chan 2014; summary of findings Table 2)
-
Diamond burr superficial keratectomy (after epithelial debridement) versus sham diamond burr (after epithelial debridement) (Wong 2009; summary of findings Table 3)
-
Transepithelial versus subepithelial excimer laser ablation (Hutz 2010)
-
Excimer laser ablation (after epithelial debridement) versus no excimer laser ablation (after epithelial debridement) (Ohman 1998)
-
Epithelial debridement versus anterior stromal puncture (Yamada 1998)
-
Anterior stromal puncture versus therapeutic contact lens (Hykin 1994)
-
Oral oxytetracycline and topical prednisolone (in addition to 'standard therapy') versus oral oxytetracycline (in addition to 'standard therapy') versus 'standard therapy' (Hope‐Ross 1994)
1. Therapeutic contact lens versus topical lubrication
summary of findings Table for the main comparison
Two studies addressed this comparison. Williams 1985 included 31 participants with recurrent corneal erosion from map‐dot‐fingerprint (epithelial basement membrane) dystrophy who had received no previous treatment other than topical therapy, presenting to the Casualty Department, Moorfields Eye Hospital, United Kingdom. Participants were excluded if they wore contact lenses. Ahad 2013 included 29 participants with recurrent corneal erosions and who had not "undergone any treatment other than lubricants or antibiotics…in previous episodes". Participants were recruited from the Royal Berkshire Hospital and Oxford Eye Hospital, UK. Exclusion criteria included ocular surface disease, refractive surgery and history of corneal infection or surgery.
In Ahad 2013 the therapeutic contact lens was Air Optix Night and Day (CIBA Vision) and they compared this to topical lubrication with Celluvisc and Lacri‐Lube ointment. Co‐intervention with chloramphenicol eye drops was given to all participants with macroerosions or epithelial defects. Williams 1985 compared a 14 mm Duragel 75 therapeutic contact lens (high water‐content hydrogel lens) with hypromellose drops and paraffin ointment at night. This contact lens type has since been superseded for therapeutic use by newer lens designs (such as silicone hydrogel lens and collagen shields).
Resolution of symptoms after treatment
Ahad 2013 found a comparable proportion of participants achieved complete resolution after treatment between the therapeutic contact lens (10/14) and topical lubrication (11/15) groups at four months (RR 0.97, 95% confidence interval (CI) 0.62 to 1.53; Analysis 1.1). ‘Resolution’ included both subjective symptom reporting and objective slit‐lamp ocular findings. Williams 1985 did not report this outcome. We judged this low‐certainty evidence, downgrading for imprecision and risk of bias.
Total number of erosions after treatment
Neither study reported this outcome.
Time to resolution of symptoms
Ahad 2013 reported a faster time to resolution in the therapeutic contact lens group versus the topical lubrication group (5 weeks versus 9 weeks, P = 0.02).
Recurrences after complete or partial resolution
Ahad 2013 reported that one participant (7.1%) in the contact lens group and one participant (6.7%) in the topical lubrication group developed recurrence after complete or partial resolution at seven‐month follow‐up (RR 1.07, 95% CI 0.07 to 15.54; Analysis 1.1). Williams 1985 did not report this outcome. We judged this very low‐certainty evidence downgrading one level for limitations in design due to study personnel not being masked and downgrading two levels for imprecision due to the small number of events.
Time to recurrence
Neither study reported this outcome.
Recurrences requiring further treatment
Ahad 2013 did not state explicitly whether participants with recurrences after complete resolution (one per group) required further treatment although they stated they were minor symptoms of recurrent corneal erosions with no obvious macroerosions. Williams 1985 did not report this outcome.
Symptoms (pain score)
Ahad 2013 used a visual analogue scale to grade pain postintervention at one month intervals for three months. The study reported no difference in pain scores between the groups at all measured time intervals but did not provide standard deviations or details regarding the pain scale. At three months, people in the therapeutic contact lens group had an average reported pain score of 3 and people in the topical lubrication group of 2. Williams 1985 reported that more participants in the therapeutic contact lens group (8/11) had pain symptoms compared to the topical lubrication group (3/13) at eight weeks' follow‐up (RR 3.15, 95% CI 1.10 to 9.06; Analysis 1.3). This evidence is of low certainty, downgraded for limitation in design due to lack of masking and imprecision due to small sample size.
Adverse effects (corneal haze, astigmatism)
Ahad 2013 reported that, "none of the participants in the therapeutic contact lens group developed any complications". Development of any adverse effects in the topical lubrication group was not stated explicitly. Williams 1985 reported a significantly higher rate of ocular complications in the therapeutic contact lens group compared to the topical lubrication group. In the contact lens group, three participants had extensive epithelial loss under the contact lens (two of these participants abandoned the lens); this complication is associated with the type of contact lens used and is not seen in newer lenses with higher oxygen transmission. Contact lens treatment failed in four participants as they frequently lost the lens and it had to be replaced.
2. Phototherapeutic keratectomy (after epithelial debridement) versus alcohol delamination and sham excimer laser (after epithelial debridement)
Chan 2014 recruited 33 participants presenting with symptomatic recurrent corneal erosions not responding to conservative treatment (topical lubricants and a therapeutic contact lens) at the Royal Victorian Eye and Ear Hospital, Melbourne Australia. Participants were excluded if they had had previous ocular surgery, prior treatment for recurrent corneal erosion other than manual epithelial debridement, a history of corneal or external eye disorders, corneal hypoaesthesia or diabetes mellitus.
The study compared phototherapeutic keratectomy (excimer laser ablation) versus alcohol delamination. Postoperatively diclofenac, chloramphenicol, prednisolone, therapeutic contact lens and paraffin based lubricating ointment were given to all participants.
Resolution of symptoms after treatment
Chan 2014 reported complete resolution of symptoms in six of 16 of the phototherapeutic keratopathy group and 10 of 17 participants receiving alcohol delamination (RR 0.64, 95% CI 0.30 to 1.35; Analysis 2.1). ‘Improvement’ was judged symptomatically without ocular findings stated explicitly. We judged this to be low‐certainty evidence, downgrading for risk of bias and imprecision.
Total number of erosions after treatment
Chan 2014 did not explicitly report the total number of erosions after treatment.
Time to resolution of symptoms
Chan 2014 did not report the time to resolution of symptoms.
