| 1 Perinatal mortality Show forest plot | 1 | 459 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
|
| 2 Major neonatal morbidity Show forest plot | 1 | 459 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.15 [0.01, 2.81] |
|
| 3 Neurodevelopmental disability/impairment Show forest plot | 1 | 459 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.04 [0.62, 6.69] |
|
| 4 Maternal mortality Show forest plot | 1 | 459 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.07 [0.13, 74.87] |
|
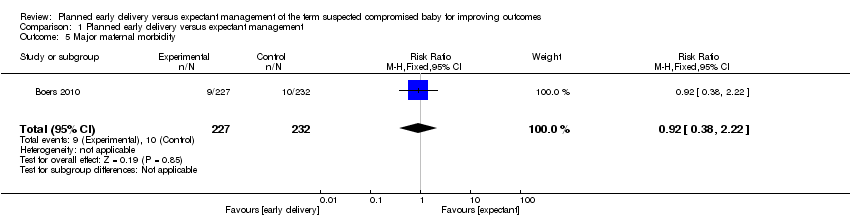
| 5 Major maternal morbidity Show forest plot | 1 | 459 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.92 [0.38, 2.22] |
|
| 6 Neonatal seizures Show forest plot | 1 | 336 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
|
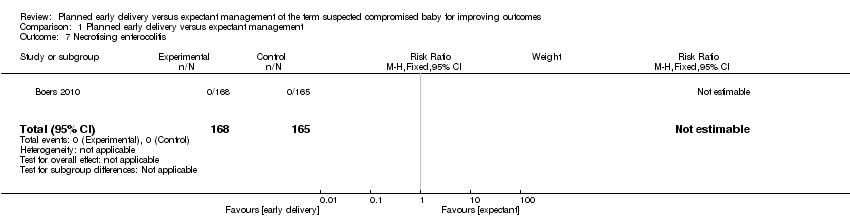
| 7 Necrotising enterocolitis Show forest plot | 1 | 333 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
|
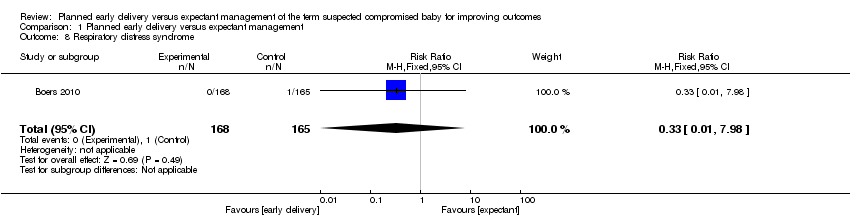
| 8 Respiratory distress syndrome Show forest plot | 1 | 333 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.98] |
|
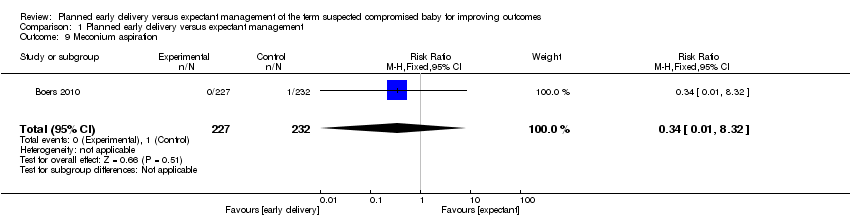
| 9 Meconium aspiration Show forest plot | 1 | 459 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.34 [0.01, 8.32] |
|
| 10 Gestational age at birth (days) Show forest plot | 1 | 459 | Mean Difference (IV, Fixed, 95% CI) | ‐9.5 [‐10.82, ‐8.18] |
|
| 11 Gestational age ≥ 40 weeks (not pre‐specified) Show forest plot | 1 | 33 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.10 [0.01, 0.67] |
|
| 12 Apgar score < 7 at 5 minutes Show forest plot | 3 | 546 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.56 [0.50, 13.04] |
|
| 13 Resuscitation required Show forest plot | 1 | 459 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.11 [0.01, 2.10] |
|
| 14 Requirement for mechanical ventilation Show forest plot | 1 | 337 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.20 [0.01, 4.11] |
|
| 15 Birthweight < 10 centile Show forest plot | 2 | 491 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.88, 1.10] |
|
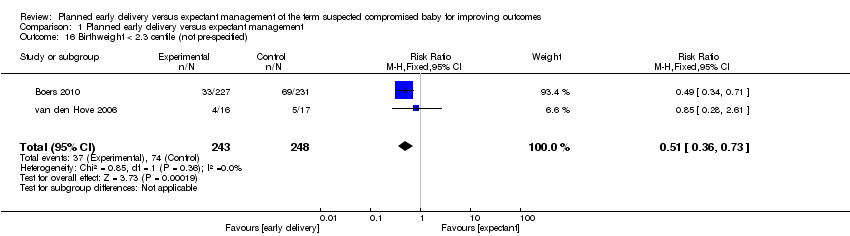
| 16 Birthweight < 2.3 centile (not pre‐specified) Show forest plot | 2 | 491 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.51 [0.36, 0.73] |
|
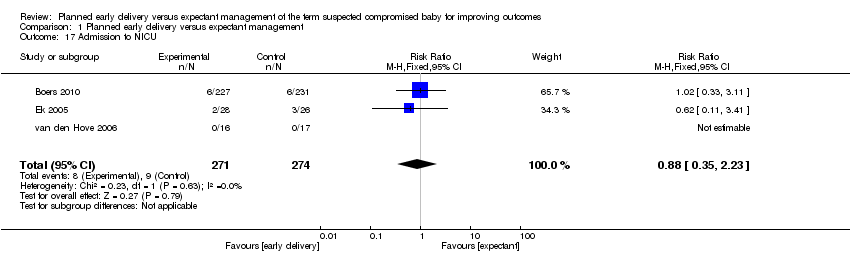
| 17 Admission to NICU Show forest plot | 3 | 545 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.35, 2.23] |
|
| 18 Admission to intermediate care nursery (not pre‐specified) Show forest plot | 2 | 491 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.28 [1.02, 1.61] |
|
| 19 Length of stay in NICU/SCN (days) Show forest plot | 1 | 459 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [‐1.28, 1.28] |
|
| 20 Interval (days) between randomisation and delivery Show forest plot | 1 | 459 | Mean Difference (IV, Fixed, 95% CI) | ‐8.68 [‐10.04, ‐7.32] |
|
| 21 Neonatal sepsis Show forest plot | 2 | 366 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.18 [0.14, 72.75] |
|
| 22 Caesarean section Show forest plot | 3 | 546 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.65, 1.59] |
|
| 23 Placental abruption Show forest plot | 1 | 459 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.07 [0.13, 74.87] |
|
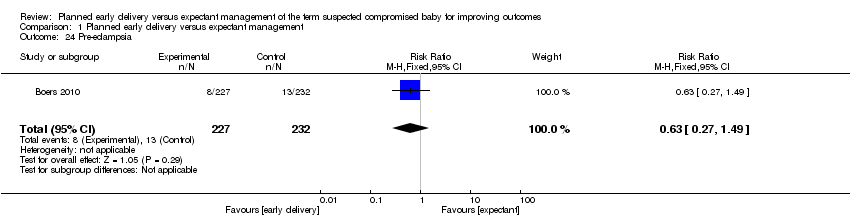
| 24 Pre‐eclampsia Show forest plot | 1 | 459 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.63 [0.27, 1.49] |
|
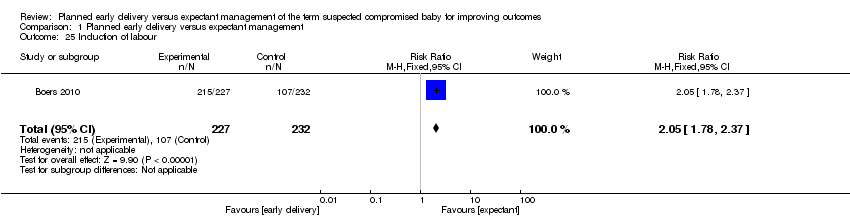
| 25 Induction of labour Show forest plot | 1 | 459 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.05 [1.78, 2.37] |
|
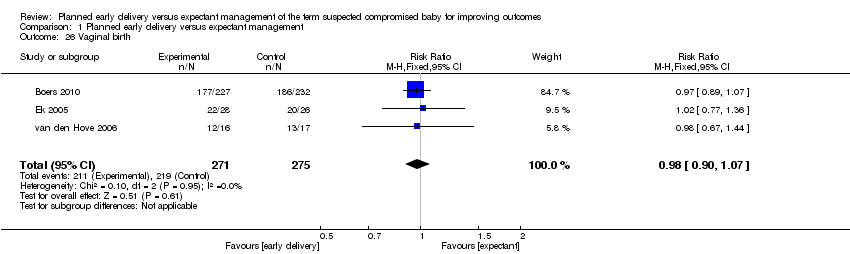
| 26 Vaginal birth Show forest plot | 3 | 546 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.90, 1.07] |
|
| 27 Assisted vaginal birth Show forest plot | 3 | 546 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.19 [0.69, 2.04] |
|
| 28 Breastfeeding Show forest plot | 1 | 218 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.09 [0.85, 1.40] |
|
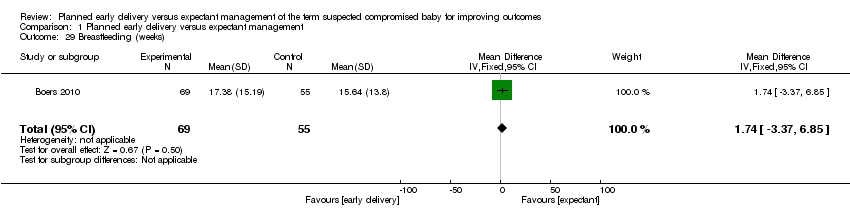
| 29 Breastfeeding (weeks) Show forest plot | 1 | 124 | Mean Difference (IV, Fixed, 95% CI) | 1.74 [‐3.37, 6.85] |
|
| 30 Maternal hospital stay (days) (not pre‐specified) Show forest plot | 1 | 33 | Mean Difference (IV, Fixed, 95% CI) | 1.0 [0.68, 1.32] |
|