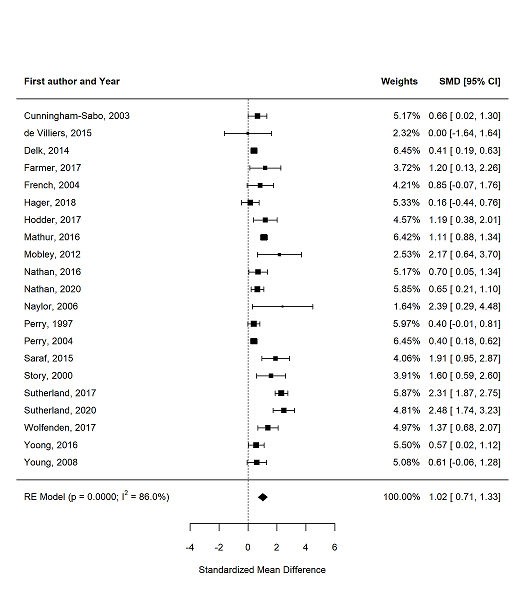
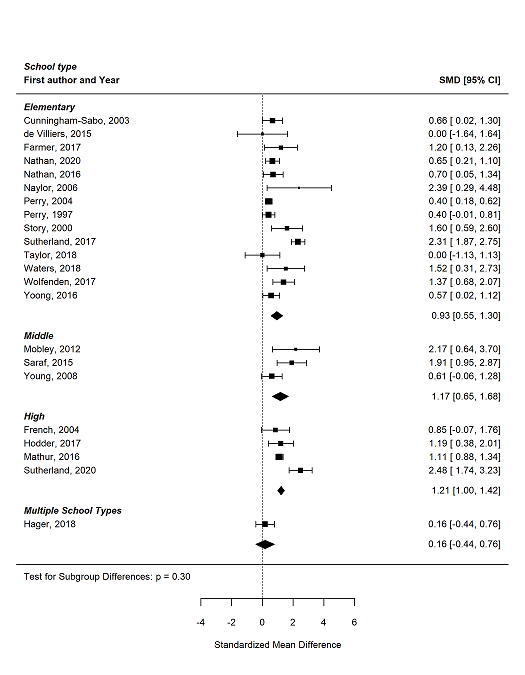
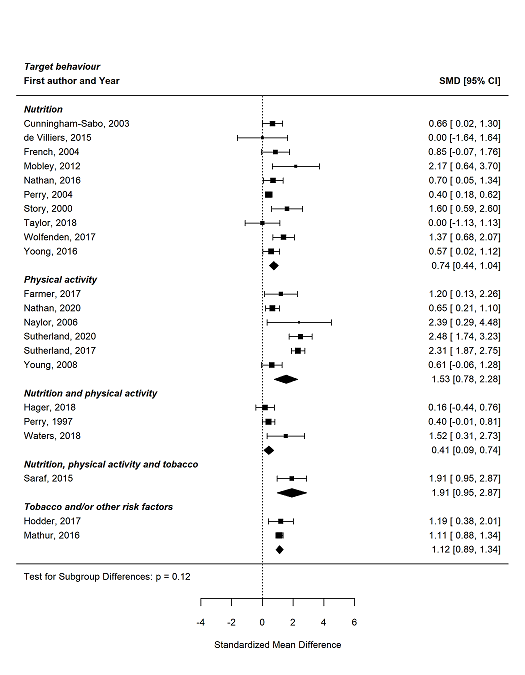
| Cunningham‐Sabo 2003 cRCTa | Nutrition | Clinical practice guidelines, educational materials, educational meetings, educational outreach visits or academic detailing | Usual practice | % calories total fat breakfast (less is better), 2 years, 5‐day menu and recipe data collection. | FU LS mean −3.3 (SE 1.50); P = 0.03 | 0.66 (95% CI 0.02 to 1.30) |
| de Villiers 2015 cRCTa | Nutrition | Local opinion leaders, educational materials, educational outreach visits, educational meetings | Minimal support control | % schools with nutrition related policy (more is better), 3 years, situational analysis (included a structured interview with the school principal and completion of an observation schedule). | No effect estimate between groups reported. FU n/N: intervention 7/8; control 7/8 | 0 (95% CI −1.64 to 1.64) |
| French 2004 cRCT | Nutrition | Local consensus processes, tailored intervention, educational meetings, pay for performance | Usual practice or waitlist control | % low fat à la carte foods (more is better), 2 years, observation of lunchtime meals offered. | No effect estimate between groups reported. FU mean: intervention 42.0 (range 28–58); control 27.7 (16–39) | 0.85 (95% CI −0.07 to 1.76) |
| Hager 2018 cRCT | Nutrition, PA | Tailored interventions, educational meetings, external funding, educational materials, local opinion leaders | Usual practice or waitlist control | Implementation score (more is better), 1 year, online survey. | FU mean: 0.70; P = 0.501b | 0.16 (95% CI −0.44 to 0.76) |
| Lytle 2006 cRCTa | Nutrition | Educational materials, educational meetings, local opinion leaders, local consensus processes | Usual practice or waitlist control | % of items in the foods to promote category (more is better), 3 years, 5‐day service observations. | P = 0.04 (1‐tailed test), no other data reported | NA |
| Mobley 2012 cRCTa | Nutrition | Educational games, educational meetings, external funding, tailored intervention, educational materials, educational outreach or academic detailing, other, the use of information and communication technology | Usual practice or waitlist control | % eliminate milk > 1% fat, all other added sugar beverages and 100% juice only served in < 150 g (more is better), about 3.5 years, data collection on all food/beverage product labels. | No effect estimate between groups reported. FU %: intervention 94%; control 6% | 2.17 (95% CI 0.64 to 3.70) |
| Nathan 2016 cRCTa | Nutrition | Audit and feedback, continuous quality improvement, education materials, education meeting, local consensus process, local opinion leader, tailored intervention, other | Usual practice | Healthy canteen items represent > 50% of products listed on the menu (more is better), 1 year, canteen menu audits. | FU RR (95% CI): 2.03 (95% CI 1.01 to 4.08); P = 0.03 | 0.70 (95% CI 0.05 to 1.34) |
| Perry 1997 cRCT | Nutrition, PA | Educational materials, educational meetings, educational outreach visits or academic detailing, other | Usual practice or waitlist control | Cholesterol in lunches provided (mean milligrams) (less is better), 3 years, menu analysis. | FU mean (SD): intervention 74.9 (SD 18.8); control 83.2 (SD 22.6), P = significant difference | 0.40 (95% CI −0.01 to 0.81) |