Recurrences after complete or partial resolution
Six participants (37.5%) in the phototherapeutic keratectomy group and five participants (29.4%) in the alcohol delamination group developed recurrence after complete or partial resolution at 24‐month follow‐up. This finding was not statistically significant (RR 1.27, 95% CI 0.48 to 3.37; Analysis 2.2) and is of low certainty given limitations in design due to lack of masking and imprecision due to small sample size.
Time to recurrence
Chan 2014 reported a similar time to recurrence after complete or partial resolution of 6.5 months (range 3 to 12 months) and 6 months (range 3 to 12 months) in the phototherapeutic keratectomy and alcohol delamination groups respectively. This difference was not statistically significant (P = 0.85). The evidence is of low certainty given limitations in design due to lack of masking and imprecision due to small sample size.
Recurrences requiring further treatment
Chan 2014 reported that two participants with recurrence in the phototherapeutic keratectomy group underwent repeat phototherapeutic keratectomy that achieved resolution. In the alcohol delamination group, three people with recurrence subsequently underwent phototherapeutic keratectomy, of whom one was lost to follow‐up, one had symptom improvement and one had symptom resolution. This finding was of very low certainty given limitations in design due to lack of masking and imprecision due to very small numbers (RR 0.71, 95% 0.14 to 3.70; Analysis 2.4).
Symptoms (pain score)
Chan 2014 scored pain using a numerical scale and demonstrated lower pain scores (less pain) in the phototherapeutic keratectomy group compared to the alcohol delamination group at 24‐month follow‐up (MD ‐0.7, 95% CI ‐2.23 to 0.83; Analysis 2.3). The evidence is of low certainty given limitations in design due to lack of masking and imprecision due to small sample size.
Adverse effects (corneal haze, astigmatism)
Chan 2014 reported no cases of corneal haze at the 12‐month time point in either group. The evidence is of very low certainty given limitations in design due to lack of masking and imprecision due to a small sample size where event rate could not be estimated.
3. Diamond burr superficial keratectomy (after epithelial debridement) versus sham diamond burr (after epithelial debridement)
Wong 2009 recruited 48 participants from Hong Kong Eye Hospital who had recurrent corneal erosions secondary to trauma or anterior basement membrane dystrophy with more than one episode of corneal erosion within the past month, or with symptoms affecting activities of daily living. Participants with corneal dystrophies other than anterior basement membrane dystrophy were excluded.
All participants had epithelial debridement whereby loose epithelium was removed using a cellulose sponge. In the diamond burr group, the denuded area was "gently and evenly polished" with a diamond burr with a 5.0 mm ball. In the comparator group, the diamond burr was switched on but did not touch the cornea. All participants received levofloxacin 0.5% for one week and topical lubrication (Viscotears) tapered over three to four months.
Resolution of symptoms after treatment
Wong 2009 did not report this outcome.
Total number of erosions after treatment
Wong 2009 did not report this outcome.
Time to resolution of symptoms
Wong 2009 did not report this outcome.
Recurrences after complete or partial resolution
One participant (4%) in the diamond burr superficial keratectomy group and 13 participants (56.6%) in the sham diamond burr group developed recurrence after complete or partial resolution at six‐month follow‐up. This finding suggests recurrences were less common in the diamond burr superficial keratectomy group (RR 0.07, 95% CI 0.01 to 0.50; Analysis 3.1). This evidence is of moderate certainty, downgraded for imprecision as it is based on small numbers (one event in the intervention group).
Time to recurrence
Wong 2009 reported that time to recurrence was prolonged in the diamond burr superficial keratectomy group compared to the sham diamond burr group (6.0 versus 2.4 months, 95% CI not provided). This result was of low certainty given imprecision from a small sample size (only one recurrence in the diamond burr group).
Recurrences requiring further treatment
Wong 2009 did not report the number of recurrences requiring further treatment.
Symptoms (pain score)
The study authors did not report pain symptoms in the participants.
Wong 2009 reported lesser minor symptom recurrence (self‐limiting, not requiring ophthalmological consultation) in the diamond burr‐polishing group compared with sham diamond burr group at six months' follow‐up (20% versus 65%). Major symptoms requiring ophthalmological consultation occurred more commonly in the epithelial debridement group compared to the diamond burr‐polishing group (57% versus 4%).
Adverse effects (corneal haze, astigmatism)
Wong 2009 reported one participant with corneal haze at six months in each of the diamond burr superficial keratectomy (4%) and sham diamond burr group (4.3%) (RR 0.92, 95% CI 0.06 to 13.87; Analysis 3.2) and was of low certainty given imprecision due to small sample size and wide confidence interval.
The mean astigmatism was 0.44 and 0.88 dioptres in the diamond burr superficial keratectomy and sham diamond burr groups respectively. We could not estimate the significance and the finding is of moderate certainty given imprecision due to small sample size.
4. Transepithelial versus subepithelial excimer laser ablation
Hutz 2010 included 100 participants with recurrent corneal erosions occurring "at least three times per year" and with the first occurrence of the erosion being of "traumatic origin". Participants were recruited from several centres in Germany by "transferring physicians". The study was conducted in one location.
Transepithelial versus subepithelial technique of excimer laser ablation (20 pulses of 193 nm). Ofloxacin was given to both groups postoperatively but only the subepithelial group had their eyelids closed "underneath bandages" until re‐epithelialisation. None of the participants received steroid eye drops during the study (Hutz 2010).
Resolution of symptoms after treatment
This outcome was not reported.
Total number of erosions after treatment
This outcome was not reported.
Time to resolution of symptoms
This outcome was not reported.
Recurrences after complete or partial resolution
This outcome was not reported.
Time to recurrence
This outcome was not reported.
Recurrences requiring further treatment
Hutz 2010 had seven of 50 participants with recurrent corneal erosion in both groups at four‐week follow‐up after excimer laser ablation. These participants were excluded from follow‐up at 52 weeks. At 52‐week follow‐up, 12 of 43 and 10 of 43 participants developed recurrent corneal erosions in the transepithelial and subepithelial groups, respectively (RR 1.20, 95% CI 0.58 to 2.48; Analysis 4.1). It was stated that the recurrences were "subsequently treated".
Symptoms (pain score)
Hutz 2010 reported only risks of occurrence of recurrent corneal erosions, which were similar in both groups (24% versus 20% at 52 weeks). Symptoms were not explicitly stated.
