Treatment for hepatitis C virus‐associated mixed cryoglobulinaemia
Information
- DOI:
- https://doi.org/10.1002/14651858.CD011403.pub2Copy DOI
- Database:
-
- Cochrane Database of Systematic Reviews
- Version published:
-
- 07 May 2018see what's new
- Type:
-
- Intervention
- Stage:
-
- Review
- Cochrane Editorial Group:
-
Cochrane Kidney and Transplant Group
- Copyright:
-
- Copyright © 2018 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Article metrics
Altmetric:
Cited by:
Authors
Contributions of authors
-
Draft the protocol: NM, ER, CB, JP, MS
-
Study selection: NM, MS
-
Extract data from studies: NM, AF, ER, MS
-
Enter data into RevMan: NM
-
Carry out the analysis: NM
-
Interpret the analysis: NM, MS
-
Draft the final review: All authors
-
Disagreement resolution: JP
-
Update the review: NM, MS
Sources of support
Internal sources
-
None, Other.
External sources
-
None, Other.
Declarations of interest
-
Nuria Montero: none known
-
Alexandre Fava: none known
-
Eva Rodriguez: none known
-
Clara Barrios: none known
-
Josep M Cruzado: none known
-
Julio Pascual: has advisory board and/or clinical trial involvement with Novartis, Astellas, Roche, Wyeth and Genzyme, and has also been an invited speaker at national and international meetings sponsored by Novartis and Astellas
-
Maria Jose Soler: none known
Acknowledgements
We would like to thank Narelle Willis, Fiona Russell and Gail Higgins from Cochrane Kidney and Transplant and the referees for their editorial advice and search methods help during the preparation of this review.
Version history
| Published | Title | Stage | Authors | Version |
| 2018 May 07 | Treatment for hepatitis C virus‐associated mixed cryoglobulinaemia | Review | Nuria Montero, Alexandre Favà, Eva Rodriguez, Clara Barrios, Josep M Cruzado, Julio Pascual, Maria Jose Soler | |
| 2014 Nov 28 | Treatment for hepatitis C virus‐associated cryoglobulinaemic vasculitis | Protocol | Nuria Montero, Clara Barrios, Eva Rodriguez, Julio Pascual, Maria Jose Soler | |
Differences between protocol and review
Although initially we did not want to include cluster trials, at the end we finally included one. Although it was not initially planned and consequently, it was not initially in the protocol, we decided to evaluate activity outcomes as they were the main comparison in the majority of included studies.
Keywords
MeSH
Medical Subject Headings (MeSH) Keywords
- Antiviral Agents [*therapeutic use];
- Blood Component Removal [methods];
- Cryoglobulinemia [*therapy, virology];
- Hepacivirus;
- Hepatitis C [complications, *drug therapy];
- Immunologic Factors [therapeutic use];
- Immunosorbent Techniques;
- Immunosuppressive Agents [therapeutic use];
- Interferons [therapeutic use];
- Randomized Controlled Trials as Topic;
- Rituximab [therapeutic use];
- Skin Diseases [*therapy, virology];
- Vasculitis [etiology, *therapy];
Medical Subject Headings Check Words
Humans;
PICOs

Flow chart showing source and identification of studies for inclusion.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
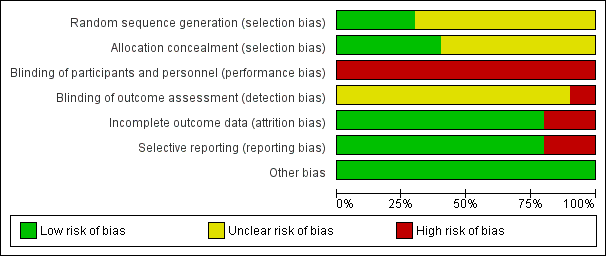
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
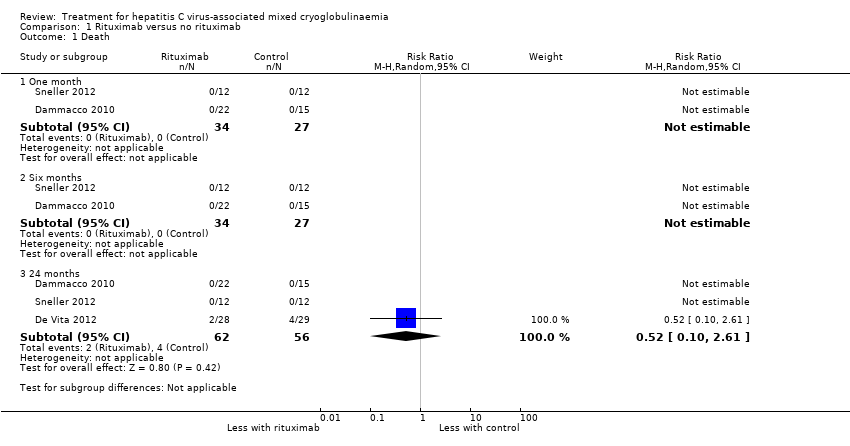
Comparison 1 Rituximab versus no rituximab, Outcome 1 Death.