| Perry 2004 cRCT | Nutrition | Educational meetings, educational outreach visits or academic detailing, educational materials, local consensus processes, other | Usual practice or waitlist control | Number of fruits and vegetables available at cafeteria (more is better), 2 years, canteen observations. | FU MD 0.48 (SE 0.11); P < 0.01 | 0.40 (95% CI 0.18 to 0.62) |
| Saraf 2015 cRCT | Nutrition, PA and tobacco | Educational games, educational materials, educational meetings, local consensus processes, local opinion leaders, tailored Interventions, other | Usual practice | Schools having a healthy food policy (more is better), 1 year, survey data. | FU n/N: intervention 16/19; control 3/21; P < 0.01 | 1.91 (95% CI 0.95 to 2.87) |
| Story 2000 cRCT | Nutrition | Educational meetings, other | Usual practice | Mean number of fruit and vegetable choices available at cafeteria (more is better), 1 year, observation of food service staff. | No effect estimate between groups reported. Data for 4th and 5th year combined by review authors FU mean: intervention 4.05 (SD 0.66), control 2.9 (SD 0.68) | 1.60 (95% CI 0.59 to 2.60) |
| Taylor 2018 cRCTa | Nutrition | Incentives, educational materials, educational outreach visits or academic detailing | Usual practice or waitlist control | Number of fruit items offered daily at cafeteria (more is better), 9 months, based on produce expenditure. | FU mean: intervention 4.17 (SD 0.98); control 4.17 (SD 0.75); P = 1.00 | 0 (95% CI −1.13 to 1.13) |
| Waters 2017 cRCT | Nutrition, PA | Educational materials, educational outreach visits or academic detailing; local consensus approach, tailored interventions | Usual practice | Existence of Healthy Eating Policy (more is better), 3.5 years, principal survey. | No effect estimate between groups reported. FU n (%): intervention 9 (75%); control 2 (20%) | 1.52 (95% CI 0.31 to 2.73) |
| Wolfenden 2017 cRCTa | Nutrition | Audit and feedback, continuous quality improvement, external funding, education materials, education meeting, education outreach visits or academic detailing, local consensus process, local opinion leader, tailored intervention | Usual practice | Healthy items represented > 50% of canteen menu (more is better), 12–14 months, menu assessment. | FU RR 3.06 (95% CI 1.64 to 5.68); P < 0.01 | 1.37 (95% CI 0.68, 2.07) |
| Yoong 2016 cRCTa | Nutrition | Audit and feedback, continuous quality improvement, education materials, tailored intervention | Usual practice | Percentage of green (healthy) items on canteen menu (more is better), 12 months, menu audit. | FU estimate difference 10.55 (95% CI 2.06 to 19.05); P = 0.014 | 0.57 (95% CI 0.02 to 1.12) |
| Farmer 2017 cRCT | PA | Incentives, local consensus approach, tailored interventions | Usual practice | Play space evaluation score (total) (more is better), 1 year, principal survey. | FU MD 4.50 (95% CI 1.82 to 7.18); P = 0.005 | 1.20 (95% CI 0.13 to 2.26) |
| Nathan 2020 cRCT | PA | Educational outreach visits, centralised technical support, mandate change, identify and prepare champions, provide ongoing consultation, educational material | Usual practice | Teacher implementation (minutes) of a PA policy (structured physical activities) across the week (more is better), 9 months, teacher log book data. | FU MD 36.60 (95% CI 2.68 to 70.51); P = 0.04 | 0.65 (95% CI 0.21 to 1.10) |
| Naylor 2006 cRCT | PA | Educational materials, educational meetings, educational outreach meetings or academic detailing, local consensus process, other, tailored interventions | Usual practice or waitlist control | Minutes per week of planned PA (more is better), 11 months, teacher activity log. | No effect estimate between groups reported. FU mean: usual practice schools: 91.4 (95% CI 70.7 to 112.2); champion schools: 137.8 (95% CI 117.0 to 158.6); liaison schools: 154.8 (95% CI 136.6 to 173.0) | 2.39 (95% CI 0.29 to 4.48) |
| Saunders 2006 cRCTa | PA | Educational materials, educational meetings, educational outreach visits or academic detailing, local consensus processes, local opinion leaders, other | Usual practice or waitlist control | Implementation score (more is better), 12 months, survey. | Did not report aggregate results by group | NA |
| Sutherland 2017 cRCT | PA | Audit and feedback, education materials, education meeting, education outreach visits or academic detailing, local opinion leader, other | Usual practice or waitlist control | Overall lesson quality score (more is better), 6 months, observation checklist. | FU mean: intervention 57.5; control 36.0; P < 0.0b | 2.31 (95% CI 1.87 to 2.75) |
| Sutherland 2020 cRCT | PA | Audit and feedback, educational materials, educational meetings, educational outreach visits or academic detailing, clinical practice guidelines, interprofessional education, local opinion leaders, other | Usual practice | Mean number of PA practices implemented (more is better), 12 months, survey. | FU MD 3.2 (95% CI 2.5 to 3.9); P < 0.001 | 2.48 (95% CI 1.74 to 3.23) |
| Young 2008 cRCT | PA | Education materials, education meetings, educational outreach visits or academic detailing, interprofessional education, local consensus processes, local opinion leaders | Usual practice | Mean number of PA programmes implemented semesters 1–4 (more is better), 2 years, survey. | FU mean: intervention 15.2 (SD 10.8); control 10.1 (SD 4.0); P = 0.8 | 0.61 (95% CI −0.06 to 1.28) |
| Hodder 2017 cRCT | Tobacco, alcohol | Educational outreach visits, educational meetings, local consensus processes, educational materials, external funding, audit and feedback | Usual practice | Number of programmes components used by teachers (more is better), 3 years, survey. | FU mean: intervention 3.1 (SD 1.83); control 1.2 (SD 0.87); P = 0.004 | 1.19 (95% CI 0.38 to 2.01) |
| Mathur 2016 cRCT | Tobacco | Local opinion leader, continuous quality improvement, education materials, education meeting, local consensus process | Usual practice or waitlist control | School policy or rule specifically prohibiting smokeless tobacco use inside school (more is better), 12 months, policy observation checklist. | FU OR 7.54 (95% CI 4.92, 11.60); P value not reported | 1.11 (95% CI 0.88 to 1.34) |
| McCormick 1995 cRCT | Tobacco | Educational meetings, local consensus processes, educational materials | Minimal support control | Number of curriculum activities taught by each teacher, 1 year, implementation checklist. | FU mean: intervention 68.11; control 67.99; P = not significantb | NA |
| Alaimo 2015 Non‐randomised | Nutrition | Clinical practice guidelines, educational materials, educational outreach visits or academic detailing, external funding, local consensus processes, tailored interventions | Usual practice or waitlist control | Mean nutrition education and practice score (more is better), 2 years, survey. | FU mean: intervention 5.9 (SD 3.2); control 4.8 (SD 3.7); P = not significant | 0.32 (95% CI −0.23 to 0.87) |
| Evenhuis 2020 Non‐randomised | Nutrition | Educational materials, educational meeting, audit with feedback, educational outreach visit or academic detailing | Waitlist control | Healthy products available in the cafeteria (more is better), 6 months, audit by canteen supervisor. | FU mean: intervention 77.20 (SD 13.41); control 60.10 (SD 15.67); P = not significant | 1.12 (95% CI 0.18 to 2.07) |
| Heath 2002 Non‐randomised | Nutrition | Educational materials, educational meetings, educational outreach visits or academic detailing | Usual practice | % of fat in breakfast served (less is better), 12 months, menu and recipe audit. | FU %: intervention 20.0%; control 19.2%; P = not significantb | NA |
| Nathan 2012 Non‐randomised | Nutrition | Educational materials, educational meetings, local consensus processes, local opinion leaders, other, monitoring the performance of the delivery of the healthcare, tailored interventions | Minimal support control | Prevalence of fruit and vegetable break (more is better), 11–15 months, principal report. | FU OR 1.91 (95% CI 1.47 to 2.48); P < 0.1 | 0.59 (95% CI 0.32 to 0.86) |
| Simons‐Morton 1988 Non‐randomised | Nutrition | Educational materials, educational outreach visits or academic detailing, local consensus processes, local opinion leaders, managerial supervision, monitoring of performance, other | Usual practice | Fat content in grams per 100 g school cafeteria lunches served (less is better), 1 year, chemical analysis. | No effect estimate between groups reported. FU mean: intervention school 1: −1.8; intervention school 2: −3.4; control school 1: −1.1; control school 2: 0.3 | 0.36 (95% CI 0.07 to 0.66) |
| Whatley Blum 2007 Non‐randomised | Nutrition | Clinical practice guidelines, educational materials, educational meetings, educational outreach visits or academic detailing, external funding, distribution of supplies, local consensus process, other | Usual practice or waitlist control | % meeting nutrient and proportion criteria – à la carte (more is better), 1 year, observations. | No effect estimate between groups reported. FU mean: intervention 69.2 (SD 3.7); control 23.3 (SD 7.6) | 6.90 (95% CI 2.99 to 10.81) |
| Bremer 2018 Non‐randomised | PA | Educational meetings, educational materials | Usual practice | Quantity of PE classes score (more is better), 20 weeks, teacher survey. | FU MD: t(27) = −0.23; P = 0.82 | NA |
| Cheung 2018 Non‐randomised | PA | Educational meeting, educational materials | Usual practice | Total PA time (before school, after school, in class, recess and PE time) (more is better), 1 year, teacher survey. | FU MD 36.3 (95% CI 16.2 to 56.4); P < 0.01 | NA |
| Egan 2018 Non‐randomised | PA | Educational materials; Educational outreach visit or academic detailing, tailored intervention, audit and feedback | Waitlist control | Implementation score (more is better), 12 months, coded interviews with teachers. | FU MD: Mann‐Whitney U analyses 5; P = 0.04 | 0.78 (95% CI −0.88 to 2.44) |
| Sallis 1997 Non‐randomised | PA | Educational materials, educational meetings, educational outreach visits or academic detailing, length of consultation, other | Usual practice or waitlist control | Amount of PE per week (minutes) (more is better), 2.5 years, direct observation. | FU mean: intervention 64.6 (95% CI 59.0, 70.2); control 38.0 (27.9, 48.1); P < 0.001 | 1.10 (95% CI 0.55 to 1.64) |
| Gingiss 2006 Non‐randomised | Tobacco | Educational meetings, educational outreach visits, external funding, local consensus processes | Usual practice | % of schools extremely or moderately active in providing faculty or staff cessation support (more is better), 2 years, survey | No effect estimate between groups reported. FU %: intervention 37%; control 26% | 0.30 (95% CI −0.32 to 0.91) |