Single versus multiple visits for endodontic treatment of permanent teeth
Abstract
Background
Root canal treatment (RoCT), or endodontic treatment, is a common procedure in dentistry. The main indications for RoCT are irreversible pulpitis and necrosis of the dental pulp caused by carious processes, tooth cracks or chips, or dental trauma. Successful RoCT is characterised by an absence of symptoms (i.e. pain) and clinical signs (i.e. swelling and sinus tract) in teeth without radiographic evidence of periodontal involvement (i.e. normal periodontal ligament). The success of RoCT depends on a number of variables related to the preoperative condition of the tooth, as well as the endodontic procedures. This review updates the previous version published in 2007.
Objectives
To determine whether completion of root canal treatment (RoCT) in a single visit or over two or more visits, with or without medication, makes any difference in term of effectiveness or complications.
Search methods
We searched the following electronic databases: Cochrane Oral Health's Trials Register (to 14 June 2016), Cochrane Central Register of Controlled Trials (CENTRAL) (the Cochrane Library, 2016, Issue 5), MEDLINE Ovid (1946 to 14 June 2016), and Embase Ovid (1980 to 14 June 2016). We searched ClinicalTrials.gov and the World Health Organization International Clinical Trials Registry Platform for ongoing trials to 14 June 2016. We did not place any restrictions on the language or date of publication when searching the electronic databases.
Selection criteria
We included randomised controlled trials (RCTs) and quasi‐RCTs of people needing RoCT. We excluded surgical endodontic treatment. The outcomes of interest were tooth extraction for endodontic problems; radiological failure after at least one year, i.e. periapical radiolucency; postoperative pain; swelling or flare‐up; painkiller use; sinus track or fistula formation; and complications (composite outcome including any adverse event).
Data collection and analysis
We collected data using a specially designed extraction form. We contacted trial authors for further details where these were unclear. We assessed the risk of bias in the studies using the Cochrane tool and we assessed the quality of the body of evidence using GRADE criteria. When valid and relevant data were collected, we undertook a meta‐analysis of the data using the random‐effects model. For dichotomous outcomes, we calculated risk ratios (RRs) and 95% confidence intervals (CIs). For continuous data, we calculated mean differences (MDs) and 95% CIs. We examined potential sources of heterogeneity. We conducted subgroup analyses for necrotic and vital teeth.
Main results
We included 25 RCTs in the review, with a total of 3780 participants, of whom we analysed 3751. We judged three studies to be at low risk of bias, 14 at high risk, and eight as unclear.
Only one study reported data on tooth extraction due to endodontic problems. This study found no difference between treatment in one visit or treatment over multiple visits (1/117 single‐visit participants lost a tooth versus 2/103 multiple‐visit participants; odds ratio (OR) 0.44, 95% confidence interval (CI) 0.04 to 4.78; very low‐quality evidence).
We found no evidence of a difference between single‐visit and multiple‐visit treatment in terms of radiological failure (risk ratio (RR) 0.91, 95% CI 0.68 to 1.21; 1493 participants, 11 studies, I2 = 18%; low‐quality evidence); immediate postoperative pain (dichotomous outcome) (RR 0.99, 95% CI 0.84 to 1.17; 1560 participants, 9 studies, I2 = 33%; moderate‐quality evidence); swelling or flare‐up incidence (RR 1.36, 95% CI 0.66 to 2.81; 281 participants, 4 studies, I2 = 0%; low‐quality evidence); sinus tract or fistula formation (RR 0.98, 95% CI 0.15 to 6.48; 345 participants, 2 studies, I2 = 0%; low‐quality evidence); or complications (RR 0.92, 95% CI 0.77 to 1.11; 1686 participants, 10 studies, I2 = 18%; moderate‐quality evidence).
The studies suggested people undergoing RoCT in a single visit may be more likely to experience pain in the first week than those whose RoCT was over multiple visits (RR 1.50, 95% CI 0.99 to 2.28; 1383 participants, 8 studies, I2 = 54%), though the quality of the evidence for this finding is low.
Moderate‐quality evidence showed people undergoing RoCT in a single visit were more likely to use painkillers than those receiving treatment over multiple visits (RR 2.35, 95% CI 1.60 to 3.45; 648 participants, 4 studies, I2 = 0%).
Authors' conclusions
There is no evidence to suggest that one treatment regimen (single‐visit or multiple‐visit root canal treatment) is better than the other. Neither can prevent all short‐ and long‐term complications. On the basis of the available evidence, it seems likely that the benefit of a single‐visit treatment, in terms of time and convenience, for both patient and dentist, has the cost of a higher frequency of late postoperative pain (and as a consequence, painkiller use).
PICOs
Plain language summary
Should root canal treatment be performed in one dental visit or over several visits?
Review question
Is there any difference in effectiveness when undertaking root canal treatment in one visit compared to over several visits, and what are the effects on pain and complications, regardless of whether medication is used?
Background
This is an update of a review first published in 2007.
Root canal treatment, or endodontic treatment, is a common procedure in dentistry. The main reasons that root canal treatment are needed are persistent inflammation of the dental pulp (pulpitis) and death of the dental pulp (dead or non‐vital tooth) caused by tooth decay, cracks or chips, or other accidental damage to teeth.
Root canal treatment is considered successful when there are no symptoms, for example pain, and when x‐rays show no signs of damage to bone and other supporting tissues of the tooth. The success of root canal treatment depends on the preoperative condition of the tooth, as well as the endodontic procedures used.
Study characteristics
We searched the literature up to 14 June 2016. We found 25 relevant studies with a total of 3780 participants. The studies compared root canal treatment performed at a single appointment with root canal treatment performed over two or more appointments on vital permanent teeth, non‐vital permanent teeth, or both.
Key results
No apparent difference exists between single‐ and multiple‐visit root canal treatment on x‐ray examination, an indicator which does not affect the patient directly, but is known to be important as a measure of effective treatment. Only one study measured the likelihood of tooth extraction due to endodontic problems and did not find evidence of a difference between single‐ and multiple‐visit treatment. Most short‐ and long‐term complications (pain, swelling, fistula, and tooth extraction) were similar in terms of frequency, although people undergoing a single visit were more likely to experience pain in the first week and to take painkillers.
Quality of the evidence
We assessed the available evidence as moderate to low quality because a number of the studies were at high risk of bias, there was inconsistency between study results, and results were imprecise.
Authors' conclusions
Summary of findings
| Single‐visit compared to multiple‐visit treatment for endodontic treatment of permanent teeth | ||||||
| Patient or population: people receiving endodontic treatment of permanent teeth | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | Number of participants | Quality of the evidence | Comments | |
| Risk with multiple‐visit treatment | Risk with single‐visit treatment | |||||
| Tooth extraction due to endodontic problems | 19 per 1000 | 9 per 1000 | RR 0.44 | 220 | ⊕⊝⊝⊝ | |
| Radiological failure | 146 per 1000 | 132 per 1000 | RR 0.91 | 1493 | ⊕⊕⊝⊝ | |
| Pain (dichotomous) ‐ pain in the immediate postoperative period (until 72 hours postobturation) | 379 per 1000 | 375 per 1000 | RR 0.99 | 1560 | ⊕⊕⊕⊝ | |
| Pain (dichotomous) ‐ pain at 1 week | 109 per 1000 | 164 per 1000 | RR 1.50 | 1383 | ⊕⊕⊝⊝ | |
| Swelling or flare‐up | 81 per 1000 | 110 per 1000 | RR 1.36 | 281 | ⊕⊕⊝⊝ | |
| Painkiller use | 97 per 1000 | 228 per 1000 | RR 2.35 | 648 | ⊕⊕⊕⊝ | |
| Sinus track or fistula formation | 12 per 1000 | 12 per 1000 | RR 0.98 | 345 | ⊕⊕⊝⊝ | |
| Any complication | 286 per 1000 | 263 per 1000 | RR 0.92 | 1686 | ⊕⊕⊕⊝ | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 The study was judged at high risk of bias. | ||||||
Background
Description of the condition
Irreversible pulpitis of the dental pulp and its subsequent necrosis (death of dental pulp) are caused by carious processes, tooth cracks or chips, or dental trauma and represent the main indications for root canal treatment (RoCT). The primary symptom of irreversible pulpitis is severe pain, and RoCT is necessary to relieve symptoms and to avoid tooth extraction due to complications following necrosis of the dental pulp.
Description of the intervention
RoCT is a common procedure in dentistry that is performed to remove organic tissue, infected debris, and pathogenic bacteria from the root canal system by means of mechanical instrumentation associated with copious irrigation with disinfectant agents. Two approaches have been proposed to solve this problem. In the first approach, residual bacteria are eliminated or prevented from repopulating the root canal system by introducing an interappointment dressing into the root canal, generally falling into the following categories: phenolic derivatives (eugenol, camphorated para‐monochlorophenol, camphorated phenol, metacresyl acetate, beechwood creosote), aldehydes (formocresol), halides (iodine‐potassium iodide), calcium hydroxide, antibiotics, or other combinations. The most popular intracanal medication currently in use is calcium hydroxide. Some studies have shown that calcium hydroxide fails to produce sterile root canals and even allows regrowth in some cases (Kvist 2004; Orstavik 1991; Reit 1988). However, even a negative culture before obturation gives no guarantee of healing in all cases (Trope 1999; Weiger 2000). The second approach aims to eliminate remaining bacteria or render them harmless by entombing them by complete and three‐dimensional obturation, finishing the treatment in one visit to deprive the micro‐organisms of nutrition and the space required to survive and multiply (Soltanoff 1978; Weiger 2000). The antimicrobial activity of the sealer or the zinc ions of gutta‐percha can kill the residual bacteria (Moorer 1982; Siqueira 2000).
Endodontic techniques can claim many improvements through the use of rubber dam, magnifying devices, electronic apex locators, and engine‐driven rotary nickel titanium files, which have improved the success rate of endodontic treatment and shortened the time needed for treatment (Bystrom 1981; Orstavik 1998; Reit 1988). The basic biological rationale for achieving final success of RoCT consists primarily of eliminating micro‐organisms from the entire root canal system and preventing their re‐entry. Different therapeutic procedures can be employed, depending upon the biological condition of the tooth being treated, its pathological state, clinician expertise, instrument availability, and patient preference. Successful RoCT is characterised by the absence of symptoms and clinical signs of infection in a tooth without radiographic evidence of periodontal involvement (Friedman 2002). The success of RoCT depends on variables related to the preoperative condition of the tooth, as well as the endodontic procedures.
How the intervention might work
RoCT can be followed by numerous short‐ and long‐term complications (Battrum 1996). The former include immediate postoperative inflammation of periradicular tissues associated with pain, either spontaneous or provoked. The correlation of postoperative pain with different variables, including the number of visits needed to complete RoCT, operative procedures, pulp vitality and dental anatomy, has been the objective of numerous studies (Albashaireh 1998; DiRenzo 2002; Gambarini 1991; Soltanoff 1978). The main long‐term complications include the persistence of inflammation of fistula or sinus track, pain, or both, and an absence of radiographic healing. Several studies have investigated the frequency of radiographic healing in teeth with preoperative periapical pathology and have compared single‐ and multiple‐visit approaches, employing interappointment medication (Katebzadeh 2000; Peters 2002; Soltanoff 1978; Trope 1999; Weiger 2000). The results of such investigations have led to conflicting conclusions. Some studies have suggested that the use of different medications between visits can contribute to the elimination of all bacteria (Fava 1995). In contrast, others have emphasised the need to seal the endodontic space as quickly as possible, i.e. in a single visit, as temporary cements are unreliable in maintaining a good coronal seal during the time between visits. Postoperative complications have been reported with both methods, varying from 5% in Abbott 2000 to more than 20% in Friedman 1995.
Why it is important to do this review
Cochrane Oral Health undertook an extensive prioritisation exercise in 2014 to identify a core portfolio of titles that were the most clinically important ones to maintain in the Cochrane Library (Worthington 2015). The operative and prosthodontic dentistry expert panel identified this review as a priority title (Cochrane Oral Health priority review portfolio).
RoCT is an extremely common procedure, performed on thousands of people every day. If a single‐visit approach is shown to be as effective and safe as multiple‐visit treatment, it could result in a significant saving in time and money for patients and dentists.
Objectives
To determine whether completion of root canal treatment (RoCT) in a single visit or over two or more visits, with or without medication, makes any difference in term of effectiveness or complications.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled trials (RCTs) and quasi‐RCTs (i.e. those using an alternative assignment based on, for example, birth date). We also considered split‐mouth studies. We excluded studies that did not measure at least one of our outcomes.
Types of participants
Participants aged 10 years or above who required root canal treatment. All participants had teeth with a completely formed apex and without internal resorption.
Types of interventions
Root canal treatment in a single visit or multiple visits, i.e. two or more appointments.
Any systemic medical treatment (antibiotics, non‐steroidal anti‐inflammatories or analgesics) was to be the same in both groups.
Types of outcome measures
Primary outcomes
-
Tooth extraction due to endodontic problems (binary, yes/no).
-
Radiological failure after at least one year, i.e. the presence of any periapical radiolucency (binary, yes/no). Additional Table 1 summarises how we adapted the most common scales of radiological healing to a binary outcome.
| Classification | Success (binary) | Failure (binary) |
| PAI score 1 (normal periapical), PAI score 2 (bone structural changes) | PAI score 3 (structural changes with mineral loss), PAI score 4 (radiolucency), PAI score 5 (radiolucency with features of exacerbation) | |
| Success (normal to slightly thickened periodontal ligament space < 1 mm, elimination of previous rarefaction, normal lamina dura in relation to adjacent teeth, no evidence of resorption) | Questionable (increased periodontal ligament space > 1 mm and < 2 mm, stationary rarefaction or slight repair evident, increased lamina dura in relation to adjacent teeth, evidence of resorption); failure (increased width of periodontal ligament space > 2 mm, lack of osseous repair within rarefaction or increased rarefaction, lack of new lamina dura, presence of osseous rarefactions in periradicular areas where previously none existed) | |
| Healed (normal pattern of trabecular bone and normal width of periodontal ligament space) | Improved (reduction in lesion size); failed (increased or no change in the lesion size) | |
| Healed (normal pattern of trabecular bone and normal width of periodontal ligament space) | Increased width of the periodontal space, pathological findings | |
| Success (A) the width and contour of the periodontal ligament is normal, or there is a slight radiolucent zone around apical | Uncertain (B) the radiolucency is clearly decreased but additional follow‐up is not available; failure (C) there is an unchanged, increased, or new periradicular radiolucency | |
| Complete healing: no clinical signs and symptoms, radiographically a periodontal ligament space of normal width | Incomplete healing: no clinical signs and symptoms, radiographically a reduction of the lesion in size or an unchanged lesion within an observation time of 4 years. No healing: clinical signs and symptoms indicating an acute phase of apical periodontitis and\or radiographically a persisting lesion after a follow‐up time of 4 to 5 years and\or a new lesion formed at an initially uninvolved root of a multi‐rooted tooth | |
| Healed (by Rx but the criteria not specified in a satisfactory way) | Not healed (by Rx but the criteria not specified in a satisfactory way) | |
| Normal periapical condition or unclear apical condition (widened apical periodontal space or diffused lamina dura) | Presence of periapical radiolucency when there was a distinct radiolucent area associated with the apical portion of the root | |
| Normal ‐ normal appearance of the surrounding | Apical periodontitis ‐ periapical radiolucency observed Periapical status not classified ‐ the quality of the radiograph was insufficient for examination of the periapical structure |
PAI: periapical index
Rx: radiological evaluation
Secondary outcomes
-
Postoperative pain (binary, yes/no; continuous).
-
Swelling or flare‐up (binary, yes/no).
-
Painkiller use (binary, yes/no).
-
Sinus track or fistula formation (binary, yes/no).
-
Any complication defined as a composite outcome including any adverse event (pain, painkiller use, swelling or flare‐up) occurring within one month from the treatment (binary, yes/no).
Search methods for identification of studies
To identify studies for this review, we developed detailed search strategies for each database searched. These were based on the search strategy developed for MEDLINE Ovid (Appendix 3), but revised appropriately for each database.
Electronic searches
We searched the following electronic databases.
-
Cochrane Oral Health Group's Trials Register (to 14 June 2016) (see Appendix 1).
-
Cochrane Central Register of Controlled Trials (CENTRAL; 2015, Issue 5) in the Cochrane Library (searched 14 June 2016) (see Appendix 2).
-
MEDLINE Ovid (1946 to 14 June 2016) (see Appendix 3).
-
Embase Ovid (1980 to 14 June 2016) (see Appendix 4).
We did not place any restrictions on the language or date of publication when searching the electronic databases.
Searching other resources
We searched the following trial registries for ongoing studies (see Appendix 5).
-
US National Institutes of Health Ongoing Trials Register ClinicalTrials.gov (clinicaltrials.gov; searched 14 June 2016).
-
World Health Organization International Clinical Trials Registry Platform (apps.who.int/trialsearch; searched 14 June 2016).
We did not perform a separate search for adverse effects of interventions; we considered adverse effects as described in included studies only.
We checked all references in the identified papers and we contacted the authors to identify any additional published or unpublished data.
Data collection and analysis
Selection of studies
Two review authors (MM and LF) independently examined the title and abstract (when available) of each article identified by the search strategy. Where studies appeared to meet the inclusion criteria for this review or where there were insufficient data in the title and abstract to make a clear decision, we obtained the full report. The full report was then assessed by at least two of the review authors (MM, LF, GL, MG), to determine whether studies met the inclusion criteria. We resolved any disagreements by discussion. We recorded studies rejected at this or subsequent stages in the Characteristics of excluded studies table, with the reason(s) for exclusion. See Figure 1 for a flow chart that summarises the results of the search.

Study flow diagram: review update
Data extraction and management
At least two review authors (MM, LF) independently extracted data using a specially designed data extraction form and entered them into a spreadsheet. At least two review authors (GL, MM) authors independently assessed the risk of bias in the included studies. We discussed any discrepancies to reach agreement. When necessary, we contacted study authors for clarification or missing information. For each trial, we recorded the following data.
-
Year of publication, country of origin, number of centres, source of study funding, recruitment period.
-
Details of the participants including demographic characteristics and criteria for inclusion and exclusion, type of tooth treated (vital or non‐vital) and reasons of the treatment, diagnostic criteria for pulpal or periapical disease, numbers randomised to each treatment group.
-
Details about the number of visits performed to treat the root canal (single or multiple), number of operators involved in the treatment, use of rubber dam and magnification loupes, type of canal shaping, type of irrigation, method used to establish the working length of the root canal, type of obturation of the canal. In the multiple visits approach, we also recorded the type of medication used in the interappointment period.
-
Details of pain management.
-
Details of the outcomes reported, including method of assessment, and time(s) assessed.
-
Description of operators.
Assessment of risk of bias in included studies
Two review authors (GL, MM) independently assessed the risk of bias of the included trials and any disagreement was resolved through discussion and consensus. We used the recommended approach for assessing risk of bias in studies included in Cochrane Reviews (Higgins 2011). We addressed six domains:
-
random sequence generation (selection bias);
-
allocation concealment (selection bias);
-
blinding of outcome assessment (detection bias);
-
incomplete outcome data (attrition bias);
-
selective reporting (reporting bias);
-
other bias.
Each domain in the tool includes one or more entries in the 'Characteristics of included studies' table. Within each entry, we described what was reported to have happened in the study, in sufficient detail to support a judgement about the risk of bias. We then assigned a judgement relating to the risk of bias for that entry, either 'low', 'high', or 'unclear' risk of bias. After taking into account the additional information provided by the authors of the trials, we summarised the risk of bias in the studies as:
-
low risk of bias = low risk of bias for all key domains;
-
unclear risk of bias = unclear risk of bias for one or more key domains;
-
high risk of bias = high risk of bias for one or more key domains.
We completed a 'Risk of bias' table for each included study (see Characteristics of included studies), and presented results graphically by study and by domain across all studies (Figure 2; Figure 3).

'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study

'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies
Measures of treatment effect
Our primary measures of intervention effect were tooth extraction due to endodontic problems and radiological failure after one year. We dichotomised data on radiological healing when this was measured on ordinal scales (see Table 1 for details). Our other outcomes were incidence of postoperative pain, presence of swelling or flare‐up, painkiller use, sinus track or fistula formation, and any complication. We analysed dichotomous data by calculating risk ratios (RRs) and 95% confidence intervals (CIs). When pain was recorded as a continuous outcome, we analysed data by calculating mean differences (MDs) and 95% CIs.
Unit of analysis issues
The statistical unit was the individual participant. We considered studies using the tooth as the statistical unit, making the assumption that participants were randomised a number of times equal to the number of teeth. When this was not explicitly stated, we considered the study potentially affected by a bias of allocation.
Dealing with missing data
When raw data were not available, we obtained them by consulting tables and graphs, or by contacting the trial authors.
Assessment of heterogeneity
We assessed heterogeneity by inspection of the point estimates and CIs on the forest plots. We assessed the variation in treatment effects by means of Cochran's test for heterogeneity and quantified by the I2 statistic. We considered heterogeneity statistically significant if P < 0.1. A rough guide to the interpretation of the I2 statistic given in the Cochrane Handbook for Systematic Reviews of Interventions is: 0% to 40% might not be important, 30% to 60% may represent moderate heterogeneity, 50% to 90% may represent substantial heterogeneity, 75% to 100% may represent very substantial ('considerable') heterogeneity (Higgins 2011).
Assessment of reporting biases
Only a proportion of research projects conducted are ultimately published in an indexed journal and become easily identifiable for inclusion in systematic reviews. Reporting biases arise when the reporting of research findings is influenced by the nature and direction of the findings of the research. We attempted to minimise potential reporting biases including publication bias, time lag bias, multiple (duplicate) publication bias, and language bias in this review. If there had been more than 10 studies evaluating one outcome, we planned to construct a funnel plot. If there had been asymmetry in the funnel plot indicating possible publication bias, we planned to undertake statistical analysis using the methods introduced by Egger 1997 (continuous outcome) and Rucher 2008 (dichotomous outcome). We attempted to avoid time lag bias, multiple (duplicate) publication bias, and language bias by conducting a detailed sensitive search, including searching for ongoing studies. We did not impose any restrictions on language, and we found translators for potentially relevant trials published in other languages.
Data synthesis
For each intervention, we sought and summarised data on the number of participants in intervention and control groups who experienced the event (outcome) and the total number of participants. We only conducted a meta‐analysis if there were studies of similar comparisons reporting the same outcome measures. We combined RRs for dichotomous data, and MDs for continuous data, using a random‐effects model in Review Manager software (RevMan 2014).
Subgroup analysis and investigation of heterogeneity
We had planned subgroup analyses to investigate the relevance of pretreatment conditions (vital teeth versus necrotic teeth), pretreatment symptoms (symptomatic versus asymptomatic teeth), pretreatment radiographic periapical appearance (apical radiolucency versus no apical radiolucency), endodontic technique, and antimicrobials employed (antimicrobial A versus antimicrobial B). Only data on pretreatment conditions (vital teeth versus necrotic teeth) were available for a subgroup analysis.
Sensitivity analysis
We performed a sensitivity analysis, excluding studies at high risk of bias.
Presentation of main results
Using GRADEpro GDT software (GRADEpro GDT 2014), we produced Summary of findings table 1 for all outcomes. We assessed the quality of the evidence as high, moderate, low, or very low, with reference to study limitations, inconsistency, imprecision, indirectness, and risk of publication bias (Atkins 2004). We explained decisions to downgrade the quality of evidence using footnotes in the 'Summary of findings' table.
Results
Description of studies
Results of the search
We found 25 studies suitable for inclusion in this review (see Figure 1).
Included studies
Characteristics of trial design and settings
For a summary of the characteristics of each of the included studies, see Characteristics of included studies.
Of the 25 included studies, five were conducted in the USA (DiRenzo 2002; Mulhern 1982; Penenis 2008; Soltanoff 1978; Trope 1999), four in India (Dorasani 2013; Patil 2016; Rao 2014; Singh 2012), two in Jordan (Albashaireh 1998; Al‐Negrish 2006), three in China (Wang 2010; Wong 2015; Xiao 2010), two in Turkey (Ince 2009; Yoldas 2004), and single studies were conducted in Italy (Gesi 2006), Iran (Ghoddusi 2006), Sweden (Molander 2007), Nigeria (Oginni 2004), Mexico (Paredes‐Vieyra 2012), the Netherlands (Peters 2002), Brazil (Risso 2008), Germany (Weiger 2000), and Pakistan (Akbar 2013).
Twenty‐two of the studies were performed in university clinics or hospitals. Gesi 2006 was undertaken in private practice. Two studies did not provide details about the settings of the study (Mulhern 1982; Rao 2014).
All the studies used parallel group designs and most had two treatment arms. Two studies had three arms, which compared a single visit, multiple visits without intracanal medication, and multiple visits with intracanal medication (calcium hydroxide) (Ghoddusi 2006; Trope 1999). In order to include such data in the meta‐analysis, we combined the two multi‐visit arms. In the same meta‐analysis, we pooled data from studies that used or did not use a dressing.
Four studies reported that they had received research grants for the conduct of the study (Ghoddusi 2006; Mulhern 1982; Penenis 2008; Risso 2008).
Characteristics of participants
A total of 3780 participants were enrolled in the 25 studies included in this review, and a total of 3571 participants were analysed.
All studies considered one tooth per participant, with the exception of Dorasani 2013, Oginni 2004, Paredes‐Vieyra 2012, Trope 1999, Wong 2015, and Xiao 2010. Dorasani 2013 considered 64 teeth in 43 participants (5 participants contributed 2 teeth and 1 participant contributed 3 teeth). In Oginni 2004, participants requiring root canal treatment (RoCT) on more than one tooth, underwent consecutive treatment of each tooth with an interval of at least four weeks to allow proper evaluation: 283 teeth were randomised in 255 participants. In Paredes‐Vieyra 2012, the study authors reported that 287 participants and 300 teeth were enrolled; they stated that 21 participants contributed more than one tooth, but according to these figures, no more than 13 participants could have contributed more than one tooth. Trope 1999 considered 102 teeth in 81 participants (61 participants had a single tooth, 18 had 2 teeth and 2 participants had 3 teeth). Finally in Xiao 2010, 86 participants were enrolled with a total of 138 teeth. For these five studies, the analysis was conducted at the level of the tooth.
Fourteen studies included participants with necrotic teeth only (Akbar 2013; Al‐Negrish 2006; Dorasani 2013; Ghoddusi 2006; Molander 2007; Mulhern 1982; Paredes‐Vieyra 2012; Penenis 2008; Peters 2002; Rao 2014; Risso 2008; Trope 1999; Weiger 2000; Xiao 2010). Yoldas 2004 is the only study that included retreatment, while Gesi 2006 and Wang 2010 included only participants with vital teeth. Seven studies included both necrotic teeth and vital teeth (Albashaireh 1998; DiRenzo 2002; Ince 2009; Oginni 2004; Patil 2016; Singh 2012, Wong 2015), but two of them did not provide details on the numbers in the two categories (DiRenzo 2002; Oginni 2004). One study did not provide details on the pretreatment status (Soltanoff 1978). One study included maxillary central incisors only (Patil 2016).
None of the data reported by the included studies allowed us to analyse the effects of the two approaches stratified on the basis of preoperative conditions of patients, specifically presence of symptoms (pain) or signs (infection).
Characteristics of interventions
Of the 25 studies included in this review, the majority compared RoCT performed in a single visit with RoCT performed in two visits (Akbar 2013; Al‐Negrish 2006; Albashaireh 1998; DiRenzo 2002; Dorasani 2013; Gesi 2006; Ghoddusi 2006; Ince 2009; Molander 2007; Paredes‐Vieyra 2012; Patil 2016; Penenis 2008Peters 2002; Rao 2014; Singh 2012; Trope 1999; Weiger 2000; Wang 2010; Yoldas 2004). In one study, the multiple‐visit RoCT lasted three visits (Mulhern 1982). One study (Wong 2015) reported that multiple visit treatment had been performed in two or three appointments depending on the complexity of the RoCT. In two studies, the number of visits was not specified (Oginni 2004; Soltanoff 1978).
In the multiple‐visit approach, nine studies did not use any intracanal medications in the interappointment period (Albashaireh 1998; DiRenzo 2002; Ghoddusi 2006; Ince 2009; Mulhern 1982; Patil 2016; Rao 2014; Singh 2012; Trope 1999). In 12 studies, the root canals were medicated with a calcium hydroxide paste (Akbar 2013; Al‐Negrish 2006; Dorasani 2013; Gesi 2006; Molander 2007; Paredes‐Vieyra 2012; Peters 2002; Risso 2008; Wang 2010; Weiger 2000; Wong 2015; Xiao 2010), while two studies used a medication with calcium hydroxide and chlorhexidine (Penenis 2008; Yoldas 2004). Two studies did not specify the type of interappointment medication (Oginni 2004; Soltanoff 1978).
Eleven studies did not report use of rubber dam to isolate the tooth during RoCT (Albashaireh 1998; Ince 2009; Molander 2007; Oginni 2004; Rao 2014; Risso 2008; Singh 2012; Soltanoff 1978; Wang 2010; Xiao 2010; Yoldas 2004), and use of magnification loupes was reported by three studies only (Penenis 2008; Peters 2002; Wong 2015).
Working length was established using an electronic apex locator and radiographs in seven studies (DiRenzo 2002; Paredes‐Vieyra 2012; Patil 2016; Peters 2002; Rao 2014; Risso 2008; Yoldas 2004), by an electronic apex locator only in four studies (Penenis 2008; Singh 2012; Wang 2010; Xiao 2010), and by radiographs only in nine studies (Akbar 2013; Al‐Negrish 2006; Dorasani 2013; Gesi 2006; Ghoddusi 2006; Ince 2009; Mulhern 1982; Trope 1999; Weiger 2000). Five studies did not report information about working length evaluation (Albashaireh 1998; Molander 2007; Oginni 2004; Soltanoff 1978; Wong 2015).
Canal shaping was performed using conventional hand instruments in 10 studies (Akbar 2013; Al‐Negrish 2006; Dorasani 2013; Gesi 2006; Ghoddusi 2006; Ince 2009; Peters 2002; Risso 2008; Soltanoff 1978; Weiger 2000), a combination of hand files and nickel titanium rotary files in seven studies (DiRenzo 2002; Molander 2007; Paredes‐Vieyra 2012; Rao 2014; Singh 2012; Wang 2010; Yoldas 2004), and rotary nickel titanium files only in four studies (Patil 2016; Penenis 2008; Wong 2015; Xiao 2010). Four studies did not report canal shaping instrumentation in a satisfactory way (Albashaireh 1998; Mulhern 1982; Oginni 2004; Trope 1999).
Twenty‐four studies reported that canal obturation was performed with gutta‐percha using the lateral condensation technique; only one study reported use of the vertical condensation technique (Penenis 2008).
In 21 studies, sodium hypochlorite with a range between 0.5% to 5.25% was used as irrigant (Akbar 2013; Al‐Negrish 2006; Albashaireh 1998; DiRenzo 2002; Dorasani 2013; Gesi 2006; Ince 2009; Molander 2007; Mulhern 1982; Paredes‐Vieyra 2012; Patil 2016; Penenis 2008; Peters 2002; Rao 2014; Singh 2012; Trope 1999; Wang 2010; Weiger 2000; Wong 2015; Xiao 2010; Yoldas 2004), while two studies used saline solution as irrigant (Ghoddusi 2006; Soltanoff 1978). In Risso 2008, a combination of sodium hypochlorite, citric acid, and sodium thiosulfate was used as irrigant. In Oginni 2004, the type of irrigant used was not specified.
Nine studies reported that RoCT was performed by a single operator (Al‐Negrish 2006; Albashaireh 1998; Dorasani 2013; Ghoddusi 2006; Paredes‐Vieyra 2012; Patil 2016; Peters 2002; Risso 2008; Trope 1999), while 10 studies reported two or more operators were involved in RoCT (DiRenzo 2002; Gesi 2006; Ince 2009; Molander 2007; Mulhern 1982; Penenis 2008; Wang 2010; Weiger 2000; Wong 2015; Yoldas 2004). Six studies specified that treatment was conducted by trained or experienced operators (Ince 2009; Molander 2007; Penenis 2008; Peters 2002; Wang 2010; Weiger 2000), while three studies reported that RoCT was performed by postgraduate students (DiRenzo 2002; Mulhern 1982; Risso 2008). Six studies did not provide details about the operators (Akbar 2013; Oginni 2004; Rao 2014; Singh 2012; Soltanoff 1978; Xiao 2010).
Characteristics of outcomes
One study only provided information on tooth extraction due to endodontic problems as outcome measure (Wong 2015).
Radiological failure was investigated in 11 studies (Dorasani 2013; Gesi 2006; Molander 2007; Paredes‐Vieyra 2012; Penenis 2008; Peters 2002; Soltanoff 1978; Trope 1999; Weiger 2000; Wong 2015; Xiao 2010). Additional Table 1 shows methods adopted to construct scales for radiological healing or failure. Follow‐up varied from one year in Trope 1999 to five years in Weiger 2000.
Seventeen studies investigated postoperative pain (Al‐Negrish 2006; Albashaireh 1998; DiRenzo 2002; Gesi 2006; Ghoddusi 2006; Ince 2009; Mulhern 1982; Oginni 2004; Patil 2016; Rao 2014; Risso 2008; Singh 2012; Soltanoff 1978; Wang 2010; Wong 2015; Xiao 2010; Yoldas 2004). The methods for evaluating postoperative pain are summarised in the 'Characteristics of included studies' table. Whenever possible, we dichotomised pain data into 'pain' or 'no pain' values. Four studies recorded pain as a continuous variable measured by visual analogue scale (VAS) (DiRenzo 2002; Patil 2016; Singh 2012; Wang 2010). We only considered pain after canal obturation, assessing pain incidence in the immediate postobturation period (until 72 hours), at one week, and at one month. We did not consider pain during the interappointment period in the multiple‐visit approach, as we could not compare this with a similar situation in the single‐visit approach. Five studies examined the need for participants to take analgesics to relieve pain (Mulhern 1982; Rao 2014; Soltanoff 1978;Wang 2010; Yoldas 2004).
Eight studies investigated the incidence of swelling or flare‐up (Akbar 2013; DiRenzo 2002; Ghoddusi 2006; Mulhern 1982; Paredes‐Vieyra 2012; Penenis 2008; Rao 2014; Wang 2010). Definitions of flare‐up varied (see Table 2). Only DiRenzo 2002, Mulhern 1982, Ghoddusi 2006, and Akbar 2013 clearly defined flare‐up as swelling. Therefore, we considered only studies clearly indicating swelling as a specific outcome, not simply as one of the signs related to the tooth infection.
| Study | Definition of flare‐up |
| Moderate to severe postoperative pain or moderate to severe swelling that begins 12 to 48 hours after treatment and lasts at least 48 hours | |
| Percentage of participants experiencing moderate to severe pain evaluated after 2 and 7 days | |
| Swelling that needs antibiotics and narcotic analgesics | |
| Swelling | |
| Swelling | |
| Participant report of pain not controlled with over‐the‐counter medication or increasing swelling or both | |
| Intensive pain (visual analogue scale > 4) | |
| Swelling | |
| Severe postoperative pain or occurrence of swelling or both |
Four studies provided information on fistula or sinus track formation as an outcome measure (Penenis 2008; Paredes‐Vieyra 2012; Wong 2015; Xiao 2010).
Excluded studies
Our main reason for excluding each of the 20 studies is recorded in the 'Characteristics of excluded studies' tables.
We excluded 10 studies because they were not RCTs (ElMubarak 2010; Fava 1989; Fava 1994; Friedman 1995; Jabeen 2014; Ng 2004; Prashanth 2011; Roane 1983; Walton 1992; Jabeen 2014). We excluded five studies because they evaluated only the microbiological status of RoCT (Gurgel‐Filho 2007; Kvist 2004; Trusewicz 2005; Vera 2012; Xavier 2013), and two because the studies were conducted in animals (Holland 2003; Silveira 2007). We excluded two studies because they included primary teeth (Orhan 2010; Kabaktchieva 2013). We excluded one study because it did not include any of the outcomes considered in this review (Waltimo 2005).
Risk of bias in included studies
On the basis of criteria used in the critical appraisal of the studies, we assessed three studies as being at overall low risk of bias (Molander 2007; Singh 2012; Wang 2010); eight studies as being at unclear risk of bias (Akbar 2013; DiRenzo 2002; Gesi 2006; Ghoddusi 2006; Ince 2009; Mulhern 1982; Soltanoff 1978; Weiger 2000); and the remaining studies as being at high risk of bias (Albashaireh 1998; Al‐Negrish 2006; Dorasani 2013; Oginni 2004; Paredes‐Vieyra 2012; Patil 2016; Penenis 2008; Peters 2002; Rao 2014; Risso 2008; Trope 1999; Wong 2015; Xiao 2010; Yoldas 2004). See Figure 2.
Allocation
We assessed the generation of randomisation sequence as being at low risk of bias in 16 trials (64%), unclear risk in three trials (12%), and high risk in six trials (24%). The concealment of allocation was at low risk of bias in eight trials (32%), unclear risk in 13 (52%), and high risk in four (16%). See Figure 3.
Blinding
We assessed blinding of outcome assessment as being at low risk of detection bias for 22 trials (88%), unclear for two trials (8%), and high risk for one trial (4%) (Patil 2016).
Incomplete outcome data
The reported dropout rate ranged from 0% to 35% (Penenis 2008). We assessed 21 (84%) trials as being at low risk with regard to attrition bias, either due to no dropouts or dropouts being unlikely to influence findings. For one study (4%), it was not possible to assess such bias. For three trials, we considered the high dropout rates to put the studies at high risk of attrition bias (12%).
Selective reporting
Two trials (8%) did not report one of the outcomes planned and for this reason we assessed them as being at high risk of reporting bias. For another trial, this bias was impossible to assess (4%). We assessed the remaining 22 studies (88%) as being at low risk of bias.
Other potential sources of bias
We judged fIve studies (20%) as being at high risk of other bias because they did not explicitly state that participants with more that one tooth needing treatment were randomised the same number of times.
Effects of interventions
Single visit versus multiple visit root canal treatment
Primary outcomes
Tooth extraction due to endodontic problems (binary, yes/no)
Only one study reported data on tooth extraction due to endodontic problems (Wong 2015); there was no evidence of a difference between single‐ and multiple‐visit treatment (odds ratio (OR) 0.44, 95% confidence interval (CI) 0.04 to 4.78; 220 participants) (Analysis 1.1). The quality of the evidence was very low (summary of findings Table for the main comparison).
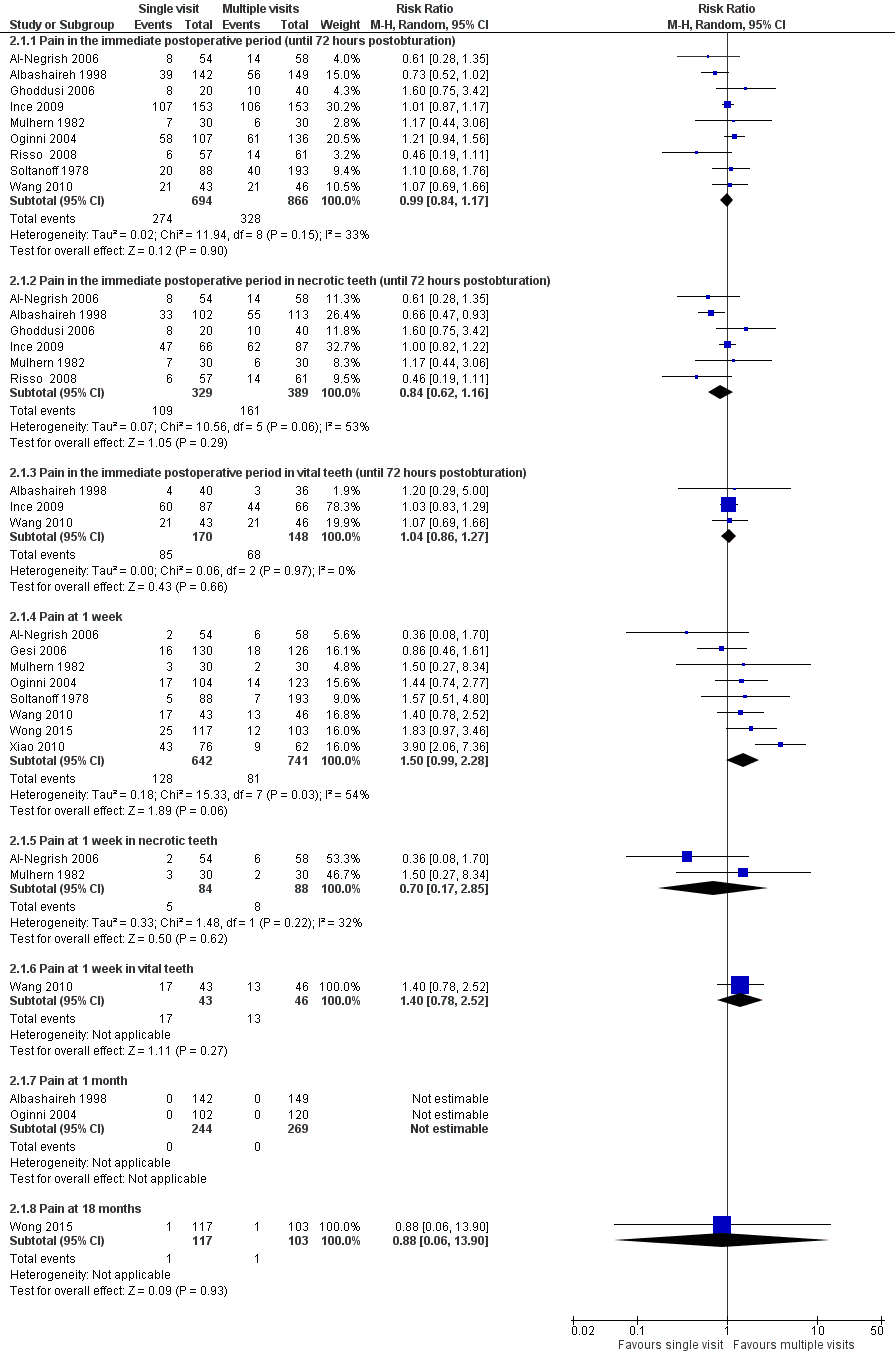
Radiological failure after at least one year, i.e. the presence of any periapical radiolucency (binary, yes/no)
We combined results from 11 studies (Dorasani 2013; Gesi 2006; Molander 2007; Penenis 2008; Paredes‐Vieyra 2012; Peters 2002; Soltanoff 1978; Trope 1999; Weiger 2000; Wong 2015; Xiao 2010), that included 1467 participants with 1493 teeth (Analysis 1.2; Figure 4). The follow‐up was one year (Dorasani 2013; Penenis 2008; Trope 1999), 18 months (Wong 2015), two years (Molander 2007; Paredes‐Vieyra 2012; Soltanoff 1978; Xiao 2010), or more than three years (Gesi 2006; Peters 2002; Weiger 2000). The radiological failure rate was based on binary data, that is, radiological healing versus lack of such healing; scores including more than two values were dichotomised according to the methods indicated in Table 1. The studies, when pooled together, irrespective of the follow‐up duration, showed no difference in terms of radiological failure between the treatments and were homogeneous (RR 0.91, 95% CI 0.68 to 1.21; 1493 participants, 11 studies, I2 = 18%). The quality of the evidence related to this outcome, as assessed using the GRADE method and presented in summary of findings Table for the main comparison was low (Atkins 2004).

Forest plot of comparison: 1 Primary outcomes, outcome: 1.2 Radiological failure
Necrotic teeth
For eight studies (Dorasani 2013; Molander 2007; Paredes‐Vieyra 2012; Penenis 2008; Peters 2002; Trope 1999; Weiger 2000; Xiao 2010), it was possible to analyse radiological failure for necrotic teeth only. Meta‐analysis of these studies showed no difference between participants treated in a single visit versus those treated in multiple visits, with low statistical heterogeneity (RR 0.82, 95% CI 0.55 to 1.21; 823 participants, 8 studies, I2 = 35%; Figure 4).
Vital teeth
There was one study reporting the rate of radiological failure in teeth vital at enrolment (Gesi 2006). This study found no difference between participants treated in single‐visit RoCT in comparison to those treated in multiple visits (RR 0.80, 95% CI 0.59 to 1.07; 184 participants).
Secondary outcomes
Pain in the immediate postoperative period (up to 72 hours postobturation)
Nine studies, with a total of 1560 participants, reported pain incidence 72 hours after canal obturation as a dichotomous outcome (Al‐Negrish 2006; Albashaireh 1998; Ghoddusi 2006; Ince 2009; Mulhern 1982; Oginni 2004; Risso 2008; Soltanoff 1978; Wang 2010). No difference was found between groups, with low statistical heterogeneity (RR 0.99, 95% CI 0.84 to 1.17; I2 = 33%; Figure 5; Analysis 2.1).
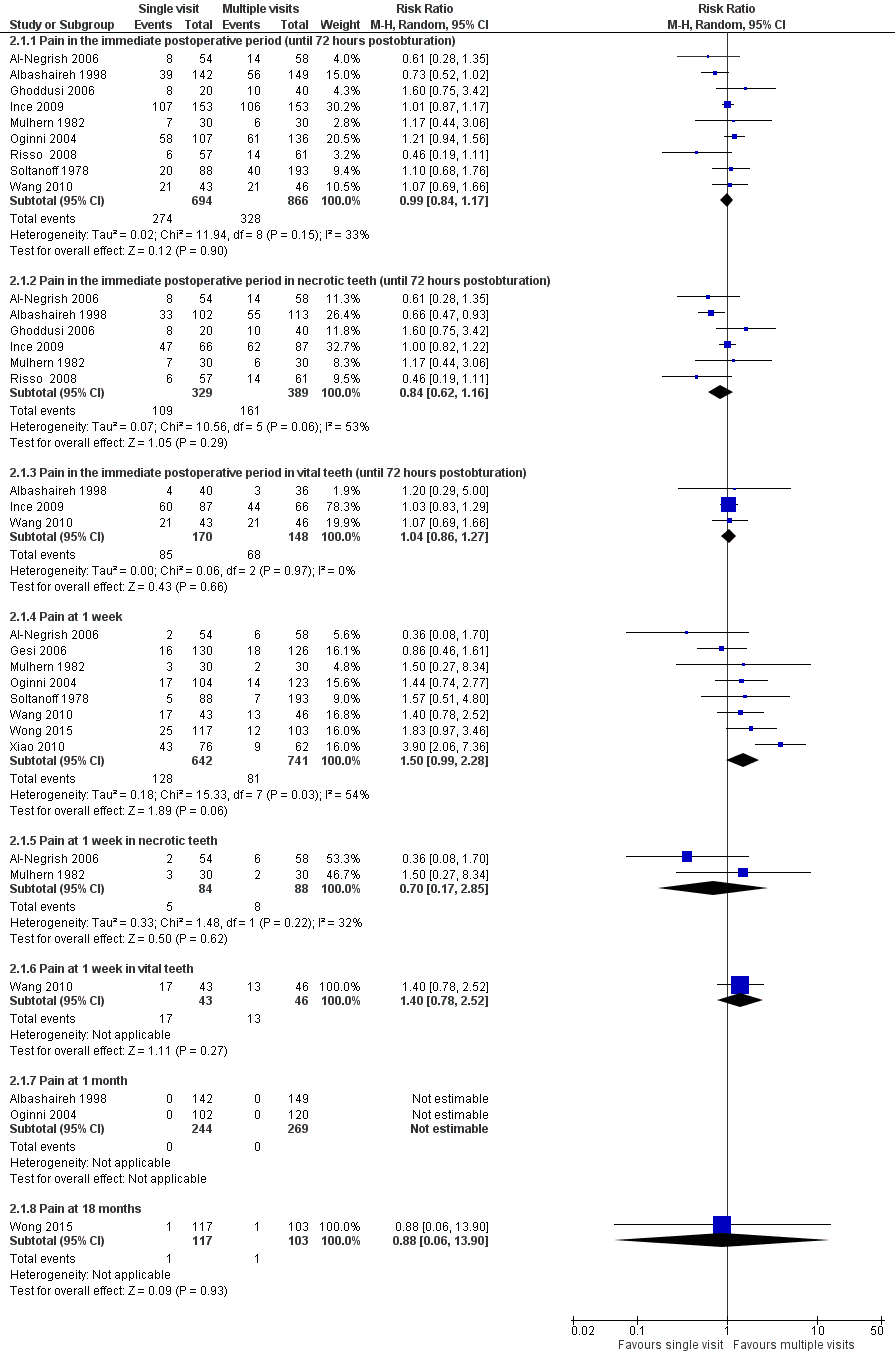
Forest plot of comparison: 2 Secondary outcomes, outcome: 2.1 Pain (dichotomous)
The evidence related to this outcome, as assessed using the GRADE method and presented in 'summary of findings Table for the main comparison, is moderate quality.
Gesi 2006, Ghoddusi 2006, Mulhern 1982, and Xiao 2010 reported pain incidence in the interappointment period of the multiple‐visit RoCT; such data are not included in the meta‐analysis, as they cannot be compared with a similar outcome of the single‐visit approach.
Four studies with 414 participants evaluated postoperative pain as a continuous outcome (DiRenzo 2002; Patil 2016; Singh 2012; Wang 2010). In order to perform a meta‐analysis, we standardised the results of the VAS in two studies from a 170 mm scale to a 100 mm scale (DiRenzo 2002; Patil 2016). No difference was found between the two treatments, with no statistical heterogeneity (mean difference (MD) 0.12, 95% CI ‐0.59 to 0.82; I2 = 0%; Analysis 2.2).
Results from Yoldas 2004 were excluded from meta‐analysis of postoperative pain because the data were not stratified according to time of onset. In this study, single‐ and multiple‐visit RoCT showed no significant difference in incidence of pain. The incidence of pain was greatest during the first 48 hours after obturation, and then decreased steadily in the subsequent seven days. Of the 227 participants enrolled in the study, 68 had symptomatic and 159 had asymptomatic teeth. When data were analysed to consider the presence of symptoms before RoCT, postoperative pain was found significantly more often in participants with symptomatic teeth.
Necrotic teeth
Six studies with 718 participants reported immediate pain as a dichotomous outcome in necrotic teeth (Albashaireh 1998; Al‐Negrish 2006; Ghoddusi 2006; Ince 2009; Mulhern 1982; Risso 2008). The pooled estimate from the studies showed no differences between treatments in participants with necrotic teeth (RR 0.84, 95% CI 0.62 to 1.16; I2 = 53%; Figure 5).
Three studies (DiRenzo 2002; Patil 2016; Singh 2012), including a total of 158 participants, evaluated pain in the immediate postoperative period in non‐vital teeth, as a continuous outcome, and found no difference between the two treatment groups, with no statistical heterogeneity (MD ‐0.21, 95% CI ‐0.44 to 0.03; I2 = 0%).
Vital teeth
Three studies analysed immediate postoperative pain as a dichotomous outcome in teeth vital at enrolment, for a total of 318 participants (Albashaireh 1998; Ince 2009; Wang 2010). There was no difference in the pain incidence immediately after RoCT between treatment groups, with no statistical heterogeneity (RR 1.04, 95% CI 0.86 to 1.27; I2 = 0%; Figure 5). One study (30 participants) reported no difference between treatments for postoperative pain as a continuous outcome in vital teeth (Patil 2016).
Pain at one week
Eight studies reported pain at one week as a dichotomous outcome in a total of 1383 participants and suggested that participants treated in a single visit were more likely to experience pain than those treated over multiple visits (Al‐Negrish 2006; Gesi 2006; Mulhern 1982; Oginni 2004; Soltanoff 1978; Wang 2010; Wong 2015; Xiao 2010), though the difference is not statistically significant and the meta‐analysis showed substantial statistical heterogeneity (RR 1.50, 95% CI 0.99 to 2.28; I2 = 54%; Figure 5). The evidence related to this outcome, as assessed using the GRADE method and presented in summary of findings Table for the main comparison, is low‐quality.
Pain at one week in necrotic teeth
Al‐Negrish 2006 and Mulhern 1982 evaluated the incidence of pain one week after the RoCT in non‐vital teeth and found no difference between participants treated in a single visit in comparison to those treated in multiple visits, with low statistical heterogeneity (RR 0.70, 95% CI 0.17 to 2.85; 172 participants, 2 studies, I2 = 32%; Figure 5).
Pain at one week in vital teeth
Wang 2010 was the only study reporting the incidence of pain at one week after RoCT in teeth vital at enrolment. This study found no difference in this outcome between participants treated in one single visit in comparison to those treated in multiple visits (RR 1.40, 95% CI 0.78 to 2.52; Figure 5).
Pain at one month
Only two studies reported pain at one month after canal obturation as a dichotomous outcome (Albashaireh 1998; Oginni 2004). In both studies, no participant had persistent pain at one month. Thus, a meta‐analysis of the studies was not possible.
Pain at 18 months
Wong 2015 was the only study reporting incidence of pain at 18 months after RoCT. This study found no difference in this outcome between participants treated in one single visit in comparison to those treated in multiple visits (RR 0.88, 95% CI 0.06 to 13.90; 220 participants).
Swelling or flare‐up
We considered all studies reporting flare‐up as swelling and those where flare‐up was defined as swelling (with or without moderate or intense pain). For definitions of flare‐up, see Table 2. We included four studies with 281 participants in a meta‐analysis (DiRenzo 2002; Ghoddusi 2006; Mulhern 1982; Wang 2010), which did not find a difference between single and multiple visits (RR 1.36, 95% CI 0.66 to 2.81; I2 = 0%). The evidence related to this outcome, as assessed using the GRADE method and presented in summary of findings Table for the main comparison, is low quality.
Swelling or flare‐up in necrotic teeth
Two studies reported data on this outcome in necrotic teeth for a total of 120 participants (Ghoddusi 2006; Mulhern 1982), showing no difference between participants treated in a single visit versus those treated in multiple visits, with no statistical heterogeneity (RR 1.52, 95% CI 0.70 to 3.31; I2 = 0%).
Swelling or flare‐up in vital teeth
Wang 2010 was the only study reporting the incidence of swelling or flare‐up in teeth vital at enrolment. This study found no difference between participants treated in one single visit in comparison to those treated in multiple visits (RR 1.07, 95% CI 0.07 to 16.57; 89 participants).
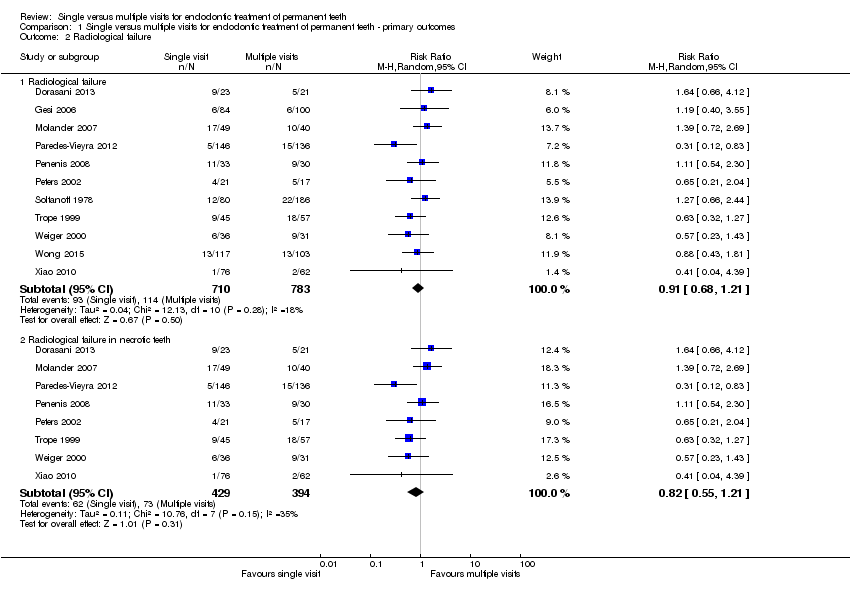
Painkiller use
Use of painkillers was reported by four studies (Mulhern 1982; Soltanoff 1978; Wang 2010; Yoldas 2004), including a total of 648 participants. Pooled estimates from all studies showed that the use of painkillers after RoCT was more common among participants undergoing the single‐visit approach (RR 2.35, 95% CI 1.60 to 3.45; Figure 6). The studies were homogeneous (Chi² = 1.81, df = 3 (P = 0.61); I² = 0%). The evidence related to this outcome, as assessed using the GRADE method and presented in summary of findings Table for the main comparison, is moderate quality.

Forest plot of comparison: 2 Secondary outcomes, outcome: 2.4 Painkiller use
Necrotic teeth
Mulhern 1982 reported the use of painkillers in necrotic teeth, showing no difference between participants treated in a single visit versus those treated in multiple visits (RR 1.25, 95% CI 0.37 to 4.21; 60 participants).
Sinus track or fistula formation
Only two studies reported persistent sinus track or fistula, both of which included necrotic teeth only (Paredes‐Vieyra 2012; Penenis 2008). The studies were homogeneous and did not find a difference between single and multiple visits (RR 0.98, 95% CI 0.15 to 6.48; 345 participants; I2 = 0%, Figure 7). The evidence related to this outcome, as assessed using the GRADE method and presented in summary of findings Table for the main comparison is low quality.

Forest plot of comparison: 2 Secondary outcomes, outcome: 2.6 Any complication
Any complication
We could extrapolate accurate data for 10 studies: Akbar 2013; Albashaireh 1998; DiRenzo 2002; Gesi 2006; Ince 2009; Mulhern 1982; Paredes‐Vieyra 2012; Penenis 2008; Risso 2008; Xiao 2010. A total of 1686 participants were included in this meta‐analysis, which did not find a difference between single and multiple visits; the studies were homogeneous (RR 0.92, 95% CI 0.77 to 1.11; I2 = 18%; Figure 7). The evidence related to this outcome, as assessed using the GRADE method and presented in summary of findings Table for the main comparison is moderate quality.
Any complication in necrotic teeth
We could extrapolate accurate data on necrotic teeth from nine studies (Akbar 2013; Albashaireh 1998; DiRenzo 2002; Ince 2009; Mulhern 1982; Paredes‐Vieyra 2012; Penenis 2008; Risso 2008; Xiao 2010), with a total of 1201 participants. Meta‐analysis showed no difference between participants treated in a single visit versus those treated in multiple visits, with low statistical heterogeneity (RR 0.88, 95% CI 0.68 to 1.13; I2 = 34%; Figure 7).
Any complication in vital teeth
There were three studies (Albashaireh 1998; Gesi 2006; Ince 2009), including 485 participants, available to analyse the frequencies of any complication. No difference in frequency of complications was found between participants treated in a single visit versus those treated in multiple visits, with no statistical heterogeneity (RR 1.02, 95% CI 0.83 to 1.25; I2 = 0%; Figure 7).
Discussion
Summary of main results
This review included 25 randomised controlled trials (RCTs) with a total of 3780 participants undergoing root canal treatment (RoCT) in a single visit or over multiple visits. Only one study reported data on dental extraction due to endodontic problems (Wong 2015).
The results of this review show that, at present, there is no evidence of a substantial advantage of one of the two approaches of RoCT we compared.
Endodontic success indicators can be short‐ or long‐term. The short‐term indicators concern the absence of any postoperative discomfort, the most important short‐term outcome of RoCT. Pain perception is highly subjective and modulated by multiple physical and psychological factors, and the measurement of pain is fraught with hazards and opportunities for errors. The level of discomfort must be rated in categories arranged in advance and exactly described (for example, slight pain: the tooth involved was slightly painful for a time, regardless of duration, but no need existed to take analgesics). From the results obtained in this review, there is evidence that the incidence of postobturation pain (evaluated at different times and using both dichotomous and continuous data) is similar in single‐ and multiple‐visit RoCT, although pain at one week and painkiller use might be less in people undergoing multiple‐visit RoCT. It is possible that in the single‐visit approach the working time is longer, causing a more severe acute inflammatory response. Another factor could be the beneficial effect of the intracanal medication in the between‐visit interval.
There is no evidence of a difference in the incidence of short‐term swelling between people undergoing the single and multiple‐visit approach. Among the four studies considering this outcome (DiRenzo 2002; Ghoddusi 2006; Mulhern 1982; Wang 2010), one evaluated teeth with vital pulp only (Wang 2010). Only two participants (one from the single‐visit group and one from the multiple‐visit group) experienced slight swelling and flare‐up that required a visit to the clinic the day after obturation. The Ghoddusi 2006 study is of particular interest. In fact, when no interappointment canal medication was employed, the incidence of swelling was very similar in the two groups, while when calcium hydroxide was left in the canals between visits, the multiple‐visit treatment performed much better. Such a difference may have occurred because normal saline solution was used as the sole irrigant during RoCT. Thus, with the single‐visit approach, nothing with any antibacterial activity was included in the RoCT. While with the multiple‐visit treatment employing interappointment medication, antibacterial activity was provided by calcium hydroxide.
Only two studies reported data on sinus track or fistula formation and from the data available there is no evidence of a difference between RoCT performed in a single visit versus multiple visits (Paredes‐Vieyra 2012; Penenis 2008).
Long‐term success is based mainly on the healing of periapical lesions, whenever present, and the prevention of new lesions. The healing rate can be established by radiographic interpretation, a method very dependent on human visual perception. There is no evidence of a difference, however, in terms of radiological healing between people treated in a single visit when compared with those undergoing a multiple‐visit approach.
We pooled data from 10 studies to assess the incidence of any complication reported by participants in the short‐term (Akbar 2013; Albashaireh 1998; DiRenzo 2002; Gesi 2006; Ince 2009; Mulhern 1982; Paredes‐Vieyra 2012; Penenis 2008; Risso 2008; Xiao 2010), finding no evidence of a difference between the two groups.
We performed subgroup analysis for vital and necrotic teeth when data were available. In the previous version of this systematic review (Figini 2007), a meta‐analysis of a small number of studies suggested a possible difference in radiological healing among necrotic teeth, in favour of single‐visit RoCT; this result was not confirmed in this update, where a larger number of studies were included in the meta‐analysis.
Thus, the effectiveness of single‐ and multiple‐visit RoCT does not seem to be substantially different. Most short‐ and long‐term complications are similar in terms of frequency, although patients undergoing single‐visit RoCT may experience a higher level of pain at one week after RoCT and are more likely to take analgesics.
Overall completeness and applicability of evidence
The available evidence is from a range of countries and is applicable to healthy patients aged over 10 years. Identified trials did not include patients with depressed immune systems, patients with other illnesses, or elderly patients. The results of this review may or may not be generalisable to these groups, which would be expected to have different rates of short‐ and long‐term endodontic success.
The majority of the trials were conducted in public structures (hospitals or university clinics) and only one trial was performed in a private practice. This may influence the generalisability of our results, with particular regard to the number of operators involved in the RoCT or their clinical skill, as those in the included studies varied from expert endodontists working in referral centres to postgraduate students. Whether results would be similar for general dental practitioners is unclear.
About half of the studies (11/25) did not report the use of rubber dam during the RoCT procedure. Although the use of rubber dam is considered part of the RoCT, and for this reason several authors may have not reported its use during the procedure, this might represent a limit in terms of external validity.
Quality of the evidence
On the basis of the criteria used in the critical appraisal of the studies, only three of the 25 included studies resulted in a low risk of bias (Molander 2007; Singh 2012; Wang 2010). Less than 25% of the studies were at low risk of selection bias (i.e. with inadequate random sequence generation and/or allocation concealment). We judged the risk of attrition bias, detection bias, reporting bias, and other bias, as low in more than 75% of the studies. When assessed using the GRADE method (Atkins 2004), evidence on immediate pain (dichotomous), painkiller use and any complication, resulted in moderate quality; radiological failure, swelling or flare‐up, pain at one week and persistent sinus tract or fistula resulted in low quality; extraction due to endodontic problems resulted in very low quality (summary of findings Table for the main comparison).
Potential biases in the review process
We have taken steps to minimise the bias in every step of the review. We searched databases, and trial registries with no language limitations, to identify all the relevant reports. We tried to contact the study authors for missing data through e‐mails. We did not detect publication bias on the basis of the funnel plots analysis (Figure 8).

Funnel plot of comparison: 2 Signs, outcome: 2.3 Radiological failure
Agreements and disagreements with other studies or reviews
We found four other systematic reviews that compared pain and long‐term radiological healing between single‐ and multiple‐visit RoCT. The Sathorn 2005 review focused on postoperative pain and flare‐up, coming to the same conclusions as our present review. Su 2011 and Zhang 2015 analysed the differences between the two approaches, in teeth with infected root canals only. The results of the two reviews did not differ significantly from those of our subgroup analysis in necrotic teeth. In the systematic review by Su 2011, when short‐term postobturation pain was analysed, a benefit for patients undergoing single‐visit RoCT was evident. This difference from our result reporting no statistical difference can be explained by the difference in inclusion criteria (necrotic teeth only), which led to a different set of studies being combined. The review by Wong 2014 concluded that the studies reported in the literature showed that neither single‐visit endodontic treatment nor multiple‐visit treatment could guarantee the absence of postoperative pain. It found that neither single‐visit endodontic treatment nor multiple‐visit treatment had superior results in terms of healing or success rate, which our review also found.

Study flow diagram: review update

'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study

'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies

Forest plot of comparison: 1 Primary outcomes, outcome: 1.2 Radiological failure
Forest plot of comparison: 2 Secondary outcomes, outcome: 2.1 Pain (dichotomous)

Forest plot of comparison: 2 Secondary outcomes, outcome: 2.4 Painkiller use

Forest plot of comparison: 2 Secondary outcomes, outcome: 2.6 Any complication

Funnel plot of comparison: 2 Signs, outcome: 2.3 Radiological failure

Comparison 1 Single versus multiple visits for endodontic treatment of permanent teeth ‐ primary outcomes, Outcome 1 Extraction due to endodontic problems.
Comparison 1 Single versus multiple visits for endodontic treatment of permanent teeth ‐ primary outcomes, Outcome 2 Radiological failure.

Comparison 2 Single versus multiple visits for endodontic treatment of permanent teeth ‐ secondary outcomes, Outcome 1 Pain (dichotomous).

Comparison 2 Single versus multiple visits for endodontic treatment of permanent teeth ‐ secondary outcomes, Outcome 2 Pain (continuous).

Comparison 2 Single versus multiple visits for endodontic treatment of permanent teeth ‐ secondary outcomes, Outcome 3 Swelling or flare‐up.

Comparison 2 Single versus multiple visits for endodontic treatment of permanent teeth ‐ secondary outcomes, Outcome 4 Painkiller use.

Comparison 2 Single versus multiple visits for endodontic treatment of permanent teeth ‐ secondary outcomes, Outcome 5 Persistent sinus track or fistula.

Comparison 2 Single versus multiple visits for endodontic treatment of permanent teeth ‐ secondary outcomes, Outcome 6 Any complication.
| Single‐visit compared to multiple‐visit treatment for endodontic treatment of permanent teeth | ||||||
| Patient or population: people receiving endodontic treatment of permanent teeth | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | Number of participants | Quality of the evidence | Comments | |
| Risk with multiple‐visit treatment | Risk with single‐visit treatment | |||||
| Tooth extraction due to endodontic problems | 19 per 1000 | 9 per 1000 | RR 0.44 | 220 | ⊕⊝⊝⊝ | |
| Radiological failure | 146 per 1000 | 132 per 1000 | RR 0.91 | 1493 | ⊕⊕⊝⊝ | |
| Pain (dichotomous) ‐ pain in the immediate postoperative period (until 72 hours postobturation) | 379 per 1000 | 375 per 1000 | RR 0.99 | 1560 | ⊕⊕⊕⊝ | |
| Pain (dichotomous) ‐ pain at 1 week | 109 per 1000 | 164 per 1000 | RR 1.50 | 1383 | ⊕⊕⊝⊝ | |
| Swelling or flare‐up | 81 per 1000 | 110 per 1000 | RR 1.36 | 281 | ⊕⊕⊝⊝ | |
| Painkiller use | 97 per 1000 | 228 per 1000 | RR 2.35 | 648 | ⊕⊕⊕⊝ | |
| Sinus track or fistula formation | 12 per 1000 | 12 per 1000 | RR 0.98 | 345 | ⊕⊕⊝⊝ | |
| Any complication | 286 per 1000 | 263 per 1000 | RR 0.92 | 1686 | ⊕⊕⊕⊝ | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 The study was judged at high risk of bias. | ||||||
| Classification | Success (binary) | Failure (binary) |
| PAI score 1 (normal periapical), PAI score 2 (bone structural changes) | PAI score 3 (structural changes with mineral loss), PAI score 4 (radiolucency), PAI score 5 (radiolucency with features of exacerbation) | |
| Success (normal to slightly thickened periodontal ligament space < 1 mm, elimination of previous rarefaction, normal lamina dura in relation to adjacent teeth, no evidence of resorption) | Questionable (increased periodontal ligament space > 1 mm and < 2 mm, stationary rarefaction or slight repair evident, increased lamina dura in relation to adjacent teeth, evidence of resorption); failure (increased width of periodontal ligament space > 2 mm, lack of osseous repair within rarefaction or increased rarefaction, lack of new lamina dura, presence of osseous rarefactions in periradicular areas where previously none existed) | |
| Healed (normal pattern of trabecular bone and normal width of periodontal ligament space) | Improved (reduction in lesion size); failed (increased or no change in the lesion size) | |
| Healed (normal pattern of trabecular bone and normal width of periodontal ligament space) | Increased width of the periodontal space, pathological findings | |
| Success (A) the width and contour of the periodontal ligament is normal, or there is a slight radiolucent zone around apical | Uncertain (B) the radiolucency is clearly decreased but additional follow‐up is not available; failure (C) there is an unchanged, increased, or new periradicular radiolucency | |
| Complete healing: no clinical signs and symptoms, radiographically a periodontal ligament space of normal width | Incomplete healing: no clinical signs and symptoms, radiographically a reduction of the lesion in size or an unchanged lesion within an observation time of 4 years. No healing: clinical signs and symptoms indicating an acute phase of apical periodontitis and\or radiographically a persisting lesion after a follow‐up time of 4 to 5 years and\or a new lesion formed at an initially uninvolved root of a multi‐rooted tooth | |
| Healed (by Rx but the criteria not specified in a satisfactory way) | Not healed (by Rx but the criteria not specified in a satisfactory way) | |
| Normal periapical condition or unclear apical condition (widened apical periodontal space or diffused lamina dura) | Presence of periapical radiolucency when there was a distinct radiolucent area associated with the apical portion of the root | |
| Normal ‐ normal appearance of the surrounding | Apical periodontitis ‐ periapical radiolucency observed Periapical status not classified ‐ the quality of the radiograph was insufficient for examination of the periapical structure | |
| PAI: periapical index | ||
| Study | Definition of flare‐up |
| Moderate to severe postoperative pain or moderate to severe swelling that begins 12 to 48 hours after treatment and lasts at least 48 hours | |
| Percentage of participants experiencing moderate to severe pain evaluated after 2 and 7 days | |
| Swelling that needs antibiotics and narcotic analgesics | |
| Swelling | |
| Swelling | |
| Participant report of pain not controlled with over‐the‐counter medication or increasing swelling or both | |
| Intensive pain (visual analogue scale > 4) | |
| Swelling | |
| Severe postoperative pain or occurrence of swelling or both |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Extraction due to endodontic problems Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Radiological failure Show forest plot | 11 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 2.1 Radiological failure | 11 | 1493 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.68, 1.21] |
| 2.2 Radiological failure in necrotic teeth | 8 | 823 | Risk Ratio (M‐H, Random, 95% CI) | 0.82 [0.55, 1.21] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain (dichotomous) Show forest plot | 12 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.1 Pain in the immediate postoperative period (until 72 hours postobturation) | 9 | 1560 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.84, 1.17] |
| 1.2 Pain in the immediate postoperative period in necrotic teeth (until 72 hours postobturation) | 6 | 718 | Risk Ratio (M‐H, Random, 95% CI) | 0.84 [0.62, 1.16] |
| 1.3 Pain in the immediate postoperative period in vital teeth (until 72 hours postobturation) | 3 | 318 | Risk Ratio (M‐H, Random, 95% CI) | 1.04 [0.86, 1.27] |
| 1.4 Pain at 1 week | 8 | 1383 | Risk Ratio (M‐H, Random, 95% CI) | 1.50 [0.99, 2.28] |
| 1.5 Pain at 1 week in necrotic teeth | 2 | 172 | Risk Ratio (M‐H, Random, 95% CI) | 0.70 [0.17, 2.85] |
| 1.6 Pain at 1 week in vital teeth | 1 | 89 | Risk Ratio (M‐H, Random, 95% CI) | 1.40 [0.78, 2.52] |
| 1.7 Pain at 1 month | 2 | 513 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 1.8 Pain at 18 months | 1 | 220 | Risk Ratio (M‐H, Random, 95% CI) | 0.88 [0.06, 13.90] |
| 2 Pain (continuous) Show forest plot | 4 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 Pain in the immediate postoperative period (until 72 hours postobturation) | 4 | 414 | Mean Difference (IV, Random, 95% CI) | 0.12 [‐0.59, 0.82] |
| 2.2 Pain in the immediate postoperative period in necrotic teeth (until 72 hours postobturation) | 3 | 158 | Mean Difference (IV, Random, 95% CI) | ‐0.21 [‐0.44, 0.03] |
| 2.3 Pain in the immediate postoperative period in vital teeth (until 72 hours postobturation) | 1 | 30 | Mean Difference (IV, Random, 95% CI) | 0.60 [‐1.03, 2.23] |
| 3 Swelling or flare‐up Show forest plot | 4 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 3.1 Swelling or flare‐up | 4 | 281 | Risk Ratio (M‐H, Random, 95% CI) | 1.36 [0.66, 2.81] |
| 3.2 Swelling or flare‐up in necrotic teeth | 2 | 120 | Risk Ratio (M‐H, Random, 95% CI) | 1.52 [0.70, 3.31] |
| 3.3 Swelling or flare‐up in vital teeth | 1 | 89 | Risk Ratio (M‐H, Random, 95% CI) | 1.07 [0.07, 16.57] |
| 4 Painkiller use Show forest plot | 4 | 648 | Risk Ratio (M‐H, Random, 95% CI) | 2.35 [1.60, 3.45] |
| 5 Persistent sinus track or fistula Show forest plot | 2 | 345 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.15, 6.48] |
| 6 Any complication Show forest plot | 10 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 6.1 Any complication | 10 | 1686 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.77, 1.11] |
| 6.2 Any complication in necrotic teeth | 9 | 1201 | Risk Ratio (M‐H, Random, 95% CI) | 0.88 [0.68, 1.13] |
| 6.3 Any complication in vital teeth | 3 | 485 | Risk Ratio (M‐H, Random, 95% CI) | 1.02 [0.83, 1.25] |