Comparison 1 Rituximab versus no rituximab, Outcome 2 Clinical manifestations.
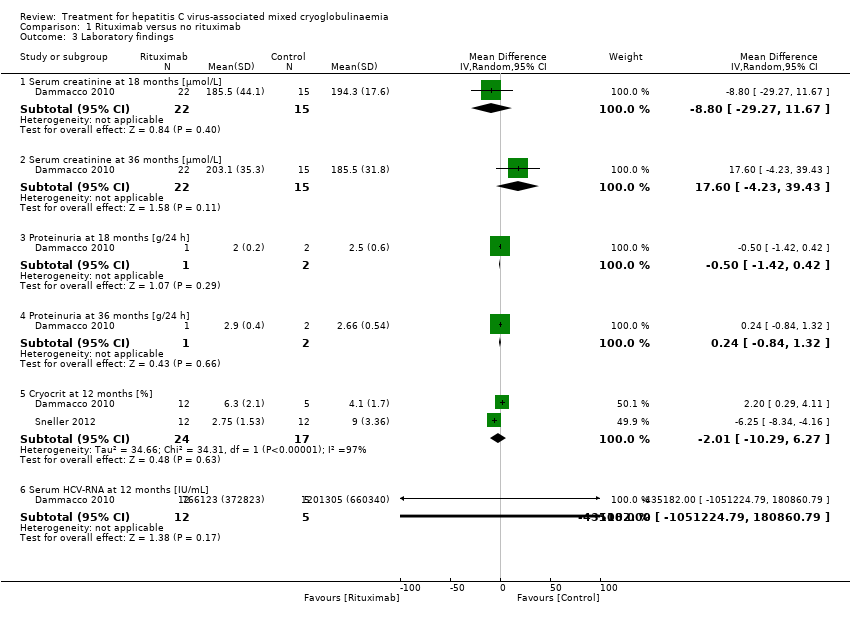
Comparison 1 Rituximab versus no rituximab, Outcome 3 Laboratory findings.