Adverse effects
This outcome was not reported.
5. Excimer laser (after epithelial debridement) versus no excimer laser (after epithelial debridement)
Ohman 1998 included 56 participants from St Erik Eye Hospital, Stockholm, Sweden who had had symptoms of recurrent corneal erosion for longer than three months, some of whom had already been treated with ointment and patching and in some cases manual debridement.
The study compared epithelial debridement followed by excimer laser and an eye patch overnight versus epithelial debridement and an eye patch overnight alone.
Resolution of symptoms after treatment
Ohman 1998 did not explicitly report resolution of symptoms after treatment.
Total number of erosions after treatment
This outcome was not reported.
Time to resolution of symptoms
This outcome was not reported.
Recurrences after complete or partial resolution
Ohman 1998 found two erosion recurrences in 28 participants in the excimer laser ablation plus debridement group compared to 16 in 28 participants in the debridement‐alone group (RR 0.13, 95% CI 0.03 to 0.51). Of the 16 participants in the control group with recurrence, three did not want treatment and 13 accepted treatment with excimer laser ablation.
Time to recurrence
This outcome was not reported.
Recurrences requiring further treatment
Ohman 1998 had 2 of 25 (8%) participants with recurrent corneal erosion after excimer laser ablation; these participants did not receive further treatment as their remaining symptoms were acceptable. After epithelial debridement alone, 16 of 26 (62%) participants had recurrent erosions; of these, three did not want treatment and 13 accepted treatment with laser ablation (RR 0.13, 95% CI 0.03 to 0.51; Analysis 5.1).
Symptoms (pain score)
Ohman 1998 reported that 24 of 26 (92%) of participants given epithelial debridement followed by excimer laser had much improved or no symptoms compared with 9 of 25 (36%) of participants given epithelial debridement alone (RR 2.56, 95% CI 1.50 to 4.38; Analysis 5.2).
Adverse effects
Ohman 1998 stated that there was no change in their adverse effect outcomes (visual acuity, intraocular pressure and refraction) though slight subepithelial haze was seen in treatment and control groups at three and six months but not afterwards.
6. Epithelial debridement versus anterior stromal puncture
Yamada 1998 fitted a therapeutic contact lens for people whose prophylactic regimen had failed, and if this was not successful, the participants were to be randomised into a treatment arm. Participants were recruited from a single centre in Japan. Three participants (two using hypertonic saline and one using tetracycline ointment) required further treatment with a therapeutic contact lens (non‐randomised). The use of the therapeutic contact lens cured one participant only. The other two participants stopped contact lens wear, one as they had a relapse and the other as they required frequent lens replacement. Anterior stromal puncture was not performed for these two participants as cure was achieved by a change in ointment. Therefore no participants were randomised into their treatment am.
Epithelial debridement versus anterior stromal puncture (Yamada 1998).
In the study conducted by Yamada 1998, if prophylactic therapy failed, participants were given a hydrogel (80% water content) therapeutic contact lens (not randomised) and if this was not successful they were then randomised to receive one of two treatments.
7. Anterior stromal puncture versus therapeutic contact lens
Hykin 1994, in the treatment arm of their trial, included participants presenting to Moorfields Eye Hospital, UK with an acute episode of recurrent corneal erosion where the erosion was off the visual axis and had not resolved in five days with topical chloramphenicol ointment, cycloplegia and patching. Only one participant met these criteria.
The study compared therapeutic contact lens (hydrogel lens with 80% water content) versus anterior stromal puncture (Hykin 1994).
Recurrences requiring further treatment
Hykin 1994 had five participants requiring further treatment. Four were fitted with a contact lens and one person was excluded as they developed an anterior stromal infiltrate that was presumed to be infectious but was culture‐negative. Symptomatic control was achieved with a contact lens except for one participant who required a superficial keratectomy and then anterior stromal puncture resulting in almost complete abolition of their symptoms.
Symptoms (pain score)
Hykin 1994 treated four of 82 participants (5%) with a contact lens (five instances, non‐randomised). In one participant (two eyes) the symptoms were not controlled and abrasion of the cornea with a Bard Parker blade was performed with symptom control. Anterior stromal puncture was performed in one participant and achieved symptom control.
Adverse effects
Hykin 1994 reported no complications in the one participant who had anterior stromal puncture, and in the five eyes fitted with a contact lens. However, one participant with an acute episode of recurrent erosion developed an anterior stromal infiltrate that was presumed to be microbial keratitis (culture‐negative but resolution on topical antibiotic therapy); this is an uncommon complication of recurrent corneal erosion.
Total number of erosions after treatment
Hykin 1994 did not report the total number of erosions after treatment.
8. Oral oxytetracycline and topical prednisolone (in addition to 'standard therapy') versus oral oxytetracycline (in addition to 'standard therapy') versus 'standard therapy'
Hope‐Ross 1994 included 30 participants with 'recalcitrant recurrent corneal erosion'; this was defined as participants with recurrent corneal erosion who had not responded to standard therapy. Over 80% of their participants had evidence of meibomian gland dysfunction. Participants were recruited from Birmingham and Midlands Eye Hospital, UK.
The study compared standard therapy alone (preservative‐free cyclopentolate and chloramphenicol drops and paraffin (lubricating) ointment at night combined with manual debridement if the epithelium appeared wrinkled) versus oral tetracycline 250 mg twice daily for 12 weeks and lid hygiene plus standard therapy; and versus topical prednisolone 0.5% four times daily for one week, oral tetracycline 250 mg twice daily for 12 weeks and lid hygiene plus standard therapy (Hope‐Ross 1994).
Resolution of symptoms after treatment
This outcome was not reported.
Total number of erosions after treatment
Hope‐Ross 1994 found a significant reduction in the total number of macroerosions with standard therapy plus oral tetracycline (two erosions for 10 participants, P = 0.04) and standard therapy, oral tetracycline and topical prednisolone (three erosions for 10 participants, P = 0.0003) but not for those on standard therapy alone (11 erosions for 10 participants, P = 0.66) using repeated measures analysis of variance over the 24‐week study period.
Time to resolution of symptoms
This outcome was not reported.
Recurrences after complete or partial resolution
This outcome was not reported.
Time to recurrence
This outcome was not reported.
Recurrences which required further treatment
Hope‐Ross 1994 reported an acceleration in healing rate from enrolment to study completion in participants on standard therapy plus oral tetracycline and those on standard therapy, oral tetracycline and topical prednisolone over the 24‐week study period. No acceleration in healing rate was found for those on standard therapy alone. The acceleration in healing rate was significantly different when participants receiving standard therapy plus oral tetracycline were compared to those on standard therapy alone (P = 0.001) and for those on standard therapy, oral tetracycline and topical prednisolone compared to standard treatment alone (P = 0.001). There was no difference in the accelerated healing rate when those on standard therapy plus oral tetracycline were compared to the group receiving standard therapy, oral tetracycline and topical prednisolone (P = 0.07). No participants required further treatment (epithelial debridement) during the study.
Symptoms (pain score)
Hope‐Ross 1994 used a visual analogue scale to grade the severity of three symptoms (pain, light sensitivity and watering). They found a statistically significant decrease in symptom scores for participants receiving standard therapy plus oral tetracycline (P = 0.005) and standard therapy, oral tetracycline and topical prednisolone (P = 0.005) but not for those on standard therapy alone (P = 0.15) using repeated measures analysis of variance over the 24‐week study period.
Adverse effects
Hope‐Ross 1994 reported two participants with altered bowel habit after starting oral tetracycline therapy. They did not specify ocular adverse effects.
Prophylactic regimen to avert the development of recurrent corneal erosion
Topical lubrication (combined with 'standard therapy') versus no topical lubrication ('standard therapy alone').
One study examined a regimen to avert the development of recurrent corneal erosion following a traumatic corneal abrasion (Eke 1999). Participants with a traumatic corneal abrasion (following a fingernail injury) were recruited from the Eye Casualty Unit at the Royal Leicester Infirmary, UK. Topical lubrication nightly for two months combined with standard therapy (cyclopentolate drops and chloramphenicol ointment but no eye pad for five days) was compared with standard therapy alone.
Development of recurrent corneal erosions
At three months, on telephone interview, 28% of participants reported mostly mild ('non‐disabling') symptoms consistent with recurrent corneal erosion but only one person (in the control group) developed a confirmed macroform recurrent corneal erosion (RR 0.30, 95% CI 0.01 to 7.07; Analysis 6.1). There were more participants in the topical lubrication group who developed moderate (RR 3.64, 95% CI 0.44 to 29.87; Analysis 6.1) or mild and moderate symptoms (RR 3.33, 95% CI 1.08 to 10.26; Analysis 6.1) of recurrent corneal erosion at three months compared to the control group that received standard therapy alone. At two years, on review of the case notes, two of 42 participants had presented back to the study centre with recurrent corneal erosion, one in the treatment group and one in the control (RR 0.91, 95% CI 0.06 to 13.59; Analysis 6.2).
Time to recurrence
This outcome was not reported.
Recurrences which required further treatment
This outcome was not reported
Symptoms (pain score)
This outcome was not reported.
Adverse effects
No adverse effects were reported.
Prophylactic regimens to prevent further episodes of recurrent corneal erosion
The studies conducted by Hykin 1994 and Yamada 1998 each had a 'prophylactic arm' that examined measures to prevent further episodes of recurrent corneal erosion once recurrent corneal erosion had been diagnosed.
Paraffin versus hypertonic saline
Hykin 1994 included in their prophylactic arm 98 participants with recurrent corneal erosion who had chronic symptoms (including those whose treatment had failed) and participants with an acute episode that resolved within five days after treatment with topical chloramphenicol ointment, cycloplegia and patching. Hykin 1994 compared paraffin ointment to hypertonic saline ointment at night.
Total number of erosions after treatment
This outcome was not reported.
Recurrences that a) improved and b) required further treatment
Hykin 1994 reported that 78 of 82 participants (95%) presenting with an acute episode of recurrent corneal erosion (prior to randomisation into the trial) were successfully treated with patching, cycloplegia and topical antibiotic ointment. Participants with resolved acute and chronic erosions were randomised into the prophylactic arm. In this arm, prophylactic treatment with paraffin or hypertonic saline ointment failed in five of 98 participants, as their symptoms were unacceptable or they had any acute erosion. The participants whose treatment of their acute episode was unsuccessful and those whose prophylactic measures had failed, entered the treatment arm of the trial. Four years after this study 94 of the 117 participants (80%) were surveyed; 55 participants (59%) were still symptomatic, with episodes of recurrent erosion occurring at least weekly in 24% and monthly in 51%. Participants with epithelial membrane dystrophy were more likely to be using topical lubricants than the trauma group (P = 0.02) (Heyworth 1998).
Symptoms
Hykin 1994 reported that there was no difference in the effectiveness of the two ointments (paraffin and hypertonic saline) as prophylactic agents in their ability to control or abolish symptoms. Participants with epithelial basement membrane dystrophy had an increased risk of prophylactic failure in both groups (risk ratio 10.77) and required further treatment.
Adverse effects
This outcome was not reported.
Tetracycline ointment versus hypertonic saline
Yamada 1998 included 23 participants with recurrent corneal erosion and compared tetracycline ointment to hypertonic saline at night.
Total number of erosions after treatment
This outcome was not reported.
Recurrences that a) improved and b) required further treatment
Yamada 1998 reported that the objective signs of recurrent erosion disappeared for 6 of 10 participants given prophylaxis with hypertonic saline ointment and for 11 of 13 participants treated with tetracycline ointment (no statistical difference) (OR 3.67, 95% CI 0.51 to 26.22).
Time to recurrence
Yamada 1998 found no difference between tetracycline ointment and hypertonic saline ointment (mean 5.6 versus 5.7 months; MD ‐0.10, 95% CI ‐2.82 to 2.62) in the time to resolution of the objective signs of recurrent corneal erosion.
Symptoms
Yamada 1998 reported that 8 of 10 participants receiving hypertonic saline ointment and 12 of 13 receiving tetracycline ointment were "cured"; that is, they did not have symptoms and a relapse of corneal erosion for more than three months (OR 3.00, 95% 0.23 to 38.87).
Adverse effects
This outcome was not reported.
Discussion
Summary of main results
The majority of acute episodes of recurrent corneal erosion can be treated with simple medical (standard) therapy (Hykin 1994). Following resolution of an episode of recurrent erosion there is no firm evidence from the studies to suggest the best prophylactic regimen in people with recurrent corneal erosion. There was no difference in the prophylactic effect of tetracycline ointment and hypertonic saline ointment (Yamada 1998) or between paraffin (lubricating) ointment and hypertonic saline ointment (Hykin 1994). Indeed, despite prophylaxis with ointment many participants may continue to suffer with symptoms of recurrent erosion and require ongoing therapy (Eke 1999). Current clinical practice is to treat an episode of recurrent corneal erosion with antibiotic or lubricating ointment or drops, or a combination of some or all of these, which may be continued once the episode has resolved to prevent further episodes of recurrent corneal erosion. Diamond burr polishing has been shown to reduce episodes of recurrent corneal erosions compared to epithelial debridement (Wong 2009). Comparison between alcohol delamination and phototherapeutic keratectomy showed no difference in resolution or recurrence rates (Chan 2014).
For averting the development of recurrent corneal erosion following a traumatic corneal abrasion due to a fingernail injury, lubricating ointment at night for two months in addition to standard treatment (cyclopentolate drops, then chloramphenicol ointment for five days) led to increased development of the symptoms of recurrent corneal erosion at three months compared to standard therapy alone (Eke 1999). This was the only included study to examine measures to avert the development of recurrent corneal erosion following traumatic corneal abrasion; clearly more studies are needed. It is common practice to treat a traumatic corneal abrasion with antibiotic and/or lubricating ointment, however, such therapy is not always continued for months.
Adverse effects for these treatments were limited. An early study reported that excimer laser did not change the vision, intraocular pressure or refraction (Ohman 1998). However, hyperopic shift (Hutz 2010) and self‐resolving subepithelial haze (Chan 2014) have been reported with a subepithelial excimer laser ablation technique for recurrent erosion. Diamond burr polishing can cause astigmatism, although the rate of this complication was less than for epithelial debridement (Wong 2009). Oral tetracyclines disturbed the gastrointestinal system in two participants (Hope‐Ross 1994) and therapeutic contact lens wear was complicated by loss of the epithelium or contact lens, or both (Williams 1985). Newer lens styles may avoid such complications (Ahad 2013). The number of participants treated in the studies by anterior stromal puncture or superficial keratectomy was too small for conclusions to be reached on the effectiveness and adverse effects of these treatments (Chan 2014; Hykin 1994; Yamada 1998).
Overall completeness and applicability of evidence
The limited evidence from the studies suggests that the symptoms and signs of recurrent corneal erosion may be reduced or controlled by one of the following treatments: the addition of oral tetracycline 250 mg twice daily for 12 weeks or topical prednisolone 0.5% four times daily for one week, or both, to standard treatment (preservative‐free cyclopentolate and chloramphenicol drops, and paraffin (lubricating) ointment at night combined with manual debridement of loose epithelium) (Hope‐Ross 1994); or excimer laser ablation alone (Chan 2014; Hutz 2010) or in addition to mechanical debridement (Ohman 1998). However, participants in Hope‐Ross 1994 had a high rate of meibomian gland dysfunction (Hope‐Ross 1994a); oral tetracyclines and topical prednisolone may have improved this condition rather than recurrent corneal erosion. Although a previous study found that therapeutic contact lenses were inferior to lubricants and had a high complication rate (Williams 1985), newer lenses with higher oxygen transmission are now available. Indeed newer generation contact lenses are currently used to treat some episodes of recurrent corneal erosion that do not respond to medical therapy and to prevent further episodes and this is supported by new data that suggest non‐inferiority and reduced complications (Ahad 2013).
For recurrent erosion it is difficult to assess accurately on examination the number of erosions a person may have had after treatment, as erosions typically resolve quickly and therefore may be missed if the person is examined only at fixed intervals. Patient history (symptoms) may provide a more accurate measure of the number of erosions experienced by a patient. However, the studies we examined measured a variety of symptoms in different ways, and no study used a validated instrument for their measurement. Non‐validated assessments are open to bias and ambiguity. Future studies should use standardised and validated measures to assess participants' symptoms in order to provide an appropriate outcome measure for studies of recurrent corneal erosion. The examiner and participants should be masked, though for studies of therapeutic contact lens wear, patching and ointment use this may not be possible for participants. Appropriate safety information is also essential when selecting treatments. Standardised ocular and, if appropriate, systemic adverse effects should be explicitly collected and stated by all studies to allow treatment success to be weighed against the risks. The studies assessed in this review do, however, highlight regimens that are in use for recurrent erosion or its prevention and may provide the direction for future studies. Future studies of recurrent corneal erosion should standardise inclusion and exclusion criteria, improve the allocation process, ensure masking of participants and examiners where possible, use validated outcome measures, define standard therapy and, like the current studies, ensure there are no significant losses to follow‐up.
Quality of the evidence
The included studies were heterogeneous and possibly of poor quality. In particular, inclusion criteria were variable, allocation concealment was inadequate and therefore a source of potential bias, masking was unclear and outcome measures were not validated. We made attempts to contact the study authors to clarify issues regarding the possibility of allocation, performance, detection and attrition bias in these studies. However, we received no response from them. Three of the seven studies were published prior to publication of the CONSORT statement in 1996 and this may account for their variable quality. The variability and inadequacies of these studies meant that it was not appropriate to directly compare the studies; thus, it could not be determined if one prophylaxis or treatment regimen was superior to another or to no treatment. Indeed, the treatment regimens examined in the studies are all utilised in current clinical practice, reflecting the lack of firm evidence for the efficacy or adverse effects of any treatment. The one study that examined a regimen to avert the development of recurrent corneal erosion following traumatic corneal abrasion was of poor quality and did not provide firm evidence for the development of clinical guidelines.
Two additional studies included in this update, Ahad 2013 and Chan 2014, showed substantially superior quality in their assessment of bias when judged using current standards. However, the fact that we have included only two additional studies since the last update highlights the difficulty in performing randomised controlled studies for recurrent corneal erosion. Improved collaboration, such as the establishment of an international working group, may be needed to improve the quality of evidence to guide the management of recurrent corneal erosion.
Potential biases in the review process
We carefully adhered to the study protocol according to the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011b), thus minimising any potential bias that may arise in the review process.
Agreements and disagreements with other studies or reviews
Other reviews have often included non‐randomised trials and focused on different treatment modalities without substantial evidence on the balance of efficacy and adverse effects data. It is difficult to compare opinions with different reviews as the scopes of the reviews are often different.

Study flow diagram

'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.
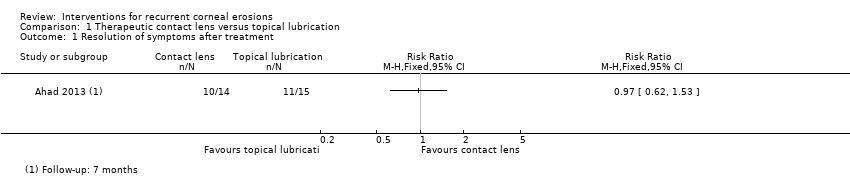
Comparison 1 Therapeutic contact lens versus topical lubrication, Outcome 1 Resolution of symptoms after treatment.

Comparison 1 Therapeutic contact lens versus topical lubrication, Outcome 2 Recurrence after partial or complete resolution.

Comparison 1 Therapeutic contact lens versus topical lubrication, Outcome 3 Pain.

Comparison 2 Phototherapeutic keratectomy (PTK) versus alcohol delamination (ALD), Outcome 1 Resolution of symptoms after treatment.
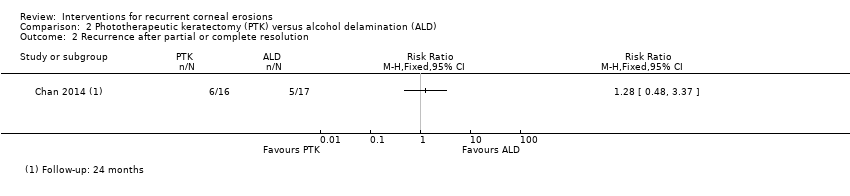
Comparison 2 Phototherapeutic keratectomy (PTK) versus alcohol delamination (ALD), Outcome 2 Recurrence after partial or complete resolution.
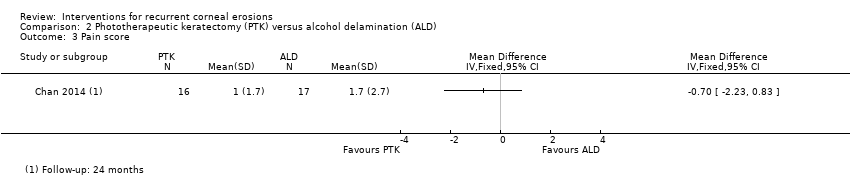
Comparison 2 Phototherapeutic keratectomy (PTK) versus alcohol delamination (ALD), Outcome 3 Pain score.

Comparison 2 Phototherapeutic keratectomy (PTK) versus alcohol delamination (ALD), Outcome 4 Recurrence requiring further treatment.

Comparison 3 Diamond burr superficial keratectomy versus epithelial debridement, Outcome 1 Recurrence after partial or complete resolution.
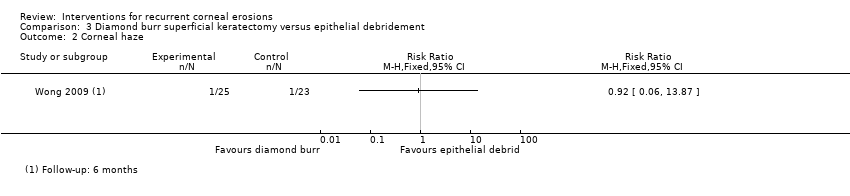
Comparison 3 Diamond burr superficial keratectomy versus epithelial debridement, Outcome 2 Corneal haze.
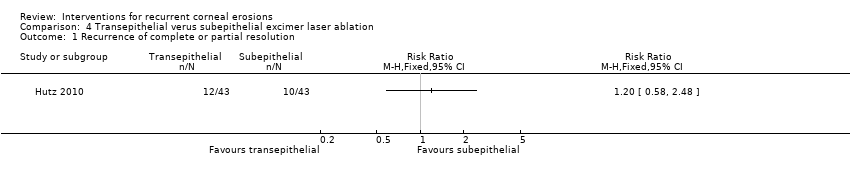
Comparison 4 Transepithelial verus subepithelial excimer laser ablation, Outcome 1 Recurrence of complete or partial resolution.
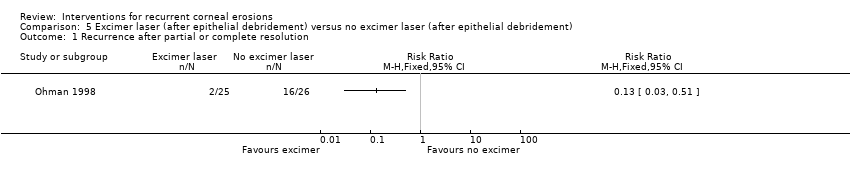
Comparison 5 Excimer laser (after epithelial debridement) versus no excimer laser (after epithelial debridement), Outcome 1 Recurrence after partial or complete resolution.

Comparison 5 Excimer laser (after epithelial debridement) versus no excimer laser (after epithelial debridement), Outcome 2 Symptoms (pain score).

Comparison 5 Excimer laser (after epithelial debridement) versus no excimer laser (after epithelial debridement), Outcome 3 Recurrences requiring further treatment.
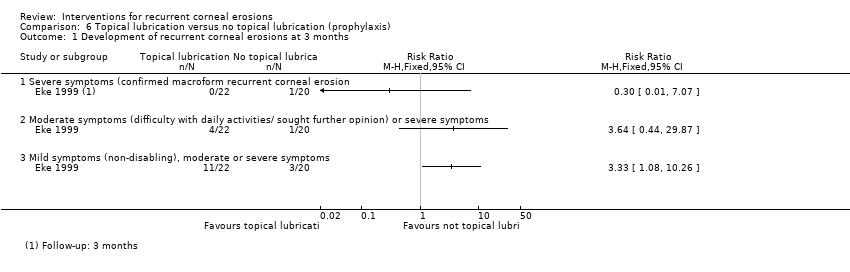
Comparison 6 Topical lubrication versus no topical lubrication (prophylaxis), Outcome 1 Development of recurrent corneal erosions at 3 months.

Comparison 6 Topical lubrication versus no topical lubrication (prophylaxis), Outcome 2 Development of recurrent corneal erosions at 3 months.
| Therapeutic contact lens versus topical lubrication | ||||||
| Patient or population: people with recurrent corneal erosion syndrome without previous surgical intervention Settings: outpatient Intervention: therapeutic contact lens Comparison: topical lubrication | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Certainty of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Topical lubrication | Therapeutic contact lens | |||||
| Resolution of symptoms after treatment Follow‐up: 4 months | 730 per 1000 | 708 per 1000 (453 to 1000) | RR 0.97 (0.62 to 1.53) | 29 participants (1 study) | ⊕⊕⊝⊝ | |
| Recurrence after complete or partial resolution Follow‐up: 7 months | 67 per 1000 | 72 per 1000 (0 to 1000) | RR 1.07 (0.07 to 15.54) | 29 participants (1 study) | ⊕⊝⊝⊝ | Single study only followed up participants with complete resolution to screen for recurrence |
| Time to recurrence | Outcome not reported for this comparison | |||||
| Recurrences requiring further treatment | See comment | ‐ | ‐ | ‐ | ‐ | Neither study reported this outcome but one study stated that the two recurrences were minor symptoms with no obvious macroerosions. |
| Symptoms (pain score) Follow‐up: 3 months (higher score indicates more pain, unclear range of scale but probably 0 to 10) | Mean pain score with topical lubrication was 2 | Mean pain score with therapeutic contact lens was 1 higher (worse) | ‐ | 29 participants (1 study) | ⊕⊕⊝⊝ | Visual analogue scale range not specified, standard deviations not reported One other study of 24 participants reported more pain in contact lens group (RR 3.15, 95% CI 1.10, 9.06) but contact lens used is no longer in common use |
| Adverse effects: corneal haze | See comment | ‐ | ‐ | ‐ | ⊕⊝⊝⊝ | The more recent study did not report this outcome. The older study using a lens no longer in common use reported more complications with the contact lens. |
| Adverse effects: astigmatism | Outcome not reported for this comparison | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence High‐certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate‐certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low‐certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low‐certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
| 1Downgraded one level for risk of bias due to serious limitation in study design and execution (the single study has a high risk of bias due to lack of blinding of study personnel). | ||||||
| Phototherapeutic keratectomy versus alcohol delamination | ||||||
| Patient or population: people with recurrent corneal erosion syndrome without previous surgical intervention Settings: outpatient Intervention: phototherapeutic keratectomy (after epithelial debridement) Comparison: alcohol delamination and sham excimer laser (after epithelial debridement) | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Certainty of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Alcohol delamination | Phototherapeutic keratectomy | |||||
| Resolution of symptoms after treatment Follow‐up: 3 months | 590 per 1000 | 378 per 1000 (177 to 797) | RR 0.64 (0.30 to 1.35) | 33 participants (1 study) | ⊕⊕⊝⊝ | |
| Recurrence after complete or partial resolution Follow‐up: 24 months | 294 per 1000 | 373 per 1000 (141 to 991) | RR 1.27 (0.48 to 3.37) | 33 participants (1 study) | ⊕⊕⊝⊝ | All participants were followed for recurrence up to 24 months |
| Time to recurrence Follow‐up: 24 months | Mean time to recurrence in the control group was 6 months | Mean time to recurrence in the intervention group was 0.5 months longer | ‐ | 33 participants (1 study) | ⊕⊕⊝⊝ | Standard deviations not reported but difference between groups was reported to be not statistically significant |
| Recurrences requiring further treatment Follow‐up: 24 months | 176 per 1000 | 125 per 1000 (25 to 651) | RR 0.71 (0.14 to 3.70) | 33 participants (1 study) | ⊕⊝⊝⊝ | Further treatment of choice not indicated |
| Symptoms (pain score) (scale 0‐10) (lower scores indicate less pain) Follow‐up: 24 months | Mean pain score in the control group was1.7 | Mean pain score in the intervention group was 0.7 lower (2.23 lower to 0.83 higher) | ‐ | 33 participants (1 study) | ⊕⊕⊝⊝ | |
| Adverse effects: corneal haze Follow‐up: 12 months | There were no events in either group. | 33 participants (1 study) | ⊕⊝⊝⊝ | |||
| Adverse effects: astigmatism | Outcome not reported for this comparison | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence High‐certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate‐certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low‐certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low‐certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
| 1Downgraded one level for imprecision: small sample size | ||||||
| Diamond burr superficial keratectomy (after epithelial debridement) versus sham diamond burr (after epithelial debridement) | ||||||
| Patient or population: people with recurrent corneal erosion syndrome without other corneal basement membrane dystrophy Settings: outpatient Intervention: diamond burr superficial keratectomy after epithelial debridement Comparison: sham diamond burr superficial keratectomy after epithelial debridement | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Certainty of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Sham diamond burr superficial keratectomy after epithelial debridement | Diamond burr superficial keratectomy after epithelial debridement | |||||
| Resolution of symptoms after treatment | Outcome not reported for this comparison | |||||
| Recurrence after complete or partial resolution Follow‐up: 6 months | 565 per 1000 | 40 per 1000 | RR 0.07 (0.01 to 0.50) | 48 participants (1 study) | ⊕⊕⊕⊝ | Single study reported major recurrence defined as those requiring ophthalmologist assessment |
| Time to recurrence Follow‐up: 6 months | Mean time to recurrence with sham diamond burr was 2.4 months | Mean time to recurrence in the intervention group was 3.6 months longer | ‐ | 48 participants (1 study) | ⊕⊕⊝⊝ | Only one event in diamond burr group |
| Recurrences requiring further treatment | Outcome not reported for this comparison | |||||
| Symptoms (pain score) | Outcome not reported for this comparison | |||||
| Adverse effects: corneal haze Follow‐up: 6 months | 43 per 1000 | 40 per 1000 | 0.92 (0.06‐13.87) | 48 participants (1 study) | ⊕⊕⊝⊝ | Four point scale was used to grade degree of haze (absent, mild, moderate, severe). Single study reported 1 mild haze and 1 moderate in the control and intervention groups respectively. Haze was analysed as dichotomous variable. |
| Adverse effects: astigmatism (mean magnitude) measured in dioptres. Higher value is worse astigmatism. Follow‐up: 3 weeks | Mean astigmatism in the sham diamond burr group was 0.88 dioptres | Mean astigmatism in the diamond burr group was 0.44 dioptres less (better) | ‐ | 48 participants (1 study) | ⊕⊕⊕⊝ | No standard deviations available |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence High‐certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate‐certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low‐certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low‐certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
| 1 Downgraded one level for imprecision: small sample size ‐ did not reach target sample size per included power calculations. | ||||||
| Study | Treatment/ prophylaxis | Country | No. of participants* | Average age | Age range | Percentage women | Intervention 1 | Intervention 2 | Comparator | Co‐intervention | Duration of treatment | |
| 1 | Treatment | UK | 29 | 39 | 21‐73 | 45% | Therapeutic contact lens Air Optix Night and Day lenses (silicon hydrogel with 24% water, CIBA vision), replaced every 30 days | Topical lubricant carbomer (celluvisc) 0.5% 4 times daily and lacrilube at night | 3 months | |||
| 2 | Treatment | Australia | 33 | 49 | NR | 45% | Phototherapeutic keratectomy epithelium removed with blade, excimer laser treatment (Zyoptix, Bausch and Lomb) | Alcohol delamination epithelium removed with blade, simulated excimer laser | Stat diclofenac (Voltaren Ophthal Eye Drops), chloramphenicol 0.5% (Chlorsig, Sigma Pharmaceuticals), prednisolone phosphate 0.5% (Minims, Bausch and Lomb), postoperative chloramphenicol and fluorometholone and therapeutic contact lens paraffin based lubricating ointment at night for 3 months following treatment participants with persistent or recurring symptoms causing discomfort were offered repeat phototherapeutic keratectomy | 3 months | ||
| 3 | Prophylaxis | UK | 42 | NR | NR | NR | Topical lubrication Lacrilube, Allergan at night | No topical lubrication | Cyclopentolate 1% drops and chloramphenicol ointment | 2 months | ||
| 4 | Treatment | UK | 30 | 45 | 27‐77 | 57% | Oral oxytetracycline 250 mg twice a day and topical prednisolone 0.5% four times a day and daily lid hygiene | Oral oxytetracycline 250 mg twice a day and daily lid hygiene | No oxytetracycline or prednisolone | Simple eye ointment. Macroerosions were treated with a single dose of cyclopentolate 1% and chloramphenicol followed by patching for 24 h and analgesia as required and paraffin (lubricating) ointment at night combined with manual debridement if the epithelium appeared wrinkled | 24 weeks for standard therapy, 12 weeks for tetracycline and 7 days for prednisolone | |
| 5 | Treatment | Germany | 100 | NR but inclusion criteria specified > 20 years | NR but inclusion criteria specified > 20 years | NR | Transepithelial excimer laser ablation (20 pulses of 193 nm) | Subepithelial excimer laser ablation (20 pulses of 193 nm). Subepithelial group also received additional contact bandages postoperatively until re‐epithelialisation | One‐off procedure | |||
| 6 | Prophylaxis study | Prophylaxis | UK | 117 | 38 | 14‐80 | 53% | Topical lubrication paraffin ointment nightly | Control hypertonic saline nightly | 3‐6 months | ||
| 6 | Treatment study | Treatment | Anterior stromal puncture purpose‐ | Therapeutic contact lens hydrogel (80% water content) soft contact lenses, left in situ for 6 weeks | If symptoms not controlled, a partial superficial keratectomy (anterior to Bowman's membrane) was performed. If this failed then the participant was withdrawn from study and total superficial keratectomy considered | 6 weeks | ||||||
| 7 | Treatment | Sweden | 56 | 45 | 21‐75 | 63% | Excimer laser ablation (after epithelial debridement) Summit ExciMed 200 central ablation of 5 microns with diameter of 6.5 mm | No excimer laser ablation (epithelial debridement alone) | Epithelial debridement using a Beaver blade or a sponge. Patch overnight. Antibiotic ointment, chloramphenicol | One‐off procedure followed by topical treatment 3 times per day for 3‐4 days | ||
| 8 | Treatment | UK | 24 | 43 | 22‐60 | 50% | Therapeutic contact lens hydrogel high water content lens (Duragel 75 plano) with chloramphenicol 2 times a day. | Topical lubrication hypromellose drops 4 times a day and paraffin ointment (oculentum simplex) nightly | 8 weeks | |||
| 9 | Treatment | China | 48 | 38 | 20‐70 | 56% | Diamond burr superficial keratectomy (after epithelial debridement) 5.0 mm diamond ball burr to polish denuded corneal surface for 30 seconds | Sham diamond burr superficial keratectomy (after epithelial debridement). Sham procedure performed without contact of corneal surface. | Epithelial debridement: loose epithelium removed using cellulose sponge. Tobramycin ointment (Tobrex; Alcon) and homatropine 4% cycloplegic eyedrops were applied followed by an eye patch overnight. Postoperatively, participants received a regimen of levofloxacin 0.5% (Cravit; Santen, Osaka, Japan) | One‐off procedure and topical treatment over 3‐4 months | ||
| 10 | Yamada 1998 prophylaxis study | Prophylaxis | Japan | 26 | 46 | 21‐71 | 35% | Antibiotic tetracycline ointment | Control hypertonic saline ointment | 6 months if no subjective symptoms, 3 months if no signs | ||
| 10 | treatment study | Treatment | Epithelial debridement | Anterior stromal puncture | Therapeutic contact lens | |||||||
| NR: not reported | ||||||||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Resolution of symptoms after treatment Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Recurrence after partial or complete resolution Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3 Pain Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Resolution of symptoms after treatment Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Recurrence after partial or complete resolution Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3 Pain score Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4 Recurrence requiring further treatment Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Recurrence after partial or complete resolution Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Corneal haze Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Recurrence of complete or partial resolution Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Recurrence after partial or complete resolution Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Symptoms (pain score) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3 Recurrences requiring further treatment Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Development of recurrent corneal erosions at 3 months Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 Severe symptoms (confirmed macroform recurrent corneal erosion | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Moderate symptoms (difficulty with daily activities/ sought further opinion) or severe symptoms | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 Mild symptoms (non‐disabling), moderate or severe symptoms | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Development of recurrent corneal erosions at 3 months Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1 Severe symptoms (confirmed macroform recurrent corneal erosion | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |

