Corticosteroides para la meningitis bacteriana aguda
Resumen
Antecedentes
En estudios experimentales, el resultado de la meningitis bacteriana se ha relacionado con la gravedad de la inflamación en el espacio subaracnoideo. Los corticosteroides reducen esta respuesta inflamatoria.
Objetivos
Examinar el efecto del tratamiento adyuvante con corticosteroides versus placebo sobre la mortalidad, la pérdida de audición y las secuelas neurológicas en pacientes de todas las edades con meningitis bacteriana aguda.
Métodos de búsqueda
Se hicieron búsquedas en CENTRAL (2015, número 1), MEDLINE (1966 hasta enero, semana 4, 2015), Embase (1974 hasta febrero de 2015), Web of Science (2010 hasta febrero de 2015), CINAHL (2010 hasta febrero de 2015) y LILACS (2010 hasta febrero de 2015).
Criterios de selección
Ensayos controlados aleatorizados (ECA) de corticosteroides para la meningitis bacteriana aguda.
Obtención y análisis de los datos
Los ECA se han clasificado por su calidad metodológica. Se obtuvieron los resultados y los efectos adversos. Se realizaron análisis de subgrupos de niños y adultos, organismos causales, países de ingresos bajos versus países de ingresos altos, tiempo de administración de los esteroides y calidad del estudio.
Resultados principales
Se incluyeron 25 estudios con 4121 participantes (2511 niños y 1517 adultos; 93 de población mixta). Cuatro estudios fueron de alta calidad sin riesgo de sesgo, 14 de calidad media y siete de calidad baja, lo que indica un riesgo moderado de sesgo en el análisis total. Se realizaron nueve estudios en países de ingresos bajos y 16 en países de ingresos altos.
No hubo evidencia suficiente de que los corticosteroides causaran una reducción de la mortalidad en general (17,8% versus 19,9%; riesgo relativo [RR] 0,90; intervalo de confianza [IC] del 95%: 0,80 a 1,01; p = 0,07), ni en los pacientes adultos (RR 0,74; IC del 95%: 0,53 a 1,05; p = 0,09). Sin embargo, causaron tasas más bajas de pérdida grave de audición (RR 0,67; IC del 95%: 0,51 a 0,88), de cualquier pérdida de audición (RR 0,74; IC del 95%: 0,63 a 0,87) y de secuelas neurológicas (RR 0,83; IC del 95%: 0,69 a 1,00).
Los análisis de subgrupos de los organismos causantes mostraron que los corticosteroides redujeron la mortalidad en la meningitis por Streptococcus pneumoniae (S pneumoniae) (RR 0,84; IC del 95%: 0,72 a 0,98), pero no en la meningitis por Haemophilus influenzae (H influenzae) o Neisseria meningitidis (N meningitidis). Los corticosteroides redujeron la pérdida grave de audición en los niños con meningitis por H influenzae (RR 0,34; IC del 95%: 0,20 a 0,59), pero no ocurrió así en los niños con meningitis debido a especies no Haemophilus .
En los países de ingresos altos, los corticosteroides redujeron la pérdida grave de audición (RR 0,51; IC del 95%: 0,35 a 0,73), cualquier pérdida de audición (RR 0,58; IC del 95%: 0,45 a 0,73) y las secuelas neurológicas a corto plazo (RR 0,64; IC del 95%: 0,48 a 0,85). El tratamiento con corticosteroides no tuvo efectos beneficiosos en los países de ingresos bajos.
El análisis de subgrupos de la calidad del estudio no mostró efectos de los corticosteroides en la pérdida grave de audición en los estudios de calidad alta.
El tratamiento con corticosteroides se asoció con un aumento de la fiebre recurrente (RR 1,27; IC del 95%: 1,09 a 1,47), pero no con otros eventos adversos.
Conclusiones de los autores
Los corticosteroides redujeron significativamente la pérdida de audición y las secuelas neurológicas, pero no redujeron la mortalidad general. Los datos apoyan el uso de corticosteroides en pacientes con meningitis bacteriana en países de ingresos altos. No se encontraron efectos beneficiosos en los países de ingresos bajos.
PICOs
Resumen en términos sencillos
Corticosteroides para la meningitis bacteriana
Pregunta de la revisión
Se revisó la evidencia sobre el efecto de los corticosteroides en la mortalidad, la pérdida de audición y las secuelas neurológicas (como la pérdida de audición, los déficits neurológicos) en pacientes adultos y niños con meningitis bacteriana aguda.
Antecedentes
La meningitis bacteriana aguda es una infección de las meninges (el sistema de membranas que envuelve el cerebro y la médula espinal), que suele causar pérdida de audición. La meningitis bacteriana es mortal en el 5% al 40% de los niños y en el 20% al 50% de los adultos a pesar del tratamiento con antibióticos adecuados. Es causada por una bacteria que se suele propagar por una infección de oído o respiratoria y se trata con antibióticos.
Los corticosteroides son fármacos que pueden reducir la inflamación causada por la infección. Se ha demostrado que esta inflamación agrava el daño al sistema nervioso en estudios experimentales de meningitis en animales. Los estudios de investigación sobre el uso de corticosteroides, además de los antibióticos, han tenido resultados contradictorios.
Se deseaba determinar si el uso de corticosteroides era mejor o peor que placebo.
Características de los estudios
La evidencia está actualizada hasta febrero de 2015. Se identificaron 25 ensayos, que incluyeron 4121 participantes con meningitis bacteriana aguda, de los cuales siete se realizaron en adultos (mayores de 16 años), dos incluyeron niños y adultos y el otro se realizó en niños. En 22 estudios el corticoesteroide utilizado fue la dexametasona, en otros tres se utilizó hidrocortisona o prednisona. Se realizaron nueve estudios en países de ingresos bajos y 16 en países de ingresos altos.
Resultados clave
Esta revisión encontró que el corticoesteroide dexametasona no redujo significativamente la tasa de mortalidad (17,8% versus 19,9%). Los pacientes tratados con corticosteroides tuvieron tasas significativamente menores de pérdida grave de audición (6,0% versus 9,3%), cualquier pérdida de audición (13,8% versus 19,0%) y secuelas neurológicas (17,9% versus 21,6%).
Un análisis de las diferentes bacterias que causan la meningitis mostró que los pacientes con meningitis por Streptococcus pneumoniae (S pneumoniae) tratados con corticosteroides tuvieron una tasa de mortalidad más baja (29,9% versus 36,0%), mientras que no se observaron efectos sobre la mortalidad en los pacientes con meningitis por Haemophilus influenzae (H influenzae) y Neisseria meningitidis (N meningitidis).
En los países de ingresos altos, los corticosteroides redujeron la pérdida grave de audición, cualquier pérdida de audición y las secuelas neurológicas a corto plazo. El tratamiento con corticosteroides no tuvo efectos beneficiosos en los países de ingresos bajos.
Los corticosteroides disminuyeron la tasa de pérdida de audición en los niños con meningitis debido a H influenzae (4% versus 12%), pero no ocurrió igual en los niños con meningitis debido a otras bacterias.
La dexametasona aumentó la tasa de fiebre recurrente (28% versus 22%), pero no se asoció a otros eventos adversos.
Calidad de la evidencia
De 25 estudios, cuatro fueron de calidad alta, 14 de calidad media y siete de calidad baja, lo que da lugar a una calidad general moderada de la evidencia.
Authors' conclusions
Summary of findings
| Comparison of corticosteroids against placebo in patients with acute bacterial meningitis | ||||||
| Patient or population: acute bacterial meningitis | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Risk with placebo | Risk with corticosteroids | |||||
| Mortality | Study population | RR 0.90 | 4121 | ⊕⊕⊖⊖ MODERATE 1 | — | |
| 199 per 1000 | 179 per 1000 | |||||
| Moderate | ||||||
| 188 per 1000 | 169 per 1000 | |||||
| Severe hearing loss | Study population | RR 0.67 | 2437 | ⊕⊕⊕⊖ HIGH | — | |
| 93 per 1000 | 62 per 1000 | |||||
| Moderate | ||||||
| 40 per 1000 | 27 per 1000 | |||||
| Any hearing loss | Study population | RR 0.74 | 2785 | ⊕⊕⊕⊖ HIGH | — | |
| 190 per 1000 | 141 per 1000 | |||||
| Moderate | ||||||
| 233 per 1000 | 173 per 1000 | |||||
| Short‐term neurological sequelae | Study population | RR 0.83 | 1756 | ⊕⊕⊕⊖ HIGH | — | |
| 216 per 1000 | 179 per 1000 | |||||
| Moderate | ||||||
| 222 per 1000 | 184 per 1000 | |||||
| Adverse events ‐ recurrent fever | Study population | RR 1.27 | 1723 | ⊕⊕⊖⊖ | — | |
| 221 per 1000 | 281 per 1000 | |||||
| Moderate | ||||||
| 281 per 1000 | 357 per 1000 | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Variable mortality between studies, consistent with differences across the world in meningitis prognosis. 2Different definitions used for recurrent fever makes this imprecise. | ||||||
Background
Description of the condition
Bacterial meningitis is a severe infection of the meninges (the membrane lining of the brain and spinal cord) that is associated with high mortality and morbidity rates despite optimal antibiotic therapy and advances in critical care (Baraff 1993; Bohr 1983; Brouwer 2010c; van de Beek 2002; van de Beek 2004b; van de Beek 2006b). Late sequelae such as cranial nerve impairment, especially hearing loss, occur in 5% to 40% of patients (Baraff 1993; Bohr 1983; Brouwer 2010b; Heckenberg 2012a; van de Beek 2002; van de Beek 2004b; van de Beek 2006b).
Description of the intervention
Intravenously or orally administered corticosteroids, such as prednisolone, hydrocortisone and dexamethasone, are given before, with or after antibiotic treatment for suspected or proven bacterial meningitis.
How the intervention might work
In experimental animal studies, the outcome of meningitis worsens with increasing severity of the inflammatory process in the subarachnoidal space (Scheld 1980; Tauber 1985). Treatment with corticosteroids was shown to result in a reduction of the inflammatory response in the cerebrospinal fluid (CSF), reversal of brain oedema and improved outcome (Scheld 1980; Tauber 1985). These pathophysiological insights prompted investigators to evaluate corticosteroids as an adjuvant therapy in acute bacterial meningitis.
Why it is important to do this review
In the 1960s two randomised controlled trials (RCTs) evaluated the effect of corticosteroids in patients with bacterial meningitis (Bennett 1963; DeLemos 1969). New randomised clinical trials were performed in the late 1980s and 1990s (Lebel 1988a; Lebel 1988b; Lebel 1989; Odio 1991), with conflicting results. Two meta‐analyses of RCTs were published showing a reduction in bilateral hearing loss in dexamethasone‐treated children with Haemophilus influenzae (H influenzae) meningitis (Geiman 1992; Havens 1989).
In the early 1990s the epidemiology of bacterial meningitis changed due to the introduction of the H influenzae type B conjugate vaccine that resulted in near elimination of this bacterium as cause of meningitis in high‐income countries (Peltola 2000). New trials were performed in children with bacterial meningitis, most commonly caused by Streptococcus pneumoniae (S pneumoniae). In 1997, a new meta‐analysis was published showing adjunctive corticosteroid therapy to prevent hearing loss in patients with H influenzae meningitis (McIntyre 1997). This meta‐analysis also showed a beneficial trend of dexamethasone on neurological sequelae and hearing loss in patients with meningitis due to S pneumoniae.
In the 2000s, five large randomised clinical trials have been performed. Two trials in children were performed in Malawi and South America and three trials in adults were performed in Europe, Vietnam and Malawi (de Gans 2002; Molyneux 2002; Nguyen 2007; Peltola 2007; Scarborough 2007). The European trial showed a beneficial effect in all patients, with the most apparent effect on mortality and unfavourable outcomes in pneumococcal meningitis (de Gans 2002). The Vietnamese trial showed a beneficial effect only in patients with proven bacterial meningitis (Nguyen 2007). The other trials did not show a beneficial effect. In 2010 an individual patient data meta‐analysis was performed with patients from these five trials to determine in which subgroups of patients adjunctive dexamethasone was effective (van de Beek 2010). In this meta‐analysis no benefit of adjunctive dexamethasone was found in any of the pre‐specified subgroups. However, a post hoc analysis did show a reduction in any hearing loss in surviving patients treated with dexamethasone.
The results of many trials have been inconclusive and most studies have been relatively small. Trials have varied greatly in study population, study design, timing and dosage of corticosteroids. Furthermore, mortality was substantially higher in studies in low‐income countries, primarily related to access to care and co‐morbidities. This Cochrane systematic review and meta‐analysis facilitates an interpretation of these varying results and might identify subgroups that benefit from adjunctive corticosteroid therapy. See Appendix 1 for a glossary of terms.
Objectives
To examine the effect of adjuvant corticosteroid therapy versus placebo on mortality, hearing loss and neurological sequelae in people of all ages with acute bacterial meningitis.
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials (RCTs).
Types of participants
Participants of any age and in any clinical condition.
Types of interventions
Participants with community‐acquired bacterial meningitis treated with antibacterial agents and randomised to adjuvant corticosteroid therapy of any type.
Types of outcome measures
At least case‐fatality rate or hearing loss had to be recorded for studies to be included.
Primary outcomes
-
Mortality
-
Hearing loss
-
Neurological sequelae
Hearing loss was defined as severe when there was bilateral hearing loss greater than 60 dB or requiring bilateral hearing aids. We analysed any hearing loss and severe hearing loss separately. Neurological sequelae were defined as focal neurological deficits other than hearing loss, epilepsy (not present before meningitis onset), severe ataxia and severe memory or concentration disturbance. We did not count children with isolated speech or language disturbances as having non‐hearing deficits if these problems were associated with severe hearing loss. We analysed both short‐ and long‐term neurological sequelae, other than hearing loss. Short‐term neurological sequelae were defined as sequelae assessed between discharge and six weeks after hospital discharge. Long‐term neurological sequelae were defined as sequelae assessed between six weeks and 12 months after discharge. Whenever possible, we extracted data for both these outcomes.
Secondary outcomes
-
Adverse events
Adverse events were defined as clinically evident gastrointestinal tract bleeding, reactive arthritis, pericarditis, herpes zoster or herpes simplex virus infection, fungal infection, recurrent fever (defined as a temperature of 38 °C or above occurring after at least one afebrile day during the course of hospitalisation) and persistent fever (defined as fever continuing longer than five consecutive days after initiation of appropriate antibiotic therapy).
Search methods for identification of studies
Electronic searches
For this 2015 update we searched the Cochrane Central Register of Controlled Trials (CENTRAL 2015, Issue 1), which includes the Cochrane Acute Respiratory Infections Group Specialised Register, MEDLINE (January 2013 to January Week 4, 2015), Embase (January 2013 to February 2015), Web of Science (January 2013 to February 2015), CINAHL (January 2013 to February 2015) and LILACS (January 2013 to February 2015). Details of earlier searches are in Appendix 2.
We used the search strategy described in Appendix 3 to search CENTRAL and MEDLINE. We combined the MEDLINE search with the Cochrane Highly Sensitive Search Strategy for identifying randomised trials in MEDLINE: sensitivity‐ and precision‐maximising version (2008 revision); Ovid format (Lefebvre 2011). We adapted the search strategy to search Embase (Appendix 4), Web of Science (Appendix 5), CINAHL (Appendix 6) and LILACS (Appendix 7). We did not apply any language or publication restrictions.
Searching other resources
Besides the electronic search we identified relevant trials by searching references listed in published studies, handsearching congress abstracts, personal communication with researchers and experts in the field and from literature lists of pharmaceutical companies. We also searched the trials registries World Health Organization (WHO) International Clinical Trials Registry Platform (ICTRP) and ClinicalTrials.gov for completed and ongoing trials (June 2015).
Data collection and analysis
Selection of studies
Two review authors (MD, DvdB) independently screened the search results and retrieved the full articles of all potentially relevant trials. We scrutinised each trial report to ensure that multiple publications from the same trial were included only once. We resolved disagreements through discussion and listed the excluded studies and the reasons for their exclusion.
Data extraction and management
Two review authors (MB, DvdB) independently extracted data according to a pre‐specified protocol. Data extracted included study design, inclusion criteria, patients' characteristics, country in which the study was performed, intervention characteristics and outcome measures. Scored intervention characteristics were corticosteroid type, daily corticosteroid dose, duration of steroid therapy and timing of corticosteroid therapy initiation (before/with the first dose of antibiotic therapy, or after first dose of antibiotic therapy). We resolved disagreements through discussion and contacted the corresponding publication author in the case of unclear or missing data.
For dichotomous outcomes, we recorded the number of participants experiencing the event and the number randomised in each treatment group. To allow an available‐case analysis, we recorded the numbers of participants analysed in each treatment group and used them in the analyses. However, we also recorded the number of participants randomised into the treatment arms and used the discrepancy between the figures to calculate the loss to follow‐up. Also, these figures allowed a worst‐case scenario analysis to be carried out to investigate the effect of missing data.
Assessment of risk of bias in included studies
For each study we completed a 'Risk of bias' table, scoring for adequacy of sequence generation, allocation concealment, blinding, if incomplete data were addressed, selective reporting and other sources of bias (Higgins 2011). We excluded studies without adequate sequence generation from the meta‐analyses.
Measures of treatment effect
All outcome measures were dichotomous. We used risk ratios (RR) with 95% confidence intervals (CI) as measures of treatment effect.
Unit of analysis issues
For studies using multiple treatment groups, we included only groups receiving corticosteroids or placebo in the meta‐analysis.
Dealing with missing data
We contacted the corresponding publication author in the case of unclear or missing data. If details were not provided, results used in the analysis were as provided in the publication.
We scored missing data in the outcome measures severe hearing loss and neurological sequelae for each study if reported. We assessed whether missing data were equally distributed between treatment and control groups using the Chi2 test. These tests were two‐tailed and we considered a P value of < 0.05 significant.
Assessment of heterogeneity
We assessed heterogeneity in all analysis with the I2 statistic with a value of >= 50% taken to indicate statistical heterogeneity.
Assessment of reporting biases
We conducted visual inspection of the funnel plot of the studies for any obvious asymmetry that could indicate publication bias.
Data synthesis
We analysed the data using Review Manager 5.3 (RevMan 2014). We performed meta‐analyses using the Mantel‐Haenszel method with a fixed‐effect model when heterogeneity was absent. When significant heterogeneity was established we used a random‐effects model.
Subgroup analysis and investigation of heterogeneity
We performed subgroup analyses for children and adults, causative organisms, low‐income versus high‐income countries, time of administration of steroids and quality of studies. Two age groups were defined: patients younger than 16 years and those aged 16 years and older. Three categories of causative organisms were defined: H influenzae,Neisseria meningitidis (N meningitidis) andS pneumoniae. We analysed studies in two subsets divided into low‐income and high‐income countries. Low‐income countries had a United Nations Human Development Index of less than 0.7 and high‐income countries had an index of 0.7 or higher (UNHDI 2009). Studies were divided into three categories of methodological quality: high, medium and low according to the score in the 'Risk of bias' table. If all questions in the 'Risk of bias' table were answered positively we categorised the study as high quality, three through five as medium quality and less than three questions answered positively as low quality.
In the subgroup analysis we used the inverse variance method with a fixed‐effect model to detect significant heterogeneity between subgroups, using a P value of < 0.05 and I2 statistic => 50%.
Sensitivity analysis
For trials with missing data, we conducted two analyses: an available‐case analysis and a worst‐case scenario analysis. We considered all participants who had dropped out of the corticosteroid group to have an unfavourable outcome whereas we considered those who had dropped out of the control group to have a favourable outcome. We conducted a sensitivity analysis by imputing the missing data in this way to determine whether the overall results were sensitive to this assumption.
We performed additional random‐effects model analyses for all studies without significant heterogeneity determined by the I2 statistic (I2 statistic < 50%) to see if results were valid with this method as well.
Finally, we performed the analyses for the primary outcome measures without studies with unclear or unknown sequence generation.
Results
Description of studies
Results of the search
Since the first publication of this review we have retrieved a total of 4421 records. After removing duplicates we identified 3559 records in the electronic databases.
In the previous publications of this review, Brouwer 2013, we identified 40 potentially eligible trials, of which two were described in one paper (Lebel 1988a; Lebel 1988b). Two papers presented data from one study (Sankar 2007; Singhi 2008). In this 2015 search we did not identify any new trials for inclusion.
Included studies
A total of 25 studies were eligible for inclusion in the meta‐analysis (Characteristics of included studies). These studies included 4121 patients (2064 dexamethasone, 2057 placebo). Participants over 16 years were included in seven studies (1517 patients: 756 dexamethasone, 761 placebo) (Bhaumik 1998; de Gans 2002; Girgis 1989; Nguyen 2007; Scarborough 2007; Thomas 1999). In two studies, participants older than 12 years were considered adults (Bhaumik 1998; Girgis 1989). The study intervention consisted of dexamethasone in 22 out of 25 studies; dosages ranged from 0.4 to 1.5 mg/kg/d and duration ranged from two to four days. In the other studies hydrocortisone, prednisolone or a combination of both were given and duration ranged from three to 14 days (Bademosi 1979; Bennett 1963; DeLemos 1969).
Study medication was administered before or with the first dose of antibiotics in 13 studies, and after the first dose in eight studies. In four studies the time of administration was not stated.
A sample size calculation was given in eight studies (de Gans 2002; Mathur 2013; Molyneux 2002; Nguyen 2007; Peltola 2007; Qazi 1996; Scarborough 2007; Thomas 1999).
Mortality rates ranged from 0% to 54%. In one study participants who died during the first 18 hours of admission were excluded (Belsey 1969); nevertheless, we included these participants in the meta‐analysis. Hearing was assessed by audiometry in seven studies in children and four studies in adults; other studies used brainstem evoked potentials (10) or age‐specific behavioural measures (eight). Four studies assessed both short‐term and long‐term neurological sequelae (Lebel 1988a; Lebel 1988b; Lebel 1989; Wald 1995). Definitions of adverse events were heterogeneous and we recalculated the number of events for each study.
Ethical review by hospital committees was described in 18 (72%) studies. Eighteen (72%) studies described informed consent procedures. There were no disagreements on inclusion or exclusion of studies between the review authors extracting study data. No study authors needed to be contacted to provide additional information for this updated version of the review.
Ten studies were funded in part by pharmaceutical companies, which were often only providing study medication. Five studies were funded by charities, four by government funding organisations, and funding was not reported for nine studies.
Excluded studies
We excluded 16 trials (Characteristics of excluded studies). Three studies did not randomise between treatment and control groups (Marguet 1993; Ozen 2006; Tolaj 2010). Nine trials did not adequately generate a randomisation sequence and in most of these alternate allocation schemes were used (Ayaz 2008; Baldy 1986; Daoud 1999; Gijwani 2002; Gupta 1996; Jensen 1969; Lepper 1959; Passos 1979; Shembesh 1997). One study compared two dexamethasone regimens (Syrogiannopoulos 1994), one was a duplicate study (Singhi 2008), and one study provided insufficient data (communications during scientific meetings only) (Farina 1995).
Risk of bias in included studies
Summary of general risk of bias
Four of 25 studies were free of bias, whereas the other 21 had one or more biases. Attrition, reporting and potential selection bias were most common, occurring in eight, 18 and 12 studies (Figure 1).
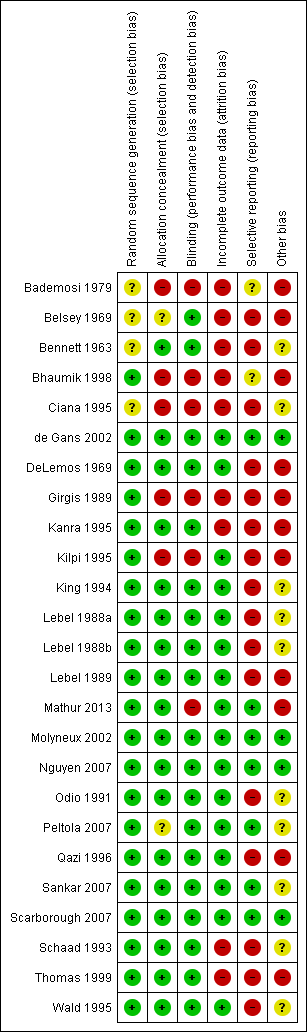
'Risk of bias' summary: review authors' judgements about each methodological quality item for each included study.
Allocation
The sequence generation for participant allocation was adequate in 20 studies. In five studies the method of sequence generation was unclear or not specified (Bademosi 1979; Belsey 1969; Bennett 1963; Ciana 1995; King 1994) (Figure 2; Figure 1). In five studies the treatment allocation was not concealed (Bademosi 1979; Bhaumik 1998; Ciana 1995; Girgis 1989; Kilpi 1995), and in one study treatment allocation concealment was unclear as participants were paired for placebo or dexamethasone (Belsey 1969). A multicentre study performed in several South American countries compared two treatments in a 2 x 2 design, dexamethasone and glycerol with placebo, in four randomisation arms (glycerol‐dexamethasone, glycerol‐placebo, dexamethasone‐placebo, placebo‐placebo). However, some centres did not include participants in the double placebo group, thereby disturbing the allocation concealment (Peltola 2007; van de Beek 2010). Data were extracted as derived from one study, comparing the dexamethasone‐placebo versus placebo‐placebo groups.

'Risk of bias' graph: review authors' judgements about each methodological quality item presented as percentages across all included studies.
Blinding
Nineteen studies had a double‐blind design and broke the treatment code after follow‐up for the last participant was complete. Six studies did not use blinding (Bademosi 1979; Bhaumik 1998; Ciana 1995; Girgis 1989; Kilpi 1995; Mathur 2013).
Incomplete outcome data
Missing data were addressed in 16 studies and were not addressed in eight (Bademosi 1979; Belsey 1969; Bennett 1963; Bhaumik 1998; Girgis 1989; Kanra 1995; Schaad 1993; Thomas 1999). One study reported having complete data for all included participants (Mathur 2013). Out of 2694 survivors who were included in studies that analysed severe hearing loss, 216 (8.0%) were not tested or had inconclusive test results. Data on any hearing loss were missing in 223 of 3029 (7.4%) surviving participants included in studies that assessed hearing loss. Short‐term neurological sequelae were assessed in 1695 of 1850 survivors included in studies that scored short‐term sequelae; data on 155 (8.3%) were missing. Data on long‐term sequelae were missing in 157 of 1705 participants (9.2%). The number of missing data was equally distributed between treatment and control group (P value for differences in missing data > 0.10 for all analyses with missing data).
Selective reporting
An intention‐to‐treat (ITT) analysis was performed in six studies (de Gans 2002; Molyneux 2002; Nguyen 2007; Peltola 2007; Sankar 2007; Scarborough 2007), comprising 2147 out of 4041 participants (53%). One study that reported no loss to follow‐up or discontinuing treatment was analysed as ITT (Mathur 2013). In the other 18 studies only per‐protocol data were available to be ascertained. The final analysis for mortality is equally based upon per‐protocol figures (46% of included participants) and ITT figures (56%).
A study protocol with pre‐specification of the analyses had not been published prior to publication of the complete study results for any of the included studies. None of the trials registered a study protocol in a trial registry.
Funnel plots of outcomes (mortality, any hearing loss, short‐term neurological sequelae and long‐term neurological sequelae and adverse events) did not show obvious asymmetry, except for severe hearing loss (Analysis 1.1; Analysis 1.2; Analysis 1.3; Analysis 1.4; Analysis 1.5; Analysis 1.6).
Other potential sources of bias
In 12 studies differences in baseline and clinical characteristics between treatment and control groups influenced comparability of groups (Bademosi 1979; Belsey 1969; Bhaumik 1998; DeLemos 1969; Kanra 1995; Kilpi 1995; Lebel 1989; Mathur 2013; Peltola 2007; Sankar 2007; Thomas 1999), indicating either insufficient sample size to equal out the random differences between randomisation arms or a selection bias. We found other indications of a selection bias in studies with high numbers of comatose participants or low numbers of culture‐positive participants (Girgis 1989; Mathur 2013; Qazi 1996; Sankar 2007). Nine studies did not present sufficient participant characteristics to determine whether the participants in each randomisation arm were comparable.
Effects of interventions
See: Summary of findings for the main comparison Summary of findings table
Primary outcomes
1. Mortality
A lower overall number of deaths in the corticosteroid‐treated group was observed compared to the placebo group (367 of 2064 (17.8%) versus 408 out of 2057 (19.8%), risk ratio (RR) 0.90, 95% confidence interval (CI) 0.80 to 1.01, P value = 0.07), although the difference did not reach statistical significance (Bademosi 1979; Belsey 1969; Bennett 1963; Bhaumik 1998; Ciana 1995; de Gans 2002; DeLemos 1969; Girgis 1989; Kanra 1995; Kilpi 1995; King 1994; Lebel 1988a; Lebel 1988b; Lebel 1989; Mathur 2013; Molyneux 2002; Nguyen 2007; Odio 1991; Peltola 2007; Qazi 1996; Sankar 2007; Scarborough 2007; Schaad 1993; Thomas 1999; Wald 1995) (Analysis 1.1; Figure 3).
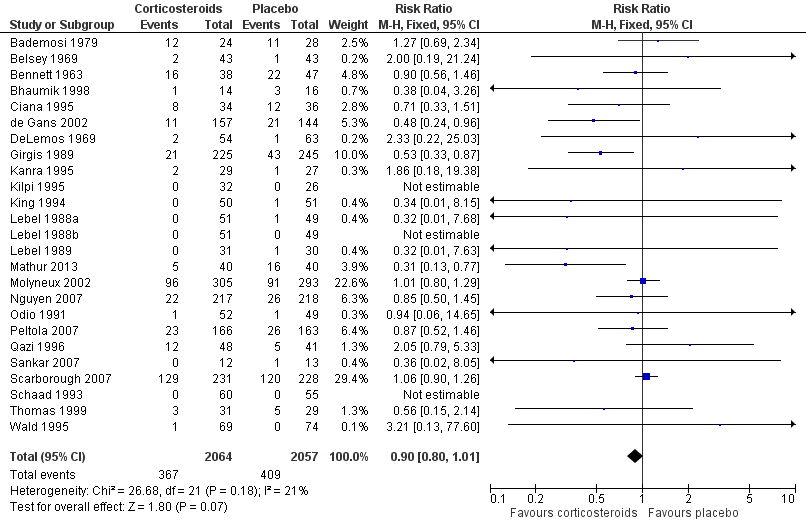
Forest plot of comparison: 1 All patients, outcome: 1.1 Mortality.
2. Hearing loss
The number of participants with hearing loss was significantly smaller in the corticosteroid‐treated group than in the placebo group (any hearing loss: 197 of 1424 (14%) versus 259 of 1361 (19%), RR 0.74, 95% CI 0.63 to 0.87; severe hearing loss: 75 of 1234 (6%) versus 112 of 1203 (9%), RR 0.67, 95% CI 0.51 to 0.88) (Belsey 1969; Bhaumik 1998; de Gans 2002; Girgis 1989; Kanra 1995; Kilpi 1995; King 1994; Lebel 1988a; Lebel 1988b; Lebel 1989; Mathur 2013; Molyneux 2002; Nguyen 2007; Odio 1991; Peltola 2007; Qazi 1996; Sankar 2007; Scarborough 2007; Schaad 1993; Wald 1995) (Analysis 1.2; Analysis 1.3; Figure 4; Figure 5).
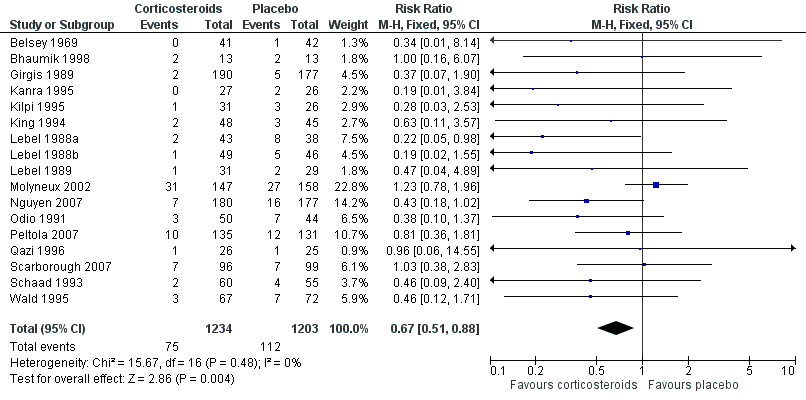
Forest plot of comparison: 1 All patients, outcome: 1.2 Severe hearing loss.
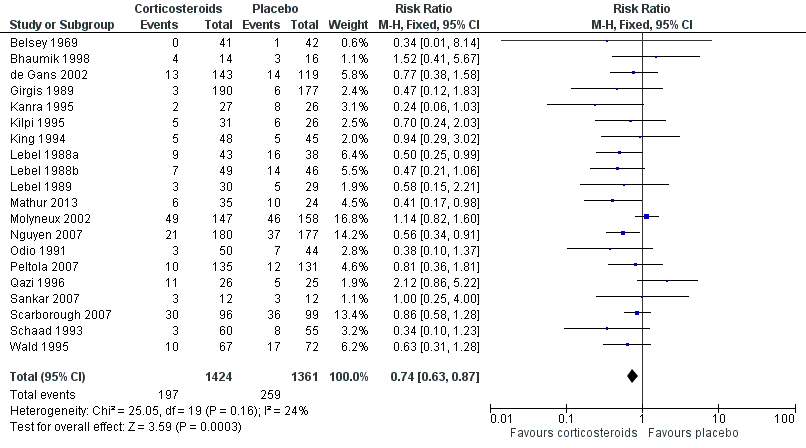
Forest plot of comparison: 1 All patients, outcome: 1.3 Any hearing loss.
3. Neurological sequelae
Short‐term neurologic sequelae (excluding hearing loss) were assessed in 13 studies including 1756 participants (Bhaumik 1998; Ciana 1995; de Gans 2002; Kanra 1995; Lebel 1988a; Lebel 1988b; Lebel 1989; Molyneux 2002; Peltola 2007; Sankar 2007; Scarborough 2007; Thomas 1999; Wald 1995) (Analysis 1.4). Fewer sequelae were observed in the corticosteroid‐treated group (161 of 900 (17.9%) versus 185 of 856 (21.6%), RR 0.83, 95% CI 0.69 to 1.00, P value = 0.05). Long‐term neurological sequelae were assessed in 12 studies including 1652 participants (DeLemos 1969; Girgis 1989; Kanra 1995; Kilpi 1995; King 1994; Lebel 1988a; Lebel 1988b; Nguyen 2007; Odio 1991; Qazi 1996; Schaad 1993; Wald 1995) (Analysis 1.5). The occurrence of long‐term sequelae was not significantly different between the corticosteroid‐treated participants and the controls (125 of 836 (15.3%) versus 136 of 816 (16.7%), RR 0.90, 95% CI 0.74 to 1.10) (Analysis 1.5).
Secondary outcome
1. Adverse events
Adverse events were recorded in 20 studies: 16 evaluated gastrointestinal haemorrhage, 12 recurrent fever, six reactive arthritis, five herpes zoster, three persistent fever and one fungal infections (Belsey 1969; Bennett 1963; Bhaumik 1998; de Gans 2002; Kanra 1995; Kilpi 1995; King 1994; Lebel 1988a; Lebel 1988b; Lebel 1989; Mathur 2013; Nguyen 2007; Odio 1991; Peltola 2007; Qazi 1996; Sankar 2007; Scarborough 2007; Schaad 1993; Thomas 1999; Wald 1995) (Analysis 1.6; Figure 6). Participants treated with corticosteroids had an increase in recurrent fever (RR 1.27, 95% CI 1.09 to 1.47). The rate of persistent fever was lower in the corticosteroid‐treated patients (RR 0.29, 95% CI 0.12 to 0.70). Other complications occurred in similar proportions of the treatment and control groups.
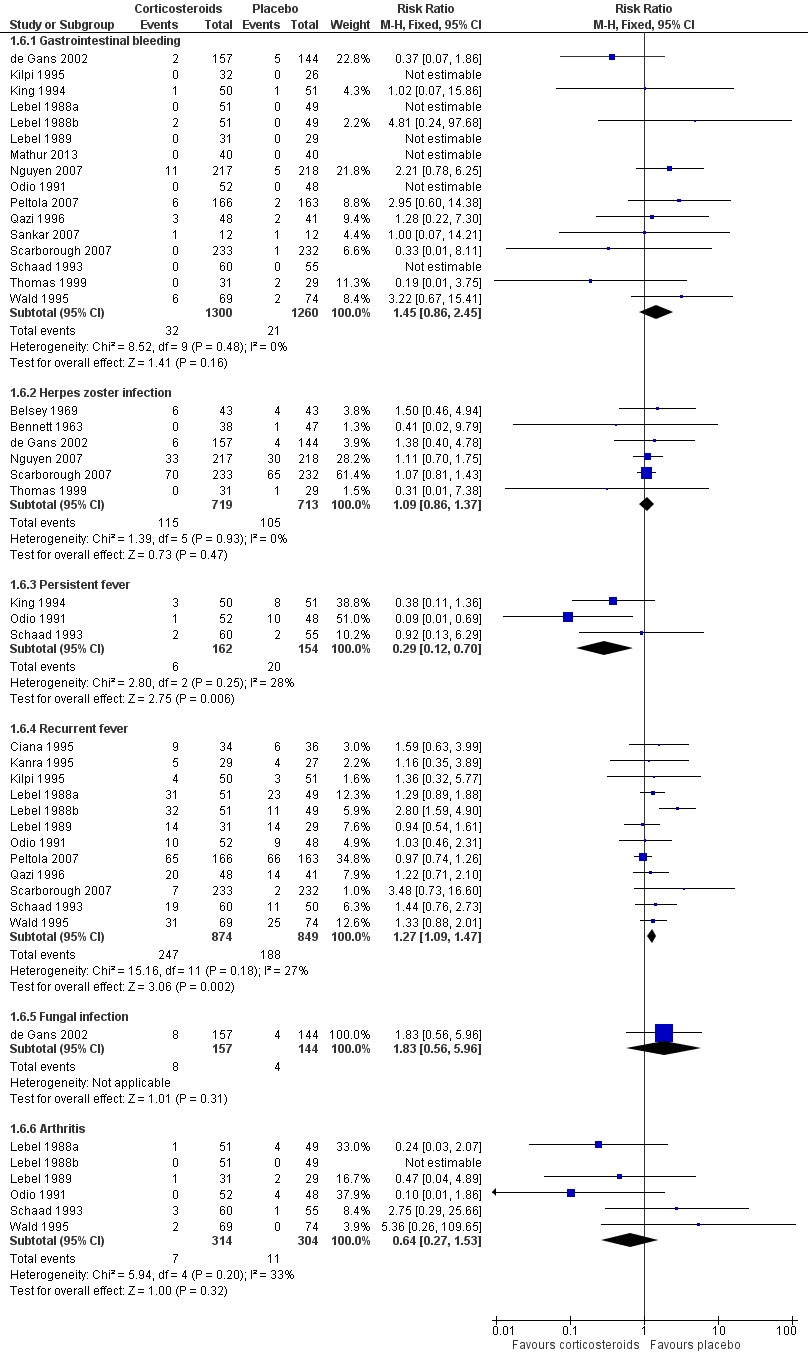
Forest plot of comparison: 1 All patients, outcome: 1.6 Adverse events.
Subgroup analysis
One hundred and sixty‐seven children out of 1269 (13.1%) in the corticosteroid‐treated group died, compared to 182 of 1242 (14.7%) in the placebo group (RR 0.89, 95% CI 0.74 to 1.07) (Belsey 1969; Ciana 1995; DeLemos 1969; Girgis 1989; Kanra 1995; Kilpi 1995; King 1994; Lebel 1988a; Lebel 1988b; Lebel 1989; Mathur 2013; Molyneux 2002; Peltola 2007; Qazi 1996; Sankar 2007; Schaad 1993; Mathur 2013) (Analysis 2.1).
Corticosteroids prevented hearing loss in children: any hearing loss was found in 146 of 1001 (14.6%) corticosteroid‐treated participants, compared to 196 of 960 (20.4%) in the control group (RR 0.73, 95% CI 0.61 to 0.86); severe hearing loss was found in 57 of 772 (7.3%) corticosteroid‐treated participants, compared to 86 of 752 (11.2%) in the control group (RR 0.67, 95% CI 0.49 to 0.91) (Analysis 2.3; Analysis 2.2).
For adults, study results on mortality were significantly heterogeneous (I2 statistic = 54%). Using the random‐effects model there was a non‐significant reduction in mortality rate: 187 of 756 (24.7%) died in the corticosteroid‐treated group versus 215 of 761 (28.3%; RR 0.74, 95% CI 0.53 to 1.05; P = 0.09) (Bennett 1963; Bhaumik 1998; de Gans 2002; Girgis 1989; Nguyen 2007; Scarborough 2007; Thomas 1999) (Analysis 3.1). The rate of hearing loss in adults was lower in corticosteroid‐treated participants as compared to controls (68 of 433 (15.7%) versus 90 of 411 (21.9%), RR 0.74, 95% CI 0.56 to 0.98; Analysis 3.2). There was a non‐significant reduction in short‐term neurologic sequelae in the corticosteroid‐treated group (RR 0.72, 95% CI 0.51 to 1.01; P = 0.06; Analysis 3.3).
Case‐fatality rate varied according to causative micro‐organism (Analysis 4.1). Out of 825 participants with H influenzae meningitis, 87 died (10.5%); compared to 371 of 1132 (32.8%) participants with pneumococcal meningitis and 27 of 620 (4.3%) participants with meningococcal meningitis. Corticosteroids protected against death in pneumococcal meningitis (RR 0.84, 95% CI 0.72 to 0.98) (Bademosi 1979; Bennett 1963; de Gans 2002; DeLemos 1969; Girgis 1989; Kanra 1995; Kilpi 1995; Lebel 1988a; Lebel 1988b; Molyneux 2002; Nguyen 2007; Odio 1991; Peltola 2007; Scarborough 2007; Schaad 1993; Thomas 1999; Wald 1995). In meningococcal meningitis, corticosteroids were associated with a non‐significant reduction in mortality (RR 0.71, 95% CI 0.35 to 1.46). For children with meningitis caused by H influenzae, hearing loss was significantly reduced by corticosteroids (RR 0.34, 95% CI 0.20 to 0.59; Analysis 4.3). For children with meningitis caused by bacteria other than H influenzae, no significant beneficial effect was seen (RR 0.95, 95% CI 0.65 to 1.39; Analysis 4.2).
We analysed studies in two subsets divided into high‐income (Belsey 1969; Bennett 1963; DeLemos 1969; de Gans 2002; Kanra 1995; Kilpi 1995; King 1994; Lebel 1988a; Lebel 1988b; Lebel 1989; Nguyen 2007; Odio 1991; Peltola 2007; Schaad 1993; Thomas 1999; Wald 1995) and low‐income countries (Bademosi 1979; Bhaumik 1998; Ciana 1995; Girgis 1989; Mathur 2013; Molyneux 2002; Qazi 1996; Scarborough 2007; Sankar 2007).
The risk ratio for mortality in high‐income countries was 0.81 (95% CI 0.63 to 1.05, P = 0.10) in corticosteroid‐treated participants and 0.87 (95% CI 0.67 to 1.15; random‐effects model; I2 statistic 55%; Analysis 5.1) in low‐income countries, with no heterogeneity between subgroups.
In high‐income countries the rates of severe hearing loss (RR 0.51, 95% CI 0.35 to 0.73; Analysis 5.2), any hearing loss (RR 0.58, 95% CI 0.45 to 0.73; Analysis 5.3) and short‐term neurologic sequelae (RR 0.64, 95% CI 0.48 to 0.85; Analysis 5.4) were lower in corticosteroid‐treated participants and showed significant heterogeneity with rates in the low‐income subgroup (severe hearing loss RR 0.99, 95% CI 0.72 to 1.38, I2 statistic for subgroups 86%; any hearing loss RR 0.89, 95% CI 0.76 to 1.04, I2 statistic 89%; short‐term neurological sequelae RR 1.03, 95% CI 0.81 to 1.31, I2 statistic 84%). Subgroup analysis for children in high‐income countries showed a decrease in risk of severe hearing loss and neurologic sequelae in the corticosteroid group (severe hearing loss, RR 0.52, 95% CI 0.35 to 0.78; short‐term sequelae, RR 0.67, 95% CI 0.46 to 0.97), whereas no difference was seen in low‐income countries (severe hearing loss, RR 1.00, 95% CI 0.69 to 1.47, I2 statistic for subgroups 81%; short‐term sequelae, RR 1.08, 95% CI 0.81 to 1.43, I2 statistic for subgroups 75%) (Analysis 5.5; Analysis 5.6; Analysis 5.7; Analysis 5.8). For adults in high‐income countries, no significant heterogeneity between subgroups was found (Analysis 5.9; Analysis 5.10).
Subgroup analysis on timing of corticosteroids (before or with the first dose of antibiotics versus after the first dose of antibiotics) showed similar results for mortality (RR 0.87 95% CI 0.69 to 1.09 (I2 statistic 52%, random‐effects model); RR 0.83, 95% CI 0.55 to 1.26) (Analysis 6.1; Analysis 6.2; Analysis 6.3; Analysis 6.4). For subgroup analyses of severe hearing loss and short‐term neurological sequelae, administration after the first dose of antibiotics had slightly more favourable point estimates than studies with early administration of corticosteroids, but there was no significant heterogeneity between subgroups.
We analysed studies in three categories of study quality according to the studies' 'Risk of bias' score (Figure 1). Four studies including 1793 participants were categorised as high quality (de Gans 2002; Molyneux 2002; Nguyen 2007; Scarborough 2007), 14 studies with 1477 participants as medium quality (DeLemos 1969; Kanra 1995; King 1994; Lebel 1988a; Lebel 1988b; Lebel 1989; Mathur 2013; Odio 1991; Peltola 2007; Qazi 1996; Sankar 2007; Sankar 2007; Schaad 1993; Thomas 1999; Wald 1995), and seven studies including 851 participants as low quality (Bademosi 1979; Belsey 1969; Bennett 1963; Bhaumik 1998; Ciana 1995; Girgis 1989; Kilpi 1995). No significant heterogeneity was found between subgroups of study quality for mortality, any hearing loss and short‐term neurological sequelae (Analysis 7.1; Analysis 7.3; Analysis 7.4). Severe hearing loss was reduced in studies of medium quality (RR 0.47, 95% 0.29 to 0.75; Analysis 7.2), but not in studies of high and low quality, with significant heterogeneity between subgroups (I2 statistic for subgroups 70%).
Sensitivity analysis
In the worst‐case scenario analyses where participants with missing data on severe hearing loss or any hearing loss in the corticosteroid groups were considered to have an unfavourable outcome, corticosteroids had no effect on severe or any hearing loss (Analysis 8.1; Analysis 8.2). In these analyses, studies were significantly heterogeneous and therefore we used the random‐effects model. One study provided 46% of missing values in the severe hearing loss analysis and 45% of missing values in the analysis on any hearing loss (Molyneux 2002). The worst‐case scenario for short‐term and long‐term neurological sequelae showed no beneficial effect of corticosteroids (Analysis 8.3; Analysis 8.4). None of the worst‐case scenarios showed evidence of harm with corticosteroid therapy.
Using the random‐effects model in analyses with no significant heterogeneity, the beneficial effect effects of corticosteroids remained significant in Analysis 1.2, Analysis 1.3, Analysis 1.6, Analysis 2.2, Analysis 2.3, Analysis 3.2, Analysis 4.3, Analysis 5.2, Analysis 5.3, Analysis 5.4, Analysis 5.6, Analysis 5.7, Analysis 6.3 and Analysis 7.2. The decrease in short‐term neurological sequelae did not remain significant with the random‐effects model, but did show a trend towards benefit (RR 0.83, 95% CI 0.69 to 1.00; P = 0.05). The beneficial effect of corticosteroids on mortality in pneumococcal meningitis found with the fixed‐effect model did not remain significant in the random‐effects model (RR 0.81, 95% CI 0.61 to 1.08; P = 0.16; Analysis 4.1).
The sensitivity analyses of studies with adequate sequence generation only showed that the decrease in short‐term neurological sequelae did not remain significant (RR 0.83, 95% CI 0.69 to 1.01). Results for other primary outcome measures did not differ from the initial analyses.
Discussion
Summary of main results
This meta‐analysis showed a beneficial effect of adjunctive corticosteroids in acute bacterial meningitis. Overall, corticosteroids significantly reduced the rate of hearing loss (risk ratio (RR) 0.74, 95% confidence interval (CI) 0.63 to 0.87), severe hearing loss (RR 0.67, 95% CI 0.51 to 0.88) and short‐term neurological sequelae (RR 0.83, 95% CI 0.69 to 1.00). The use of adjunctive corticosteroids was associated with a non‐significant decrease in mortality (RR 0.90, 95% CI 0.80 to 1.01). Use of adjunctive corticosteroids was not associated with a decrease in long‐term neurological sequelae (RR 0.90, 95% CI 0.74 to 1.10). Recurrent fever occurred more often in corticosteroid‐treated participants (RR 1.27, 95% CI 1.09 to 1.47), but other adverse events were found in similar proportions of the treatment and control group.
Subgroup analyses for age showed that in children with bacterial meningitis, corticosteroids prevented severe hearing loss (RR 0.67, 95% CI 0.49 to 0.91) and any hearing loss (RR 0.73, 95% CI 0.61 to 0.86). In adults, the rate of any hearing loss was lower in the corticosteroid‐treated group (RR 0.74, 95% CI 0.56 to 0.98); there was a non‐significant reduction in mortality in adults receiving corticosteroids (RR 0.74, 95% CI 0.53 to 1.05, P value = 0.09).
Subgroup analysis for causative organism showed that corticosteroids reduce severe hearing loss in children with meningitis due to H influenzae (RR 0.34, 95% CI 0.20 to 0.59), while no effect of corticosteroids on hearing loss was observed in children with non‐Haemophilus meningitis. Subgroup analysis on S pneumoniae showed a favourable effect of corticosteroids on mortality (RR 0.84, 95% CI 0.72 to 0.98). A non‐significant reduction in mortality was found in the N. meningitidis meningitis subgroup (RR 0.71, 95% CI 0.35 to 1.46). No effect on mortality was shown in H influenzae meningitis.
Subgroup analysis for high‐income and low‐income countries showed no significant effect on mortality for corticosteroid‐treated participants in high‐income and low‐income countries overall. Corticosteroids were protective against severe hearing loss (RR 0.51, 95% CI 0.35 to 0.73), any hearing loss (RR 0.58, 95% CI 0.45 to 0.73) and short‐term neurological sequelae (RR 0.64, 95% CI 0.48 to 0.85) in high‐income countries, with significant heterogeneity between subgroups. For children in high‐income countries, corticosteroids showed a protective effect against severe hearing loss (RR 0.52, 95% CI 0.35 to 0.78) and short‐term neurological sequelae (RR 0.67, 95% CI 0.46 to 0.97). No effect was observed in low‐income countries.
The sensitivity analyses showed that corticosteroids would have no effect on severe or any hearing loss and short‐ or long‐term neurological sequelae if all missing data were imputed as unfavourable events in the corticosteroid‐treated participants. Corticosteroids were not associated with harm in this worst‐case scenario. Further sensitivity analyses showed that the effect of corticosteroids on overall short‐term neurological sequelae and mortality in pneumococcal meningitis would not be significant if the random‐effects model was used. The beneficial effect on short‐term neurological sequelae changed to a trend towards benefit if only studies with adequate sequence generation were included.
Overall completeness and applicability of evidence
Overall completeness
The available studies do not address four important issues ‐ the minimum duration of corticosteroid therapy, type of corticosteroids, the maximum length of time after parenteral antibiotic therapy for commencement of corticosteroid therapy and long‐term effect of corticosteroid therapy. In most studies, a four‐day regimen of dexamethasone (0.4 or 0.6 mg/kg/day) divided into four daily doses was used. One randomised, prospective study involving 118 children with bacterial meningitis showed a two‐day and four‐day regimen of dexamethasone to be similarly effective (Syrogiannopoulos 1994). In this study physicians were not blinded to the treatment groups. Long‐term neurological sequelae, or moderate hearing impairment (or both), were found in 1.8% and 3.8% of patients treated with dexamethasone for two and four days, respectively. It is unlikely that a randomised controlled trial (RCT) will be performed to answer the question of whether a two‐day or four‐day regimen should be used in bacterial meningitis; such a clinical trial would need a very large number of patients enrolled to detect significant differences between groups. Since most studies used a four‐day regimen (without increase of side effects) we advise the use of the four‐day corticosteroid therapy.
Three studies used hydrocortisone and/or prednisolone; all others used dexamethasone. Clinical efficacy depends on glucocorticoid pharmacokinetics and pharmacodynamics; of glucocorticoids, dexamethasone has superior penetration in the cerebrospinal fluid (CSF) and a longer half life (Balis 1987). Therefore, dexamethasone is considered to be the corticosteroid of choice in bacterial meningitis.
Subgroup analyses for timing of corticosteroids (before or with the first dose of antibiotics versus after the first dose of antibiotic) showed no differences in efficacy of corticosteroids. In previous reports, administration of corticosteroids before or with the first dose of parenteral antibiotics seemed to be more effective than administration after the first dose of antibiotics (King 1994; McIntyre 1997). A RCT involving 301 adults with bacterial meningitis in European countries showed a beneficial effect of the corticosteroid dexamethasone on unfavourable outcome and mortality (de Gans 2002). In this European study, dexamethasone or placebo was administered before or with the first dose of antibiotic (de Gans 2002). The beneficial effect of dexamethasone on mortality was most apparent in patients with pneumococcal meningitis. In a post hoc analysis of this study, the beneficial effect of dexamethasone on mortality in patients with pneumococcal meningitis was attributable to a reduction in systemic complications (van de Beek 2004a). Although speculative and not supported by clinical data, one implication of this finding might be that the effect of dexamethasone is not restricted to the first hours after administration (van de Beek 2006b).
A meta‐analysis of individual patient data (van de Beek 2010) was performed with five recent large RCTs on adjunctive dexamethasone therapy in bacterial meningitis (de Gans 2002; Molyneux 2002; Nguyen 2007; Peltola 2007; Scarborough 2007). Data from 2029 patients from five trials were included and the aim of this analysis was to establish whether any subgroups of patients with acute bacterial meningitis might benefit from adjunctive dexamethasone. Extensive exploration of 15 pre‐specified subgroups did not show robust evidence that a particular subgroup would benefit; although there was a benefit in adults aged over 55 years (McIntyre 2010; van de Beek 2010). There were no differences in efficacy of adjunctive dexamethasone with regard to the timing of corticosteroids.
In experimental pneumococcal meningitis, CSF bacterial concentrations appeared to be more important than the timing of dexamethasone therapy in influencing the antibacterial‐induced inflammatory response (Lutsar 2003). Hence, there is a time period beyond which corticosteroid loses its effectiveness after the first (parenteral) administration of an antibiotic agent but this time interval has not been clearly defined. On the basis of the available evidence, dexamethasone should be preferably started before or with the first dose of antibiotic therapy.
A long‐term follow‐up study on adjunctive dexamethasone treatment in tuberculous meningitis showed the initial beneficial effect of adjunctive dexamethasone was abolished because of delayed mortality within five years (Török 2011). To assess the long‐term effects of adjunctive corticosteroid treatment in bacterial meningitis and determine whether a similar phenomenon could be identified, a long‐term follow‐up study was performed in participants included in the European Dexamethasone Study (de Gans 2002; Fritz 2012). The study included 228 of 246 evaluable participants surviving the initial trial period. After a median follow‐up of 13 years, mortality in the dexamethasone group was 22% compared to 33% in the placebo group (P = 0.029) (Fritz 2012). The authors conclude that the beneficial effect of dexamethasone that is obtained in the acute phase of the disease remains for years. This provides another reason to administer adjunctive corticosteroids in adult bacterial meningitis patients in high‐income countries.
However, long‐term follow‐up studies of patients included in other RCTs are needed to confirm the persistence of benefit from adjunctive dexamethasone.
Applicability of evidence
In children with acute bacterial meningitis, corticosteroids reduced hearing loss from 20.4% to 14.6% and severe hearing loss from 11.2% to 7.3%. A large proportion of included children had meningitis due to H influenzae type B, which has been virtually eliminated in high‐income countries since routine vaccination of children against this bacterium started (McIntyre 2012; Peltola 2000; van de Beek 2006b). Nevertheless, subgroup analysis in children in high‐income countries showed a protective effect of adjunctive corticosteroids on severe hearing loss overall and a favourable point estimate for severe hearing loss due to non‐Haemophilus meningitis. The results of this review support the use of adjunctive corticosteroids in children in high‐income countries with meningitis due to all micro‐organisms based on the lack of evidence of adverse events (in general and micro‐organism specific) of dexamethasone in the corticosteroid‐treated group. However, as conclusive evidence is lacking for this subgroup, administration of corticosteroids to children with meningitis due to bacteria other than H influenzae remains controversial.
Only one study in this analysis involved children with neonatal meningitis and showed a beneficial effect of corticosteroids on outcomes (Mathur 2013). However, the study was relatively small and treatment groups were not well balanced with regards to patient age, culture positivity and causative micro‐organisms. Additional RCTs evaluating corticosteroids in neonatal meningitis need to be performed before definitive conclusions can be drawn on the role of dexamethasone treatment in neonatal meningitis.
On the basis of the benefits of corticosteroid therapy in the adult population in high‐income countries, dexamethasone should be commenced in adults with suspected or proven community‐acquired bacterial meningitis in high‐income countries (van de Beek 2006a). For adults in low‐income countries, the use of corticosteroids is neither beneficial nor harmful.
The use of steroids was associated with fewer cases of persistent fever and more cases of recurrent fever, but not with serious adverse events. However, definitions of adverse events used in the studies were heterogeneous and most studies had no specified criteria in advance, so under‐ascertainment is likely.
Concerns have been raised over the interference by corticosteroids in CSF eradication of meningeal pathogens by reducing the blood‐brain barrier permeability and thereby the penetration of antibiotics in the subarachnoid space. Therapeutic failures have been described in adults treated with standard doses of vancomycin and adjunctive dexamethasone (Viladrich 1991). However, two studies showed with repeated lumbar punctures that, in both adults and children, treatment with dexamethasone did not reduce vancomycin levels in the CSF (Klugman 1995; Ricard 2007). Although these results are reassuring, patients with pneumococcal meningitis who are treated with vancomycin and dexamethasone should still be carefully observed throughout therapy (van de Beek 2006a).
In adults who survive acute bacterial meningitis, cognitive impairment occurs frequently (van de Beek 2002; van de Beek 2006a). As corticosteroids may potentiate ischaemic injury to neurons (Sapolsky 1985), it is important to know whether corticosteroids have beneficial effects on hearing loss and mortality but worsen cerebral cortical functioning (van de Beek 2006b). Neuropsychological outcome was evaluated in patients included in the European Dexamethasone Study who survived pneumococcal or meningococcal meningitis (Weisfelt 2006). In 87 out of 99 eligible patients, 46 (53%) of whom were treated with dexamethasone and 41 (47%) of whom received placebo, no significant differences in outcome were found between patients in the dexamethasone and placebo groups (medium time between meningitis and testing was eight years). In another study on long‐term neuropsychological outcomes and dexamethasone in children, children who contracted pneumococcal meningitis and were treated with corticosteroids showed better academic achievements compared with children with pneumococcal meningitis who were not treated with adjunctive corticosteroids (Ozen 2006).
Quality of the evidence
Of the 25 randomised clinical trials included in the meta‐analysis four were of high quality, 14 of medium quality and seven of low quality. Although the number of high‐quality studies was low, the number of participants in these studies accounted for 45% of participants included in the meta‐analysis. Studies were mostly categorised as medium or low quality due to a lack of addressing missing data or because no intention‐to‐treat analysis was performed. For the analysis on severe hearing loss, significant heterogeneity between trials of high, medium and low quality was found. As studies of high quality showed no effect the results of this meta‐analysis should interpreted with caution.
The sensitivity analysis showed that in a worst‐case scenario dexamethasone would have no beneficial or harmful effect on hearing loss or neurological sequelae. However, this analysis was heavily influenced by a single study accounting for 46% of missing values. When this study was left out a trend towards benefit of dexamethasone on any hearing loss was found (Molyneux 2002). Further sensitivity analyses showed that the effect of corticosteroids on overall short‐term neurological sequelae and mortality in pneumococcal meningitis would not be significant if the random‐effects model was used.
Potential biases in the review process
Several biases may have diminished the reliability of our results. The first confounding factor is selection bias. Several studies on childhood meningitis had exceptionally low mortality rates; nine studies had mortality rates of 3% or less. Mortality rates of childhood bacterial meningitis in previous reported studies ranged from 8% to 20% (Baraff 1993; Bohr 1983). Inclusion of studies in the meta‐analysis with less severe illness, as reflected in the very low case‐fatality rates, will probably underestimate the protective effect of corticosteroids (Glasziou 1995). Five studies had very high mortality rates (over 25%). For patients admitted in a late state of disease, adjuvant corticosteroids are less protective and might even be harmful (Prasad 1995). Inclusion of such patients might again lead to an underestimation of the treatment effect.
A second bias is introduced when participants are withdrawn (Prasad 1995; Qazi 1996). The analysis was based upon per‐protocol figures, as intention‐to‐treat (ITT) figures were only available for six studies (24%). A total of 211 participants were withdrawn after the randomisation process, often for unknown reasons. Reasons for withdrawal include ineligibility according to the trial criteria or inability to complete the treatment protocol (Prasad 1995). Withdrawals on the grounds on ineligibility may have been influenced by knowledge of outcome; if so, this would advantage the corticosteroid regimen. Excluding participants because of an inability to complete the course of corticosteroids due to side effects (for example, upper gastrointestinal bleeding) clearly introduces bias in favour of the study medication, whereas withdrawals due to loss to follow‐up might favour the placebo group. In the Egyptian study, which was not placebo‐controlled and not double‐blinded, only three pathogens were cultured from the cerebral spinal fluid of enrolled participants, suggesting withdrawal of participants with other bacteria culture from CSF and those with negative CSF cultures (Girgis 1989).
A third bias is introduced by competing risks. The comparisons of hearing loss and neurologic sequelae (other than hearing loss) were made excluding all participants who died. Since mortality is possibly a treatment‐related outcome, the treatment groups that exclude fatality cases may not be comparable. Competing risks in this analysis will lead to an underestimation of the treatment effect of corticosteroids.
Finally, the included studies were heterogeneous with respect to the study protocols. The first study was published in 1963 (Bennett 1963), the last in 2012 (Mathur 2013). Several different study interventions were used. Therefore, study population effect sizes were calculated as risk ratios.
Agreements and disagreements with other studies or reviews
Four meta‐analyses on the use of adjunctive dexamethasone in adults were published, two in 2009 (Assiri 2009; Vardakas 2009) and two in 2012 (Borchorst 2012; Bernardo 2012). The first meta‐analysis (Vardakas 2009) concluded that dexamethasone was associated with a non‐significant decrease in mortality, but when the trial from Malawi was left out the decrease in mortality did reach significance. The reasons for excluding the Malawian trial were a HIV‐positive population, high mortality, poor general status and low human development index (HDI) (< 0.5). However, other countries that were included had only slightly higher HDIs at the time of inclusion (Girgis 1989, Egypt 0.53; Bhaumik 1998 India 0.53, Scarborough 2007 Malawi 0.49). Several subgroup analyses showed that dexamethasone was most beneficial in patients with definite meningitis, in high‐ and medium‐income countries and patients with a short duration of symptoms. Out of four analyses eight subgroups consisted of only one or two studies, limiting the value of the meta‐analysis. Analyses on mortality and hearing loss in high‐ and medium‐income countries were similar to our results. The study by Bennett 1963 was not included in this meta‐analysis for unknown reasons. The second meta‐analysis included four recent trials in adults (de Gans 2002; Nguyen 2007; Scarborough 2007; Thomas 1999) and concluded that dexamethasone reduced mortality in high‐income countries (Assiri 2009). The third meta‐analysis (Borchorst 2012) included 29 randomised studies and had similar conclusions as the Cochrane 2010 meta‐analysis (Brouwer 2010a), which were that adjunctive dexamethasone was beneficial in adults in high‐income countries, especially in patients with pneumococcal meningitis. The fourth meta‐analysis (Bernardo 2012) included only paediatric studies and concluded that adjunctive dexamethasone was not associated with a reduction in mortality, hearing loss or sequelae (Bernardo 2012). The reason why seven studies included in the Cochrane 2013 updated meta‐analysis were not included in the meta‐analysis of paediatric studies was not specified (Brouwer 2013). According to the classification of study quality used, most of these studies were of similar quality to those that were included.
The difference in efficacy of corticosteroids between high‐ and low‐income countries was mainly driven by two large studies from Malawi (Molyneux 2002; Scarborough 2007), together representing 60% of included participants from low‐income countries. Participants included in these studies were often HIV‐positive, presented late in the disease course or received inappropriate antibiotic therapy (Molyneux 2002; Scarborough 2007). There may be several reasons for the difference in efficacy of corticosteroids such as delayed presentation, clinical severity, underlying anaemia, malnutrition, the antibiotics used, HIV infection or other unidentified differences between populations. Recently, genetic factors were suggested to influence the patient's response to corticosteroids (Brouwer 2012). A study compared characteristics of children with culture‐positive community‐acquired bacterial meningitis in the Children's Unit, Queen Elizabeth Central Hospital, Blantyre, Malawi and in the Royal Liverpool Children's Hospital, UK from time periods before the introduction of vaccines (Molyneux 2006). Children in Malawi presented later and were more often comatose and malnourished, compared to children in Britain. Mortality from bacterial meningitis in children in Malawi was much higher than in children in Britain (41% versus 7%), even when infected with the same organism. Several studies have shown that a delay in initiation of antibiotic treatment is associated with worse outcome in bacterial meningitis (McMillan 2001; Køster‐Rasmussen 2008; Proulx 2005). A meta‐analysis on timing of steroids with respect to initial symptoms could not be performed because outcome data were not specified for patients presenting early or late during clinical course in any of the studies. Nevertheless, we stress the need for early diagnosis and treatment.
A meta‐analysis of individual patient data was performed with five large RCTs (de Gans 2002; Molyneux 2002; Nguyen 2007; Peltola 2007; Scarborough 2007; van de Beek 2010). Data from 2029 patients from five trials were included in the analysis (833 (41.0%) aged < 15 years). HIV infection was confirmed or likely in 580 (28.6%) patients and bacterial meningitis was confirmed in 1639 (80.8%). Dexamethasone was not associated with a significant reduction in death (270 of 1019 (26.5%) on dexamethasone versus 275 of 1010 (27.2%) on placebo; odds ratio (OR) 0.97, 95% CI 0.79 to 1.19), death or severe neurological sequelae or bilateral severe deafness (42.3% versus 44.3%; OR 0.92, 95% CI 0.76 to 1.11), death or any neurological sequelae or any hearing loss (54.2% versus 57.4%; OR 0.89, 95% CI 0.74 to 1.07), or death or severe bilateral hearing loss (36.4% versus 38.9%; OR 0.89, 95% CI 0.73 to 1.69). However, dexamethasone reduced hearing loss among survivors (24.1% versus 29.5%; OR 0.77, 95% CI 0.60 to 0.99, P = 0.04). Dexamethasone had no effect in any of the pre‐specified subgroups, including specific causative organisms, pre‐dexamethasone antibiotic treatment, HIV status or age. The differences between Malawi and the other clinical settings call into question the appropriateness of summary measures that combine the results, even if statistical tests of heterogeneity are deemed acceptable. Mortality rates in the two studies from Malawi were three to five‐fold higher than in the studies from Europe, South America and Vietnam (de Gans 2002; Molyneux 2002; Nguyen 2007; Peltola 2007; Scarborough 2007). In subgroups of the individual patient data meta‐analysis, there were several instances in which the I2 statistic was more than 50%, which indicates at least moderate heterogeneity (McIntyre 2010). This current Cochrane review confirms the beneficial effect of corticosteroids on hearing loss that was found in the subgroups of the individual meta‐analysis (van de Beek 2010). Treatment with adjunctive corticosteroids was not associated with harm. In order to establish with certainty whether or not dexamethasone has a place in the treatment of bacterial meningitis, a large multinational RCT in that subgroup would be necessary. Such a trial would need to include approximately 13,500 participants to show an odds ratio (OR) of 0.9 with a power of 90% in a population with 27% risk of death in the placebo group, and is therefore unlikely to be performed or finished in the next decade. Meanwhile, results of our analysis support the use of corticosteroids in children and adults with community‐acquired bacterial meningitis in high‐income countries.
Implementation studies
Seven studies evaluated the implementation of adjunctive dexamethasone treatment and its effect on the outcome of bacterial meningitis (Bodilsen 2014; Brouwer 2010b; Castelblanco 2014; Cornelis 2011; Heckenberg 2012b; Koopmans 2013; Peterković 2012). Three studies compared the prognosis of adult pneumococcal, meningococcal and Listeria monocytogenes meningitis between two nationwide prospective cohort studies; one was performed before and the other after the implementation of adjunctive dexamethasone (Brouwer 2010b; Heckenberg 2012b; Koopmans 2013). The studies showed that after the introduction of adjunctive dexamethasone, 84% of patients with pneumococcal meningitis, 89% of adults with meningococcal meningitis and 53% of L monocytogenes meningitis received the recommended four‐day regimen (40 mg/day in four doses). The mortality from pneumococcal meningitis decreased from 30% to 20% after the introduction of dexamethasone (P value = 0.001) and the rate of hearing loss decreased from 22% to 12% (P value = 0.001) (Brouwer 2010b). Meningococcal disease mortality declined from 7% to 4% and hearing loss from 8% to 3%, but these differences did not reach statistical significance (Heckenberg 2012b). No evidence of harm from dexamethasone was identified in studies on pneumococcal and meningococcal meningitis. The beneficial effect of dexamethasone on pneumococcal meningitis was similar to that identified in the European Dexamethasone Study (de Gans 2002). For listerial meningitis, an increase in unfavourable outcome from 27% to 61% was observed between the first and second cohort study (Koopmans 2013). In a multivariate analysis bacterial genotype was found to be the main cause of the poorer prognosis. Dexamethasone was not associated with a change in mortality, hearing loss or sequelae in listerial meningitis. However, as adjunctive dexamethasone treatment was another major change between cohorts, it was suggested to discontinue dexamethasone when L monocytogenes is identified. A nationwide retrospective study from Denmark showed dexamethasone was administered to 60% of meningitis cases between 2008 and 2012 compared to 37% between 2003 and 2007 (Bodilsen 2014). Dexamethasone treatment was associated with a significant decrease in the risk of an unfavourable outcome (33% versus 53%) and mortality (15% versus 24%). The implementation studies provide additional (class III) evidence that adjunctive dexamethasone is beneficial in adults with bacterial meningitis in high‐income countries.
In a population‐based observational study from the USA, incidence and mortality of bacterial meningitis due to the five most common pathogens between 1997 and 2010 were studied in a network database (Castelblanco 2014). The study showed that over time mortality declined. This was attributed to the publication of the IDSA guideline of 2004, which advised adjunctive dexamethasone for all suspected bacterial meningitis cases (Castelblanco 2014). However, data on dexamethasone use were not available and therefore a causal relation could not be established.
Retrospective studies in Belgium and Croatia evaluated whether the use of dexamethasone improved prognosis in adults (Peterković 2012), or both adults and children (Cornelis 2011). Both studies showed no effect of dexamethasone. However, in both studies the rationale to give or withhold dexamethasone was unclear and therefore confounding by indication (patients with severe sickness get more medication, i.e. dexamethasone, but still have a worse prognosis) is a major problem in these studies, as is the retrospective design.
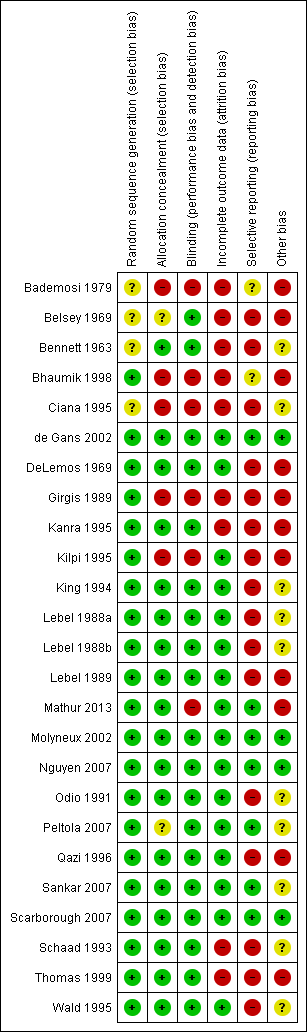
'Risk of bias' summary: review authors' judgements about each methodological quality item for each included study.

'Risk of bias' graph: review authors' judgements about each methodological quality item presented as percentages across all included studies.
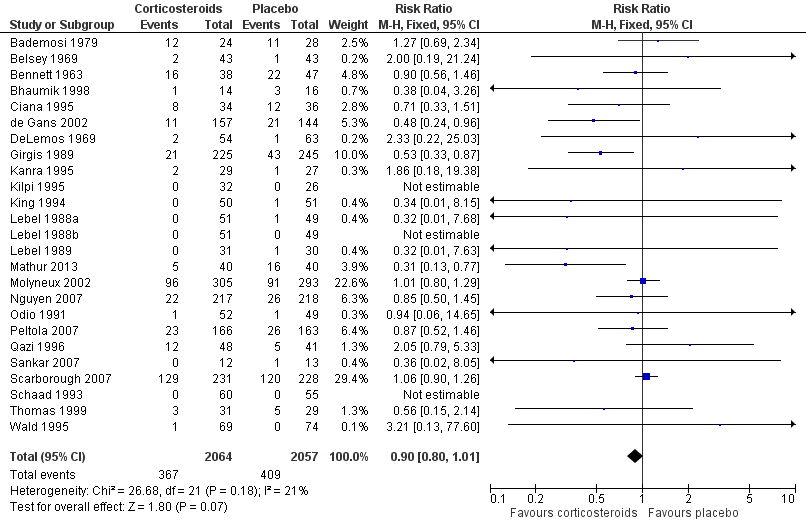
Forest plot of comparison: 1 All patients, outcome: 1.1 Mortality.
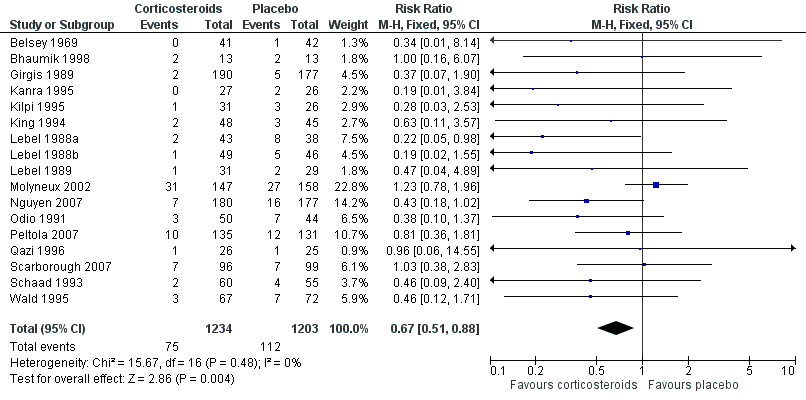
Forest plot of comparison: 1 All patients, outcome: 1.2 Severe hearing loss.
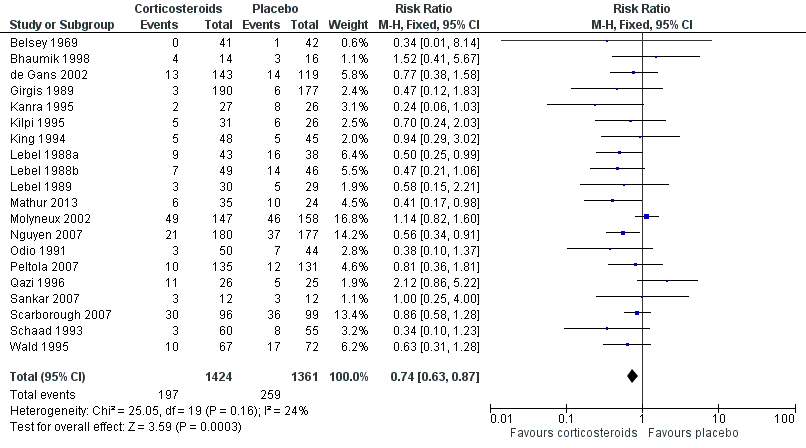
Forest plot of comparison: 1 All patients, outcome: 1.3 Any hearing loss.
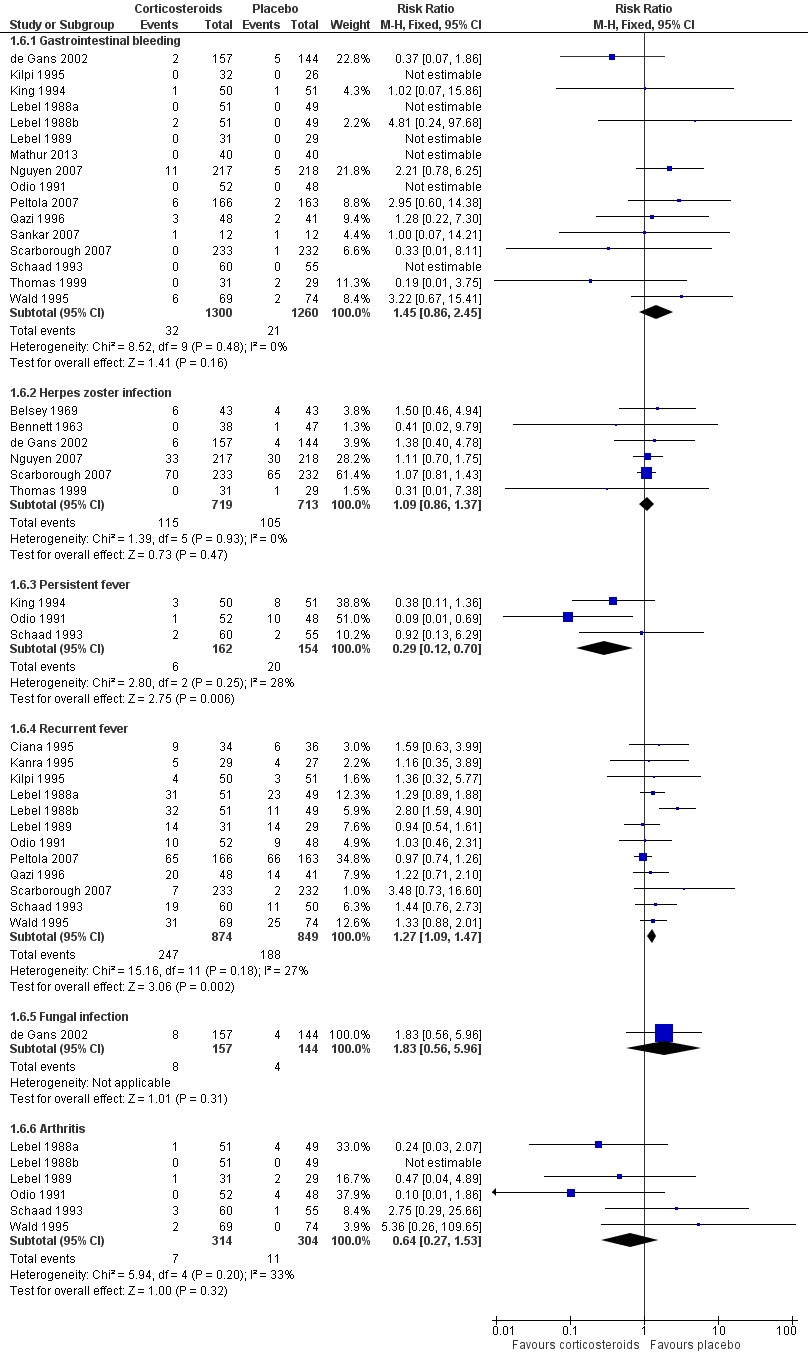
Forest plot of comparison: 1 All patients, outcome: 1.6 Adverse events.

Comparison 1 All patients, Outcome 1 Mortality.

Comparison 1 All patients, Outcome 2 Severe hearing loss.

Comparison 1 All patients, Outcome 3 Any hearing loss.

Comparison 1 All patients, Outcome 4 Short‐term neurological sequelae.
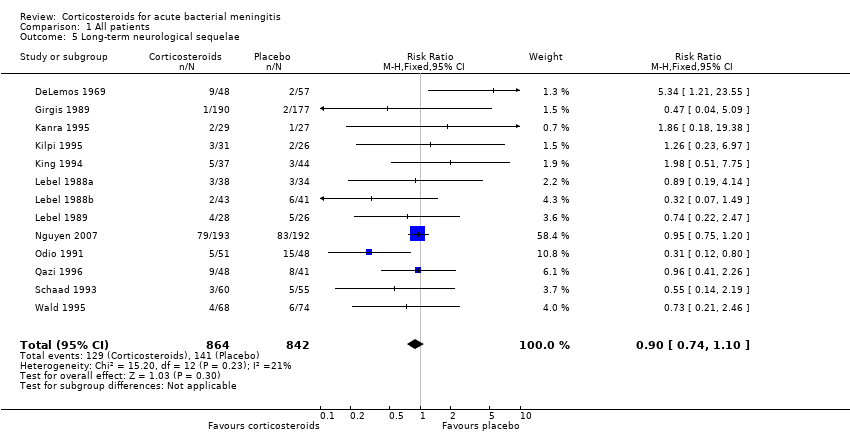
Comparison 1 All patients, Outcome 5 Long‐term neurological sequelae.
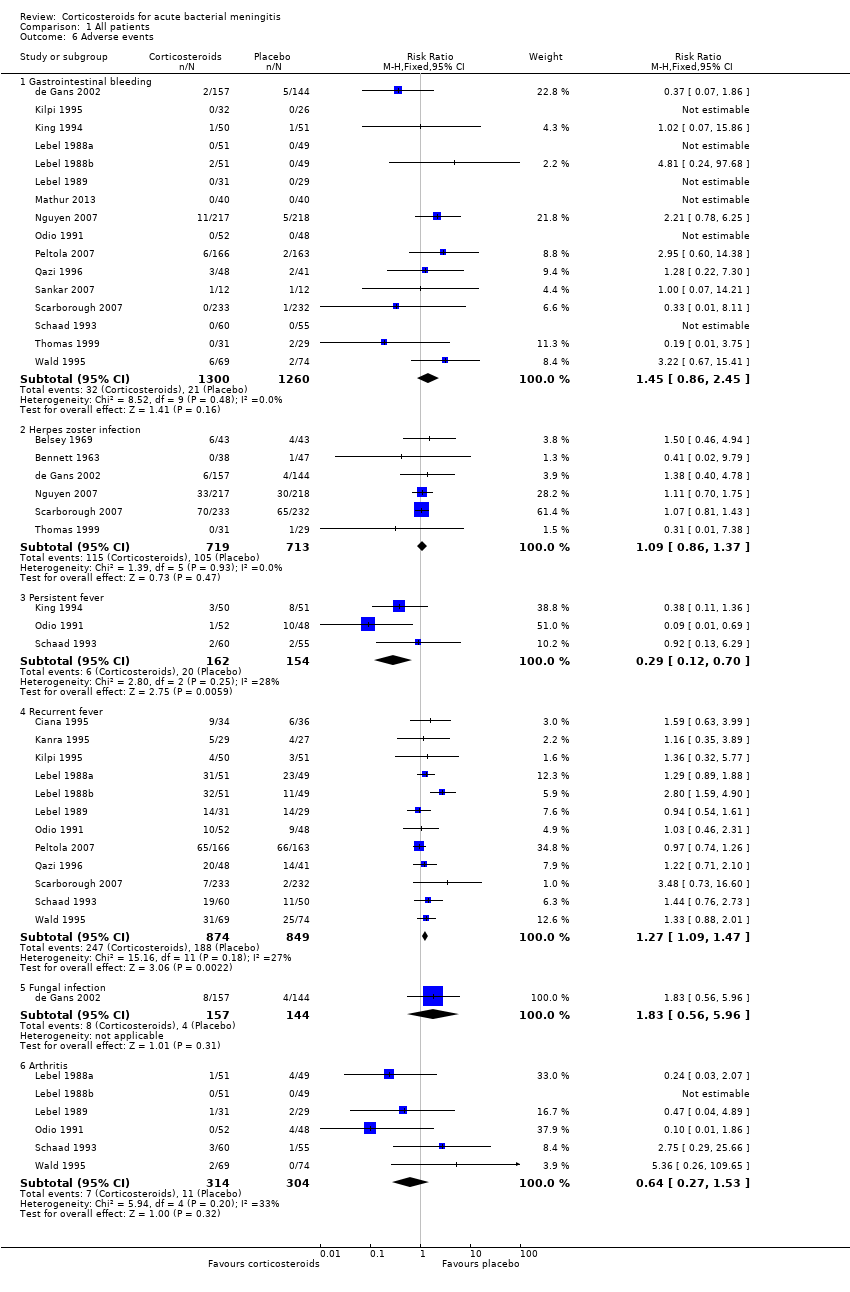
Comparison 1 All patients, Outcome 6 Adverse events.

Comparison 2 Children, Outcome 1 Mortality.
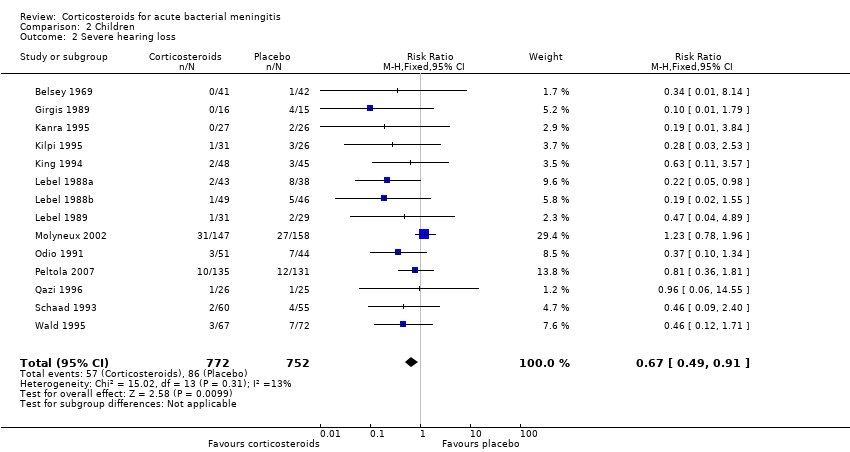
Comparison 2 Children, Outcome 2 Severe hearing loss.
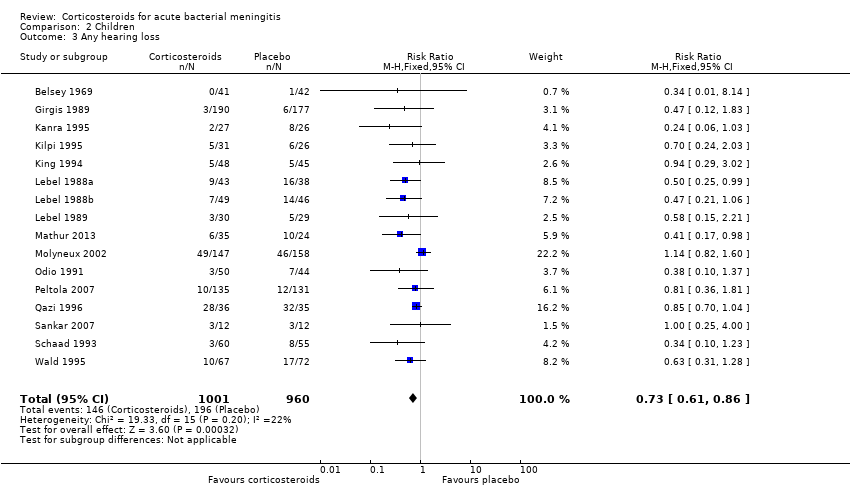
Comparison 2 Children, Outcome 3 Any hearing loss.

Comparison 3 Adults, Outcome 1 Mortality.
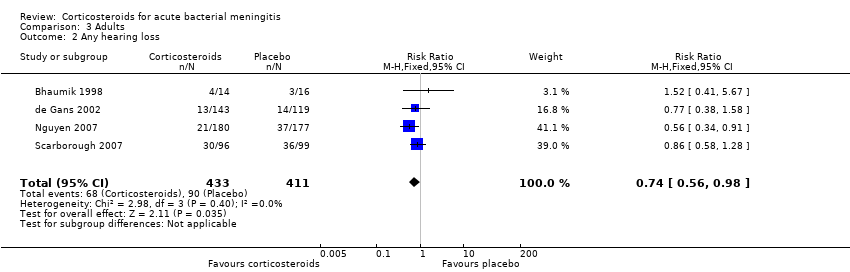
Comparison 3 Adults, Outcome 2 Any hearing loss.
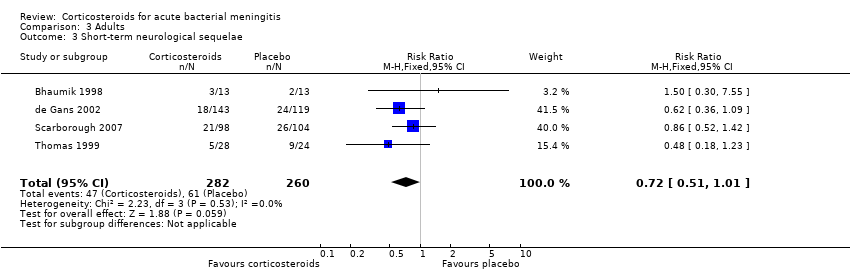
Comparison 3 Adults, Outcome 3 Short‐term neurological sequelae.
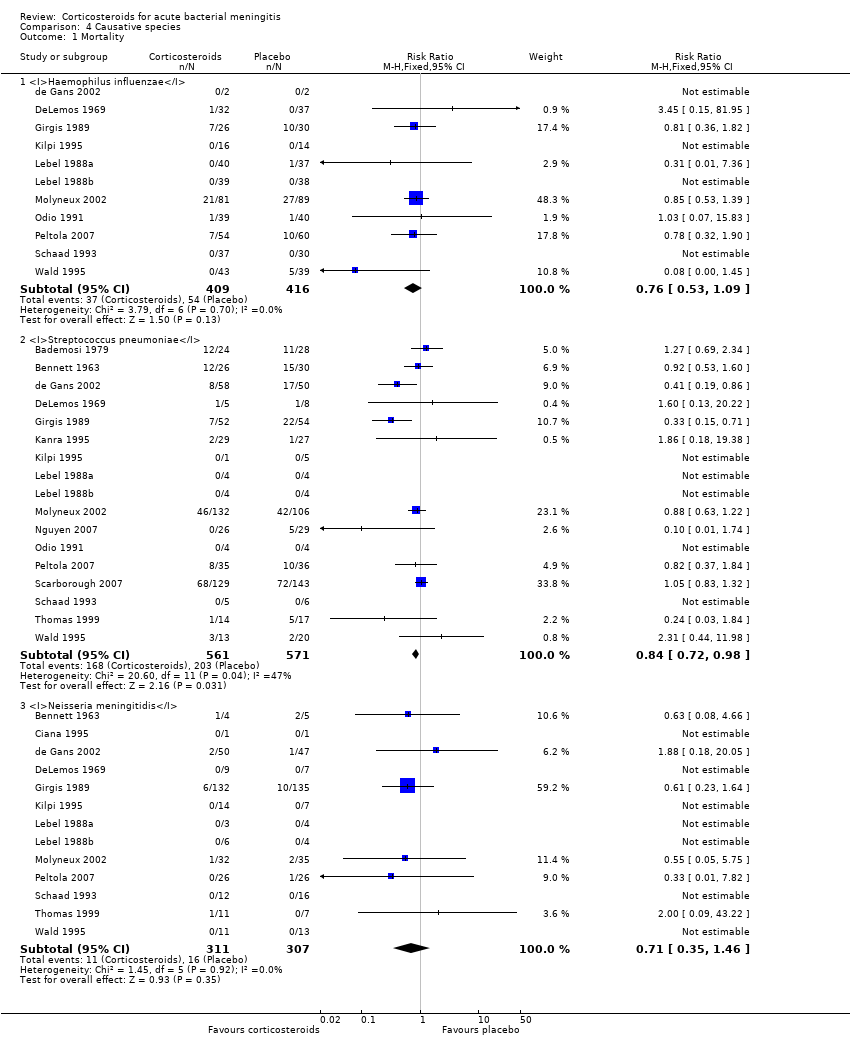
Comparison 4 Causative species, Outcome 1 Mortality.

Comparison 4 Causative species, Outcome 2 Severe hearing loss in children ‐ non‐Haemophilus influenzae species.

Comparison 4 Causative species, Outcome 3 Severe hearing loss in children ‐ Haemophilus influenzae.

Comparison 5 Income of countries, Outcome 1 Mortality ‐ all patients.

Comparison 5 Income of countries, Outcome 2 Severe hearing loss ‐ all patients.

Comparison 5 Income of countries, Outcome 3 Any hearing loss.
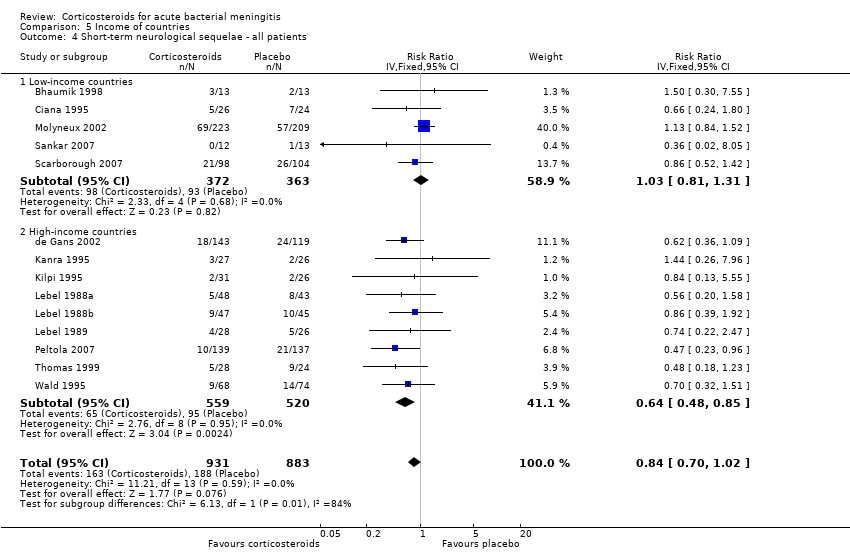
Comparison 5 Income of countries, Outcome 4 Short‐term neurological sequelae ‐ all patients.

Comparison 5 Income of countries, Outcome 5 Mortality ‐ children.
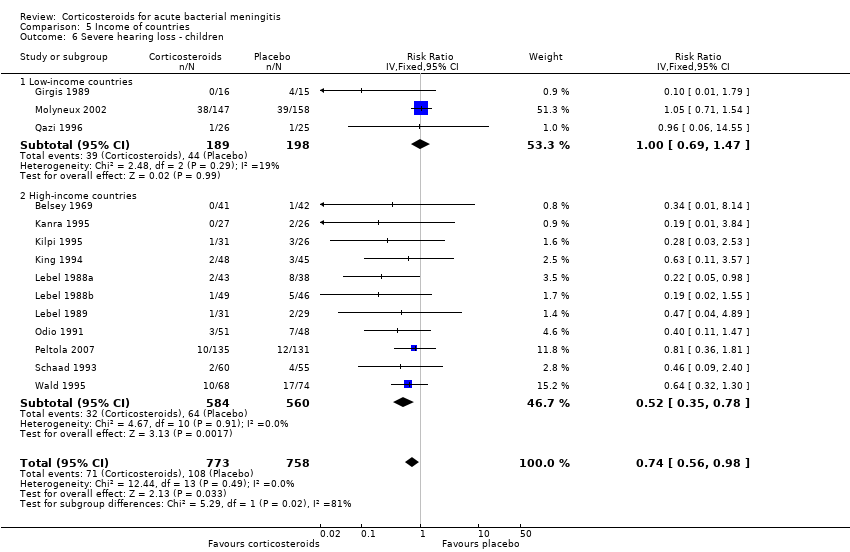
Comparison 5 Income of countries, Outcome 6 Severe hearing loss ‐ children.

Comparison 5 Income of countries, Outcome 7 Short‐term neurological sequelae ‐ children.

Comparison 5 Income of countries, Outcome 8 Severe hearing loss in children due to non‐Haemophilus influenzae species.

Comparison 5 Income of countries, Outcome 9 Mortality ‐ adults.

Comparison 5 Income of countries, Outcome 10 Any hearing loss adults.
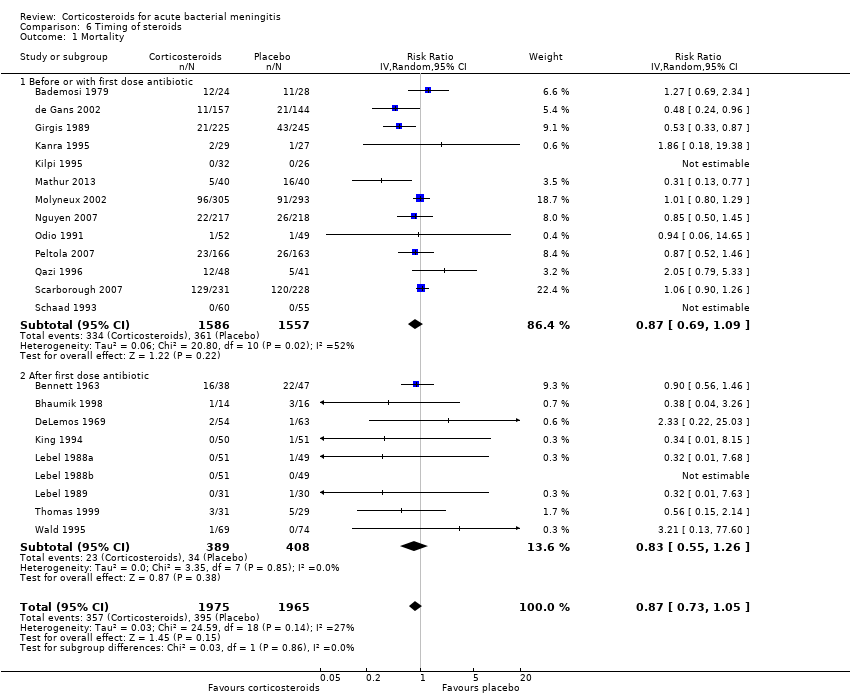
Comparison 6 Timing of steroids, Outcome 1 Mortality.

Comparison 6 Timing of steroids, Outcome 2 Severe hearing loss.
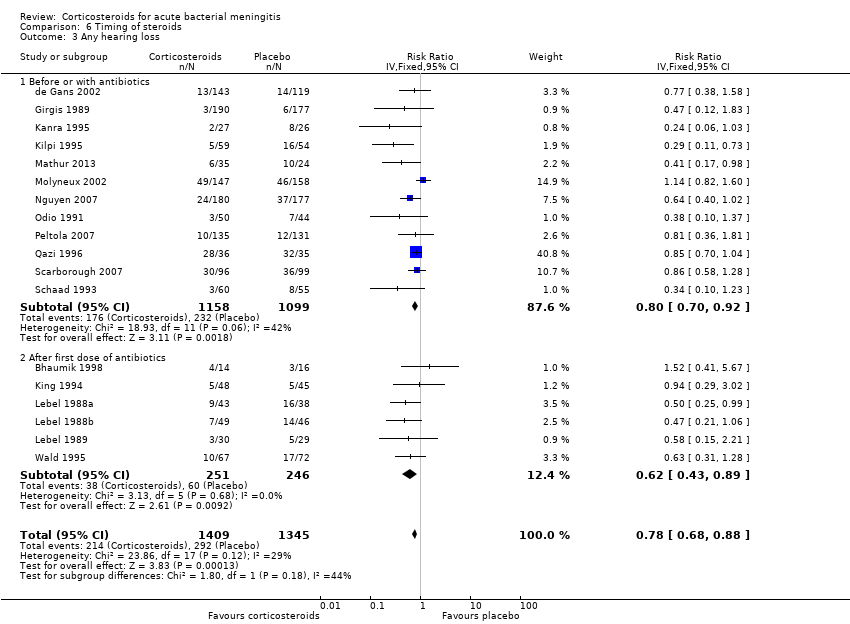
Comparison 6 Timing of steroids, Outcome 3 Any hearing loss.
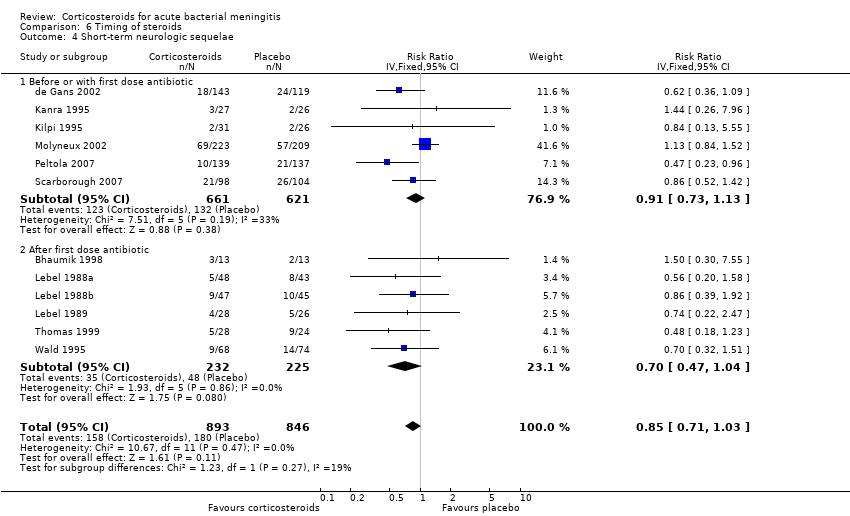
Comparison 6 Timing of steroids, Outcome 4 Short‐term neurologic sequelae.

Comparison 7 Study quality, Outcome 1 Mortality.

Comparison 7 Study quality, Outcome 2 Severe hearing loss.
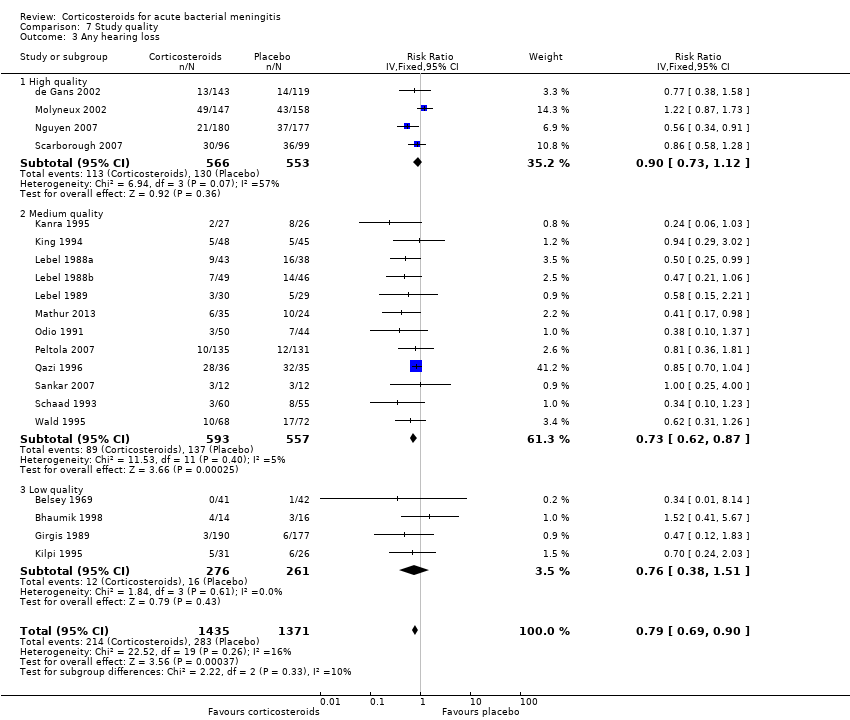
Comparison 7 Study quality, Outcome 3 Any hearing loss.

Comparison 7 Study quality, Outcome 4 Short‐term neurological sequelae.

Comparison 8 Sensitivity analysis ‐ worst‐case scenario, Outcome 1 Severe hearing loss.
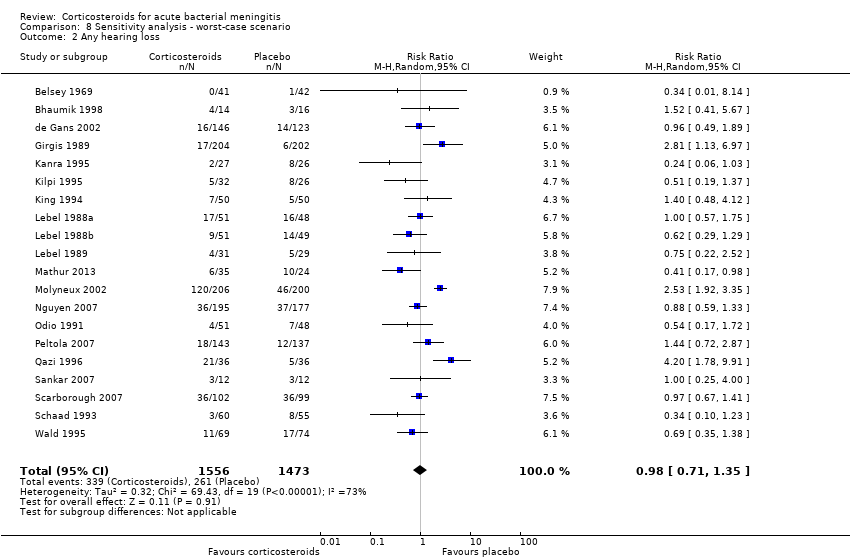
Comparison 8 Sensitivity analysis ‐ worst‐case scenario, Outcome 2 Any hearing loss.

Comparison 8 Sensitivity analysis ‐ worst‐case scenario, Outcome 3 Short‐term neurological sequelae.
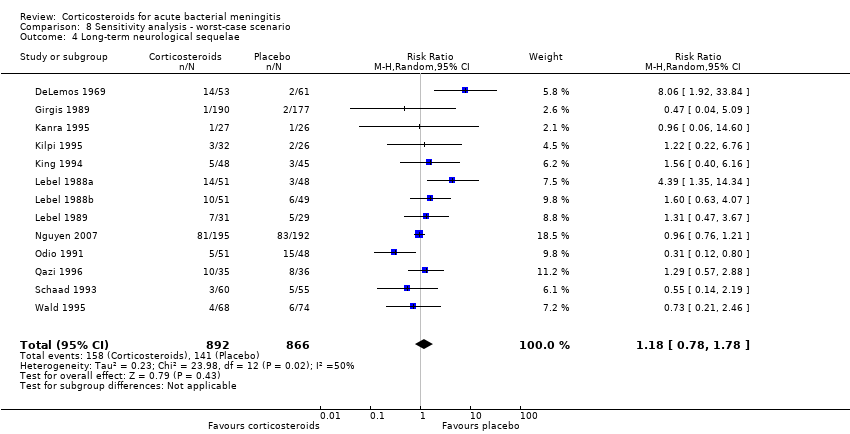
Comparison 8 Sensitivity analysis ‐ worst‐case scenario, Outcome 4 Long‐term neurological sequelae.
| Comparison of corticosteroids against placebo in patients with acute bacterial meningitis | ||||||
| Patient or population: acute bacterial meningitis | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Risk with placebo | Risk with corticosteroids | |||||
| Mortality | Study population | RR 0.90 | 4121 | ⊕⊕⊖⊖ MODERATE 1 | — | |
| 199 per 1000 | 179 per 1000 | |||||
| Moderate | ||||||
| 188 per 1000 | 169 per 1000 | |||||
| Severe hearing loss | Study population | RR 0.67 | 2437 | ⊕⊕⊕⊖ HIGH | — | |
| 93 per 1000 | 62 per 1000 | |||||
| Moderate | ||||||
| 40 per 1000 | 27 per 1000 | |||||
| Any hearing loss | Study population | RR 0.74 | 2785 | ⊕⊕⊕⊖ HIGH | — | |
| 190 per 1000 | 141 per 1000 | |||||
| Moderate | ||||||
| 233 per 1000 | 173 per 1000 | |||||
| Short‐term neurological sequelae | Study population | RR 0.83 | 1756 | ⊕⊕⊕⊖ HIGH | — | |
| 216 per 1000 | 179 per 1000 | |||||
| Moderate | ||||||
| 222 per 1000 | 184 per 1000 | |||||
| Adverse events ‐ recurrent fever | Study population | RR 1.27 | 1723 | ⊕⊕⊖⊖ | — | |
| 221 per 1000 | 281 per 1000 | |||||
| Moderate | ||||||
| 281 per 1000 | 357 per 1000 | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Variable mortality between studies, consistent with differences across the world in meningitis prognosis. 2Different definitions used for recurrent fever makes this imprecise. | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Mortality Show forest plot | 25 | 4121 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.80, 1.01] |
| 2 Severe hearing loss Show forest plot | 17 | 2437 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.51, 0.88] |
| 3 Any hearing loss Show forest plot | 20 | 2785 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.74 [0.63, 0.87] |
| 4 Short‐term neurological sequelae Show forest plot | 13 | 1756 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.83 [0.69, 1.00] |
| 5 Long‐term neurological sequelae Show forest plot | 13 | 1706 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.74, 1.10] |
| 6 Adverse events Show forest plot | 20 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 6.1 Gastrointestinal bleeding | 16 | 2560 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.45 [0.86, 2.45] |
| 6.2 Herpes zoster infection | 6 | 1432 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.09 [0.86, 1.37] |
| 6.3 Persistent fever | 3 | 316 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.29 [0.12, 0.70] |
| 6.4 Recurrent fever | 12 | 1723 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.27 [1.09, 1.47] |
| 6.5 Fungal infection | 1 | 301 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.83 [0.56, 5.96] |
| 6.6 Arthritis | 6 | 618 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.64 [0.27, 1.53] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Mortality Show forest plot | 18 | 2511 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.74, 1.07] |
| 2 Severe hearing loss Show forest plot | 14 | 1524 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.49, 0.91] |
| 3 Any hearing loss Show forest plot | 16 | 1961 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.73 [0.61, 0.86] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Mortality Show forest plot | 7 | 1517 | Risk Ratio (M‐H, Random, 95% CI) | 0.74 [0.53, 1.05] |
| 2 Any hearing loss Show forest plot | 4 | 844 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.74 [0.56, 0.98] |
| 3 Short‐term neurological sequelae Show forest plot | 4 | 542 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.72 [0.51, 1.01] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Mortality Show forest plot | 18 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 Haemophilus influenzae | 11 | 825 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.76 [0.53, 1.09] |
| 1.2 Streptococcus pneumoniae | 17 | 1132 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.84 [0.72, 0.98] |
| 1.3 Neisseria meningitidis | 13 | 618 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.71 [0.35, 1.46] |
| 2 Severe hearing loss in children ‐ non‐Haemophilus influenzae species Show forest plot | 13 | 860 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.65, 1.39] |
| 3 Severe hearing loss in children ‐ Haemophilus influenzae Show forest plot | 10 | 756 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.34 [0.20, 0.59] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Mortality ‐ all patients Show forest plot | 25 | 4121 | Risk Ratio (IV, Random, 95% CI) | 0.88 [0.75, 1.03] |
| 1.1 Low‐income countries | 9 | 1873 | Risk Ratio (IV, Random, 95% CI) | 0.87 [0.67, 1.15] |
| 1.2 High‐income countries | 16 | 2248 | Risk Ratio (IV, Random, 95% CI) | 0.81 [0.63, 1.05] |
| 2 Severe hearing loss ‐ all patients Show forest plot | 17 | 2445 | Risk Ratio (IV, Fixed, 95% CI) | 0.74 [0.58, 0.94] |
| 2.1 Low‐income countries | 5 | 944 | Risk Ratio (IV, Fixed, 95% CI) | 0.99 [0.72, 1.38] |
| 2.2 High‐income countries | 12 | 1501 | Risk Ratio (IV, Fixed, 95% CI) | 0.51 [0.35, 0.73] |
| 3 Any hearing loss Show forest plot | 20 | 2805 | Risk Ratio (IV, Fixed, 95% CI) | 0.79 [0.69, 0.89] |
| 3.1 Low‐income countries | 7 | 1051 | Risk Ratio (IV, Fixed, 95% CI) | 0.89 [0.76, 1.04] |
| 3.2 High‐income countries | 13 | 1754 | Risk Ratio (IV, Fixed, 95% CI) | 0.58 [0.45, 0.73] |
| 4 Short‐term neurological sequelae ‐ all patients Show forest plot | 14 | 1814 | Risk Ratio (IV, Fixed, 95% CI) | 0.84 [0.70, 1.02] |
| 4.1 Low‐income countries | 5 | 735 | Risk Ratio (IV, Fixed, 95% CI) | 1.03 [0.81, 1.31] |
| 4.2 High‐income countries | 9 | 1079 | Risk Ratio (IV, Fixed, 95% CI) | 0.64 [0.48, 0.85] |
| 5 Mortality ‐ children Show forest plot | 17 | 2486 | Risk Ratio (IV, Fixed, 95% CI) | 0.92 [0.77, 1.11] |
| 5.1 Low‐income countries | 5 | 1119 | Risk Ratio (IV, Fixed, 95% CI) | 0.91 [0.75, 1.12] |
| 5.2 High‐income countries | 12 | 1367 | Risk Ratio (IV, Fixed, 95% CI) | 0.96 [0.61, 1.50] |
| 6 Severe hearing loss ‐ children Show forest plot | 14 | 1531 | Risk Ratio (IV, Fixed, 95% CI) | 0.74 [0.56, 0.98] |
| 6.1 Low‐income countries | 3 | 387 | Risk Ratio (IV, Fixed, 95% CI) | 1.00 [0.69, 1.47] |
| 6.2 High‐income countries | 11 | 1144 | Risk Ratio (IV, Fixed, 95% CI) | 0.52 [0.35, 0.78] |
| 7 Short‐term neurological sequelae ‐ children Show forest plot | 10 | 1271 | Risk Ratio (IV, Fixed, 95% CI) | 0.90 [0.72, 1.13] |
| 7.1 Low‐income countries | 3 | 506 | Risk Ratio (IV, Fixed, 95% CI) | 1.08 [0.81, 1.43] |
| 7.2 High‐income countries | 7 | 765 | Risk Ratio (IV, Fixed, 95% CI) | 0.67 [0.46, 0.97] |
| 8 Severe hearing loss in children due to non‐Haemophilus influenzae species Show forest plot | 13 | 862 | Risk Ratio (IV, Fixed, 95% CI) | 0.97 [0.66, 1.42] |
| 8.1 Low‐income countries | 2 | 297 | Risk Ratio (IV, Fixed, 95% CI) | 1.20 [0.72, 2.00] |
| 8.2 High‐income countries | 11 | 565 | Risk Ratio (IV, Fixed, 95% CI) | 0.73 [0.41, 1.31] |
| 9 Mortality ‐ adults Show forest plot | 7 | 1517 | Risk Ratio (IV, Fixed, 95% CI) | 0.95 [0.82, 1.10] |
| 9.1 Low‐income countries | 3 | 636 | Risk Ratio (IV, Fixed, 95% CI) | 1.02 [0.86, 1.20] |
| 9.2 High‐income countries | 4 | 881 | Risk Ratio (IV, Fixed, 95% CI) | 0.76 [0.56, 1.04] |
| 10 Any hearing loss adults Show forest plot | 4 | 844 | Odds Ratio (IV, Fixed, 95% CI) | 0.68 [0.47, 0.98] |
| 10.1 Low‐income countries | 2 | 225 | Odds Ratio (IV, Fixed, 95% CI) | 0.87 [0.49, 1.52] |
| 10.2 High‐income countries | 2 | 619 | Odds Ratio (IV, Fixed, 95% CI) | 0.58 [0.36, 0.92] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Mortality Show forest plot | 22 | 3940 | Risk Ratio (IV, Random, 95% CI) | 0.87 [0.73, 1.05] |
| 1.1 Before or with first dose antibiotic | 13 | 3143 | Risk Ratio (IV, Random, 95% CI) | 0.87 [0.69, 1.09] |
| 1.2 After first dose antibiotic | 9 | 797 | Risk Ratio (IV, Random, 95% CI) | 0.83 [0.55, 1.26] |
| 2 Severe hearing loss Show forest plot | 16 | 2300 | Risk Ratio (IV, Fixed, 95% CI) | 0.82 [0.64, 1.06] |
| 2.1 Before or with first dose antibiotic | 10 | 1866 | Risk Ratio (IV, Fixed, 95% CI) | 0.81 [0.62, 1.07] |
| 2.2 After first dose antibiotic | 6 | 434 | Risk Ratio (IV, Fixed, 95% CI) | 0.89 [0.47, 1.68] |
| 3 Any hearing loss Show forest plot | 18 | 2754 | Risk Ratio (IV, Fixed, 95% CI) | 0.78 [0.68, 0.88] |
| 3.1 Before or with antibiotics | 12 | 2257 | Risk Ratio (IV, Fixed, 95% CI) | 0.80 [0.70, 0.92] |
| 3.2 After first dose of antibiotics | 6 | 497 | Risk Ratio (IV, Fixed, 95% CI) | 0.62 [0.43, 0.89] |
| 4 Short‐term neurologic sequelae Show forest plot | 12 | 1739 | Risk Ratio (IV, Fixed, 95% CI) | 0.85 [0.71, 1.03] |
| 4.1 Before or with first dose antibiotic | 6 | 1282 | Risk Ratio (IV, Fixed, 95% CI) | 0.91 [0.73, 1.13] |
| 4.2 After first dose antibiotic | 6 | 457 | Risk Ratio (IV, Fixed, 95% CI) | 0.70 [0.47, 1.04] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Mortality Show forest plot | 25 | 4121 | Risk Ratio (IV, Fixed, 95% CI) | 0.95 [0.85, 1.06] |
| 1.1 High quality | 4 | 1793 | Risk Ratio (IV, Fixed, 95% CI) | 1.00 [0.88, 1.14] |
| 1.2 Medium quality | 14 | 1477 | Risk Ratio (IV, Fixed, 95% CI) | 0.81 [0.57, 1.17] |
| 1.3 Low quality | 7 | 851 | Risk Ratio (IV, Fixed, 95% CI) | 0.79 [0.60, 1.04] |
| 2 Severe hearing loss Show forest plot | 17 | 2442 | Risk Ratio (IV, Fixed, 95% CI) | 0.72 [0.55, 0.95] |
| 2.1 High quality | 3 | 857 | Risk Ratio (IV, Fixed, 95% CI) | 0.99 [0.69, 1.41] |
| 2.2 Medium quality | 10 | 1051 | Risk Ratio (IV, Fixed, 95% CI) | 0.47 [0.29, 0.75] |
| 2.3 Low quality | 4 | 534 | Risk Ratio (IV, Fixed, 95% CI) | 0.50 [0.20, 1.29] |
| 3 Any hearing loss Show forest plot | 20 | 2806 | Risk Ratio (IV, Fixed, 95% CI) | 0.79 [0.69, 0.90] |
| 3.1 High quality | 4 | 1119 | Risk Ratio (IV, Fixed, 95% CI) | 0.90 [0.73, 1.12] |
| 3.2 Medium quality | 12 | 1150 | Risk Ratio (IV, Fixed, 95% CI) | 0.73 [0.62, 0.87] |
| 3.3 Low quality | 4 | 537 | Risk Ratio (IV, Fixed, 95% CI) | 0.76 [0.38, 1.51] |
| 4 Short‐term neurological sequelae Show forest plot | 13 | 1756 | Risk Ratio (IV, Fixed, 95% CI) | 0.85 [0.70, 1.03] |
| 4.1 High quality | 3 | 896 | Risk Ratio (IV, Fixed, 95% CI) | 0.97 [0.77, 1.23] |
| 4.2 Medium quality | 8 | 784 | Risk Ratio (IV, Fixed, 95% CI) | 0.63 [0.45, 0.89] |
| 4.3 Low quality | 2 | 76 | Risk Ratio (IV, Fixed, 95% CI) | 0.83 [0.35, 1.95] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Severe hearing loss Show forest plot | 17 | 2694 | Risk Ratio (M‐H, Random, 95% CI) | 1.25 [0.81, 1.93] |
| 2 Any hearing loss Show forest plot | 20 | 3029 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.71, 1.35] |
| 3 Short‐term neurological sequelae Show forest plot | 13 | 1850 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.82, 1.18] |
| 4 Long‐term neurological sequelae Show forest plot | 13 | 1758 | Risk Ratio (M‐H, Random, 95% CI) | 1.18 [0.78, 1.78] |

