| Comparison | | No. of participants (studies) | Direct evidence | Network meta‐analysis |
| | | | Absolute risk difference, NNTB | Quality of evidence | | Absolute risk difference, NNTB | Quality of evidence |
| Outcome: ACR50 | | | RR (95% CI) | | | RR (95% Crl) | | |
| All biologics | vs. placebo | 548 (3 studies) | 4.10 (1.97 to 8.55) | 14% (6% to 21%), NNTB = 8 (4 to 23) | ⊕⊕⊕⊖ moderate (downgraded for imprecision)a | n/a |
| All biologics + MTX | vs. MTX/DMARD | 1479 (3 studies) | 4.07 (2.76 to 5.99) | 16% (10% to 21%), NNTB = 7 (5 to 11) | ⊕⊕⊕⊕ highb | n/a |
| TNF biologic + MTX | vs. MTX/DMARD | 461 (1 study) | 2.84 (1.49 to 5.40) | 12% (6% to 18%), NNTB = 9 (5 to 25) | ⊕⊕⊕⊖ moderate (downgraded for imprecision)a | 2.97 (1.38 to 6.41) | 10% (2% to 25%), NNTB = 10 (4 to 48) | ⊕⊕⊕⊖ moderate (downgraded for indirectness)c |
| Non‐TNF biologic + MTX | vs. MTX/DMARD | 1018 (2 studies) | 4.99 (3.07 to 8.11) | 18% (10% to 25%), NNTB = 6 (4 to 10) | ⊕⊕⊕⊖ moderate (downgraded for imprecision)a | 5.07 (3.21 to 8.14) | 21% (13% to 30%), NNTB = 5 (3 to 9) | ⊕⊕⊕⊖ moderate (downgraded for indirectness)c |
| Tofacitinib + MTX | vs. MTX/DMARD | 399 (1 study) | 3.24 (1.78 to 5.89) | 19% (12% to 26%), NNTB = 6 (3 to 14) | ⊕⊕⊕⊖ moderate (downgraded for imprecision)a | 3.61 (1.74 to 7.24) | 13% (4% to 29%), NNTB = 8 (4 to 25) | ⊕⊕⊕⊖ moderate (downgraded for indirectness)c |
| Outcome: Health Assessment Questionnaire (HAQ) score, 0‐3 (higher = worse; A "negative sign" indicates improvement): A measure of function | | | MD (95% CI) | | | | | |
| All biologics | vs. placebo | n/a |
| All biologics + MTX | vs. MTX/DMARD | 959 (2 studies) | ‐0.29 (‐0.36 to ‐0.21) | ‐9.7% (‐12% to ‐7.0%), NNTB = 5 (4 to 7) | ⊕⊕⊕⊕ highb | n/a |
| TNF biologic + MTX | vs. MTX/DMARD | 461 (1 study) | ‐0.25 (‐0.40 to ‐0.10) | ‐8.3% (‐13% to ‐3%), NNTB = 5 (7 to 16) | ⊕⊕⊕⊕ highb | ‐0.37 (‐6.67 to 5.89) | ‐12.3% (‐222.3% to 196.3%), NNTB = n/a | ⊕⊕⊖⊖ low (downgraded for imprecision and indirectness)c,d |
| Non‐TNF biologic + MTX | vs. MTX/DMARD | 498 (1 study) | ‐0.37 (‐0.46 to ‐0.28) | ‐12.3% (‐15% to ‐9%), NNTB = 4 (3 to 5) | ⊕⊕⊕⊕ highb | ‐0.25 (‐6.54 to 5.99) | ‐8.3% (‐218% to 199.7%), NNTB = n/a | ⊕⊕⊖⊖ low (downgraded for imprecision and indirectness)c,d |
| Tofacitinib + MTX | vs. MTX/DMARD | 399 (1 study) | ‐0.27 (‐0.39 to ‐0.14) | ‐9% (‐13% to ‐4.7%), NNTB = 5 (4 to 10) | ⊕⊕⊕⊕ highb | ‐0.26 (‐6.57 to 5.95) | ‐8.7% (‐219% to 198.3%), NNTB = n/a | ⊕⊕⊖⊖ low (downgraded for imprecision and indirectness)c,d |
| Outcome: Remission (defined as DAS <1.6 or DAS28 <2.6) | | | RR (95% CI) | | | RR (95% CI) | | |
| All biologics | vs. placebo | 389 (1 study) | 13.51 (1.85 to 98.45) | 9% (5% to 13%), NNTB = 11 (3 to 136) | ⊕⊕⊕⊖ moderate (downgraded for imprecision)a | n/a |
| All biologics + MTX | vs. MTX/DMARD | 959 (2 studies) | 20.73 (4.13 to 104.16) | 10% (8% to 13%), NNTB = 17 (4 to 96) | ⊕⊕⊕⊖ moderate (downgraded for imprecision)a | n/a |
| TNF biologic + MTX | vs. MTX/DMARD | 461 (1 study) | 16.21 (2.24 to 117.51) | 10% (6% to 13%), NNTB = 11 (3 to 110) | ⊕⊕⊕⊖ moderate (downgraded for imprecision)a | 22.27 (3.60 to 400.70) | 8% (1% to 52%), NNTB = 9 (2 to 61) | ⊕⊕⊕⊖ moderate (downgraded for indirectness)c |
| Non‐TNF biologic + MTX | vs. MTX/DMARD | 498 (1 study) | 33.72 (2.08 to 546.23) | 10% (7% to 14%), NNTB = n/ae | ⊕⊕⊕⊖ moderate (downgraded for imprecision)a | 31.20 (6.70 to 456.30) | 11% (3% to 32%), NNTB = 18 (3 to 93) | ⊕⊕⊕⊖ moderate (downgraded for indirectness)c |
