Transpyloric versus gastric tube feeding for preterm infants
Abstract
Background
Enteral feeding tubes for preterm infants may be placed in the stomach (gastric tube feeding) or in the upper small bowel (transpyloric tube feeding). There are potential advantages and disadvantages to both routes.
Objectives
To determine the effect of feeding via the transpyloric route versus feeding via the gastric route on feeding tolerance, growth and development, and adverse consequences (death, gastro‐intestinal disturbance including necrotising enterocolitis, aspiration pneumonia, chronic lung disease, pyloric stenosis) in preterm infants.
Search methods
We used the standard search strategy of the Cochrane Neonatal Review Group. This included searches of the Cochrane Central Register of Controlled Trials (The Cochrane Library 2012, Issue 3), MEDLINE, EMBASE, and CINAHL (to June 2012), conference proceedings, and previous reviews.
Selection criteria
Randomised or quasi‐randomised controlled trials comparing transpyloric with gastric tube feeding in preterm infants.
Data collection and analysis
We extracted data using the standard methods of the Cochrane Neonatal Review Group with separate evaluation of trial quality and data extraction by two review authors. We synthesised data using a fixed‐effect model and reported typical risk ratio (RR), risk difference (RD), and mean difference (MD).
Main results
We found nine eligible trials in which a total of 359 preterm infants participated. All of the trials contained methodological weaknesses with lack of allocation concealment, absence of blinding of caregivers or assessors, and incomplete follow‐up being the major potential sources of bias. The included trials did not detect any statistically significant effects on feeding tolerance or in‐hospital growth rates. Meta‐analyses found that infants allocated to receive transpyloric feeding had a higher risk of gastro‐intestinal disturbance (typical RR 1.48 (95% confidence interval (CI) 1.05 to 2.09); typical RD 0.09 (95% CI 0.02 to 0.17); number needed to treat for an additional harmful outcome (NNTH) 10 (95% CI 6 to 50); six studies, 245 infants) and all‐case mortality (typical RR 2.46 (95% CI 1.36 to 4.46); typical RD 0.16 (95% CI 0.07 to 0.26); NNTH 6 (95% CI 4 to 14); six studies, 217 infants). However, the trial that contributed most weight to these findings was likely to have been affected by selective allocation of the less mature and sicker infants to transpyloric feeding. We did not find any statistically significant differences in the incidence of other adverse events, including necrotising enterocolitis, intestinal perforation, and aspiration pneumonia.
Authors' conclusions
The available data do not provide evidence of any beneficial effect of transpyloric feeding for preterm infants. Some evidence of harm exists, including a higher risk of gastrointestinal disturbance and mortality, but these findings should be interpreted and applied cautiously because of methodological weaknesses in the included trials.
PICOs
Plain language summary
Transpyloric versus gastric tube feeding for preterm infants
Preterm infants often have poor co‐ordination of sucking and swallowing and this can delay the establishment of safe oral feeding. Enteral feeds may be delivered through a catheter passed via the nose or the mouth into either the stomach (gastric feeding) or beyond the stomach into the next part of the bowel (transpyloric feeding). This review of trials found that babies receiving transpyloric feeding had more adverse events without any evidence of benefit over gastric feeding.
Authors' conclusions
Background
Description of the condition
Preterm infants have poor co‐ordination of sucking and swallowing and this can delay the establishment of safe oral feeding. Enteral feeds may be delivered through a catheter passed via the nose or the mouth into the stomach or upper small intestine. The gastro‐oesophageal valve is more lax and gastric peristalsis and emptying is less effective in preterm than in term infants (Berseth 1989). A further concern with intragastric feeding for preterm infants is that lower oesophageal sphincter laxity results in gastro‐oesophageal reflux (GOR) and, putatively, GOR‐attributed apnoea or bradycardia and aspiration pneumonia (Misra 2007; Malcolm 2009).
Description of the intervention
Placement of the enteral feeding tube in the duodenum or jejunum (transpyloric feeding) rather than the stomach (gastric feeding) ensures delivery of enteral feeds to the main sites of nutrient absorption and has the theoretical advantage of decreasing the potential for oesophageal reflux, reflux‐associated apnoea or bradycardia, and aspiration pneumonia.
Why it is important to do this review
Feeding by the transpyloric route also has potential problems. The gastric phase of the digestion is by‐passed and secretion of upper intestinal hormones and growth factors may be impaired (Milner 1981). There is also a risk that potentially pathogenic organisms, which would have been removed in the acidic environment of the stomach, may be delivered directly into upper small bowel (Dellagrammaticas 1983). These factors might contribute to a higher risk of necrotising enterocolitis in infants fed via the transpyloric route as suggested by observational studies (Vazquez 1980; Vinocur 1990). Additionally, transpyloric feeding tubes are difficult to position and, unlike gastric tubes, the position of the transpyloric catheter must be confirmed with imaging. Following placement, the transpyloric tube may still migrate back to the stomach. Serious adverse events including cases of intestinal perforation and of pyloric stenosis have also been reported (Boros 1974; Raine 1982).
Objectives