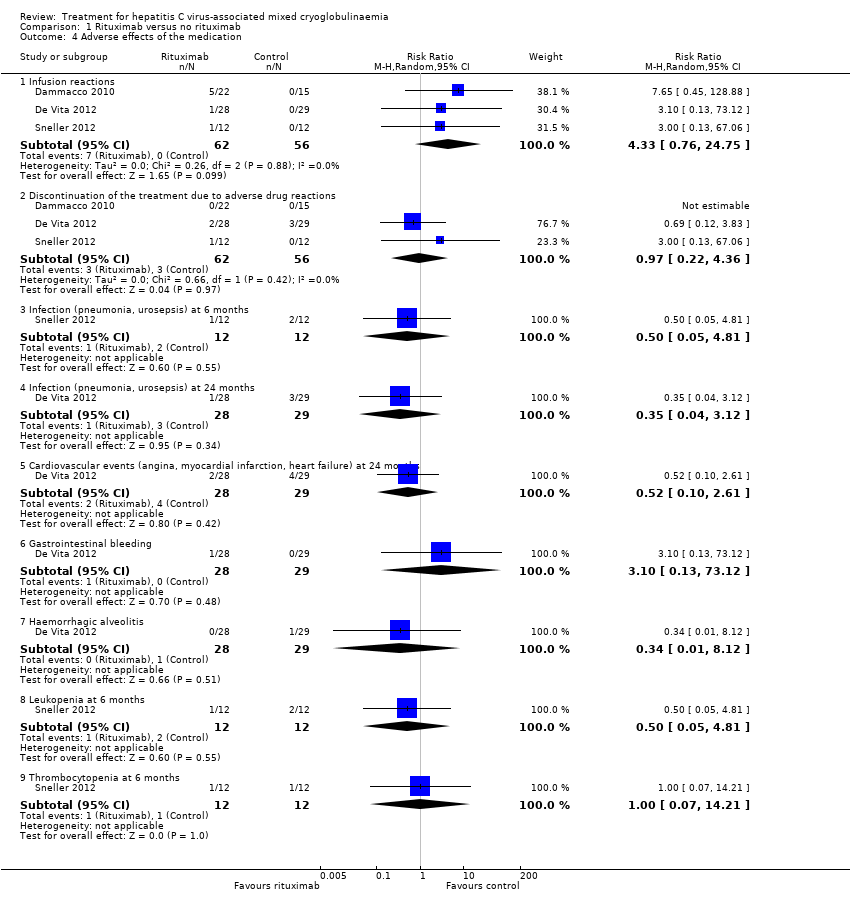
Comparison 1 Rituximab versus no rituximab, Outcome 4 Adverse effects of the medication.
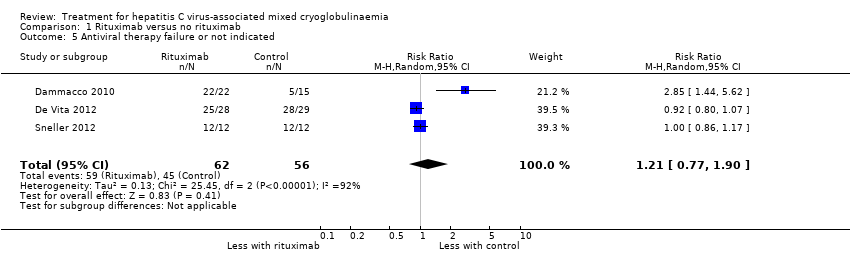
Comparison 1 Rituximab versus no rituximab, Outcome 5 Antiviral therapy failure or not indicated.

Comparison 2 Interferon versus control, Outcome 1 Death.
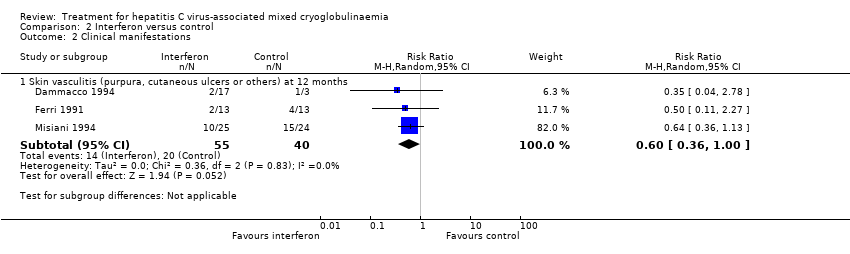
Comparison 2 Interferon versus control, Outcome 2 Clinical manifestations.

Comparison 2 Interferon versus control, Outcome 3 Laboratory findings.