| Tofacitinib + MTX | vs. MTX/DMARD | 398 (1 study) | 15.44 (0.93 to 256.10) | 6% (3% to 9%), NNTB = n/ae | ⊕⊕⊕⊖ moderate (downgraded for imprecision)a | n/a |
| Outcome: Radiographic progression | No studies reported this outcome. |
| Outcome: Withdrawals due to adverse events | | | RR (95% CI) | | | RR (95% CI) | | |
| All biologics | vs. placebo | 428 (2 studies) | 0.62 (0.13 to 2.93) | ‐1% (‐4% to 3%), NNTB = n/a | ⊕⊕⊖⊖ low (downgraded for serious imprecision)a,e | n/a |
| All biologics + MTX | vs. MTX/DMARD | 611 (2 studies) | 3.32 (0.86 to 12.85) | 5% (‐3% to 13%), NNTB = n/a | ⊕⊕⊖⊖ low (downgraded for serious imprecision)a,e | n/a |
| TNF biologic + MTX | vs. MTX/DMARD | n/a |
| Non‐TNF biologic + MTX | vs. MTX/DMARD | 611 (2 studies) | 3.32 (0.86 to 12.85) | 5% (‐4% to 13%), NNTB = n/a | ⊕⊖⊖⊖ very low (downgraded for serious imprecision/inconsistency)a,d,f | 1.99 (0.80 to 5.98) | 3% (‐1% to 8%), NNTB = n/a | ⊕⊕⊖⊖ low (downgraded for imprecision and indirectness)c,d |
| Tofacitinib + MTX | vs. MTX/DMARD | 399 (1 study) | 0.99 (0.41 to 2.39) | 0% (‐5% to 5%), NNTB = n/a | ⊕⊕⊖⊖ low (downgraded for serious imprecision)a,d | 1.02 (0.29 to 3.65) | 0% (‐2% to 6%), NNTB = n/a | ⊕⊕⊖c low (downgraded for imprecision and indirectness)c,d |
| Outcome: Serious adverse events | | | RR (95% CI) | | | RR (95% CI) | | |
| All biologics | vs. placebo | 428 (2 studies) | 0.93 (0.51 to 1.68) | ‐1% (‐7% to 5%), NNTB = n/a | ⊕⊕⊖⊖ low (downgraded for serious imprecision)a,d | n/a |
| All biologics + MTX | vs. MTX/DMARD | 1072 (3 studies) | 0.69 (0.44 to 1.09) | ‐2% (‐5% to 1%), NNTB = n/a | ⊕⊕⊕⊖ moderate (downgraded for imprecision)a | n/a |
| TNF biologic + MTX | vs. MTX/DMARD | 461 (1 study) | 0.55 (0.25 to 1.22) | ‐3% (‐8% to 1%), NNTB = n/a | ⊕⊕⊖⊖ low (downgraded for serious imprecision)a,d | 0.56 (0.20 to 1.51) | ‐3% (‐6% to 3%), NNTB = n/a | ⊕⊕⊖⊖ low (downgraded for imprecision and indirectness)c,d |
| Non‐TNF biologic + MTX | vs. MTX/DMARD | 611 (2 studies) | 0.77 (0.45 to 1.33) | ‐1% (‐6% to 3%), NNTB = n/a | ⊕⊕⊖⊖ low (downgraded for serious imprecision)a,d | 0.85 (0.49 to 1.53) | ‐1% (‐4% to 3%), NNTB = n/a | ⊕⊕⊖⊖ low (downgraded for imprecision and indirectness)c,d |
| Tofacitinib + MTX | vs. MTX/DMARD | 399 (1 study) | 0.33 (0.09 to 1.15) | ‐3% (‐7% to 1%), NNTB = n/a | ⊕⊕⊖⊖ low (downgraded for serious imprecision)a,d | 0.32 (0.07 to 1.27) | ‐4% (‐8% to 2%), NNTB = n/a | ⊕⊕⊖⊖ low (downgraded for imprecision and indirectness)c,d |
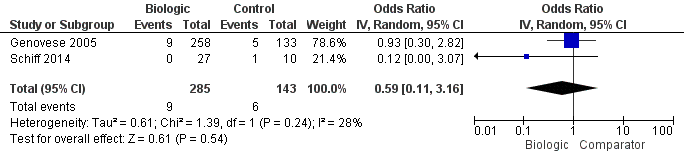
| Outcome: Cancer (note: Peto OR used but can interpret as RR due to low event rate) | | | RR (95% CI) | | | RR (95% CI) | | |
| All biologics | vs. placebo | n/a |
| All biologics + MTX | vs. MTX/DMARD | 550 (2 studies) | 4.54 (0.24 to 85.36) | 1% (‐1% to 2%), NNTB = n/a | ⊕⊕⊖⊖ low (downgraded for serious imprecision)a,d | n/a | | |
| TNF biologic + MTX | vs. MTX/DMARD | 459 (1 study) | 4.54 (0.24 to 85.36) | 1% (‐1% to 2%), NNTB = n/a | ⊕⊕⊖⊖ low (downgraded for serious imprecision)a,d | | | |
| Non‐TNF biologic + MTX | vs. MTX/DMARD | 91 (1 study) | Not estimable | 0% (‐5% to 5%), NNTB = n/a | ⊕⊕⊖⊖ low (downgraded for serious imprecision)a,d | | | |
| Tofacitinib + MTX | vs. MTX/DMARD | n/a | | | | | | | | | |