To determine the effect of feeding via the transpyloric route versus feeding via the gastric route on feeding tolerance, growth and development, and adverse consequences (death, gastro‐intestinal disturbance including necrotising enterocolitis, aspiration pneumonia, chronic lung disease, pyloric stenosis) in preterm infants.
Methods
Criteria for considering studies for this review
Types of studies
Controlled trials using either random or quasi‐random patient allocation.
Types of participants
Preterm infants who receive enteral tube feeding.
Types of interventions
Trials comparing transpyloric versus gastric tube feeding with catheters passed via the nose or mouth. Trials of gastrostomy, duodenostomy, or jejunostomy feeding were not included. Trials in which parenteral nutritional support was available during the period of advancement of enteral feeds were acceptable, provided that the groups received similar treatment other than the route of enteral feeding.
Types of outcome measures
Primary: feed tolerance and growth
-
Days from birth to establish full enteral tube feeds independently of parenteral fluids or nutrition.
-
Growth: rates of change in weight, length, head circumference, or skinfold thickness.
Secondary: adverse effects
-
Death prior to hospital discharge.
-
Gastrointestinal disturbance such as diarrhoea or feeding intolerance that results in cessation of enteral feeding.
-
Necrotising enterocolitis confirmed by at least two of the following features:
-
abdominal radiograph showing pneumatosis intestinalis or gas in the portal venous system or free air in the abdomen;
-
abdominal distension with abdominal radiograph with gaseous distension or frothy appearance of bowel lumen (or both);
-
blood in stool;
-
lethargy, hypotonia, or apnoea (or combination of these); or
-
a diagnosis confirmed at surgery or autopsy.
-
-
Aspiration pneumonia/pneumonitis: clinical or radiological evidence of lower respiratory tract compromise that has been attributed to covert or evident aspiration of gastric contents.
-
Intestinal perforation.
-
Pyloric stenosis requiring surgical intervention.
-
Frequency of episodes of prolonged apnoea (no respiratory effort > 20 seconds) or bradycardia (< 60 beats per minute), or apnoea/bradycardia necessitating stimulation, oxygen administration increase, or positive pressure ventilation.
-
Chronic lung disease defined as an additional oxygen requirement at 36 weeks post menstrual age.
Search methods for identification of studies
We used the standard search strategy of the Cochrane Neonatal Review Group.
Electronic searches
We searched the Cochrane Central Register of Controlled Trials (The Cochrane Library 2012, Issue 3), MEDLINE (1966 to June 2012), and EMBASE (1980 to June 2012). The search strategy used the following text words and Medical Subject Headings: [Infant‐Newborn/, OR infan*, OR neonat*, OR prematur*, OR preterm], AND [Infant‐Nutrition/, OR Feeding‐Methods/, OR Intubation, Gastrointestinal/, OR gastric, OR transpyloric, OR nasoduodenal, OR nasojejunal]. We used a search filter in MEDLINE and EMBASE to limit retrieval to clinical trials. We did not apply any language restrictions.
We searched ClinicalTrials.gov, Current Controlled Trials, and WHO Clinical Trials Registry for completed or ongoing trials.
Searching other resources
We examined the references in studies identified as potentially relevant. We also searched the abstracts from the annual meetings of the Pediatric Academic Societies (1993 to 2012), the European Society for Pediatric Research (1995 to 2011), the UK Royal College of Paediatrics and Child Health (2000 to 2012), and the Perinatal Society of Australia and New Zealand (2000 to 2012). We considered trials reported only as abstracts to be eligible if sufficient information was available from the report, or from contact with the authors, to fulfil the inclusion criteria.
Data collection and analysis
We used the standard methods of the Cochrane Neonatal Review Group.
Selection of studies
Two review authors screened the title and abstract of all studies identified by the above search strategy. We assessed the full text of any potentially eligible reports and excluded those studies that did not meet all of the inclusion criteria. We discussed any disagreements until consensus was achieved.
Data extraction and management
We used a data collection form to aid extraction of relevant information from each included study. Two review authors extracted the data separately. We discussed any disagreements until consensus was achieved. We asked the investigators for further information if data from the trial reports were insufficient.
Assessment of risk of bias in included studies
We used the criteria and standard methods of the Cochrane Neonatal Review Group to assess the methodological quality of any included trials. Additional information from the trial authors was requested to clarify methodology and results as necessary. We evaluated and reported the following issues in the 'Risk of bias' tables:
-
Sequence generation: We categorised the method used to generate the allocation sequence as:
-
low risk: any random process e.g. random number table; computer random number generator;
-
high risk: any non random process e.g. odd or even date of birth; patient case‐record number;
-
unclear.
-
-
Allocation concealment: We categorised the method used to conceal the allocation sequence as:
-
low risk: e.g. telephone or central randomisation; consecutively numbered sealed opaque envelopes;
-
high risk: open random allocation; unsealed or non‐opaque envelopes, alternation; date of birth;
-
unclear.
-
-
Blinding: We assessed blinding of participants, clinicians and caregivers, and outcome assessors separately for different outcomes and categorised the methods as:
-
low risk;
-
high risk;
-
unclear.
-
-