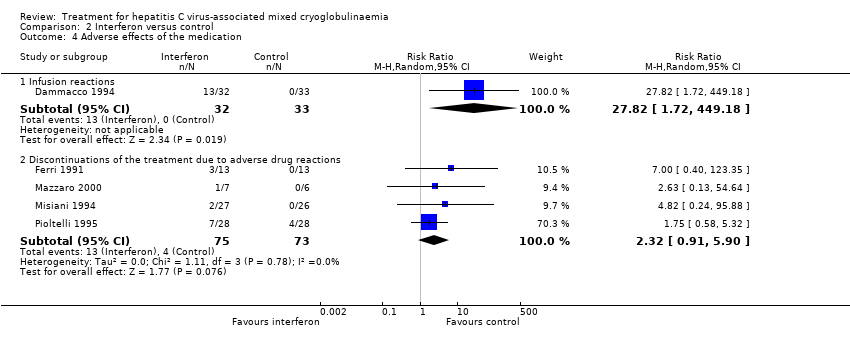
Comparison 2 Interferon versus control, Outcome 4 Adverse effects of the medication.
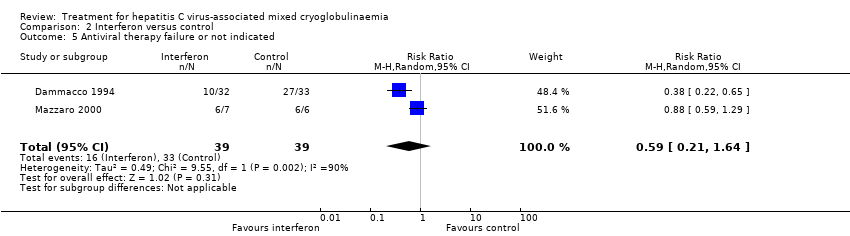
Comparison 2 Interferon versus control, Outcome 5 Antiviral therapy failure or not indicated.

Comparison 3 Interferon for 6 months versus 1 year, Outcome 1 Death at 24 months.

Comparison 4 Immunoadsorption apheresis versus immunosuppressive drug therapy, Outcome 1 Death at 24 months.

Comparison 4 Immunoadsorption apheresis versus immunosuppressive drug therapy, Outcome 2 Clinical manifestations.

Comparison 4 Immunoadsorption apheresis versus immunosuppressive drug therapy, Outcome 3 Laboratory findings.
Comparison 4 Immunoadsorption apheresis versus immunosuppressive drug therapy, Outcome 4 Adverse effects of the medication.
| Rituximab compared to no rituximab for hepatitis C virus‐associated mixed cryoglobulinaemia | |||||
| Patient or population: hepatitis C virus‐associated mixed cryoglobulinaemia | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No. of participants | Quality of the evidence | |
| Risk with no rituximab | Risk with rituximab | ||||
| Skin vasculitis (purpura, cutaneous ulcers or others) at 18 and 24 months: number of affected patients | Study population | RR 0.57 | 78 (2) | ⊕⊕⊕⊝ | |
| 26 per 100 | 15 per 100 | ||||
| SCr at 18 months | The mean SCr at 18 months was 194.3 μmol/L | MD was 8.8 μmol/L lower | ‐ | 37 (1) | ⊕⊕⊕⊝ |
| Cryocrit at 12 months | The mean cryocrit at 12 months was 6.55% | MD was 2.01% lower | ‐ | 41 (2) | ⊕⊕⊝⊝ |
| Adverse effects ‐ infusion reactions: number of events | Study population | RR 4.33 | 118 (3) | ⊕⊕⊕⊝ | |
| 0 per 100 | 0 per 100 | ||||
| Activity outcomes | De Vita 2012 found a significant reduction in the BVAS at 2 months in the rituximab group (from mean ± SD: 11.9 ± 5.4 to 7.1 ± 5.7; P < 0.001), and this difference persisted at 6 months (6.9 ± 6.8; P < 0.001), 12 months (5.4 ± 6.2; P 0.0001), and 24 months (4.4 ± 4.6; P < 0.0001). Without differences in the control group. Sneller 2012 BVAS scores became significantly lower in the rituximab group at month 4 (from 10.2 ± 8.4, at 6 months: 0 ± 0; P < 0.02). Without differences in control group. | ‐ | 81 (2) | ⊕⊕⊕⊝ | |
| *The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | |||||
| GRADE Working Group grades of evidence | |||||
| 1 95% CI overlaps no effect, and the CI fails to exclude important benefit or important harm 2 Base on tests of heterogeneity which test the null hypothesis that all studies have the same underlying magnitude of effect, have a low P‐value (P = 0.00001), indicating to reject the null hypothesis I2 statistic, which quantifies the proportion of the variation in point estimates due to among‐study differences, is large (97%) 3 High risk of performance bias: non‐blinded participants and personnel | |||||
| Study ID | Study design | Patient profile | Objective | No. of patients | Treatment | Results | Adverse effects |
