Intervenções para prevenir e tratar dor pélvica e lombar na gravidez
Referencias
References to studies included in this review
References to studies excluded from this review
References to ongoing studies
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | 8‐week prospective RCT conducted in the Antenatal Care Unit of the Department of Obstetrics and Gynecology, Faculty of Medicine, Ege University, Turkey. | |
| Participants | Inclusion criteria:
Exclusion criteria:
| |
| Interventions | Intervention group (N = 37/33 analysed): PMR; 20‐minute session completed by each participant at home twice a day (morning and evening) for 8 weeks. At baseline, each participant attended a 2‐hour education session at the obstetrics department to check they understood and could complete the PMR exercises and breathing techniques. Each participant received handbook and a CD (prepared by Turkish Psychological Association). At 4‐weeks a follow‐up session took place at the obstetrics dept. to give feedback and check exercises. Control group (N = 36/33 analysed): participants instructed to lie down twice a day (morning and evening) for 20 minutes. At the end of the study participants received the same CD and handbook as the intervention group. Routine daily activity was not restricted for any group. Participants were asked to record their performance of the specified activities on a calendar in an attempt to encourage compliance. They were 'warned not to use any complementary treatment for LBP' during the study. | |
| Outcomes | Primary outcome: pain (VAS 0 to 10), completed at baseline, weeks 4 and 8. Secondary outcome: Generic Health Status (Short Form‐36), completed at baseline, weeks 4 and 8. Personal information form (PIF), completed at baseline: demographics, pregnancy and obstetric history. | |
| Condition (LBP, PP, LBPP) | LBP. | |
| Notes | Financial support was provided by Ege University Scientific Research Project (No. 2007/ASYO/004). Note: on page 2, higher score for SF‐36 was attributed to deterioration, while the reverse is true, which was borne out in the results section, where improvement is illustrated with a higher score. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | 'Random number table used to assign participants to control and experimental groups' but no further details on how the random number table was used. |
| Allocation concealment (selection bias) | Unclear risk | No information provided on allocation concealment. |
| Blinding of participants and personnel (performance bias) | High risk | Experimental group were aware of the benefit of exercise for their condition. Providers of training for PMR could not be blinded. |
| Blinding of outcome assessment (detection bias) | Low risk | No assistance was given by staff to any participants completing assessment forms/questionnaires. At the end of the study (week 8) the study co‐ordinator, who was blinded to group and timing of assessment, collected all assessment forms. |
| Incomplete outcome data (attrition bias) | Low risk | There was a 8% drop‐out rate from each group that were not accounted for in the analysis, nor were reasons provided for drop‐out. |
| Selective reporting (reporting bias) | Low risk | Means and SD were provided for primary and secondary outcomes at each time point (weeks 4 and 8) for all participants completing the study, N = 33 in experimental and N = 33 in control group. |
| Other bias | Low risk | VAS scores were similar between groups at baseline, however SF‐36 scores were not similar at baseline. Sample size very small, however there were very specific inclusion criteria and the authors controlled for use of co‐interventions in both groups and participants reported similar adherence to program. |
| Methods | 'Following ethical approval and through a randomised controlled clinical trial, 120 pregnant women with LBP were recruited into experimental and control groups.' Conducted in Iran. | |
| Participants | Inclusion criteria:
Exclusion criteria:
| |
| Interventions | Intervention group (N = 60/57 analysed):
Control group (N = 60/55 analysed): Usual prenatal care. | |
| Outcomes | Pain (VAS 0 to 10) and disability (ODI) were measured in both groups but, in the results, only the baseline and the difference from baseline was reported in each study group (with no report of SD). The comparison of all changes between 2 study groups were statistically significant with P < 0.0001. | |
| Condition (LBP, PP, LBPP) | LBP. | |
| Notes | Change score from immediately after treatment was subtracted from the baseline pain score for an 'immediately after treatment' VAS score; reported lost to follow‐up was assumed to have happened during treatment; RevMan calculator was used to calculate SD to allow results to be included in meta‐analysis for 'any exercise vs usual prenatal care', analysis 1.1. Translated from Arabic by single Iranian researcher. Funding = no information provided. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Block randomisation with matching (stratification?) for age, gestational age, and BMI. |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned in paper. |
| Blinding of participants and personnel (performance bias) | High risk | Patients were not blinded. Nothing mentioned about blinding of providers. |
| Blinding of outcome assessment (detection bias) | High risk | Nothing mentioned about blinding of outcome assessors. |
| Incomplete outcome data (attrition bias) | Low risk | 120 patients were enrolled (60 in each group). 3 patients in intervention group, 5 in control group missed. In all cases the researchers lost track of the patients due to the change in living location. |
| Selective reporting (reporting bias) | Unclear risk | The outcomes were also measured at 6 months and 1 year after delivery. But only the results for immediately after treatment, and 3 months after delivery were reported. Pain (VAS) and disability (ODI) were measured in both groups. But in the results, only the baseline and the difference from baseline, with no report of SD, were reported in each study group. The comparison of all changes between 2 study groups were statistically significant with P < 0.0001. |
| Other bias | Low risk | Nothing noted in the paper. |
| Methods | 'Prospective masked randomised experimental clinical trial', carried out at the National Women's Hospital, Physical Therapy outpatient department, Auckland, NZ. Those meeting inclusion criteria were assessed by 1 of 4 therapists (identically trained); 36 withdrew prior to randomisation because they did not meet the inclusion criteria. To see a small to medium effect size (0.35) on a modified RMDQ, with power set at 0.8 and alpha at 0.05, 30 women were needed per group. Number randomised = 90; number analysed = 87. | |
| Participants | Inclusion criteria:
Exclusion criteria:
| |
| Interventions | Intervention groups: 1. Exercise plus non‐rigid support belt (N = 29 analysed): participants received same information and exercises as the control group, plus a non‐rigid neoprene support belt (Smiley Belt) and logbook for recording number of hours the belt was worn and number of times exercises done. 2. Exercise plus rigid support belt (N = 28 analysed): participants received same information and exercises as the control group, a rigid belt (Lifecare Pubic Belt) and a logbook for recording number of hours the belt was worn and number of times exercises done. Control group: Exercise only (N = 30 analysed): participants received an exercise booklet with 5 exercises aimed to increase the stability of the pelvic bones. A trained physical therapist demonstrated the exercises and checked that they were being performed correctly. Exercises needed to be completed 3 times daily for 1 week. Participants were given logbook to record the frequency they exercised. Participants also received verbal and written education about the anatomy and pathology of symphysis pubis dysfunction and self‐help management. See study’s Appendix 2 and 3 for specific exercises and self‐help management techniques). | |
| Outcomes | Average and worst pain in last week ‐ NRS (0 to 100); modified RMDQ; Patient Specific Functional Scale; measured at baseline, after treatment. | |
| Condition (LBP, PP, LBPP) | PP. | |
| Notes | There were no significant differences between the groups in adherence to their exercise program or belt wearing. The adherence rate was acceptable (average for all participants: Exercises = 16.5/21 times, Number of hours belt worn/week = 44.2). Funding = Maurice and Phyllis Paykel Trust for a Research Scholarship. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: 'Randomization process involved the use of a table of 3 randomly permuted blocks'. |
| Allocation concealment (selection bias) | Unclear risk | Not specifically mentioned: patients assigned to groups by independent person (not connected to study) but unclear how this was actually done. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Patients not blinded; therapists providing exercise therapy were unaware of the intervention groups to which participants were assigned. However, unclear as to who distributed the belts. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Authors did not specify who collected the outcomes (outcomes were self‐report measures). |
| Incomplete outcome data (attrition bias) | Low risk | No withdrawals in the control group. 1 woman in the non‐rigid support belt group delivered her baby before the post‐intervention assessment. 2 women in the rigid support belt group delivered their babies before their post‐intervention assessment. 1 woman refused to be in the study as she was 'not prepared to be in the exercise‐only group'. No exclusions mentioned. |
| Selective reporting (reporting bias) | Low risk | Study reported all outcomes as indicated in methods. |
| Other bias | Low risk | Groups similar at baseline; adherence similar between groups; outcomes taken at same time for each group, co‐interventions likely to be similar. |
| Methods | Observer‐blinded RCT. | |
| Participants | 257 women were randomised. Inclusion criteria: Healthy Norwegian speaking women between 18 to 40 years from 2 Maternity Care Units (within the Norwegian Public Health System). Exclusion criteria: 1. Pregnant women carrying twins. 2. Inflammatory rheumatic disorders. 3. Risk factors for miscarriage. | |
| Interventions | Intervention group (N = 129/106 analysed): Participants, referred to 1 of 2 specially trained physical therapists, received tailored supervised group exercise once a week, along with advice to do daily HEP. Specific attention to body awareness and ergonomic advice in real‐life situations; the main focus of the intervention being the specific training of the transversely oriented abdominal muscles with co‐activation of the lumbar multifidus at the lumbosacral region, and stretching the hip abductors. Intervention took place for a maximum of 16 weeks, between 20 to 36 weeks' gestation, with no follow‐up after 36 weeks' gestation. Control group (N = 128/107 analysed): Usual prenatal care. | |
| Outcomes | Primary outcome: The proportion of women experiencing pain in the lumbar spine/pelvic girdle. Secondary outcomes: 1. Functional disability measured with the modified RMDQ (0 to 24). 2. LBP and LBPP measured using the VAS scale (0 to 10). 3. Health‐related quality of life measured with the SF‐8 Health Survey. All outcomes measured at 24, 28, 32, and 36 weeks' gestation. | |
| Condition (LBP, PP, LBPP) | LBPP. | |
| Notes | Funding/sponsor: Norwegian Fund for Postgraduate Training in Physiotherapy (Norway). Lead author contacted to clarify the number analysed in intervention group; she confirmed that it should be 106, not 103 as stated in the Figure and tables. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | 'randomisation procedure was computer generated by the statistician not involved in data collection.' |
| Allocation concealment (selection bias) | Low risk | 'group allocation was concealed in consecutively numbered, sealed, opaque envelopes.' |
| Blinding of participants and personnel (performance bias) | High risk | Participants not blinded. |
| Blinding of outcome assessment (detection bias) | High risk | Outcomes were self‐reported, therefore not blinded; however the midwives who distributed the questionnaires to the women were not aware of their group allocation. |
| Incomplete outcome data (attrition bias) | Low risk | Treatment group lost 22/129 (17.8%) and the control group lost 21/128 (16.4%) by the end of follow‐up at 36 weeks' gestation. |
| Selective reporting (reporting bias) | Low risk | Results provided for all the outcomes outlined in the trial registration (ISRCTN95014448). |
| Other bias | Low risk | Groups were similar at baseline except that the training group had significantly higher BMI; almost twice as many women in the training group had experienced moderate to severe PGP in a previous pregnancy but this was adjusted for in the outcome analyses; adherence to exercises did not seem to vary between groups, nor did consultation with healthcare providers. |
| Methods | 40 pregnant women 'from the same demographic area' in Sweden; N = 20 in each group (group 1 and 2). After diagnosis with pelvic and LBP, women were referred to the acupuncturist at the hospital 'where randomisation was carried out; women were phoned to give them the dates for their acupuncture; baseline data were collected when they came for treatment'. | |
| Participants | Inclusion criteria:
Exclusion criteria:
| |
| Interventions | Both groups received the same treatment; 8 acupuncture treatments over a 6‐week period (2 treatments per week in the first 2 weeks and once per week thereafter) with first treatment lasting 20 minutes and number of needles limited to 5, and remainder 30 minutes with maximum 10 needles. Intervention group 1 (N = 20/16 analysed): mean age 28.6 years, started treatment at 20 weeks' gestation and Intervention group 2 (N = 20/16 analysed): mean age 27.9 years, started treatment at 26 weeks' gestation. No control group: acupuncture intervention was started either at 20 (group 1) or 26 weeks' (group 2) gestation. | |
| Outcomes | Short Form Health survey questionnaire (SF‐36), Short Form Magill Pain Questionnaire (MPQ), Pain‐o‐meter, fetal sound measured at baseline, at 4th and 8th treatment sessions, at same times for each group; qualitative data collected via telephone interviews 2 to 3 months after delivery. Both groups had similar experience of acupuncture (from qualitative interviews). Small number of study participants acknowledged by authors. Non compliance in both groups reported. | |
| Condition (LBP, PP, LBPP) | LBPP. | |
| Notes | Funding = Council of Research and Development (FoU‐centrum), Landstinget Kronoberg, Sweden. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information given about sequence generation; in the discussion it states that 'the women were chosen randomly'. |
| Allocation concealment (selection bias) | Low risk | Telephone allocation. |
| Blinding of participants and personnel (performance bias) | Low risk | 'both groups had similar experience with acupuncture when asked at end of treatment'; unclear if acupuncturists were informed of gestation, or if they were able to determine by observation, however, the difference was only 20 to 26 weeks, therefore likely not a big issue. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Insufficient information provided on who collected the self‐report outcomes. |
| Incomplete outcome data (attrition bias) | Low risk | Both groups had 4 drop‐outs with reasons given ‐ did not appear to be related to intervention. |
| Selective reporting (reporting bias) | Low risk | Qualitative data supports quantitative data ‐ however the telephone interviews were completed by the study author. |
| Other bias | Low risk | Co‐interventions and adherence similar across groups, timing of outcome assessment same across groups, mean pain intensity was significantly lower in group 1 than group 2 at baseline. |
| Methods | Single‐blind RCT; N = 386 women consecutively selected by doctors and midwives and randomised to 3 groups; acupuncture, stabilising exercises and standard treatment. ITT: those who finished the study were analysed in the group to which they had been assigned. | |
| Participants | Inclusion criteria:
Exclusion criteria:
| |
| Interventions | Intervention group 1: acupuncture (N = 125/110 analysed). Intervention group 2: stabilising exercises (N = 131/112 analysed). Control group: standard treatment (N = 130/108 analysed). | |
| Outcomes | Pain intensity (VAS 0 to 100): self‐report each am and at 1 week post‐treatment: examiner assessment of recovery from symptoms ‐ positive pain drawing; examiner assessment of recovery from symptoms ‐ P4 test; examiner assessment of recovery from symptoms ‐ pain when turning in bed. Adverse events: none reported for any of the 3 groups. | |
| Condition (LBP, PP, LBPP) | PP. | |
| Notes | Women recruited from East Hospital, Sahlgrenska Academy and 27 maternity care centres in the hospital's reference area in Gothenburg, Sweden between 2000 and 2002. Funding = The Vardal Foundation, the Dagmar Foundation, the Trygg‐Hansa Insurance Company, the Sahlgrenska University Foundation. 14 March 2012 ‐ email and LinkedIn message sent to Dr Elden to clarify number of participants in Table 3; response received ‐ clarified that there were 130 in the standard group and 131 in the exercise group; other data are correct. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random table to determine the allocation sequence before the study. |
| Allocation concealment (selection bias) | Low risk | Pre‐sealed opaque envelopes. |
| Blinding of participants and personnel (performance bias) | High risk | Participants and providers were not blinded. |
| Blinding of outcome assessment (detection bias) | Low risk | 'Results coded and entered by personnel from independent institution; Statistician blinded to group and treatment.' |
| Incomplete outcome data (attrition bias) | Low risk | Standard treatment group; randomised = 130; analysed = 108 [83.0%] (lost to follow‐up: declined treatment N = 15, early delivery N = 3, declined visit N = 3, moved from area N = 1). Acupuncture group: randomised = 125; analysed = 110 [88%] (lost to follow‐up: declined treatment N = 10, declined visit N = 1, early delivery N = 4). Stabilising exercises: randomised = 131; analysed = 112 [85.5%] (lost to follow‐up: declined treatment N = 9, moved from area N = 1, early delivery N = 4, declined visit N = 5). ITT: analysed participants measured 1 week post‐treatment against those randomised. |
| Selective reporting (reporting bias) | Low risk | Data presented for a priori determined outcomes. |
| Other bias | Low risk | Table 3 seems to have the number of women reversed between 'Standard' and 'Exercise' groups. Author clarified this to be so. |
| Methods | 'Randomised double‐blind controlled trial.' N = 115 randomised; N = 58 to standard treatment plus acupuncture; N = 57 to standard treatment plus non‐penetrating acupuncture. | |
| Participants | Inclusion criteria:
Exclusion criteria:
| |
| Interventions | Intervention group (N = 58/56 analysed): standard treatment + penetrating acupuncture Standard treatment: general information about condition and anatomy of back and pelvis and a pelvic belt, gave advice and HEP designed to increase strength in the abdominal and gluteal muscles. Information was supplemented by a leaflet. Also instructed to avoid other treatments during intervention period. Penetrating acupuncture: see study methods for exact acupuncture points used. Sterilised disposable needles were used and inserted intramuscularly to depth of 15‐50 mm. Needles were left in situ for 30 minutes and manually stimulated every 10 minutes. Control group (N = 57/52 analysed): standard treatment + non‐penetrating acupuncture Standard treatment: identical to experimental group Non‐penetrating acupuncture: used a validated sham acupuncture device (which looks like real acupuncture needles but the tip of needle is blunted). The shaft of the sham needle did not penetrate the skin, it collapsed into the handle and creates an illusion of insertion. Needles were left in situ for 30 minutes and manually stimulated every 10 minutes. | |
| Outcomes | EQ‐5d questionnaire and EQ‐5d VAS; pain (VAS 0 to 100) in the morning and evening; ODI (back specific function); frequency of sick leave; Disability Rating Index (DRI) measured at baseline, after treatment and 1‐week follow‐up. Adverse events: transient, tingling, needle pain, slight bleeding, fainting, sleepiness. | |
| Condition (LBP, PP, LBPP) | PP. | |
| Notes | Pain severity diagnosed with ASLR and P4 tests. N = 165 women assessed for eligibility (N = 50 did not meet inclusion criteria). All women acupuncture naive and singleton fetus. No serious adverse events reported. Same contact time, manual contact during search and stimulation of needles, interaction between patient and therapist in both groups. Drop‐outs reported with reasons. Funding = grants from the Foundation of the Health and Medical care committee of the Region of Västra Götaland (Sweden), grants from the Swedish Medical Research Council and Swedish government grants to researchers in the public health service. Women recruited between June 2006 and May 2007 from 25 units within the Västra Götaland region, Sweden. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: 'Computer‐generated random table was used'. |
| Allocation concealment (selection bias) | Low risk | Statistician who was not involved in the study administered pre‐coded numbered identical opaque envelopes to assign participants to the intervention groups. |
| Blinding of participants and personnel (performance bias) | Low risk | Participants: low risk as only LI4 (on hand) not blinded. 'Women were blinded to whether they were receiving sham or active treatment.' Providers: high risk Not blinded. |
| Blinding of outcome assessment (detection bias) | Low risk | Assessors: low risk Blinded to treatment allocation, doctors handling decisions about sick‐listing were also blinded. |
| Incomplete outcome data (attrition bias) | Low risk | Drop‐outs: 2 in treatment and 5 in control dropped intervention because it 'violated protocol'. At follow‐up: 3 drop‐outs in treatment group due to early birth and declined visit, 2 in control group due to declined visit. Low drop‐out rate, and similar reasons between the groups. Low risk: attrition and drop‐outs reported and reasons, numbers at each stage add up, ITT ‐ last value carried forward. |
| Selective reporting (reporting bias) | Low risk | Study reported all outcomes it said it would report in methods. All outcome data are found in tables. |
| Other bias | Low risk | Randomisation procedure successful (however more in control group on sick leave?). |
| Methods | Multicentre single‐blind RCT. | |
| Participants | Inclusion criteria:
Participants were diagnosed according to the European PGP Guidelines. Exclusion criteria:
| |
| Interventions | Intervention group (N = 63 randomised/analysed): craniosacral therapy (CST) as adjunct to standard treatment.
Control group (N = 60 randomised/analysed):
All information provided as standard treatment was supplemented by a leaflet. | |
| Outcomes | Primary outcomes: pain intensity (VAS 0 to 100) in the morning and evening; sick leave. Secondary outcomes: function (modified ODI); Disability Rating Index; Quality of Life. (EuroQol‐5d); unpleasantness of pain (VAS); helpfulness of treatment. Physical tests used: Faber Test, 4P test, Modified Trendelenberg Test, Symphysis Pubis Pressure Test, ASLR. Women also completed a pain drawing denoting the location of their symptoms. | |
| Condition (LBP, PP, LBPP) | PP. | |
| Notes | Study supported by research grants from the Health and Medical Care Committee of the Regional Executive Board, Region Vastra Gotaland (Sweden), Grant No. [VGFOUREG‐155171]. Study conducted in Gothenberg, Sweden. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random table used. Stratified balanced randomisation was used to guarantee balance between groups for frequency of sick leave. |
| Allocation concealment (selection bias) | Low risk | Research assessor not involved in the study administered pre‐coded, numbered identical opaque envelopes to assign participant to groups. |
| Blinding of participants and personnel (performance bias) | Low risk | Blinding not possible for participants or providers, however the researchers did assess the credibility of treatment to reduce the effect of treatment preference for participants. |
| Blinding of outcome assessment (detection bias) | Low risk | Independent observer measured and entered VAS without knowledge of group assignment; Statistican blinded to group allocation and treatments. |
| Incomplete outcome data (attrition bias) | Low risk | Attrition and exclusions given with reasons, ITT analysis used (last value carried forward). 6 women withdrew from CST. |
| Selective reporting (reporting bias) | Low risk | Results presented as described in the methods. All outcome data are found in tables. |
| Other bias | Low risk | Women asked to conceal information about their treatment during assessment. Interventions carried out by 2 experienced craniosacral therapists who met to ensure consistent approach throughout study. No serious adverse events ‐ 5 minor adverse events reported including only partial pain relief (N = 1), belt discomfort (N = 1), drowsiness (N = 3). |
| Methods | 266 randomised: those who could not exercise were excluded from the exercise group, but it is unclear why 54 people dropped out of exercise group and none dropped out of control group. | |
| Participants | 280 women invited to participate from those who registered at the hospital (no details about how they were selected from the 2358 who had registered at the clinic during the study period). Inclusion criteria:
Exclusion criteria:
Baseline characteristics: | |
| Interventions | Intervention group (N = 161/107 analysed): (54 who could not participate in exercises = 107). Control group (N = 105 randomised/analysed?): usual prenatal care. | |
| Outcomes | No scales/units given for outcomes measured, but may be assumed they are reporting the group mean, measured on the KEBEK questionnaire (Iranian version of Quebec Questionnaire for assessing pain; range 0 to 100, higher = worse pain); change scores do not appear to be included; the degree of lordosis and degree of flexibility of the spine. Outcomes assessed at baseline and after 12 weeks for both groups. Adverse events: none reported. | |
| Condition (LBP, PP, LBPP) | LBP. | |
| Notes | Numbers do not add up; there are contradictions in text; we tried unsuccessfully to clarify data with lead author during the 2007 update. Funding: not stated. Study conducted at Hazrat Zaynab Hospital prenatal clinic in Tehran, Iran. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | ‘prospective randomised study’ but method of randomisation not described. |
| Allocation concealment (selection bias) | Low risk | Sealed envelopes. |
| Blinding of participants and personnel (performance bias) | High risk | Participants and providers were not blinded. |
| Blinding of outcome assessment (detection bias) | Low risk | Report states that the outcome assessor was blinded. |
| Incomplete outcome data (attrition bias) | High risk | Difficult to assess since numbers do not add up; appears that 14 withdrew prior to randomisation; about 20% withdrew/dropped out after randomisation; it appears that 54 dropped out of the intervention group and none out of the control group. |
| Selective reporting (reporting bias) | High risk | Results are difficult to interpret and appear to be reversed. |
| Other bias | Low risk | Nothing more to add. |
| Methods | Prospective RCT including 169 pregnant women recruited from 3 obstetric centres. Women randomised into experimental (N = 87) and control (N = 82) groups. | |
| Participants | Inclusion criteria:
Women were evaluated by their obstetric provider. Those with symptoms were screened by a dedicated study co‐ordinator. Women were not excluded if they had lower limb symptoms or radiculopathy. Exclusion criteria:
| |
| Interventions | Intervention group (N = 87 randomised/analysed): multi‐modal musculoskeletal and obstetric management (MOM) ‐ standard obstetric care PLUS a chiropractic specialist provided manual therapy, stabilisation exercises and patient education based on the biopsychosocial model. Women attended weekly for MOM until 33 weeks' gestation, and were expected to complete home exercises twice a day. The aim was for women to receive 4 to 6 treatments each but number actually received was not recorded. NB: sacroiliac belts were reserved for women with severe hypermobility. Control group (N = 82 randomised/analysed): Standard Obstetric Care (STOB). Frequency of visits at the discretion of the obstetrics provider who also could recommend 1 or more of the following; rest, aerobic exercise, heat pad application (maximum 10 minutes), use of acetaminophen or narcotics if severe comfort not relieved with other methods, or onward referral. | |
| Outcomes | Primary outcomes: pain intensity (NRS 0 to 10), Disability (Quebec Disability Questionnaire ‐ QDQ). Secondary outcomes: personal pain history (PPH), SLR, P4 test, ASLR, long dorsal ligament test, sick leave, Patients' Global Impression of Change (patients' perception of clinical improvement), use of over‐the‐counter medications, trouble sleeping. | |
| Condition (LBP, PP, LBPP) | LBPP. | |
| Notes | This study is the full paper associated with Gross (2012) reported in the previous update of this review (presented at the 32nd Annual Meeting for the Society for Maternal‐Fetal Medicine, Dallas in February, 2012). The study was funded by the Health Resources and Services Administration, Grant number: R18HP07640. Study took place in St Louis, USA. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Blocked randomisation scheme used across the 3 recruitment sites using a computer‐generated list of randomised numbers. |
| Allocation concealment (selection bias) | Low risk | Online Web Data Entry System used to allocate women to experimental or control groups. |
| Blinding of participants and personnel (performance bias) | High risk | No report on blinding of providers or participants. |
| Blinding of outcome assessment (detection bias) | Low risk | Chiropractic specialist performing baseline evaluation and follow‐up exams 'single masked'. |
| Incomplete outcome data (attrition bias) | Low risk | Data from all recruited participants were analysed, but there was 24% drop‐out from MOM group and only 13% drop‐out from control group; reasons for drop‐out not provided. |
| Selective reporting (reporting bias) | Low risk | NRS, QDQ, PPH, SLR (left leg only) and ASLR measured at baseline and 33 weeks. Means and SD were presented along with P values however, there were 10 more drop‐outs from the experimental group than the control group. Query re: number of individuals approached versus number randomised ‐ first author (JG) confirmed via email, 30 January 2015 (N = 2510 approached, N = 2341 excluded). |
| Other bias | Low risk | Groups were demographically similar and baseline evaluation showed no differences in pain, disability, physical assessments or other secondary outcomes between groups. |
| Methods | Potential women were identified through obstetric records and approached, in person or by phone, to determine if they met the inclusion criteria. 41 women were invited to attend; 4 declined, 3 did not attend the first follow‐up. 34 women randomised to either Global Postural Re‐education (GPR) treatment or usual prenatal care. | |
| Participants | Women selected from those receiving prenatal care in 3 health centres and those who attended lectures in preparation for birth at a private hospital in Campinas, Brazil. Both groups of women were similar in most of the characteristics studied on admission to the study: in the GPR group 10 women came from a private hospital and 7 from a health (public) centres. In the control group there were 6 women from the private hospital and 11 from health (public) centres. Inclusion criteria:
Differentiation made between LBP and posterior PP at baseline physiotherapy assessment. | |
| Interventions | Intervention group = GPR (N = 17 analysed): Weekly 40‐minute sessions for 8 weeks. Stretching of the muscles of the posterior chain ‐ angle closure coxo‐femoral and abduction of the upper limbs and closing angle coxo‐femoral with adduction of the upper limbs. Control group (N = 17 analysed): usual prenatal care. | |
| Outcomes | GPR group: Intensity of LBP, using VAS (0 to 10) at baseline, before/after each treatment session. Back‐related functional disability, using the RMDQ at baseline, before/after each session. Control group: Intensity of LBP (0 to 10) and RMDQ measured at baseline, at 4 and 8 weeks. Use of pain medication collected for both study groups. | |
| Condition (LBP, PP, LBPP) | LBP. | |
| Notes | Used Google Translate (Google Translate) to translate from Portuguese; verified by single Portuguese researcher. Paper stated that there was no external funding. Data needed for the meta‐analyses appeared to be incorrectly reported in the paper and we re‐analysed. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | 'randomisation was performed by using a list of random numbers generated by computer.' |
| Allocation concealment (selection bias) | Unclear risk | No mention in translated version of allocation concealment. |
| Blinding of participants and personnel (performance bias) | High risk | 'these professionals had lagged randomisation, so did not know to which group each woman was allocated' ... however, those who provided the exercise therapy and those who received it would have known to which group they were allocated. |
| Blinding of outcome assessment (detection bias) | High risk | 'at the end of the participation on each woman in the study, they conducted a professional full re‐evaluation of LBP' ... however, the women were the ones who reported their symptoms via the VAS and RMDQ. |
| Incomplete outcome data (attrition bias) | Unclear risk | 3 participants are reported as lost to follow‐up; there is no real clarification of their initial group ‐ it could be control group, but the 17 in each group do not seem to take any losses into consideration. |
| Selective reporting (reporting bias) | Low risk | Data provided for baseline and after intervention outcome measures for pain and disability. |
| Other bias | High risk | Not similar at baseline for education or age (intervention group was better educated and older), but similar in other prognostic factors; women in control group used more pain medication (87% versus 12% in intervention group); no information provided on compliance, co‐interventions or use of pain medication; the control group was only measured twice after baseline, the intervention group was measured 8 times, but all within the same time‐frame. |
| Methods | Randomised trial conducted in private practice in Jena, Germany. Group allocation was 'by external randomisation'. | |
| Participants | Inclusion criteria:
| |
| Interventions | Intervention group = OMT (N = 21 randomised/analysed): usual prenatal care plus 4 custom tailored osteopathic treatments in 2‐week intervals based on osteopathic principles. Control group (N = 20 randomised/analysed): usual prenatal care; also received osteopathic treatment after an 8‐week untreated waiting period. | |
| Outcomes | Primary outcomes: pain intensity (VAS 0 to 10); pain frequency measured using a Likert scale; Secondary outcomes: functional disability (RMDQ), parturition characteristics and frequency of osteopathic dysfunctions. | |
| Condition (LBP, PP, LBPP) | LBP. | |
| Notes | Full thesis is in German and has not been requested as of Jan 2015; information and data extracted from the English abstract and the systematic review by Franke 2014. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | 'randomised via external randomisation.' |
| Allocation concealment (selection bias) | Unclear risk | Methods of concealment not noted in abstract, but Franke et al assessed as low risk. |
| Blinding of participants and personnel (performance bias) | High risk | 'One trained osteopath conducted the study in her private practice in Jena, Germany.' |
| Blinding of outcome assessment (detection bias) | High risk | 'One trained osteopath conducted the study in her private practice in Jena, Germany.' |
| Incomplete outcome data (attrition bias) | Low risk | No attrition reported in the abstract. |
| Selective reporting (reporting bias) | Unclear risk | Data only provided for pain intensity in the abstract; in Franke 2014, data for pain intensity and RMDQ provided in forest plots, Figures 6 and 7; Franke 2014 assessed as low risk. |
| Other bias | Unclear risk | It was difficult to note because of limited information in the abstract, but Franke 2014 assessed as low risk. |
| Methods | A randomised, controlled, clinical study (PROMOTE). Clinical personnel referred interested women to the research co‐ordinators for screening. N = 400 randomised. | |
| Participants | Inclusion criteria:
| |
| Interventions | All groups received usual prenatal care. Intervention group 1 (N = 136): Osteopathic Manipulative Therapy (OMT) to specific body regions x 7 treatments of approximately 20 minutes each at weeks 30, 32, 34, 36, 37, 38 and 39. Intervention group 2 (N = 131): placebo ultrasound (US) incorporating tactile and manual stimulation of the same body regions as OMT, using steady, circular movements with an US wand, and the usual auditory and visual cues of an US machine, but not emitting any US waves. Each treatment lasted approximately 20 minutes and was conducted at the same weeks' gestation as the OMT group. Control group (N = 133): Usual prenatal care only. This group did not spend any additional time with, or intervention from the treating physician. | |
| Outcomes | Primary outcomes: collected at baseline, and each visit.
Secondary outcomes: collected from participants' clinical notes after delivery.
Additional baseline data collected:
| |
| Condition (LBP, PP, LBPP) | LBP. | |
| Notes | Study conducted from 2007 to 2011 at 3 Obstetrics and Gynecology clinics in Texas, USA. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation program used to allocate women, in blocks of 15, by clinical obstetric clinic. |
| Allocation concealment (selection bias) | Low risk | No specific information provided. However, the authors state that a 'randomisation envelope' was opened to reveal participant's group assignment, which would suggest appropriate concealment method. |
| Blinding of participants and personnel (performance bias) | High risk | Participants in the OMT and placebo US groups received same duration of treatment, number of treatments and to same bodily regions, however it was not possible to blind to intervention. Providers could not be blinded. |
| Blinding of outcome assessment (detection bias) | Low risk | After delivery, the research co‐ordinator collected data from each participant's medical record in paper format. Data were then transferred to an electronic data set using 'double data entry'. |
| Incomplete outcome data (attrition bias) | Low risk | Attrition and exclusions reported, including number and reasons. An ITT analysis was completed initially (imply last measure carried forward), followed by a PPA as high numbers did not complete the protocol (all 7 visits) in each group. Each type of analysis gave similar results. |
| Selective reporting (reporting bias) | Low risk | All data reported as stated in methodology. |
| Other bias | Low risk | Outcomes assessed at same time points; co‐interventions controlled as women unable to continue in the study if they reported using any other body‐based therapies. Characteristics similar at baseline except BMI. At baseline, pain at best higher in OMT group versus usual prenatal care only, and 'pain now' higher in OMT versus placebo US. Results showed no difference in improvements in pain and function between OMT and placebo US groups. |
| Methods | RCT conducted in a tertiary referral hospital in Australia (N = 115 women randomised). | |
| Participants | Inclusion criteria:
Exclusion criteria:
| |
| Interventions | Intervention group (N = 55/46 analysed): BellyBra. A nylon/spandex undergarment worn like a vest, has a 1‐way stretch panel across the thoracolumbar back that is designed to provide support and assisted by the involvement of shoulder straps, to improve posture. A wide elastic band sits below the abdomen supporting the uterus and lifting weight off the pelvis. Control group (N = 60/48 analysed): Tubigrip. More generic form of support. Worn as a double layer and extends from the mid‐thoracic spine to the sacral spine and pelvis. | |
| Outcomes | VAS (0 to 10 cm), physical activity including work, satisfaction with life survey (SWLS), use of analgesic medication, usefulness of garment at baseline, completion of 3‐week intervention, 'on a return visit to the antenatal clinic' ‐ ? timing. | |
| Condition (LBP, PP, LBPP) | LBP. | |
| Notes | Although the primary aim was to assess the severity of LBP and posterior PP, the PP was primarily due to pain in the sacroiliac joint. Conducted in Australia. Funding = no funding or support was provided for any of the authors; Furtile Mind Pty Ltd (retailers for maternity and postpartum clothes, supplies) provided the BellyBras used in the study. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: 'Participants were randomised...by means of computer‐generated numbered, sealed, opaque envelopes'. |
| Allocation concealment (selection bias) | Low risk | Opaque sealed envelopes used. |
| Blinding of participants and personnel (performance bias) | High risk | No blinding of participants, providers mentioned. |
| Blinding of outcome assessment (detection bias) | High risk | No blinding of assessors mentioned. |
| Incomplete outcome data (attrition bias) | High risk | 9 participants (16%) in intervention group were lost at follow‐up (2 delivered within study period, 7 failed to attend appointment and could not be contacted). 12 participants in control group (20%) were lost at follow‐up (3 delivered within study period, 9 failed to attend their follow‐up appointment and could not be contacted). No exclusions mentioned; 14% were lost to follow‐up with no reason. |
| Selective reporting (reporting bias) | Low risk | Study reported all outcomes it said it would report in methods. |
| Other bias | High risk | 11 women (23.9%) in intervention group and 23 women (47.9%) in control group reported the use of other treatments for their back pain during the study period, including the use of analgesic medication, physiotherapy, acupuncture, massage, etc. (co‐interventions make it difficult to attribute change to the intervention). Most noticeably, 3 in the intervention and 14 in the control group used analgesic medication during the study period. 44 (95.7%) women in intervention group stated that they wore the garment at least once a week compared with 33 (68.8%) in the control group. High risk: co‐interventions and compliance different. |
| Methods | 43 women 'randomly assigned' to study group; 30 women completed the study and were analysed. | |
| Participants | Inclusion criteria:
Exclusion criteria:
| |
| Interventions | Intervention group (N = 15 analysed): exercise. 1 hour introduction session with 7 exercises and relaxation movements taught. Each exercise session lasted 30 minutes x 3/week x 8 weeks. Exercise included warm up (4.5 minutes) walking, stretching (spine extensors, hamstrings, thigh adductors, lumbar paravertebral muscles), strengthening (thigh extensors and abdominal obliques) x 21 minutes, relaxation x 4.5 minutes. Control group (N = 15 analysed): routine prenatal care ‐ did not perform any of the study exercises. | |
| Outcomes | Disability (RMDQ); lumbar lordosis using flexible ruler and formula measured at baseline, after 1 and 2 months. | |
| Condition (LBP, PP, LBPP) | LBP. | |
| Notes | This paper was part of the journal's 'brief communication' section only, so biases are difficult to assess; there was no reference to other publications on this study and none were identified. Assume the study was carried out in Iran, since all authors were affiliated with Iranian universities. 14 March 2012 ‐ email and Linked‐In message sent to lead author, requesting more information. 10 January 2014 ‐ author sent answer to questions on ROB and copy of paper. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | 'randomly assigned' ‐ details not provided in paper. From author: Randomization was performed using 4 parts, block sealed, sequentially distributed envelopes to which the letters A, B, C and D had been allocated: the letters A and C to the exercise program group and the letters B and D to the control group. |
| Allocation concealment (selection bias) | Low risk | Details not provided in paper. From author: The patients chose one of the envelopes which were opened by the investigator’s colleague and according to the letters, the groups of patients were determined. |
| Blinding of participants and personnel (performance bias) | High risk | Details not provided in paper. From author: therapists were blinded, they were different and knew the groups of women as group 1 and group 2; women were not blinded. |
| Blinding of outcome assessment (detection bias) | Low risk | Details not provided in paper. From author: assessors were blinded, they were different and knew the groups of women as group 1 and group 2. |
| Incomplete outcome data (attrition bias) | High risk | Details not provided in paper, but number randomised are included in the results table. From author: 43 women were selected for the study and 30 women finished the study, and we analysed the 15 [in each group] who finished the study. High risk because > 20% drop‐out rate. |
| Selective reporting (reporting bias) | Low risk | Limited data provided; e.g. states that RMDQ was used, but no values given for this outcome. From author: RMDQ [for pain] and lordosis results provided in the paper forwarded by author. |
| Other bias | Unclear risk | This was part of the journal's 'brief communication' section only, so biases are difficult to assess; there was no reference to other publications on this study and none were identified during a Google search 13 March 2012. In January 2014, author responded to request for more information, which is inserted above. |
| Methods | A prospective, randomised study to compare the efficiency of Kinesio Tape, compared to exercise and acetaminophen (Ex + A) for the treatment of pregnancy‐related LBP during the third trimester of pregnancy. | |
| Participants | Inclusion criteria:
| |
| Interventions | Intervention group: Kinesio Tape (N = 15): no further detail provided. Control group: Ex + A (N = 14): no further detail provided. | |
| Outcomes | Pain: VAS (0 to 10). Functional disability: RMDQ. Outcomes completed before and 7 days after treatment. | |
| Condition (LBP, PP, LBPP) | LBP. | |
| Notes | Poster presentation to the 24th National Physical Medicine and Rehabilitation Congress. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information available from abstract. Abstract only available. |
| Allocation concealment (selection bias) | Unclear risk | No information available from abstract. |
| Blinding of participants and personnel (performance bias) | High risk | Not possible to blind participants and personnel to an exercise intervention, or Kinesio Tape. |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information available from abstract. |
| Incomplete outcome data (attrition bias) | Unclear risk | As above. |
| Selective reporting (reporting bias) | Unclear risk | Only P values provided. Abstract reports a significant decrease in VAS and RMDQ in both groups (P < 0.001) with a significantly greater degree of pain relief in the Kinesio Tape group (P < 0.001). |
| Other bias | Unclear risk | No adverse events of Kinesio Tape reported. No further detail provided about other possible sources of bias. |
| Methods | Prospective randomised study. | |
| Participants | Women were identified via self‐report of LBP symptoms: this was followed up with physical tests of palpation, spinal range of motion and P4 test to rule out PP. N = 88 randomised to 1 of 3 groups. Inclusion criteria:
Exclusion criteria:
| |
| Interventions | TENS (N = 22/20 analysed): dual channel portable TENS, using 4 x 5 cm2 electrodes placed over pain lumbar region. High frequency stimulation to achieve a tingling sensation 2 to 3 times above the sensory threshold. Each participant received 6 treatments (2 x/week for 3 weeks), no detail on duration of each treatment. Exercise (N = 22/19 analysed): HEP prescribed by a physiotherapist incorporating pelvic tilting, lower limb stretching, postural exercises, isometric abdominal contractions. Each exercise to be completed 10 times, twice a week for 3 weeks. Acetaminophen (N = 22/19 analysed): 1 500 mg paracetamol tablet 2 x/day for 3 weeks. Control group (N = 22/21 analysed): usual prenatal care | |
| Outcomes | The following outcomes were collected at baseline and 3 weeks' after treatment. Pain: VAS (0 to 10); functional disability (RMDQ); palpation of symphysis pubis, sacroiliac joint and gluteal regions for tenderness/reproduction of symptoms. | |
| Condition (LBP, PP, LBPP) | LBP. | |
| Notes | Study conducted at Department of Obstetrics and Gynecology, Fatih University, Turkey. No funding information provided. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were divided randomly into 1 of 4 groups, by drawing a sealed opaque envelope with group names ‐ prepared by 1 author and opened by another. |
| Allocation concealment (selection bias) | Low risk | Sealed opaque envelopes, prepared by 1 of the authors of the study from a box containing group names, opened by another study author who was blinded to the contents of the envelope. |
| Blinding of participants and personnel (performance bias) | High risk | Participants could not be blinded nor could providers due to nature of interventions. |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information provided on blinding of outcome assessment. An experienced physical medicine and rehabilitation specialist carried out the physical assessments, i.e. palpation, ROM, posterior pain provocation tests, however unclear whether this person also collected pain and disability assessments. |
| Incomplete outcome data (attrition bias) | Low risk | Attrition and exclusions reported with number and reasons provided. Numbers included in the analysis at each stage add up. Authors did not specifically indicate how they dealt with missing data however, given that analyses were conducted on those participants completing the 3‐week study period only, it appears they completed a PPA. (Small numbers did not complete the 3 week study period from each group; N = 2 TENS; N = 3 acetaminophen; N = 3 exercise; N = 1 control). |
| Selective reporting (reporting bias) | Unclear risk | Median scores provided as along with P values for both pain (VAS) and disability (RMDQ). |
| Other bias | Low risk | 3 women reported adverse events. Groups similar at baseline for all variables with the exception of VAS, which was higher in the TENS and acetaminophen groups at baseline. Compliance reported as > 90% in all groups. No information about controlling for co‐interventions. |
| Methods | Preventive RCT. | |
| Participants | Women registering at 1 of 6 maternity clinics (N = 967) run by Falun County Health Care Board in Sweden and had their ultrasound between gestational age 15 to 18 weeks. Inclusion criteria:
Exclusion criteria:
Drop‐outs due to inability to participate in water gymnastics, recurrent UTIs, shift work, baby‐sitting problems, miscarriage, intrauterine death, lack of time, invited to participate after date of closure. | |
| Interventions | Intervention group (N = 129/123 analysed): Control group (N = 129/118 analysed): no water gymnastics. | |
| Outcomes | LBP (VAS 0 to 10). (LBP was not measured until 1 week postpartum, which is outside the timelines of this review); number of days off work because of LBP in pregnancy. Adverse events: no excess risk for pregnancy associated with water gymnastics observed: no differences with gyn/UTI infections, maternal weight gain, gestational age at delivery, weight/height of neonate, delivery characteristics. | |
| Condition (LBP, PP, LBPP) | LBP. | |
| Notes | Funding: Dalarna Research Institute; Local Insurance Office. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | 'Preventive randomised controlled trial' randomised 'using sealed envelopes' ‐ actual method of randomisation not described, but it was conducted 'by a mid‐wife when the women had their ultrasound.' |
| Allocation concealment (selection bias) | Low risk | Adequate ‐ sealed envelopes. |
| Blinding of participants and personnel (performance bias) | High risk | Participants and caregiver not blinded. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Assessor blinding unclear. |
| Incomplete outcome data (attrition bias) | High risk | Participants who completed the study were analysed in the groups to which they were randomised; less than 5% reported as lost to follow‐up; numbers do not always add up ‐ query if N for outcomes are based on those who answered specific questions on follow‐up?. |
| Selective reporting (reporting bias) | High risk | Not enough data were given to allow use of the VAS; pain data provided in graphs from which one cannot extract exact values. Difficult to follow the path of recruitment, drop‐outs since numbers given in text do not add up. |
| Other bias | Low risk | Nothing noted. |
| Methods | RCT (N = 50 women). | |
| Participants | South African women of 20 to 40 years between 16 and 24 weeks' gestation; LBP/PP (with or without radiation to the knee) that had started during current pregnancy (72% of sample had LBP). | |
| Interventions | Intervention group (N = 26/24 analysed): exercise. 1 formal exercise class lasting 30 to 45 minutes with warm‐up and cool‐down periods incorporated. Handout illustrating and explaining the exercise program which consisted of postural, transversus abdominis and pelvic floor exercises to train correct isolation and isometric contraction. Exercises then individually progressed to increase level of difficulty and facilitate co‐contraction of transversus abdominis and PFM with gluteals, quadriceps and other muscle groups. Follow‐up class every second week for 10 weeks. Women also asked to complete a daily HEP and record their goals in their training diary. Verbal information on basic back care and posture during pregnancy and an information pamphlet. Control group (N = 24/22 analysed): verbal information on basic back care and posture during pregnancy and an information pamphlet as for exercise group but no specific instructions given to participants regarding whether to perform any exercise. | |
| Outcomes | Pain intensity (NRS 0 to 10); functional ability (Likert modified RMDQ). | |
| Condition (LBP, PP, LBPP) | LBPP. | |
| Notes | Neurological exam was completed at assessment along with erector spinae palpation, sacroiliac palpation, P4 test and passive SLR however, apart from erector spinae palpation eliciting LBP symptoms, the positive yield of these tests for subtyping of symptoms was low. Conducted in South Africa. Funding not reported. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random numbers in balanced blocks of 20. |
| Allocation concealment (selection bias) | Low risk | Sealed numbered opaque envelopes. |
| Blinding of participants and personnel (performance bias) | High risk | Unblinded. |
| Blinding of outcome assessment (detection bias) | High risk | Unblinded. |
| Incomplete outcome data (attrition bias) | Low risk | ITT analysis completed; less than 10% of sample lost to follow‐up. |
| Selective reporting (reporting bias) | Low risk | Outcomes reported as specified. |
| Other bias | Low risk | Groups similar at baseline regarding most important prognostic indicators; outcomes assessed at same time for both groups; compliance reported in detail. |
| Methods | RCT conducted at the obstetric clinic of the Imam Hospital Complex, Tehran. Women randomly allocated into 1 of 3 groups; Exercise plus information (Ex), Lumbo‐pelvic belt plus information (Belt), or Information only (Control). | |
| Participants | Inclusion criteria:
Diagnosis of PGP based on self‐reported pain (using a pain diagram) in the lumbar region between the gluteal folds and the posterior iliac crest, and a positive result from 1 of the following physical tests:
Exclusion criteria:
| |
| Interventions | Intervention group 1 (Ex) (N = 35/31 analysed): in addition to information provided to control group, this group were given a HEP including exercises to strengthen the pelvic girdle muscles, such as back pressing, pelvic tilting, leg‐lifting each held for 3 to 10 seconds and completed twice a day, 3 days per week; to encourage aerobic activity of at least 64 to 76% of their maximum heart rate for 25 minutes/day x 3 per week, e.g. walking, and stretching exercises for the lower limbs and trunk each held for 10 to 20 seconds and completed twice a day, 3 to 5 x per week. Intervention group 2 (Belt) (N = 35/34 analysed): in addition to information provided to control group, this group received a non‐rigid lumbo‐pelvic belt and asked to use it throughout the course of the study with the exception, should they wish, to remove it for sleeping. Control group (N = 35/31 analysed): this group received general information about the anatomy, body posture and ergonomic advice about sitting, walking and lying. | |
| Outcomes | Primary outcomes: pain intensity (VAS 0 to 100); functional disability (Validated Persion version of ODI). Secondary outcomes: Quality of Life (World Health Organisation's Quality of Life Questionnaire) ‐ this covers physical and psychological health along with social and environmental conditions. All outcomes assessed at baseline, week 3 and week 6 of the study. | |
| Condition (LBP, PP, LBPP) | PP. | |
| Notes | Funding = Tehran University of Medical Sciences. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated block randomisation sequence (block sizes 15 participants each). |
| Allocation concealment (selection bias) | Unclear risk | No information provided about allocation concealment. |
| Blinding of participants and personnel (performance bias) | High risk | No information provided about blinding; however participants and providers knew interventions. |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information provided about blinding. Not even clear who collected the outcomes. |
| Incomplete outcome data (attrition bias) | Low risk | Attrition and exclusions were presented along with reasons, and numbers included in the analysis at each stage add up. The authors are not clear about how they dealt with missing values but appear to have used a per protocol analysis as those lost to follow‐up are excluded from the final analyses. Control and exercise had 11% drop‐out; belt group had only 3% drop‐out. |
| Selective reporting (reporting bias) | Low risk | Means and SDs for each group along with 95% CIs provided for the primary and secondary outcomes at all time points along with P values. Comparisons are also presented to identify where the significant differences occur, i.e. between which groups. |
| Other bias | Low risk | Use of pain provocation tests as well as self‐report to diagnose PP increases validity of diagnosis. No significant differences in any of the primary or secondary outcomes at baseline. Adverse events described (one participant each in control and exercise group). No information presented on participants' use of co‐interventions or researchers attempts to control for these. |
| Methods | 100 women, enrolled and randomised to 1 of 2 groups. The code for group allocation was obtained in advance by throwing dice in pairs of 10, and enclosed in advance in an envelope, marked with the order number of inclusion and opened consecutively by midwife on inclusion to the study. Duration of study or follow‐up not given. | |
| Participants | Pregnant women presenting at the maternity ward centres in southern Sweden. Inclusion criteria:
Exclusion criteria:
Baseline: | |
| Interventions | Intervention group (N = 50/37 analysed): Acupuncture given according to written instructions and periosteal stimulation. Started with LR3 and GV20 points + local tender points, added BL60, SI3 and 1 of lumbar and sacral bladder points (BL22 to 26) if needed; stimulated to De qi, needles left in place for increasing length of time. Control group (N = 50/35 analysed): usual prenatal care. | |
| Outcomes | Pain increased, pain unchanged, pain decreased, no pain during last 3 weeks of pregnancy, pain on activity decreased, Visits to maternity centres, number of participants who used analgesics, number of participants who used TENS, number of participants who used sacroiliac belt, number of participants who used physiotherapy, baby's birthweight, baby's Apgar at 1/5/10 minutes. Adverse events: reported by 38% of acupuncture group ‐ local pain (6); heat or sweating (5); local haematoma (2); tiredness (2); nausea (2); weakness (1). | |
| Condition (LBP, PP, LBPP) | LBPP. | |
| Notes | No mention of funding. Study took place in Sweden. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | ‘code for group obtained in advance by throwing dice in pairs of 10.’ |
| Allocation concealment (selection bias) | Low risk | 'Predetermined code enclosed in advance in envelop, marked with the order number of inclusion and opened consecutively by midwife on inclusion.' |
| Blinding of participants and personnel (performance bias) | High risk | No explicit mention in the report, but it seems unlikely that either the women, midwives or acupuncturists were unaware of inclusion into the acupuncture or control group. |
| Blinding of outcome assessment (detection bias) | Low risk | 'two blinded investigators independently assessed the development of the patients' individual VAS scoring over time with a kappa coefficient of 0.68% (95% CI 0.54 to 0.83).' |
| Incomplete outcome data (attrition bias) | High risk | Over 20% lost to follow‐up in each group. 1 ward closed to recruitment after 12 months because women no longer wished to be included in the study => excluded 12 participants who had been enrolled by this clinic, leaving 44 in each group. Acupuncture group ‐ lost 3 because they delivered, 2 did not like acupuncture, 1 did not complete assessment correctly, 1 lost due to vacation of midwife (7) ‐ analysed 37/50. Control group ‐ lost 5 ‐ did not complete forms correctly, 3 insisted on acupuncture, 1 was admitted to hospital for pain management and rest (9) ‐ analysed 35/50. |
| Selective reporting (reporting bias) | High risk | Data provided on outcomes listed in methods section but at times they are difficult to follow and not presented in a fashion that allow analyses. |
| Other bias | High risk | Variety of other treatments used by the women to relieve symptoms (analgesics, TENS, pelvic belt, physio); length of study unclear. |
| Methods | RCT; N = 146 randomised (group 1: N = 49; group 2: N = 48; group 3 (controls): N = 49). Participants stratified by age and gravida. | |
| Participants | Inclusion criteria:
Exclusion criteria:
| |
| Interventions | Intervention group 1 (N = 49 randomised): usual obstetric care plus Osteomanipulative Therapy (OMT). Intervention group 2 (N = 48 randomised): usual obstetric care plus sham ultrasound (sham US). Control group (N = 49 randomised): usual obstetric care. Groups 1 and 2 received treatments each lasting 30 minutes at 30, 32, 34, 36, 37, 38, 39 weeks' gestation (in conjunction with usual obstetric care). OMT = included any of the following modalities: soft tissue, myofascial release, muscle energy, range of motion mobilisations used in a systematic manner by all providers*. No manipulations used as these pose a risk to mother and fetus. Sham US = using a non‐functional ultrasound (US) therapy unit that provided the usual visible and auditory cues provided by a normal therapeutic ultrasound unit. The US head was applied over clothing at body areas corresponding to the OMT protocol. Usual obstetric care = no study treatments provided but usual 7 visits in total, in accordance with usual obstetric care, at 30, 32, 34, 36, 37, 38, 39 weeks' gestation. | |
| Outcomes | Average pain intensity: NRS (0 to 10). Back‐specific function (RMDQ) measured at baseline and after 7th (last) treatment session; at same times for each group. | |
| Condition (LBP, PP, LBPP) | LBP. | |
| Notes | *Treatment providers met regularly to ensure consistency in duration, type, anatomic location and manner of OMT provided. OMT and Sham US provided by same physicians with same amount of attention given to both groups. 2 from each treatment group missed more than 50% of treatments. Compliance best in control group. Funding = grants from the Osteopathic Heritage Foundation and the National Center for Complementary and Alternative Medicine at the National Institutes of Health. The study took place in Texas, USA. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Patients randomly assigned and stratified by age and gestation, but no other information given about the sequence generation. |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information given. |
| Blinding of participants and personnel (performance bias) | High risk | Not possible to blind patients or care providers. |
| Blinding of outcome assessment (detection bias) | High risk | Outcome measures were by self‐report, but high risk because patients not blinded. |
| Incomplete outcome data (attrition bias) | High risk | ITT analysis = 144 participants; last observation carried forward, attrition and exclusions reported but query the reliability of imputing over 1/2 of the data (actual data for 146 ‐ 83 = 63). (23 (16%) withdrew before visit 7; a further 60 (42%) withdrew due to delivery). Adherence reported as greater than 80% in both treatment groups for those who continued the intervention. |
| Selective reporting (reporting bias) | Low risk | Several approaches used to decrease risk of bias from last observation carried forward method. |
| Other bias | Low risk | Similar compliance in treatment groups, baseline measurements similar, co‐interventions controlled, outcomes taken at same time points. |
| Methods | Prospective single‐blind RCT. Women recruited from 2 different maternity healthcare departments and randomised to superficial or deep acupuncture. 106 women examined; 70 women randomised; 23 dropped out; analyses conducted on 47 women who completed the study. | |
| Participants | Inclusion criteria:
Physical examination confirming provoked PP: (i) In 1 of 3 tests: P4 test, standing on 1 leg, Patrick’s/Fabere test; (ii) In palpating tissue over: the sacroiliac joints, the symphysis pubis, or Gluteus maximus/medius muscles. Exclusion criteria:
| |
| Interventions | Intervention group (N = 35/25 analysed): deep stimulation acupuncture. 10 acupuncture treatments of 30 minutes each, given twice weekly for 5 weeks by a registered physiotherapist. See study for exact location of acupuncture points used. Control group (N = 35/22 analysed): superficial stimulation acupuncture. 10 acupuncture treatments of 30 minutes each, given twice weekly for 5 weeks by a registered physiotherapist. See study for exact location of acupuncture points used. | |
| Outcomes | VAS pain (at rest and during 3 daily activities); Nottingham Health Profile measured 5 days prior to and 5 days after treatment; at same time for both groups. | |
| Condition (LBP, PP, LBPP) | PP. | |
| Notes | Funding = research grants from Praktikertjänst AB and the National Security in Sweden. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | 'women ... were randomised ...' but randomisation procedure not described. Unclear risk ‐ as above, randomisation procedure not explained. |
| Allocation concealment (selection bias) | Low risk | Quote: 'Sealed envelopes with labels for determination of treatment were used in randomisation provided by a statistician not involved in the study'. |
| Blinding of participants and personnel (performance bias) | Low risk | Both groups given acupuncture so could not tell difference as patients were acupuncture naive; care providers knew whether they gave superficial or deep acupuncture but acted the same towards the patient regardless. |
| Blinding of outcome assessment (detection bias) | Low risk | Self‐reported outcomes collected from patients who were unaware of their treatment group. |
| Incomplete outcome data (attrition bias) | High risk | Drop‐out rate: 23 participants out of 70 (13 in Superficial group, 10 in Deep group). Reasons for drop‐outs listed; reasons similar for both groups. It does not seem that the grouping affected the drop‐out reasons, and although almost 1/3 dropped out from each group, the over‐riding reason was non‐compliance with completing pain diaries. No excluded data mentioned ‐ and it appears that analyses only done on complete data sets. |
| Selective reporting (reporting bias) | Low risk | Study reported all outcomes it said it would report in methods. |
| Other bias | Low risk | No other bias. Women all acupuncture naive. Groups similar at baseline. |
| Methods | 'Randomised controlled study'. The physiotherapist conducting the research randomised the women into 2 groups by means of a 'raffle' or 'lottery'. | |
| Participants | Inclusion criteria:
Exclusion criteria:
| |
| Interventions | Intervention group (N = 33 randomised/analysed): exercises in groups for 'global activity and stretching'. Control group (N = 36 randomised/analysed): routine medical recommendations. | |
| Outcomes | Proportion of women with improvement in VAS categorised as VAS = 0; 1 to 3; 4 to 5; 6 to 8; 9 to 10 after 8 weeks. Adverse events: not reported. | |
| Condition (LBP, PP, LBPP) | LBPP. | |
| Notes | Funding: not reported. Translated from Portugese by single Portuguese researcher. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Used a 'Raffle' or 'lottery'. |
| Allocation concealment (selection bias) | High risk | Physiotherapist who was doing the research allocated to groups. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Description of blinding for participants, caregiver not provided. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Description of blinding for assessors not provided. |
| Incomplete outcome data (attrition bias) | High risk | Outcome table appears to indicate no drop‐outs; report appears to indicate that there is no contamination between groups, but none of this is clearly described. |
| Selective reporting (reporting bias) | High risk | Results are incomplete (only intervention group's improvement reported, no data for control group). |
| Other bias | High risk | Other treatments not described; baseline data were not comparable: Exercise group = 48% greater than 5 on VAS 0 to 10; Usual care group = 61% greater than 5 on VAS 0 to 10. |
| Methods | Randomised controlled clinical trial (N = 60 randomised). Study conducted in 'Basic Healthcare Units' in São Paulo, Brazil. | |
| Participants | Inclusion criteria:
For women reporting LBP only, an increase in pain precipitated by bending forward, circling the trunk or on palpation of paraspinal muscles confirmed the diagnosis. The 4P test was used to assist diagnosis of PGP. Exclusion criteria:
| |
| Interventions | Intervention group (N = 30/21 analysed): Hatha yoga. 10 sessions, once a week, each lasting 1 hour (up to 10 participants/group). Class consisted of a 10‐minute warm‐up to gain focus, 40 minutes of poses and breathing exercises focusing on stretching, strengthening, endurance, muscle resistance, self‐control, concentration and self‐confidence, and a 10‐minute relaxation at the end. Control group (N = 30/24 analysed): information pamphlet on postural orientation and advice on ADL's, sleeping positions sitting with adequate foot and lumbar support, | |
| Outcomes | Pain intensity (VAS 0 to 10) with facial expressions positioned at 3 points on the scale corresponding to weak/median/severe pain. This was assessed at the beginning and end of each yoga session. 4P test, lumbar flexion test. | |
| Condition (LBP, PP, LBPP) | LBPP. | |
| Notes | Study conducted in Brazil; part of Doctoral thesis. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated list of random numbers for 60 participants using SAS software. |
| Allocation concealment (selection bias) | Low risk | Sealed, opaque, sequentially numbered opaque envelopes. |
| Blinding of participants and personnel (performance bias) | High risk | No detail provided on blinding. however it is not possible to blind a yoga intervention. there was also no mention of whether participants were yoga naive. |
| Blinding of outcome assessment (detection bias) | Unclear risk | No detail provided on blinding of outcome assessment. |
| Incomplete outcome data (attrition bias) | High risk | Attrition and exclusions were reported along with reasons, and the numbers included in the analysis add up. Lost to follow‐up: N = 9 in the yoga group, N = 6 in the control group, therefore risk is high (20%+). |
| Selective reporting (reporting bias) | High risk | The sample included N = 10 (17%) with LBP, N = 12 (20%) PGP, and N = 38 (63%) with LBPP however the authors did not present baseline data according to intervention groups and did not present any findings for those who had combined LBPP. |
| Other bias | Unclear risk | Adverse events were described and similar between groups. Interim data collection was not completed for control group, just the intervention group. |
| Methods | Prospective RCT conducted at the Women's Integral Health Care Hospital, University of Campinas, Sao Paulo and 4 municipal primary healthcare centres in Sao Paulo, Brazil. | |
| Participants | Inclusion criteria:
Exclusion criteria:
| |
| Interventions | Intervention group (N = 103/97 analysed): Birth Preparation Program (BPP). HEP including pelvic floor muscle contractions, daily aerobic exercise encouraged, 2 stretches to decrease back pain, information about the physiology of labour and practice of non‐pharmacological techniques for pain control. Control group (N = 102/100 analysed): routine information about breastfeeding, signs and symptoms of labour and a visit to the delivery ward. Supervised practice of the HEP (experimental group) only occurred on the days of scheduled medical visits, which were monthly up until 30 weeks' gestation, fortnightly between 31 to 36 weeks' and weekly from 37 weeks onwards. | |
| Outcomes | Primary outcomes: average LBP/PP during preceding days (VAS 0 to 10) and marking of pain location on body chart; urinary incontinence; physical activity performed at home (PPAQ); anxiety (STAI). Secondary outcomes: perinatal variables. | |
| Condition (LBP, PP, LBPP) | LBPP. | |
| Notes | Financial support was provided by the Foundation for the Support of Research of the State of São Paulo (Fundação de Amparo à Pesquisa do Estado de São Paulo–FAPESP) grant #08/10392‐5. The first author received partial financial support from the Coordination for the Improvement of Higher Education Personnel (CAPES). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random sequence of numbers. Randomisation was 1:1. |
| Allocation concealment (selection bias) | Low risk | Sealed opaque, consecutively numbered envelopes prepared by an individual not directly involved with the study. |
| Blinding of participants and personnel (performance bias) | High risk | Authors acknowledge in the discussion that lack of participant blinding may have led to women giving what they felt were favourable answers to the questions about urinary incontinence and physical activity completed. |
| Blinding of outcome assessment (detection bias) | High risk | No information provided on outcome assessor or analyst; participants provided self‐assessment data. |
| Incomplete outcome data (attrition bias) | Low risk | Attirtion and exclusion reported with reasons and numbers included in the analysis add up. ITT analysis completed, with participants analysed according to group assignment but final analyses only included those who completed study. |
| Selective reporting (reporting bias) | Low risk | All data presented as per methods with number (%) of participants, means (+/‐ SD) and 95% CIs for VAS (LBP/PP) at 3 time points, and RR (95% CI) for prevalence of LBP or PP. Only missing data for secondary outcomes. |
| Other bias | Low risk | Co‐interventions controlled between groups. Groups similar at baseline and weight gain during course of study similar between groups. Collection of outcomes at 3 time points (same for each group). |
| Methods | RCT conducted at Trondheim University Hospital and 3 outpatient physiotherapy clinics. 1533 pregnant women in and around Trondheim, Norway were invited to join => 301 were randomised. Primary outcome was prevention and treatment of urinary incontinence; secondary outcome was prevention and treatment of LBPP. | |
| Participants | Inclusion criteria:
Exclusion criteria:
| |
| Interventions | Intervention group ‐ exercise training (N = 148 randomised/analysed): Training with a physical therapist in groups of 10 to 15 women for 60 minutes once per week for 12 weeks, where training focused on PFM and other exercises. Control group ‐ usual prenatal care (N = 153 randomised/analysed): Women received customary information given by their midwife or general practitioner. They were not discouraged from exercising on their own. | |
| Outcomes | Self‐reported pain in the low‐back area lasting for ≥ 1 week; pain drawing, off sick due to low‐back/PP (yes/no); Disability Rating index (DRI); pelvic floor muscle strength measured at baseline (20 weeks' gestation); 36 weeks' gestation, 3 months' postpartum. | |
| Condition (LBP, PP, LBPP) | LBPP. | |
| Notes | Adherence to training protocol was registered based on the women’s personal training diary (must do 2 sets of 8 to 12 contractions of PFM per day) and reports from the physical therapists that led the group training (participation in ?6 group training sessions). Funding = Norwegian Fund for Postgraduate Training in Physiotherapy and the Norwegian Women's Public Health Association. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: 'Randomisation was done in blocks of 32 with the use of opaque sealed envelopes', did not specify method used to select the blocks, but likely OK, given the fact that they used other safeguards. |
| Allocation concealment (selection bias) | Low risk | Opaque sealed envelopes used. Quote: 'A secretary with no other involvement in the study prepared the envelopes. Each woman opened 1 of the envelopes herself and was enrolled by the secretary in the secretary's office'. |
| Blinding of participants and personnel (performance bias) | High risk | Participants and care providers were aware of treatments (exercise vs usual care). |
| Blinding of outcome assessment (detection bias) | Unclear risk | Quote: 'The principal investigator was not involved in the training of the women and was blinded to group allocation while making the assessments and plotting the data'. However, the outcomes were self‐report and the women were not blinded to their treatment; unclear if those who received usual care were aware of other options. |
| Incomplete outcome data (attrition bias) | Low risk | 7 participants in control and 5 in training group withdrew after the first assessment. Reasons for withdrawal were diseases connected to pregnancy (N = 6) or personal reasons (N = 6). It does not seem that the grouping affected the drop‐out reasons. No excluded data mentioned. |
| Selective reporting (reporting bias) | Low risk | Study reported all outcomes it said it would report in methods. |
| Other bias | Unclear risk | Unclear risk: Influence of co‐interventions, adherence not reported in results. |
| Methods | 'Randomized controlled clinical trial based on the classical 'waiting list' design. Carried out by 2 osteopaths in their offices in Űberlingen and Műlheim, Germany. 60 pregnant women were recruited from 'a number of midwives and gynaecologists.' | |
| Participants | Inclusion criteria: Pregnant women with LBPP that had lasted at least a week and was at least VAS > 3. Average age 30 years, mean gestation 25 weeks. | |
| Interventions | Intervention group (N = 30 randomised/analysed): received 4 osteopathic treatments in weekly intervals. Waiting list (control) group (N = 30/27 analysed), after 5 weeks on the waiting list they received osteopathic treatment that was reported as 'having no relevance for the study'. | |
| Outcomes | Pain, measured with VAS; interference with ADL, measured with Quebec Back Pain Disability Scale at baseline and end of first 5 weeks (end of treatment for intervention group). | |
| Condition (LBP, PP, LBPP) | LBPP. | |
| Notes | Information taken from an abstract of an unpublished thesis that is available in German, for a cost, from Akademie für Osteopathie (AFO), Deutschland (funds not available to obtain full manuscript). Funding not reported. Abstract initially translated from German by single German‐speaking researcher, then English abstract found on‐line. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | 'Randomized controlled clinical trial' ‐ methodology not reported in abstract. |
| Allocation concealment (selection bias) | Unclear risk | Waiting list comparison group, after 5 weeks waiting list they get a treatment that is reported as having no relevance for the study. |
| Blinding of participants and personnel (performance bias) | Unclear risk | No mention of blinding in abstract. |
| Blinding of outcome assessment (detection bias) | Unclear risk | No mention of blinding in abstract. |
| Incomplete outcome data (attrition bias) | Unclear risk | 3 patients in the control group dropped out; no information provided on exclusions or analyses. |
| Selective reporting (reporting bias) | Low risk | Data provided for pain and Quebec Back Pain Disability Scale. |
| Other bias | Unclear risk | Difficult to assess since we were unable to access the full thesis. |
| Methods | Pilot RCT (57 participants randomised). All participants screened initially by phone and all treatments described prior to randomisation. No limit on what stage in pregnancy women could enter the study. Before randomisation all participants identified their treatment preference. | |
| Participants | Inclusion criteria:
Exclusion criteria:
| |
| Interventions | Exercise group (control; N = 22/16 analysed): exercise booklet provided with specific exercises and recommendations for postural and movement patterns to alleviate LBP, and advice on when to stop exercising. Individualised stretching and strengthening exercises were prescribed, demonstrated and practiced at each study visit. Exercisies took approximately 15 minutes to perform and participants were asked to exercise 5 x/week. Spinal manipulative therapy (N = 15 randomised/analysed): high velocity, low amplitude thrust applied to isolated joint to move it just past physiological end range in side‐lying position. Direction, velocity and amplitude determined by the clinician from palpation findings. Neuro emotional technique (NET; N = 20/19 analysed): chiropractic mind‐body technique using relaxed breathing and visualisation techniques with elements of traditional Chinese medicine (such as association of emotions with certain organs or meridians) and chiropractic medicine (adjustment of spinal levels innervating specific organs. The NET standard protocol was followed (Bablis 2008). Maximum number of treatments per participant = 8 with very few in any group reaching this amount. Co‐interventions controlled. | |
| Outcomes | Primary outcome: RMDQ (back‐specific function). Secondary outcome: Pain intensity (NRS 0 to 10); Sick leave due to pregnancy‐related LBP (assessed but not listed as 1 of the outcomes). | |
| Condition (LBP, PP, LBPP) | LBP. | |
| Notes | 138 participants screened; sick leave not listed in methods as one of the outcomes but reported in Table 2; higher drop‐out from exercise group however adherence to exercise did not affect outcomes. Funding provided by The One Foundation, the research division of the Neuro Emotional Technique; 'The One Foundation did not contribute to the study in any other way'. Conducted at Oregon Health & Science University, USA. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The method used to generate the allocation sequence was not described ‐ 'before being randomised, participants identified their treatment preference ... she would open the consecutive envelope in her preference strata in the presence of the researcher ... women were randomly allocated into 1 of 3 treatment groups'. |
| Allocation concealment (selection bias) | Low risk | 'the randomisation schedule was completed prior to initiating the study and was concealed from all study staff by using consecutively numbered, sealed, opaque envelopes for each strata of preference group.' |
| Blinding of participants and personnel (performance bias) | High risk | Participants and practitioners were not blinded to treatment group after randomisation. |
| Blinding of outcome assessment (detection bias) | High risk | Participants were outcome assessors. |
| Incomplete outcome data (attrition bias) | Low risk | ITT analysis performed. Missing data ‐ last observation carried forward. Minor inaccuracies noted in number excluded prior to randomisation, and between text and Figure 1 in drop‐outs from exercise group (N = 1). |
| Selective reporting (reporting bias) | Low risk | Last observation carried forward may limit data but carried out to replicate methods used in an earlier study by Licciardone and colleagues (2010). Sensitivity analysis completed providing similar results to primary outcome analysis. |
| Other bias | High risk | Participants randomised according to their treatment preference, entered the study at different gestational points, groups were not similar at baseline for all prognostic factors, and were paid to participate (USD$20 per visit). |
| Methods | 'Prospective randomised controlled study'. 100 women invited and divided into 2 groups; 10 withdrawn from exercise group prior to intervention => 90 analysed. | |
| Participants | Inclusion criteria:
Exclusion criteria:
| |
| Interventions | Intervention group (Exercise program): N = 50/40 analysed. Program consisted of a 15‐minute warm‐up and cool‐down plus 30 minutes cycling in the range of 55% to 65% of the maximal heart rate with respect to the age. Exercises were prescribed by a physical training specialist. The exercise sessions were 3 times a week for 8 weeks. Control group: N = 50 randomised/analysed. The study did not specify what the control group was. | |
| Outcomes | Pain, measured with Quebec questionnaire, measured at baseline and 8 weeks after start of program; demographic data collected at baseline; P value < 0.05 considered to be statistically significant. | |
| Condition (LBP, PP, LBPP) | LBP. | |
| Notes | Email to the corresponding author for clarification failed to elicit a response. Funding = grant from Sports Medicine Research Center and Vice Chancellor for Research at Tehran University of Medical Sciences. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No description of sequence generation were described except 'the total numbers of 100 invited were divided into two exercise and control groups'. 'Randomised' was only mentioned in the abstract. Unclear risk: randomisation procedure not described. |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned. |
| Blinding of participants and personnel (performance bias) | High risk | Not mentioned, but assume not. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not mentioned. |
| Incomplete outcome data (attrition bias) | High risk | Quote: 'every woman missing three session of exercise was excluded from the study' ‐ but unclear how many this affected. Drop‐outs/withdrawals from study not mentioned, however, 10 women who were randomised did not proceed to the intervention because they were unable to participate in the exercises. Did not specify how they dealt with the missing/excluded data. |
| Selective reporting (reporting bias) | Low risk | Study reported all outcomes it said it would report in methods. |
| Other bias | Unclear risk | Unclear risk: compliance not reported, nor co‐interventions. |
| Methods | 2‐armed, 2 centre RCT ‐ 855 women randomised. | |
| Participants | Inclusion criteria:
Exclusion criteria:
| |
| Interventions | Intervention group (N = 429/396 analysed): exercise. 60‐minute exercise sessions 1 x/week for 12 weeks between 20 to 36 weeks' gestation led by a physiotherapist in groups of 8 to 15 participants. Each session consisted of moderate intensity (13‐14 on Borg scale) aerobic activity, strength training and balance exercises. 45‐minute home exercise session 2 x/week consisting of 30 minutes of aerobic activity and 15 minutes of strengthening and balance exercises. Adherence monitored throughout. Control group (N = 426/365 analysed): standard antenatal care; not discouraged from exercising. Both groups given written information on pelvic floor exercises, diet and pregnancy‐related LBPP. | |
| Outcomes | LBPP: VAS (0‐100) ‐ morning and evening, sick leave due to lumbo‐PP, Disability Rating Index (DRI), Fear Avoidance Beliefs Questionnaire. | |
| Condition (LBP, PP, LBPP) | LBPP. | |
| Notes | Additional outcomes related to a related study: gestational diabetes, glucose metabolism. Approximately 60% of women who enrolled reported lumbo‐PP at time of inclusion. Funding sources: Norwegian University of Sciences and Technology, Norweigian Fund for Postgraduate Training in Physiotherapy, Liason Committee for Central Norway Regional Health Authority. 30 October 2012 ‐ email sent to lead author to clarify correct number analysed in the intervention group ‐ 396 or 397; author confirmed that there were 396 women in the intervention group. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computerised randomisation. |
| Allocation concealment (selection bias) | Low risk | 'concealed randomisation' by a web‐based computerised procedure; ... personnel had no influence over randomisation.' |
| Blinding of participants and personnel (performance bias) | High risk | While personnel had no influence over the process of randomisation, the physiotherapists who delivered the programmes were aware of the end results ... i.e. they were providing the participants with the intervention. |
| Blinding of outcome assessment (detection bias) | High risk | Outcomes were self‐reported symptoms, therefore the women were the outcome assessors and they knew whether they were receiving exercise therapy or not. |
| Incomplete outcome data (attrition bias) | High risk | Exercise group = 8% drop‐out/loss to follow‐up; control group = 14% drop‐out/loss to follow‐up with a large proportion of these giving no reason and not included in the analysis. |
| Selective reporting (reporting bias) | Low risk | All outcomes reported as specified in methods. |
| Other bias | Low risk | Groups similar at baseline even when not including those lost to follow‐up. Co‐interventions avoided or similar between groups and compliance with exercise assessed against specified level of 3 x/week. Timing of outcome assessment same for both groups. |
| Methods | 74 women were allocated to experimental or control groups by using a 'random sampling technique' (no description). | |
| Participants | Inclusion criteria:
Exclusion criteria:
Women were similar at baseline for all factors except job activities: exercise group sat more often at work (N/S); control group stood more often at work and income: exercise group were in higher paid jobs than the control group (P = 0.008). | |
| Interventions | Intervention group (N = 37/32 analysed): exercise. Control group (N = 37/35 analysed): no treatment (nothing noted in article). | |
| Outcomes | Pain improved, pain worsened, pain measured with VAS, gestational age at birth, baby's Apgar score at 1 minute, baby's Apgar score at 5 minutes. Adverse events: 'no negative effects on mother or fetus; no preterm labour; no premature rupture of membranes'. | |
| Condition (LBP, PP, LBPP) | LBP. | |
| Notes | Numbers are not consistently reported throughout the article; total number of participants seems to range from 73 to 84, with most mention of 74 randomised, which is the number we used. Data needed for the meta‐analyses appeared to be incorrectly reported in the paper and were re‐analysed. Funding: not mentioned. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | ‘random sampling technique’ but not described; in discussion section, the authors state 'the inclusion and exclusion criteria were used to match these two groups as closely as possible and scrutinize the variables that may contribute to the impact of physical conditioning or pregnancy outcomes'... which doesn't sound like 'randomisation'... |
| Allocation concealment (selection bias) | Unclear risk | Unclear ‐ 'allocated to experimental or control groups'. |
| Blinding of participants and personnel (performance bias) | High risk | No blinding of participants or providers. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Unclear about outcome assessors. |
| Incomplete outcome data (attrition bias) | High risk | 17% loss of participants from control group; 24% loss of participants from intervention group; details for withdrawals not clearly described. Analysis on 67 completers only. |
| Selective reporting (reporting bias) | Low risk | Reported on LBP for mothers, 1‐minute and 5‐minute Apgar scores and birthweight of babies. |
| Other bias | Unclear risk | Exercise diary kept and checked by exercise instructor; co‐interventions not described. |
| Methods | RCT conducted at Yale‐New Haven Hospital, USA. Women recruited by prenatal healthcare providers in the area; women called the hotline and spoke with the research assistant. N = 159 women randomised/152 analysed. | |
| Participants | Inclusion criteria: Pregnant women; between 25 to 38 weeks' gestation; LBP and/or posterior PP. Exclusion criteria:
All patients acupuncture naive. Drop‐outs and exclusions reported with reasons. | |
| Interventions | Intervention group 1 (N = 58 randomised): auricular (ear) acupuncture x 7 days plus self‐care (AA). Used specific acupuncture points (kidney, analgesia, shenmen). Intervention group 2 (N = 54 randomised): sham auricular (ear) acupuncture x 7 days plus self care (Sham AA). Used non‐specific points (shoulder, wrist, extra auricular point). Control group (N = 47 randomised): self care only waiting list control (WL). Self care only. No acupuncture treatment received. Women just given advice. NB: all women given advice to rest if desired, take 650 mg acetaminophen every 6 hours if needed, use hot/cold compress as desired. | |
| Outcomes | Pain: VAS (0 to 100 mm); Disability Rating Index (DRI) ‐ functional status; STAI, measured at baseline, after 7 days of continuous AA or Sham AA and at 1 week post treatment (for both groups). Days off work not included in outcomes. | |
| Condition (LBP, PP, LBPP) | LBPP. | |
| Notes | Funding = national Center for the Complementary and Alternative Medicine Grant. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | 'randomly assigned to one of the three treatment groups based on a computer generated randomisation sheet.' |
| Allocation concealment (selection bias) | Unclear risk | No information provided on allocation concealment. |
| Blinding of participants and personnel (performance bias) | Low risk | Women had no previous experience with acupuncture and were asked to complete a credibility questionnaire after the removal of the needles. While not blinded, acupuncturist was skilled and trained and followed a strict script during treatment to avoid any nuances being picked up by the participants. |
| Blinding of outcome assessment (detection bias) | Low risk | Assessors and statisticians were blinded; women who gave self‐reports were also blinded. |
| Incomplete outcome data (attrition bias) | Low risk | Attrition and exclusions reported, numbers add up in the analysis, authors indicate how they managed missing values in their analysis. |
| Selective reporting (reporting bias) | Low risk | Study reported all outcomes as indicated in the methods section. |
| Other bias | Low risk | Similar co‐interventions; groups similar at baseline, timing of outcome assessment same across groups and compliance acceptable across groups. |
| Methods | RCT; conducted in the Eastern part of Östergötland, Sweden. N = 60 randomised/46 analysed. | |
| Participants | Pregnant women with LBP or PP arising before 32 weeks' gestation. | |
| Interventions | Acupuncture group (N = 28): Physiotherapy group (N = 18): | |
| Outcomes | Pain (VAS 0 to 10), functional status (Disability Rating Index), and rating of overall percentage helpfulness of treatment ‐ assessed by the women in the study. Adverse events: no serious adverse effects reported, but 2 women reported small subcutaneous haematomas in the ear from acupuncture. | |
| Condition (LBP, PP, LBPP) | LBPP. | |
| Notes | There was no comparison with no treatment. The pain and disability scales were not used in this review because of insufficient data. Study funded by the Council of Research and Development of Vrinnevi Hospital, Norrkoping, Sweden. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | 60 women who accepted invitation to join study 'drew a closed envelope from a box to randomise to either the acupuncture or physiotherapy group', but method of randomisation not described. |
| Allocation concealment (selection bias) | Low risk | 'drew a closed envelope from a box.' |
| Blinding of participants and personnel (performance bias) | High risk | Participants and caregiver not blinded. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Assessor blinding unclear. |
| Incomplete outcome data (attrition bias) | High risk | Analysed those who completed the intervention in the group to which they had been randomised. 2 of 30 women were not analysed in the acupuncture group since they had both inadvertently received both acupuncture and physiotherapy. |
| Selective reporting (reporting bias) | High risk | Data for pain and disability outcomes not provided with sufficient detail to include in analyses. |
| Other bias | High risk | Statistically significant difference in the distribution of type of pain at baseline, women pursued different co‐treatments to relieve symptoms. |
AA: auricular acupuncture
ACOG: American College of Obstetricians and Gynecologists
ASLR: active straight leg raise
ADL: activities of daily living
BMI: body mass index
CI: confidence interval
gyn: gynaecological
HEP: home exercise programme
ITT: intention‐to‐treat
kg/m2: kilogram/meters squared
LBP: low‐back pain
LBPP: low‐back and pelvic pain
NET: neuro emotional technique
NRS: numerical rating scale
N/S: not significant
NSAID: non‐steroidal anti‐inflammatory drug
ODI: Oswestry Disability Index
OMT: Osteopathic Manipulative Therapy
P4: Posterior Pelvic Pain Provocation
PGP: pelvic girdle pain
PMR: progressive muscle relaxation
PP: pelvic pain
PPA: per‐protocol analysis
PFM: pelvic floor muscles
PPAQ: Pregnancy Physical Activity Questionnaire
RMDQ: Roland Morris Disability Questionnaire
PVD: peripheral vascular disease
RCT: randomised controlled trial
ROB: risk of bias
ROM: range of motion
SD: standard deviation
SLR: straight leg raise test
STAI: State‐Trait Anxiety Inventory
TENS: transcutaneous electrical nerve stimulation
UTI: urinary tract infection
VAS: visual analogue scale
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| CCT ‐ participants not randomised. | |
| QRCT ‐ participants not randomised. Translated from Polish by 1 Polish‐speaking researcher. | |
| QRCT ‐ pilot study of 8 women assigned to groups based on ability to attend classes. | |
| QRCT ‐ women assigned to groups based on the day they attended the prenatal clinic ‐ Tuesday and Thursday were assigned to study group; Monday and Wednesday were assigned to control group. | |
| Not a clinical trial; publication reports on an audit/evaluation of a Midwifery Acupuncture Service. | |
| Trial studied the effect of massage on stress reduction in pregnancy; back pain was measured, but only as a stressor that was managed with massage, not as an outcome of real interest. Attempts to contact 1st author for clarification were unsuccessful. | |
| Intervention designed to study the effect of yoga or massage compared to standard prenatal care on depressed pregnant women; back and leg pain was measured but not an outcome of real interest and not listed as one of the outcomes in methods section. | |
| Participants not randomised. Secondary analysis of intervention to prevent gestational diabetes. | |
| QRCT ‐ randomisation was by date of birth. | |
| Intervention was started during pregnancy, but goal and outcomes measured 6 and 12 weeks postpartum. | |
| Outcomes were blood pressure and heart rate, not LBP or PP. | |
| CCT ‐ sequence generation not described '...140 women were included in the study...80 patients were enrolled into the treatment group ... Pregnant women with the same pregnancy‐related pains were observed without Pycnogenol® treatment as a control group'. | |
| QRCT ‐ described as a 'Prospective controlled trial', with no details given for allocation. Report of conference proceedings, but unable to locate trial register (http://apps.who.int/trialsearch/Default.aspx; accessed 15 August 2012). | |
| Poster presentation of pilot study to assess the feasibility of using reflexology to manage LBPP in pregnant women in the third trimester; saliva, blood pressure, heart rate and pain reported as outcomes of interest, but no data provided; outcomes reported were feasibility of recruitment, intervention and outcome measures. | |
| Cross‐sectional study to determine the sensitivity and specificity of specific tests for LBP/PP. No intervention involved. | |
| Single intervention only; pilot study to determine the feasibility of undertaking a larger/longer trial to examine the effects of exercise and advice‐based physiotherapy on the prevention of pregnancy‐related LBP; no outcome analysis completed. | |
| CCT ‐ sequence generation not described ‐ attempts to contact the author for clarification unsuccessful. Translated from Japanese by 1 Japanese‐speaking researcher and a native Japanese non‐researcher. | |
| QRCT ‐ women stratified by previous pregnancies, then assigned to 1 of 3 treatment groups in sequence (1st primigravida to group 1, 2nd primigravida to group 2, 3rd primigravida to group 3, etc). | |
| QRCT ‐ 3 groups divided by whether date of birth was 1st to 10th day in the month, 11th to 20th or 21st to 31st. | |
| Not a trial but an overview of the benefits of exercise in pregnancy. | |
| Article is described as a 'Single center, prospective, randomised ,experimental study', but there are no details of allocation, the control group(s), or comparison of outcomes between groups. Results are provided for 15 participants who appear to be the only ones entered into the study. | |
| This cross‐over study was included in reviews up to and including the 2013 update. There were always concerns about the appropriateness of including this study due to study design and methods of analysis. The review authors decided to exclude this study in the 2015 update because of these concerns. | |
| Longitudinal cohort study that assessed peak oxygen uptake and incidence of back pain during and after pregnancy. | |
| Women were not pregnant at the time of intervention, just at the inception of the LBP. | |
| As for Torstensson 2009 ‐ women were not pregnant at the time of intervention, just at the inception of the LBP. | |
| Not a RCT ‐ recruited pregnant women were allocated into study groups using block technique (AABB); acronym (AABB) implies that the block allocation was not probably random. Translated from Farsi by 1 Farsi‐speaking researcher. |
CCT: controlled clinical trial
LBP: low‐back pain
PP: pelvic pain
RCT: randomised controlled trial
QRCT: quasi‐randomised controlled trial
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | Management of Antenatal Pelvic Girdle Pain Study (MAPS): a single centre blinded randomised trial evaluating the effectiveness of two pelvic support garments. |
| Methods | Randomised double‐blind parallel assignment intervention study. |
| Participants | 72 pregnant women between 20 to 36 weeks' gestation who: report intermittent PGP or symphysis pubis dysfunction (commenced or aggravated during pregnancy), which causes walking and/or stair climbing to be bothersome and are positive on at least 3 out of 7 pain provocation tests. |
| Interventions | Eligible participants will be randomised to receive either a Customised Dynamic Elastomeric Fabric Orthoses (customised orthosis ‐ intervention group) or a Serola Sacroiliac Belt (rigid 'off the shelf' pelvic support belt ‐ control group) to wear for potentially 20 weeks during pregnancy. All participants will also be issued with standardised advice on PGP management via an information leaflet from the Association of Chartered Physiotherapists in Women's health website. |
| Outcomes | Primary outcome: change in pain intensity a 2‐weekly intervals via numerical rating scale. Secondary outcomes: change in physical activity levels at 2‐weekly intervals via self‐report questionnaire, and change in quality of life at 2‐weekly intervals via Short Form 36 and the EuroQol‐5D. |
| Starting date | Start date = November 2012. Estimated end date = November 2013 (final data collection date for primary outcome measure). |
| Contact information | Jenny Freeman, University of Plymouth, UK. Tel: 01752 588835; Email: [email protected]. |
| Notes | Trial registration: ClinicalTrials.gov NCT01820013. Study sponsored by the University of Plymouth, UK. |
| Trial name or title | Randomised controlled trial for the treatment of pelvic girdle pain in pregnancy. |
| Methods | Open‐label randomised controlled single‐centre trial. |
| Participants | 226 pregnant women (primigravida and multigravida; no age limits) from 20 to 35 weeks of gestation attending Cork University Maternity Hospital (CUMH) low‐risk antenatal clinics who are referred to the physiotherapy department by their healthcare provider or following self‐referral with back pain or pelvic pain will be assessed for inclusion in the study. Women referred to the physiotherapy department with symptoms of PGP will be assessed on presentation by a 1 of 6 departmental physiotherapists specialising in women's health. |
| Interventions | Following initial assessment participants will be randomly allocated to 1 of 2 treatment groups (randomisation ratio 1:1). Patients will be asked to keep a pain score diary where they will record their pain score using a VAS scoring system. Patients will be asked to record a score every morning and every evening during the treatment course. The first treatment in both treatment arms will be 1 week following initial assessment. Group care group: weekly group exercise classes for 4 weeks (1 hour/class), focusing on core stability and strengthening exercises. |
| Outcomes | Primary outcome: a reduction in the current intensity of PGP related to motion on a 100‐point VAS in the morning and in the evening recorded in the patient's diaries (0 represented no pain and 100 represented worst conceivable pain). |
| Starting date | 01/04/2009 ‐ estimated end = 31/03/2010 ‐ trial completed. |
| Contact information | Prof Richard A Greene, Cork University Maternity Hospital ([email protected]). |
| Notes | Sponsor: Cork University Maternity Hospital (Ireland); March 8, 2012 ‐ recruiting not yet started. |
| Trial name or title | Exercise training in pregnancy for obese women (ETIP). |
| Methods | Protocol for a randomised controlled trial. |
| Participants | 150 previously sedentary, pregnant women with a pre‐pregnancy BMI at or above 30 kg/m2; randomised to intervention and control groups. |
| Interventions | Intervention group: organised exercise training 3 x/week starting in gestation week 14 (range 12 to 16 weeks' gestation). Control group: standard prenatal care. |
| Outcomes | Primary outcome: weight gain from baseline to delivery. Secondary outcomes: changes in exercise capacity, physical activity level, endothelial function, body composition, incontinence, lumbo‐pelvic pain and cardiac function from baseline to gestation week 37 (range 36 to 38). Offspring outcome measures include anthropometric variables at birth, Apgar score. |
| Starting date | September 2010. |
| Contact information | Principal Investigator: Trine T Moholdt, PhD. |
| Notes | Trial registration: ClinicalTrials.gov: NCT01243554. Sponsor: Norwegian University of Science and Technology. |
| Trial name or title | Auricular acupuncture for primary care treatment of low‐back pain and posterior pelvic pain (LBPP) in pregnancy. |
| Methods | Protocol for a 4‐parallel arm, multicentre, randomised placebo‐controlled trial. |
| Participants | 212 pregnant women (24 to 36 weeks’ gestation), aged at least 17 years, with low back and/or PGP will be randomised into 1 of 3 intervention groups including standard antenatal care or standard antenatal care alone. |
| Interventions | Intervention 1: verum auricular acupuncture (3 LBPP specific acupuncture points) x once/week x 2 weeks. Intervention 2: non‐specific auricular acupuncture (3 non‐specific acupuncture points) over the same intervention period. Intervention 3: placebo auricular acupuncture (3 non‐specific acupuncture points using the same auricular acupuncture devices but with no needle) over the same intervention period. Control group: standard antenatal care over the same period as intervention groups. |
| Outcomes | Primary outcome: reduction in pain intensity at 2 weeks using the VAS. Secondary outcomes: LBPP‐related functional disability (RMDQ), Health‐related Quality of Life (Short‐Form 12) temporary occupational incapacity and reduction in analgesic use at 2 weeks. Change in pain intensity will also be recorded at 12 and 48 weeks (outside scope of this review). |
| Starting date | February 2014. |
| Contact information | Jorge Vas, Pain Treatment Unit. Doña Mercedes Primary Health Care Centre, Segovia s/n, Dos Hermanas 41701, Spain |
| Notes | Trial registration: Current Controlled Trials ISRCTN41033073. Sponsor: Spanish Ministry of Health and Consumer Affairs. |
BMI: body mass index
LBPP: low‐back and pelvic pain
PGP: pelvic girdle pain
VAS: visual analogue scale
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain intensity Show forest plot | 7 | 645 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.64 [‐1.03, ‐0.25] |
| Analysis 1.1  Comparison 1 Low‐back pain: any exercise + usual prenatal care versus usual prenatal care, Outcome 1 Pain intensity. | ||||
| 2 Functional disability Show forest plot | 2 | 146 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.56 [‐0.89, ‐0.23] |
| Analysis 1.2  Comparison 1 Low‐back pain: any exercise + usual prenatal care versus usual prenatal care, Outcome 2 Functional disability. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Number of women taking sick leave because of low‐back pain after 32 weeks' gestation Show forest plot | 1 | 241 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.40 [0.17, 0.92] |
| Analysis 2.1  Comparison 2 Low‐back pain: water gymnastics + usual prenatal care versus usual prenatal care, Outcome 1 Number of women taking sick leave because of low‐back pain after 32 weeks' gestation. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Low‐back pain, measured with VAS; 0 to 10; 0 = no pain Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 3.1  Comparison 3 Low‐back pain: support belts ‐ Bellybra versus Tubigrip, Outcome 1 Low‐back pain, measured with VAS; 0 to 10; 0 = no pain. | ||||
| 1.1 Low‐back pain | 1 | 94 | Mean Difference (IV, Fixed, 95% CI) | ‐0.20 [‐1.19, 0.79] |
| 1.2 Functional disability (ADL) | 1 | 94 | Mean Difference (IV, Fixed, 95% CI) | ‐0.90 [‐1.81, 0.01] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Number of women reporting pain on Visual Analogue Scale Show forest plot | 2 | 374 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.80, 1.17] |
| Analysis 4.1  Comparison 4 Low‐back pain: group exercise + education + usual prenatal care versus usual prenatal care, Outcome 1 Number of women reporting pain on Visual Analogue Scale. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Evening pain Show forest plot | 1 | 47 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.06 [0.73, 1.54] |
| Analysis 5.1  Comparison 5 Pelvic pain: deep versus superficial acupuncture, Outcome 1 Evening pain. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Number of women reporting pain on Visual Analogue Scale Show forest plot | 2 | 374 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.77, 1.23] |
| Analysis 6.1  Comparison 6 Pelvic pain: group exercise + education + usual prenatal care versus usual prenatal care, Outcome 1 Number of women reporting pain on Visual Analogue Scale. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Women who reported pain on Visual Analogue Scale Show forest plot | 4 | 1176 | Risk Ratio (M‐H, Random, 95% CI) | 0.66 [0.45, 0.97] |
| Analysis 7.1  Comparison 7 Pelvic + low‐back pain: any exercises + usual prenatal care versus usual prenatal care, Outcome 1 Women who reported pain on Visual Analogue Scale. | ||||
| 2 Women who reported LBPP‐related sick leave Show forest plot | 2 | 1062 | Risk Ratio (M‐H, Random, 95% CI) | 0.76 [0.62, 0.94] |
| Analysis 7.2  Comparison 7 Pelvic + low‐back pain: any exercises + usual prenatal care versus usual prenatal care, Outcome 2 Women who reported LBPP‐related sick leave. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Number of women who reported decreased pain Show forest plot | 1 | 72 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.16 [1.77, 9.78] |
| Analysis 8.1  Comparison 8 Pelvic + low‐back pain: acupuncture + usual prenatal care versus usual prenatal care, Outcome 1 Number of women who reported decreased pain. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Numbers of women rating treatment as good or excellent Show forest plot | 1 | 46 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.24 [0.96, 1.60] |
| Analysis 9.1  Comparison 9 Pelvic + low‐back pain: acupuncture + usual prenatal care versus individualised physio + usual prenatal care, Outcome 1 Numbers of women rating treatment as good or excellent. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain Show forest plot | 1 | 169 | Mean Difference (IV, Fixed, 95% CI) | ‐2.70 [‐3.54, ‐1.86] |
| Analysis 10.1  Comparison 10 Pelvic + low‐back pain: MOM versus STOB, Outcome 1 Pain. | ||||
| 2 Functional disability Show forest plot | 1 | 169 | Mean Difference (IV, Fixed, 95% CI) | ‐1.4 [‐2.09, ‐0.71] |
| Analysis 10.2  Comparison 10 Pelvic + low‐back pain: MOM versus STOB, Outcome 2 Functional disability. | ||||
| 3 Days off work/sick leave Show forest plot | 1 | 169 | Mean Difference (IV, Fixed, 95% CI) | 0.10 [‐1.12, 1.32] |
| Analysis 10.3  Comparison 10 Pelvic + low‐back pain: MOM versus STOB, Outcome 3 Days off work/sick leave. | ||||
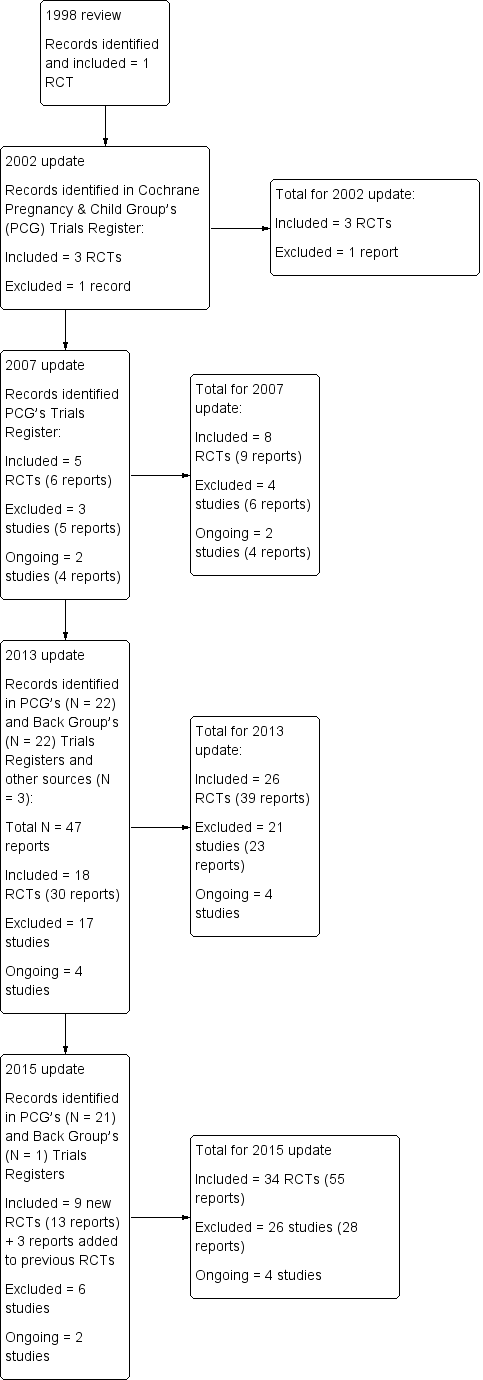
Study flow diagram.