Incomplete outcome data: We described the completeness of data including attrition and exclusions from the analysis for each outcome and any reasons for attrition or exclusion where reported. We assessed whether missing data were balanced across groups or were related to outcomes. Where sufficient information was reported or supplied by the trial authors, we re‐included missing data in the analyses. We categorised completeness as:
-
low risk: < 20% missing data;
-
high risk: > 20% missing data;
-
unclear.
-
Measures of treatment effect
We calculated risk ratio (RR) and risk difference (RD) for dichotomous data and mean difference (MD) for continuous data with respective 95% confidence intervals (CI). We determined the number needed to treat for an additional beneficial outcome (NNTB) or an additional harmful outcome (NNTH) for a statistically significant RD.
Unit of analysis issues
The unit of analysis is the participating infant in individually randomised trials and the neonatal unit for cluster‐randomised trials.
Dealing with missing data
We requested missing study data from the trial investigators.
Assessment of heterogeneity
If more than one trial was included in a meta‐analysis, we examined the treatment effects of individual trials and heterogeneity between trial results by inspecting the forest plots. We calculated the I² statistic for each analysis to quantify inconsistency across studies and describe the percentage of variability in effect estimates that may be due to heterogeneity rather than sampling error. If substantial (I² > 50%) heterogeneity was detected, we explored the possible causes (for example, differences in study design, participants, interventions, or completeness of outcome assessments) in sensitivity and subgroup analyses.
Assessment of reporting biases
If more than five trials were included in a meta‐analysis, we conducted a funnel plot analysis.
Data synthesis
We used a fixed‐effect model for meta‐analyses.
Subgroup analysis and investigation of heterogeneity
We pre‐specified subgroup analysis of trials of routine (non‐selective) use of transpyloric feeding versus selective transpyloric feeding for infants with confirmed or suspected GOR or GOR‐attributed apnoea or bradycardia.
Results
Description of studies
We found nine eligible trials (Van Caillie 1975; Wells 1975; Pyati 1976; Roy 1977; Drew 1979; Pereira 1981; Whitfield 1982; Laing 1986; Macdonald 1992; see table Characteristics of included studies).
Included studies
All of the included studies were undertaken in the 1970s or early 1980s. Most recruited very low birth weight infants (birth weight < 1500 g). However, only infants grown appropriately for gestational age were eligible for inclusion in most of the trials. In some trials infants who required respiratory or ventilatory support were not eligible for inclusion. Feeding by the allocated route was usually started within the first few days after birth when enteral feeds were commenced. Feeding tubes used were made of silastic, polyvinyl, or polypropylene. The transpyloric tubes were placed in the second or third part of duodenum or the jejunum with the assistance of positioning of the infant and peristalsis. In all of the trials the position of the tube was confirmed radiologically. All trials reported nutrient (usually energy) intake and short‐term growth as the primary outcomes. In most reports, data on adverse events (including death, necrotising enterocolitis, intestinal perforation, and aspiration pneumonia) were available.
Excluded studies
Ten reports were excluded following inspection of the full report (Cheek 1973; Valman 1973; Boros 1974; Chen 1974; Uauy 1975; Wolfsdorf 1975; Avery 1977; Celestin 1978; Price 1978; Agarwal 1980; see table Characteristics of excluded studies).
Risk of bias in included studies
All of the trials were small (total N = 359) and none presented a power or sample size calculation.
Allocation
In most of the trials, allocation was not concealed and the assignment of infants to one or other feeding route could have been predicted.
Blinding
The caregivers or assessors were aware of the intervention to which infants had been allocated in all of the included trials.
Incomplete outcome data
In general, short‐term outcome data assessment was complete. However, growth data were often not reported for infants who had failed to complete the study, for example because the enteral tube feeding method was changed (that is, not an intention‐to‐treat analysis). For adverse outcomes, reporting was generally complete or available indirectly from the text of the report.
Effects of interventions
Primary outcomes: feed tolerance and growth
1. Days from birth to establish full enteral tube feeds independently of parenteral fluids or nutrition
This outcome was reported by Macdonald 1992 and by Pereira 1981. These investigators did not find any statistically significant differences but the data were presented without standard deviations and could not be used in a meta‐analysis.
2. Growth
All of the included trials reported short‐term (prior to discharge from hospital) growth outcomes. One study provided data on longer‐term (following discharge from hospital) growth (Whitfield 1982).
a. Short‐term weight gain (Outcome 1.1)
Seven trials reported no statistically significant differences in the rate of weight gain (Pyati 1976; Roy 1977; Drew 1979; Whitfield 1982; Laing 1986; Macdonald 1992). Two trials found statistically significantly higher rates of weight gain in the group allocated to transpyloric feeding (Van Caillie 1975; Wells 1975). Four trials provided data in a form that could be used in a meta‐analysis (Roy 1977; Van Caillie 1975; Whitfield 1982; Macdonald 1992). The combined data from these studies did not reveal a statistically significant difference: mean difference (MD) ‐0.5 (95% confidence interval (CI) ‐27 to 16) g/week (Figure 1).