| Non‐randomised, non‐controlled prospective study | HCV RNA (+) + cryoglobulinaemic syndrome with organ damage and B‐cell lymphoproliferative syndrome | To assess the hepatovirological response, the clinical and immunological efficacy and the safety of using sofosbuvir‐based direct‐acting antiviral therapy in patients with HCV‐associated mixed cryoglobulinaemia(according to the latest guidelines) | 44 | 1) Sofosbuvir+ribavirin (18) 2) Sofosbuvir+simeprevir (12) ± ribavirin (6 of 12 patients) 3) Sofosbuvir+daclatasvir (4) ± ribavirin (1 patient) 4) Sofosbuvir+ledipasvir (10) ± ribavirin (3 patients) | Hepatovirological response ‐ Undetectable HCV RNA negative rate 100% at week 4; 12SVR and 24SVR remained 100% negative ‐ Decrease of ALT from 77.7 ± 10.3 IU/L at baseline to 27.3 ± 10.3 IU/L at 24SVR ‐ Decrease of AST from 55.2 ± 60.4 IU/L at baseline to 22.6 ± 8.3 IU/L at 24SVR (P < 0.001) Clinical efficacy ‐ Decrease of BVAS from 5.41 ± 3.53 at baseline to 1.27 ± 1.68 at 24SVR (P < 0.001) Immunological efficacy ‐ Decrease of cryocrit level from 7.2 ± 15.4% at baseline to 1.8 ± 5.1% at 24SVR (P < 0.001) | Total: 26/44 (59%) Withdrawals: 1 patient withdrew ribavirin while continuing sofosbuvir+simeprevir Death: none Relapse: none Most frequent AE: Anaemia (13, all receiving ribavirin); fatigue (15); nausea (7) | |
| Case series | Five patients with HVC RNA + with detectable cryoglobulins in plasma and symptomatic mixed cryoglobulinaemia Patient 1: bilateral foot neuropathy and purpura Patient 2: painful left foot drop and purpura Patient 3: purpura and MPGN Patient 4: MPGN Patient 5: MPGN + low grade lymphoma | Review of one centre's experience in treating patients with mixed cryoglobulinaemia with new oral antiviral agents and to assess common factors associated with persistence of mixed cryoglobulinaemia despite SVR | 5 | Patient 1: PEG‐IFN+ribavirin+boceprevir Patient 2: Firstly with rituximab (5 weeks); later with: PEG‐IFN+ribavirin+telaprevir for 4 weeks; PEG‐IFN+ribavirin for 12 weeks; and PEG‐IFN+ribavirin+sofosbuvir for 15 weeks (telaprevir discontinued for persistent viral load > 1000 IU/mL) Patient 3: PEG‐IFN+ribavirin+telaprevir for 47 weeks Patient 4: PEG‐IFN+ribavirin for 24 weeks; afterwards adding sofosbuvir until completing 12 weeks of triple therapy (total 36 weeks) Patient 5: 2 cycles of rituximab: weekly infusions 375mg/m2 during 4 weeks in 2010 then two extra doses of rituximab in 2013 ‐PEG‐IFN+ribavirin+sofosbuvir for 8 weeks in 2014 | Patient 1: complete clearance of virus at week 8; complete clearance of cryoglobulins at week 28. Persistence of neuropathy Patient 2: SVR and no detectable cryoglobulins at month 6 after last triple therapy. Persistence of neuropathy. Patient 3: clearance of HCV at week 4 after PEG‐IFN+ribavirin+telaprevir, with persistent cryoglobulins. Active MPGN and vasculitis after ending of previous treatment (responding to steroid therapy). Patient 4: SVR with persistence of cryoglobulinaemia. Kidney function remained stable. | ||
| Retrospective case series | HCV RNA > 1000 IU/mL + circulating purpura + cutaneous ulcers, Raynaud’s phenomenon, arthralgia, sicca syndrome, gastrointestinal vasculitis, neurologic involvement or renal involvement | Comparison of 2 historical cohorts: one treated with PEG‐IFN and ribavirin and the other sofosbuvir+simeprevir (8/12) or sofosbuvir+ribavirin (4/12). Evaluation of 12SVR, relapses, clinical, immunological (cryoglobulins) and biochemical (AST, Hb) response and adverse effects; without statistical comparison between them | 22 | 1) PEG‐IFN+ribavirin 2) IFN‐free regimens 2a) Sofosbuvir 400 mg/24 h + simeprevir 150 mg/24h 2b) Sofosbuvir 400 mg/24 h + ribavirin (adjusted to kidney function) | PEG‐IFN+ribavirin ‐ SVR12: 1/10 IFN‐free regimens ‐ SVR12: 10/12 (95%) ‐ ALT decreased from 42 U/L at baseline to 20 U/L after treatment ‐ Cryoglobulin levels decreased from 1.5% (0.5% to 4%) at baseline to 0.5% (0% to 2%) after treatment ‐ Decrease of proteinuria in all cases of kidney involvement (table IV) | Total PEG‐IFN+ribavirin: 10/10 IFN‐free regimens: 8/12 Withdrawals PEG‐IFN+ribavirin: 5/10 IFN‐free regimens: 1/12 (anxiety and insomnia) Deaths: none Relapses IFN‐free regimens: 2 (genotype 1 sofosbuvir+simeprevir; genotype 4 sofosbuvir+ribavirin) | |
| Open‐label, non‐controlled, prospective cohort study | Chronic active HCV infection with signs of mixed cryoglobulinaemia. All 23 patients had positive cryoglobulins in plasma at baseline or earlier | To analyse the safety and efficacy of Peg‐IFN‐alpha/ribavirin/protease inhibitor combination in HCV‐mixed cryoglobulinaemia | 23 | Peg‐IFN‐alpha+ribavirin a) + telaprevir (375 mg, 3 times/d for 12 weeks) for 48 weeks (15 patients) b) + boceprevir (800 mg, 3 times/d for 44 weeks) for 48 weeks (8 patients) | Complete clinical responders (improvement in all baseline clinical manifestations): 13 patients (56.5%) at week 24 Virological response (i.e., HCV RNA negative) was of 69.6% at week 24 (P = 0.005). Cryoglobulin level: decreased from 0.44 to 0.06 g/L(P = 0.0006) C4 level: increased from 0.09 to 0.15 g/L (P = 0.045) No significant difference was found between the two treatment regiments | Total: 105 Withdrawals: 8 patients (34.7%) ( virological non‐response (5); virological relapse (2); depression (1)) Death: none Relapse: 1 Most frequent AE: fatigue (87%); neutropenia (78.3%); thrombocytopenia (65.2%); infection (47.8%); pruritus (39.1%); depression (21.7%); nausea (21.7%) | |
| Open‐label, non‐controlled, prospective cohort study | Active HCV infection and active mixed cryoglobulinaemia. Excluded non‐active mixed cryoglobulinaemia, HIV or HBV active infection and current decompensated cirrhosis | To evaluate safety and efficacy of an oral IFN‐free regimen, sofosbuvir+ribavirin, in HCV‐mixed cryoglobulinaemia | 24 | Sofosbuvir (400 mg/d) + ribavirin (200 to 1400 mg/d) for 24 weeks “Rituximab was used in four cases, in addition to prednisone and plasmapheresis in two patients” | Complete response (improvement of ALL the affected organs involved at baseline) at week 24: 21 (87.5%) HCV RNA clearance at week 24: 22/24 (91.7%) SVR12: 74% Cryocrit: decrease from 0.35 g/L at baseline to 0 at 12 weeks after end‐of‐treatment. C4: increase from 0.1 g/L at baseline to 0.22 g/L at 12 week after end‐of treatment “No difference of outcome was found in patients who received immunosuppressive treatment or not” | Total: 14/24 (54%) Withdrawals: 2 (8%) (hallucination and irritability (1); grade 4 anaemia (1)) Death: 2 (severe pneumonia in the context of B cell lymphoma; pulmonary embolism in the context of hepatocellular carcinoma) Relapses: none Most frequent AE: (fatigue (25%); anaemia (25%); insomnia (21%); infection (17%); alopecia (8%)) | |
| 12SVR ‐ 12 week SVR; 24SVR ‐ 24 week SVR; AE ‐ adverse event; ALT ‐ alanine aminotransferase; AST‐ aspartate aminotransferase; BVAS ‐ Birmingham Vasculitis Activity Score; Hb ‐ haemoglobin; HBV ‐ hepatitis B virus; HCV ‐ hepatitis C virus; HIV ‐ human immunodeficiency virus; IFN ‐ interferon; MPGN ‐ membranoproliferative glomerulonephritis; PEG ‐ pegylated; SVR ‐ sustained viral response | |||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Death Show forest plot | 3 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.1 One month | 2 | 61 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 1.2 Six months | 2 | 61 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 1.3 24 months | 3 | 118 | Risk Ratio (M‐H, Random, 95% CI) | 0.52 [0.10, 2.61] |
| 2 Clinical manifestations Show forest plot | 2 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 2.1 Active urinary sediment at 1 month | 1 | 16 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.51, 1.65] |
| 2.2 Need for dialysis at 24 months | 1 | 46 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2.3 Skin vasculitis (purpura, cutaneous ulcers or others) at 1 month | 1 | 57 | Risk Ratio (M‐H, Random, 95% CI) | 2.59 [0.55, 12.27] |
| 2.4 Skin vasculitis (purpura, cutaneous ulcers or others) at 18 and 24 months | 2 | 78 | Risk Ratio (M‐H, Random, 95% CI) | 0.57 [0.28, 1.16] |
| 2.5 Skin vasculitis (purpura, cutaneous ulcers or others) at 36 months | 1 | 37 | Risk Ratio (M‐H, Random, 95% CI) | 0.68 [0.43, 1.08] |
| 3 Laboratory findings Show forest plot | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.1 Serum creatinine at 18 months [µmol/L] | 1 | 37 | Mean Difference (IV, Random, 95% CI) | ‐8.80 [‐29.27, 11.67] |
| 3.2 Serum creatinine at 36 months [µmol/L] | 1 | 37 | Mean Difference (IV, Random, 95% CI) | 17.60 [‐4.23, 39.43] |
| 3.3 Proteinuria at 18 months [g/24 h] | 1 | 3 | Mean Difference (IV, Random, 95% CI) | ‐0.5 [‐1.42, 0.42] |
| 3.4 Proteinuria at 36 months [g/24 h] | 1 | 3 | Mean Difference (IV, Random, 95% CI) | 0.24 [‐0.84, 1.32] |
| 3.5 Cryocrit at 12 months [%] | 2 | 41 | Mean Difference (IV, Random, 95% CI) | ‐2.01 [‐10.29, 6.27] |
| 3.6 Serum HCV‐RNA at 12 months [IU/mL] | 1 | 17 | Mean Difference (IV, Random, 95% CI) | ‐435182.0 [‐1051224.79, 180860.79] |
| 4 Adverse effects of the medication Show forest plot | 3 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 4.1 Infusion reactions | 3 | 118 | Risk Ratio (M‐H, Random, 95% CI) | 4.33 [0.76, 24.75] |
| 4.2 Discontinuation of the treatment due to adverse drug reactions | 3 | 118 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.22, 4.36] |
| 4.3 Infection (pneumonia, urosepsis) at 6 months | 1 | 24 | Risk Ratio (M‐H, Random, 95% CI) | 0.50 [0.05, 4.81] |
| 4.4 Infection (pneumonia, urosepsis) at 24 months | 1 | 57 | Risk Ratio (M‐H, Random, 95% CI) | 0.35 [0.04, 3.12] |
| 4.5 Cardiovascular events (angina, myocardial infarction, heart failure) at 24 months | 1 | 57 | Risk Ratio (M‐H, Random, 95% CI) | 0.52 [0.10, 2.61] |
| 4.6 Gastrointestinal bleeding | 1 | 57 | Risk Ratio (M‐H, Random, 95% CI) | 3.10 [0.13, 73.12] |
| 4.7 Haemorrhagic alveolitis | 1 | 57 | Risk Ratio (M‐H, Random, 95% CI) | 0.34 [0.01, 8.12] |
| 4.8 Leukopenia at 6 months | 1 | 24 | Risk Ratio (M‐H, Random, 95% CI) | 0.50 [0.05, 4.81] |
| 4.9 Thrombocytopenia at 6 months | 1 | 24 | Risk Ratio (M‐H, Random, 95% CI) | 1.0 [0.07, 14.21] |
| 5 Antiviral therapy failure or not indicated Show forest plot | 3 | 118 | Risk Ratio (M‐H, Random, 95% CI) | 1.21 [0.77, 1.90] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Death Show forest plot | 4 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.1 12 months | 4 | 160 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 1.2 24 months | 2 | 91 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Clinical manifestations Show forest plot | 3 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 2.1 Skin vasculitis (purpura, cutaneous ulcers or others) at 12 months | 3 | 95 | Risk Ratio (M‐H, Random, 95% CI) | 0.60 [0.36, 1.00] |
| 3 Laboratory findings Show forest plot | 4 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.1 Serum creatinine at 18 months [µmol/L] | 2 | 49 | Mean Difference (IV, Random, 95% CI) | ‐30.32 [‐80.59, 19.95] |
| 3.2 Proteinuria at 18 months [g/24h] | 2 | 49 | Mean Difference (IV, Random, 95% CI) | ‐1.98 [‐2.89, ‐1.07] |
| 3.3 ALT or GPT at 6 months [UI/L] | 2 | 39 | Mean Difference (IV, Random, 95% CI) | ‐5.89 [‐55.77, 43.99] |
| 3.4 ALT or GPT at 18 months [UI/L] | 2 | 49 | Mean Difference (IV, Random, 95% CI) | ‐28.28 [‐48.03, ‐8.54] |
| 3.5 Rheumatoid factor activity at 6 months [UI/mL] | 1 | 13 | Mean Difference (IV, Random, 95% CI) | 97.0 [‐187.37, 381.37] |
| 3.6 C4 at 18 months [mg/dL] | 2 | 49 | Mean Difference (IV, Random, 95% CI) | ‐0.04 [‐2.74, 2.67] |
| 3.7 IgM at 18 months [mg/dL] | 2 | 52 | Mean Difference (IV, Random, 95% CI) | ‐595.75 [‐877.20, ‐314.30] |
| 3.8 Cryocrit at 6 months [%] | 2 | 39 | Mean Difference (IV, Random, 95% CI) | ‐1.38 [‐2.38, ‐0.38] |
| 4 Adverse effects of the medication Show forest plot | 5 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 4.1 Infusion reactions | 1 | 65 | Risk Ratio (M‐H, Random, 95% CI) | 27.82 [1.72, 449.18] |
| 4.2 Discontinuations of the treatment due to adverse drug reactions | 4 | 148 | Risk Ratio (M‐H, Random, 95% CI) | 2.32 [0.91, 5.90] |
| 5 Antiviral therapy failure or not indicated Show forest plot | 2 | 78 | Risk Ratio (M‐H, Random, 95% CI) | 0.59 [0.21, 1.64] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Death at 24 months Show forest plot | 1 | 36 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Death at 24 months Show forest plot | 1 | 17 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Clinical manifestations Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2.1 Skin vasculitis (purpura, cutaneous ulcers or others) at 6 months | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Peripheral neuropathies at 6 months | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 Peripheral joint arthralgia at 6 months | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Laboratory findings Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 3.1 Cryocrit [%] | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Adverse effects of the medication Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 4.1 Infusion reactions | 1 | 17 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |