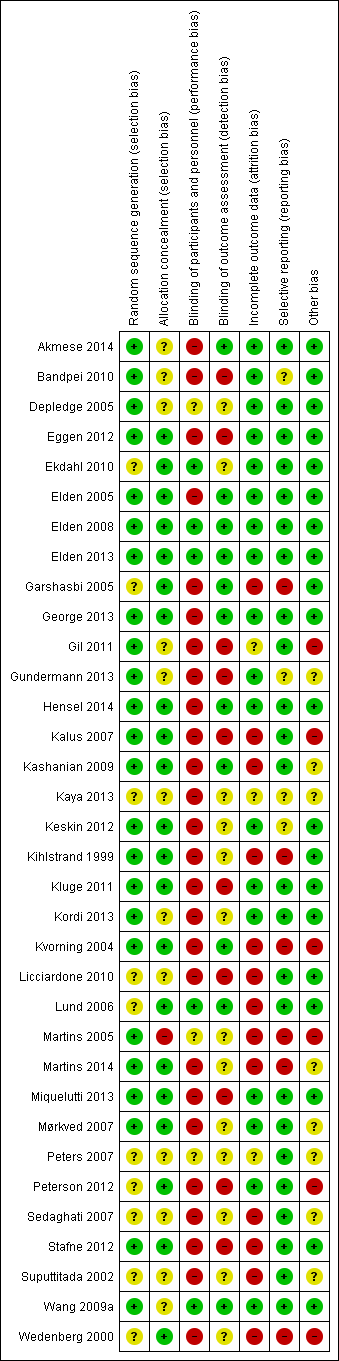
'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.
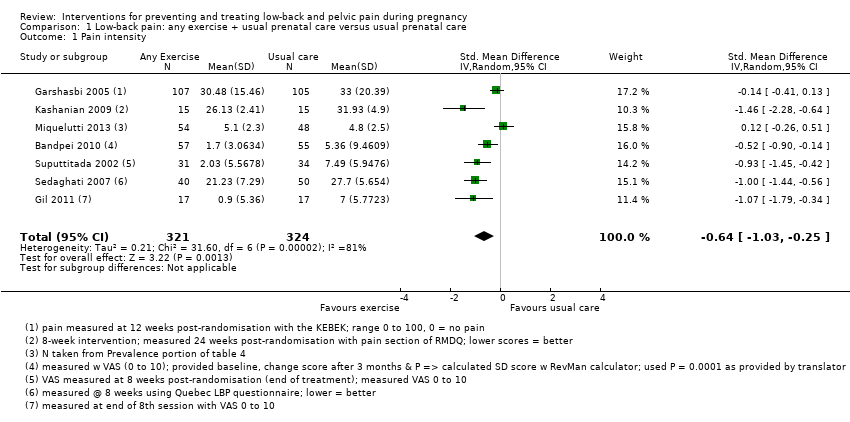
Comparison 1 Low‐back pain: any exercise + usual prenatal care versus usual prenatal care, Outcome 1 Pain intensity.

Comparison 1 Low‐back pain: any exercise + usual prenatal care versus usual prenatal care, Outcome 2 Functional disability.

Comparison 2 Low‐back pain: water gymnastics + usual prenatal care versus usual prenatal care, Outcome 1 Number of women taking sick leave because of low‐back pain after 32 weeks' gestation.
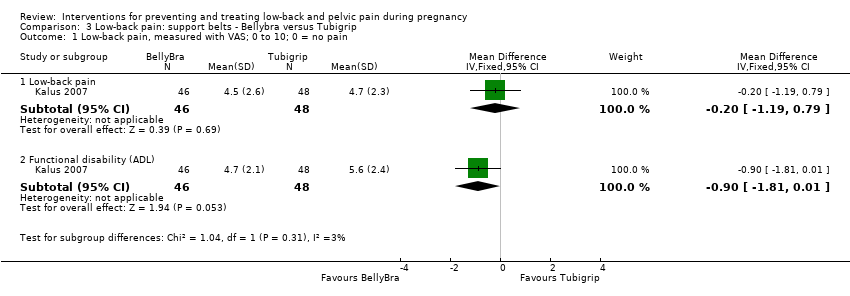
Comparison 3 Low‐back pain: support belts ‐ Bellybra versus Tubigrip, Outcome 1 Low‐back pain, measured with VAS; 0 to 10; 0 = no pain.

Comparison 4 Low‐back pain: group exercise + education + usual prenatal care versus usual prenatal care, Outcome 1 Number of women reporting pain on Visual Analogue Scale.

Comparison 5 Pelvic pain: deep versus superficial acupuncture, Outcome 1 Evening pain.
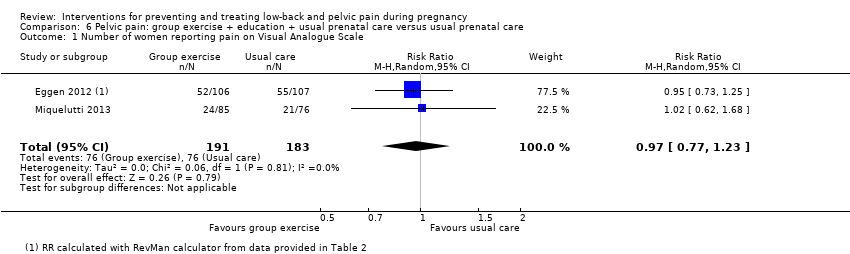
Comparison 6 Pelvic pain: group exercise + education + usual prenatal care versus usual prenatal care, Outcome 1 Number of women reporting pain on Visual Analogue Scale.

Comparison 7 Pelvic + low‐back pain: any exercises + usual prenatal care versus usual prenatal care, Outcome 1 Women who reported pain on Visual Analogue Scale.

Comparison 7 Pelvic + low‐back pain: any exercises + usual prenatal care versus usual prenatal care, Outcome 2 Women who reported LBPP‐related sick leave.
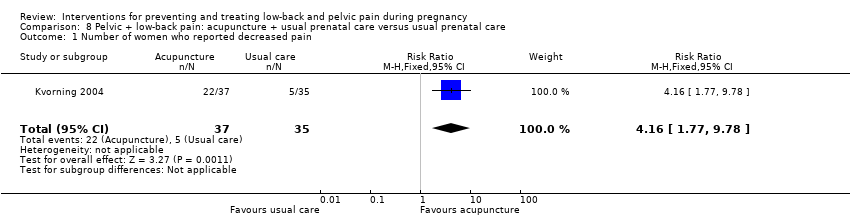
Comparison 8 Pelvic + low‐back pain: acupuncture + usual prenatal care versus usual prenatal care, Outcome 1 Number of women who reported decreased pain.
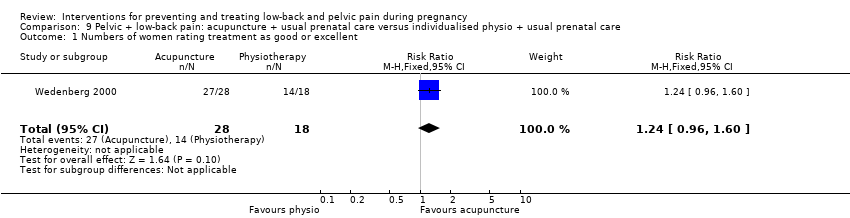
Comparison 9 Pelvic + low‐back pain: acupuncture + usual prenatal care versus individualised physio + usual prenatal care, Outcome 1 Numbers of women rating treatment as good or excellent.

Comparison 10 Pelvic + low‐back pain: MOM versus STOB, Outcome 1 Pain.

Comparison 10 Pelvic + low‐back pain: MOM versus STOB, Outcome 2 Functional disability.
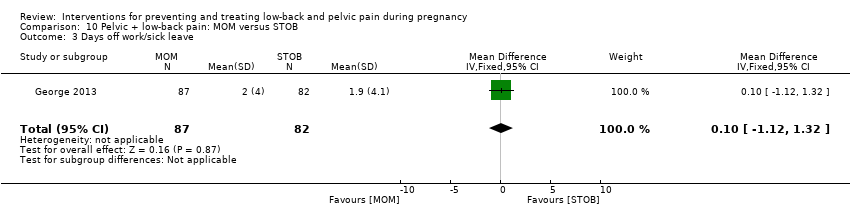
Comparison 10 Pelvic + low‐back pain: MOM versus STOB, Outcome 3 Days off work/sick leave.
| Low‐back pain: any exercises + usual prenatal care versus usual prenatal care | ||||||
| Patient or population: pregnant women with back pain | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Usual prenatal care | Any exercises + usual prenatal care | |||||
| Pain intensity measured by a number of different measurements; lower score = better. Follow‐up was measured between 8 and 24 weeks after randomisation across studies. Treatments varied from 5 to 20 weeks in duration. | The mean pain intensity in the control groups was 16.14 | The mean pain intensity in the intervention groups was 0.64standard deviations lower (SMD ‐0.64, 95% CI ‐1.03 to ‐0.25; participants = 645; studies = 7) | SMD ‐0.64, 95% CI ‐1.03 to ‐0.25 | 645 | ⊕⊕⊝⊝ | A standard deviation of 0.64 lower represents a moderate difference between groups, and may be clinically relevant. However, there was considerable clinical heterogeneity amongst the participants, interventions and outcome measures. |
| Disability measured by Roland Morris Disability Questionnaire and Oswestry Disability Index; lower score = better. Follow‐up was measured from 5 to 12 weeks after randomisation across studies. Treatments varied from 5 to 8 weeks in duration. | The mean disability in the control groups was 26.64 | The mean disability in the intervention groups was 0.56standard deviations lower | SMD ‐0.56; 95% CI ‐0.89 to ‐0.23 | 146 | ⊕⊕⊝⊝ | A standard deviation of 0.56 lower represents a moderate difference between groups and may be clinically relevant. |
| *The basis for the assumed risk (e.g. the mean control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Poor or no description of randomisation process, allocation concealment, or blinding of research personnel in most of the studies in the meta‐analyses. 4 The assumed risk was calculated by measuring the mean pain intensity and the mean disability for the control groups. | ||||||
| Pelvic + low‐back pain: any exercises + usual prenatal care versus usual prenatal care | ||||||
| Patient or population: pregnant women with, or at risk of developing, pelvic and back pain | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk (moderate risk population)3 | Corresponding risk | |||||
| Usual prenatal care | Any exercises + usual prenatal care | |||||
| Number of women who reported pain on Visual Analogue Scale. Follow‐up was measured immediately after the intervention. Treatments ran from 8 to 12 weeks in duration. | Study population | RR 0.66 | 1176 | ⊕⊕⊕⊝ | mean reduction of 34% across studies | |
| 708 per 1000 | 467 per 1000 | |||||
| Number of women who reported LBPP‐related sick leave. Follow‐up was measured immediately after the intervention, which ran for 12 weeks. | Study population | RR 0.76 | 1062 (2 studies) | ⊕⊕⊕⊝ | mean reduction of 24% across studies | |
| 288 per 1000 | 219 per 1000 | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 There was a mix of potential biases among the four studies: no allocation concealment (1); no blinding of research personnel (all); poor/no description of drop‐outs, co‐interventions and baseline inequality (mixed). 3 Moderate risk population chosen as the assumed risk because studies included pregnant women who did not have serious, systemic morbidities and entered at different points of their pregnancies, with varying levels of pain and disability. | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain intensity Show forest plot | 7 | 645 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.64 [‐1.03, ‐0.25] |
| 2 Functional disability Show forest plot | 2 | 146 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.56 [‐0.89, ‐0.23] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Number of women taking sick leave because of low‐back pain after 32 weeks' gestation Show forest plot | 1 | 241 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.40 [0.17, 0.92] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Low‐back pain, measured with VAS; 0 to 10; 0 = no pain Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 Low‐back pain | 1 | 94 | Mean Difference (IV, Fixed, 95% CI) | ‐0.20 [‐1.19, 0.79] |
| 1.2 Functional disability (ADL) | 1 | 94 | Mean Difference (IV, Fixed, 95% CI) | ‐0.90 [‐1.81, 0.01] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Number of women reporting pain on Visual Analogue Scale Show forest plot | 2 | 374 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.80, 1.17] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Evening pain Show forest plot | 1 | 47 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.06 [0.73, 1.54] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Number of women reporting pain on Visual Analogue Scale Show forest plot | 2 | 374 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.77, 1.23] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Women who reported pain on Visual Analogue Scale Show forest plot | 4 | 1176 | Risk Ratio (M‐H, Random, 95% CI) | 0.66 [0.45, 0.97] |
| 2 Women who reported LBPP‐related sick leave Show forest plot | 2 | 1062 | Risk Ratio (M‐H, Random, 95% CI) | 0.76 [0.62, 0.94] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Number of women who reported decreased pain Show forest plot | 1 | 72 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.16 [1.77, 9.78] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Numbers of women rating treatment as good or excellent Show forest plot | 1 | 46 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.24 [0.96, 1.60] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain Show forest plot | 1 | 169 | Mean Difference (IV, Fixed, 95% CI) | ‐2.70 [‐3.54, ‐1.86] |
| 2 Functional disability Show forest plot | 1 | 169 | Mean Difference (IV, Fixed, 95% CI) | ‐1.4 [‐2.09, ‐0.71] |
| 3 Days off work/sick leave Show forest plot | 1 | 169 | Mean Difference (IV, Fixed, 95% CI) | 0.10 [‐1.12, 1.32] |