Forest plot of comparison: 1 Transpyloric versus gastric tube feeding for preterm infants: Growth, outcome: 1.1 Change in weight (g/week).
b. Short‐term linear growth (Outcome 1.2)
In the five trials that reported linear growth, the investigators did not find any statistically significant difference in the rate of increase in crown heel length (Roy 1977; Drew 1979; Pereira 1981; Laing 1986; Macdonald 1992). Only three studies provided data in a form that could be used in a meta‐analysis (Roy 1977; Laing 1986; Macdonald 1992). The combined data from these studies did not reveal a statistically significant difference: MD ‐0.7 (95% CI ‐2.4 to 1.0) mm/week (Figure 2).

Forest plot of comparison: 2 Transpyloric versus gastric tube feeding for preterm infants: Adverse events, outcome: 2.1 Death prior to hospital discharge.
c. Short‐term head growth (Outcome 1.3)
In the five trials that reported head growth, the investigators did not find any statistically significant difference in the rate of increase in occipito‐frontal head circumference (Roy 1977; Drew 1979; Pereira 1981; Laing 1986; Macdonald 1992). Only two reports provided data in a form that could be used in a meta‐analysis (Laing 1986; Macdonald 1992). The combined data from these studies did not demonstrate a statistically significant difference: MD 0.6 (95% CI ‐0.9 to 2.1) mm/week.
d. Short‐term change skinfold thickness (Outcome 1.4)
This was reported in one study (Roy 1977). The investigators did not find a statistically significant difference: MD ‐0.2 (95% CI ‐1.2 to 0.8) mm/week.
e. Longer‐term growth
Growth following hospital discharge was reported in only one of the trials (Whitfield 1982). At the expected date of delivery, body weight and occipito‐frontal head circumference were statistically significantly lower in the nasojejunal group: MD ‐0.3 (95% CI ‐0.6 to ‐0.03) kg, and ‐1.0 (95% CI ‐1.7 to ‐0.3) cm, respectively. At three and six months after the expected date of delivery, there were no statistically significant differences between the groups in body weight or occipito‐frontal head circumference. However, there was considerable loss to follow‐up, mainly in the transpyloric feeding group where 12 of the recruited 28 infants were not assessed at six months.
Secondary outcomes: adverse effects
Seven of the trials reported adverse events including death, necrotising enterocolitis, gastrointestinal disturbance, aspiration pneumonia, and intestinal perforation. Adverse events were often reported as withdrawal criteria rather than as pre‐defined outcome measures. Although there was often incomplete follow‐up of recruited infants with regard to growth data, in the majority of the reports we have been able to determine the incidence of adverse events for the complete or near complete cohort.
1. Death before discharge from hospital (Outcome 2.1)
Six trials reported this outcome (Wells 1975; Van Caillie 1975; Drew 1979; Whitfield 1982; Laing 1986; Macdonald 1992). Only Laing 1986 found that nasojejunal feeding was associated with a statistically significantly higher mortality rate. The other trials did not find any statistically significant difference. Meta‐analysis found a statistically significantly higher rate of death in the infants who were fed via the transpyloric route: typical risk ratio (RR) 2.5 (95% CI 1.4 to 4.5); typical risk difference (RD) 0.16 (95% CI 0.07 to 0.26); number needed to treat for an additional harmful outcome (NNTH) 6 (95% CI 4 to 14) (Figure 2). There was not any evidence of heterogeneity (I² = 0%) or funnel plot asymmetry (Figure 3).

Funnel plot of comparison: 2 Transpyloric versus gastric tube feeding for preterm infants: Adverse events, outcome: 2.1 Death prior to hospital discharge.
In a sensitivity analysis (Outcome 2.2), Laing 1986 was excluded because of the differences in the baseline characteristics of the feeding groups. When only the remaining five studies were included in the meta‐analysis, the difference was not statistically significant: typical RR 2.2 (95% CI 0.9 to 5.4); typical RD 0.1 (95% CI 0.00 to 0.2).
2. Gastrointestinal disturbance such as diarrhoea or feeding intolerance (Outcome 2.3)
Seven trials reported this outcome (Van Caillie 1975; Roy 1977; Drew 1979; Pereira 1981; Whitfield 1982; Laing 1986; Macdonald 1992). None of the individual trials found any statistically significant difference in the incidence of gastrointestinal disturbance. Meta‐analysis found a statistically significantly higher risk of gastrointestinal disturbance in the infants fed via the transpyloric route: typical RR 1.48 (95% CI 1.05 to 2.09); typical RD 0.09 (95% CI 0.02 to 0.17); NNTH 10 (95% CI 6 to 50) (Figure 4). There was not any evidence of heterogeneity (I² = 0%) but funnel plot inspection suggested asymmetry and over‐representation of smaller trials with large effect sizes (Figure 5).

Forest plot of comparison: 2 Transpyloric versus gastric tube feeding for preterm infants: Adverse events, outcome: 2.3 Gastrointestinal disturbance (including diarrhoea) prior to hospital discharge.

Funnel plot of comparison: 2 Transpyloric versus gastric tube feeding for preterm infants: Adverse events, outcome: 2.3 Gastrointestinal disturbance (including diarrhoea) prior to hospital discharge.
In a sensitivity analysis (Outcome 2.4), removing Laing 1986, there remained a statistically significant difference in the incidence of gastrointestinal disturbance: typical RR 1.4 (95% CI 1.02 to 2.0); typical RD 0.1 (95% CI 0.01 to 0.21); NNTH 10 (95% CI 5 to 100).
3. Necrotising enterocolitis (Outcome 2.5)
Seven trials (Van Caillie 1975; Wells 1975; Drew 1979; Pereira 1981; Whitfield 1982; Laing 1986; Macdonald 1992 ) reported this outcome. None of the individual trials, nor a meta‐analysis of the studies, found any statistically significant difference in the incidence of necrotising enterocolitis: typical RR 0.6 (95% CI 0.3 to 1.5); typical RD ‐0.03 (95% CI ‐0.09 to 0.03).
In a sensitivity analysis (Outcome 2.6), removing Laing 1986, there was not any statistically significant difference in the incidence of necrotising enterocolitis: typical RR 0.9 (95% CI 0.3 to 2.6); typical RD ‐0.01 (95% CI ‐0.08 to 0.06).
4. Aspiration pneumonia/pneumonitis (Outcome 2.7)
Four trials (Van Caillie 1975; Pyati 1976; Drew 1979; Pereira 1981; Macdonald 1992) reported this outcome. None of the individual trials, nor a meta‐analysis of the studies, found any statistically significant difference in the incidence of aspiration pneumonia/pneumonitis. Meta‐analysis: typical RR 1.35 (95% CI 0.44 to 4.14); typical RD 0.02 (95% CI ‐0.06 to 0.1).
5. Intestinal perforation (Outcome 2.8)
Four trials (Van Caillie 1975; Roy 1977; Pereira 1981; Whitfield 1982) reported this outcome. Of the 129 infants studied, there was only one reported case of intestinal perforation. None of the individual trials, nor a meta‐analysis of the studies, found any statistically significant difference in the incidence of aspiration pneumonia. Meta‐analysis: typical RR 2.3 (95% CI 0.1 to 50.1); typical RD: 0.01 (95% CI ‐0.05 to 0.08).
6. Pyloric stenosis
This outcome was not reported in any of the trials.
7. Frequency of apnoea/bradycardia
This outcome was not reported in any of the trials.
8. Chronic lung disease
This outcome was not reported in any of the trials.
Discussion
Summary of main results
We did not find any evidence of benefit of transpyloric compared with gastric feeding in preterm infants. We found some evidence that transpyloric feeding increases the risk of gastrointestinal disturbance and mortality. However, many of the studies included in the review had a variety of methodological weaknesses and these findings need to be interpreted and applied with caution (Figure 6).

'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
Overall completeness and applicability of evidence
Only two of the included trials assessed the effect of transpyloric versus gastric tube feeding on measures of 'feed tolerance' such as the time taken to establish enteral feeding. With regard to growth parameters, in many of the trials the growth data from infants who developed complications during the study period, or in whom enteral tube placement was unsuccessful, were not reported. In the largest included trial only 41 of the 80 infants who entered the study were included in the growth data analysis (Laing 1986). In Drew 1979, of the 66 infants allocated to a feeding route, there were outcome data for only 44 infants. Given these levels of loss to follow‐up, the findings should be regarded with caution. For example, it may be that the repeated failed attempts to position the transpyloric tube introduces a delay in starting or establishing nutritional input. Since it is plausible that such delay may affect growth, the findings may have been different in a true intention‐to‐treat analysis.
Gastro‐oesophageal reflux (GOR), aspiration, and apnoea/bradycardia
Observational studies have suggested that transpyloric feeding may reduce the frequency or degree of GOR and GOR‐related apnoea/bradycardia and prevent pulmonary aspiration of intestinal contents (Misra 2007; Malcolm 2009). This review did not find any evidence that transpyloric feeding affected the risk of aspiration pneumonia but a modest yet important effect size has not been excluded. However, none of the included trials assessed the effect of transpyloric versus gastric tube feeding on the incidence of GOR‐related apnoea/bradycardia, and none of the trials specifically recruited infants with confirmed or suspected GOR or GOR‐attributed problems. Although uncertainty exists as to whether GOR is an important cause of apnoea/bradycardia in preterm infants (Peter 2002; Di Fiore 2005; Corvaglia 2009), it has been proposed that clinical trials are warranted to evaluate whether transpyloric feeding is an effective prevention or treatment option in preterm infants with clinical problems attributed to GOR (Misra 2007; Malcolm 2009).
Quality of the evidence
The finding that transpyloric feeding increased the risk of mortality should also be interpreted carefully since it is possible that the pooled estimate in the meta‐analysis is over‐inflated by allocation bias in several of the trials. In particular, the outcomes for Laing 1986 (which contributes > 50% of the weight to the pooled risk ratio) may have been affected by preferential allocation of less mature or sicker infants to the transpyloric feeding group. When this study was excluded from the meta‐analysis the increase in mortality in the transpyloric group was not statistically significant.
Similarly, the increase in the risk of gastrointestinal disturbance in infants who received transpyloric feeding may have been inflated by allocation bias as well as by ascertainment or surveillance biases since caregivers and clinicians were aware of the allocated intervention in all of the trials. We did not detect any statistically significant differences in the incidences of necrotising enterocolitis or intestinal perforation between the feeding groups. Additionally, although it may be pragmatic to compare continuous transpyloric feeding with intermittent or bolus gastric feeding, as was the case in seven of the included trials, this co‐intervention may also have affected the outcomes. The Cochrane review that compared continuous nasogastric tube feeding versus intermittent bolus feeding for preterm infants concluded that the clinical benefits and harms could not be reliably discerned from the available data from randomised trials (Premji 2011).

Forest plot of comparison: 1 Transpyloric versus gastric tube feeding for preterm infants: Growth, outcome: 1.1 Change in weight (g/week).

Forest plot of comparison: 2 Transpyloric versus gastric tube feeding for preterm infants: Adverse events, outcome: 2.1 Death prior to hospital discharge.

Funnel plot of comparison: 2 Transpyloric versus gastric tube feeding for preterm infants: Adverse events, outcome: 2.1 Death prior to hospital discharge.

Forest plot of comparison: 2 Transpyloric versus gastric tube feeding for preterm infants: Adverse events, outcome: 2.3 Gastrointestinal disturbance (including diarrhoea) prior to hospital discharge.

Funnel plot of comparison: 2 Transpyloric versus gastric tube feeding for preterm infants: Adverse events, outcome: 2.3 Gastrointestinal disturbance (including diarrhoea) prior to hospital discharge.

'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
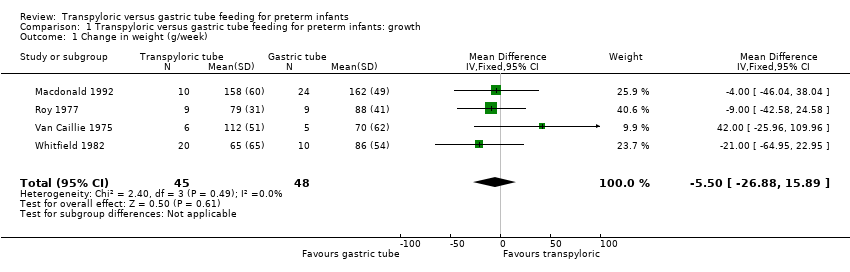
Comparison 1 Transpyloric versus gastric tube feeding for preterm infants: growth, Outcome 1 Change in weight (g/week).

Comparison 1 Transpyloric versus gastric tube feeding for preterm infants: growth, Outcome 2 Change in crown heel length (mm/week).

Comparison 1 Transpyloric versus gastric tube feeding for preterm infants: growth, Outcome 3 Change in occipito‐frontal head circumference (mm/week).

Comparison 1 Transpyloric versus gastric tube feeding for preterm infants: growth, Outcome 4 Change in subscapular skinfold thickness (mm/week).
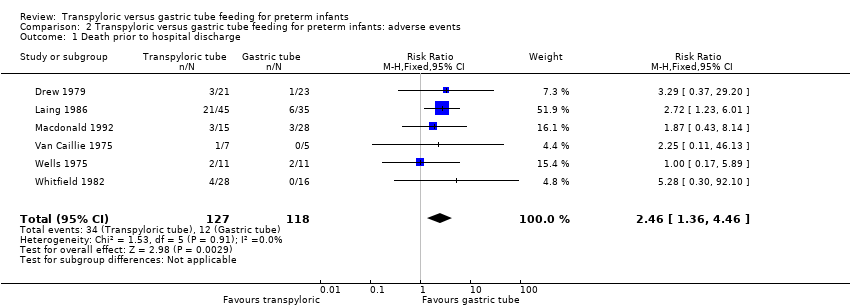
Comparison 2 Transpyloric versus gastric tube feeding for preterm infants: adverse events, Outcome 1 Death prior to hospital discharge.

Comparison 2 Transpyloric versus gastric tube feeding for preterm infants: adverse events, Outcome 2 Death prior to hospital discharge (excluding Laing 1986).
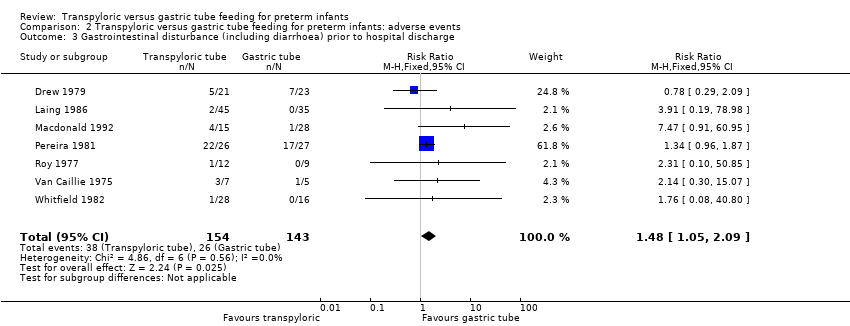
Comparison 2 Transpyloric versus gastric tube feeding for preterm infants: adverse events, Outcome 3 Gastrointestinal disturbance (including diarrhoea) prior to hospital discharge.

Comparison 2 Transpyloric versus gastric tube feeding for preterm infants: adverse events, Outcome 4 Gastrointestinal disturbance (including diarrhoea) prior to hospital discharge (excluding Laing 1986).

Comparison 2 Transpyloric versus gastric tube feeding for preterm infants: adverse events, Outcome 5 Necrotising enterocolitis prior to hospital discharge.

Comparison 2 Transpyloric versus gastric tube feeding for preterm infants: adverse events, Outcome 6 Necrotising enterocolitis prior to hospital discharge (excluding Laing 1986).

Comparison 2 Transpyloric versus gastric tube feeding for preterm infants: adverse events, Outcome 7 Aspiration pneumonia prior to hospital discharge.

Comparison 2 Transpyloric versus gastric tube feeding for preterm infants: adverse events, Outcome 8 Intestinal perforation prior to hospital discharge.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Change in weight (g/week) Show forest plot | 4 | 93 | Mean Difference (IV, Fixed, 95% CI) | ‐5.50 [‐26.88, 15.89] |
| 2 Change in crown heel length (mm/week) Show forest plot | 3 | 93 | Mean Difference (IV, Fixed, 95% CI) | ‐0.67 [‐2.36, 1.02] |
| 3 Change in occipito‐frontal head circumference (mm/week) Show forest plot | 2 | 75 | Mean Difference (IV, Fixed, 95% CI) | 0.56 [‐0.95, 2.08] |
| 4 Change in subscapular skinfold thickness (mm/week) Show forest plot | 1 | 18 | Mean Difference (IV, Fixed, 95% CI) | ‐0.20 [‐1.18, 0.78] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Death prior to hospital discharge Show forest plot | 6 | 245 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.46 [1.36, 4.46] |
| 2 Death prior to hospital discharge (excluding Laing 1986) Show forest plot | 5 | 165 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.19 [0.89, 5.35] |
| 3 Gastrointestinal disturbance (including diarrhoea) prior to hospital discharge Show forest plot | 7 | 297 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.48 [1.05, 2.09] |
| 4 Gastrointestinal disturbance (including diarrhoea) prior to hospital discharge (excluding Laing 1986) Show forest plot | 6 | 217 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.43 [1.02, 2.01] |
| 5 Necrotising enterocolitis prior to hospital discharge Show forest plot | 7 | 298 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.63 [0.26, 1.53] |
| 6 Necrotising enterocolitis prior to hospital discharge (excluding Laing 1986) Show forest plot | 6 | 218 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.32, 2.58] |
| 7 Aspiration pneumonia prior to hospital discharge Show forest plot | 5 | 171 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.35 [0.44, 4.14] |
| 8 Intestinal perforation prior to hospital discharge Show forest plot | 4 | 129 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.31 [0.10, 50.85] |

