Laparoscopic fundoplication surgery versus medical management for gastro‐oesophageal reflux disease (GORD) in adults
Information
- DOI:
- https://doi.org/10.1002/14651858.CD003243.pub3Copy DOI
- Database:
-
- Cochrane Database of Systematic Reviews
- Version published:
-
- 05 November 2015see what's new
- Type:
-
- Intervention
- Stage:
-
- Review
- Cochrane Editorial Group:
-
Cochrane Gut Group
- Copyright:
-
- Copyright © 2015 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Article metrics
Altmetric:
Cited by:
Authors
Contributions of authors
Conceiving the review: this is an update of the previous review (Wileman 2010).
Designing the review: this is an update of the previous review (Wileman 2010).
Coordinating the review: SG, KG
Designing search strategies: UGPD
Writing the review: SG, KG
Providing general advice on the review: Not applicable
Securing funding for the review: KG
Performing previous work that was the foundation of the current study: this is an update of the previous review (Wileman 2010).
Sources of support
Internal sources
-
University of Aberdeen. Health Services Research Unit, UK.
-
Department of Public Health, University of Aberdeen, UK.
External sources
-
Chief Scientist Office of the Scottish Government Health Directorates, UK.
-
NHS R&D HTA Programme, UK.
This project was supported by the National Institute for Health Research via Cochrane Programme Grant funding to the CHBG and UGPD Groups. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, NHS or the Department of Health.
Declarations of interest
SG: none known
KG: none known
Acknowledgements
We would like to thank Karin Dearness, Jan Lilleyman, and Cathy Bennett for their help and encouragement with this review. We gratefully acknowledge the work of the review team who were responsible for the original review concept, and wrote earlier published versions of the review. In these earlier versions, Samantha Wileman and Julie Bruce entered the data and wrote the text of the full review. Zygmunt Krukowski provided clinical expertise and Adrian Grant provided review expertise. All authors commented on the review.
Version history
| Published | Title | Stage | Authors | Version |
| 2015 Nov 05 | Laparoscopic fundoplication surgery versus medical management for gastro‐oesophageal reflux disease (GORD) in adults | Review | Sushil K Garg, Kurinchi Selvan Gurusamy | |
| 2010 Mar 17 | Medical versus surgical management for gastro‐oesophageal reflux disease (GORD) in adults | Review | Samantha M Wileman, Sharon McCann, Adrian M Grant, Zygmunt H Krukowski, Julie Bruce | |
| 2001 Jul 23 | Laparoscopic fundoplication versus medical management for gastro‐oesphageal reflux disease (GORD) in adults | Protocol | Samantha M Wileman, Sharon McLeer, Marion K Campbell, Ashley Mowat, Zygmunt Krukowski, Adrian Grant, Julie Bruce, Sharon McCann | |
Differences between protocol and review
The protocol for this review included the comparison of alternative surgical laparoscopic approaches (total versus partial fundoplication) as a secondary objective. A comparison of the alternative surgical approaches for the management of GORD is being addressed by a separate systematic review (MacKay 2010). The risk of bias section has been updated from the protocol and uses the assessment criteria recommended in the updated version of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011a).
Differences between previous version and current version
-
The review has been updated according to the updated version of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011a).
-
The following outcomes were moved to secondary outcomes: heartburn, reflux, and dysphagia.
-
Serious adverse events have been included as primary outcome.
-
Adverse events have been include as secondary outcome.
Keywords
MeSH
Medical Subject Headings (MeSH) Keywords
Medical Subject Headings Check Words
Adult; Humans;
PICOs

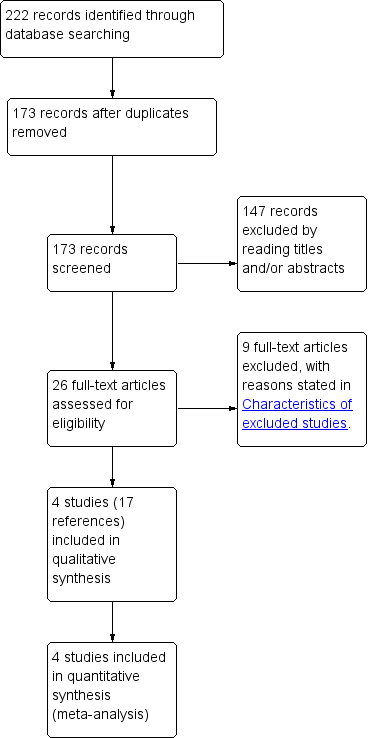
Methodological quality graph: review authors' judgements about each methodological quality item presented as percentages across all included studies.

Methodological quality summary: review authors' judgements about each methodological quality item for each included study.
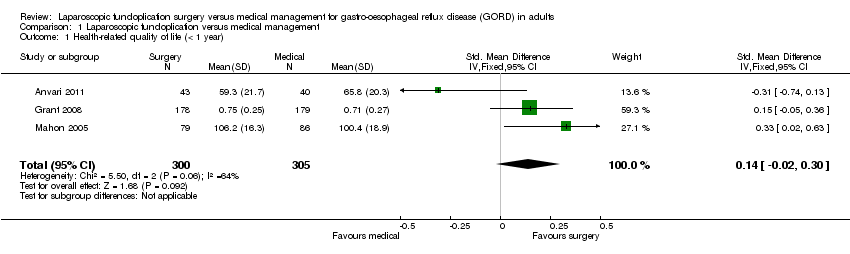
Comparison 1 Laparoscopic fundoplication versus medical management, Outcome 1 Health‐related quality of life (< 1 year).
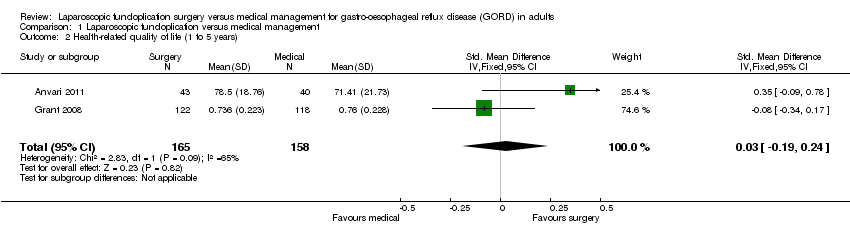
Comparison 1 Laparoscopic fundoplication versus medical management, Outcome 2 Health‐related quality of life (1 to 5 years).

Comparison 1 Laparoscopic fundoplication versus medical management, Outcome 3 GORD‐specific quality of life (< 1 year).
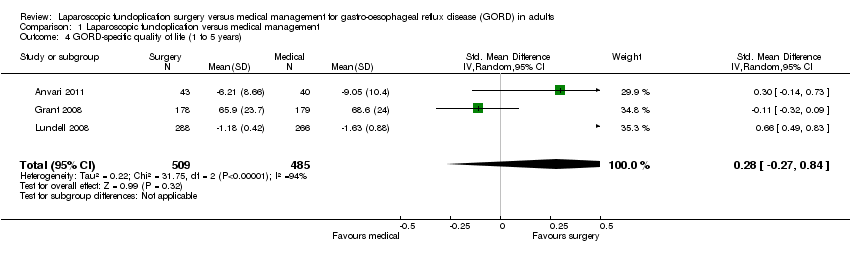
Comparison 1 Laparoscopic fundoplication versus medical management, Outcome 4 GORD‐specific quality of life (1 to 5 years).

Comparison 1 Laparoscopic fundoplication versus medical management, Outcome 5 Serious adverse events.

Comparison 1 Laparoscopic fundoplication versus medical management, Outcome 6 Adverse events.

Comparison 1 Laparoscopic fundoplication versus medical management, Outcome 7 Dysphagia (< 1 year).
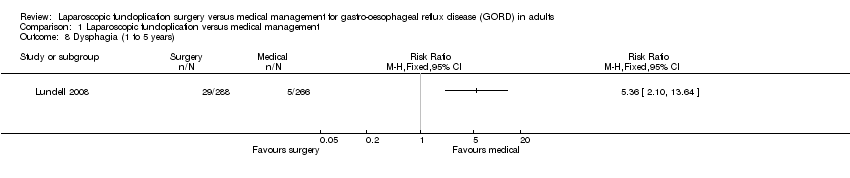
Comparison 1 Laparoscopic fundoplication versus medical management, Outcome 8 Dysphagia (1 to 5 years).

Comparison 1 Laparoscopic fundoplication versus medical management, Outcome 9 Dysphagia (5 years or more).
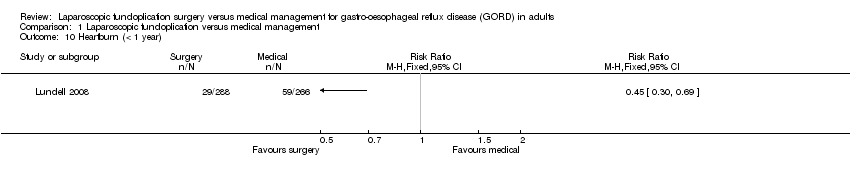
Comparison 1 Laparoscopic fundoplication versus medical management, Outcome 10 Heartburn (< 1 year).
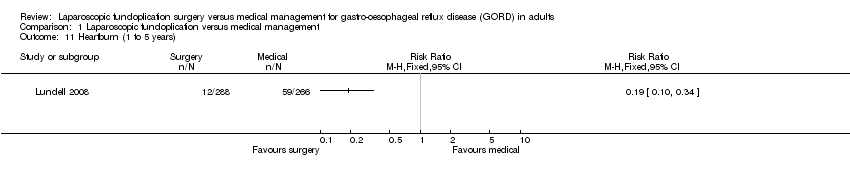
Comparison 1 Laparoscopic fundoplication versus medical management, Outcome 11 Heartburn (1 to 5 years).

Comparison 1 Laparoscopic fundoplication versus medical management, Outcome 12 Heartburn (5 years or more).
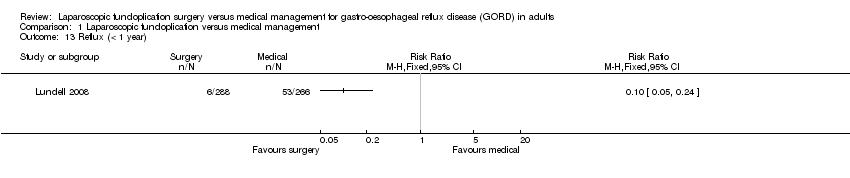
Comparison 1 Laparoscopic fundoplication versus medical management, Outcome 13 Reflux (< 1 year).

Comparison 1 Laparoscopic fundoplication versus medical management, Outcome 14 Reflux (1 to 5 years).
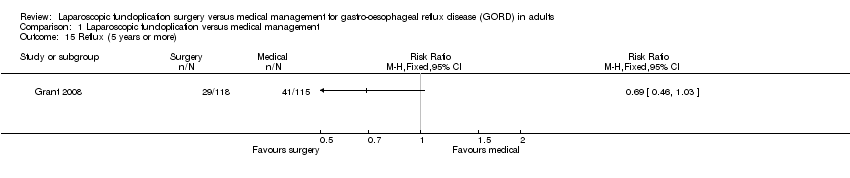
Comparison 1 Laparoscopic fundoplication versus medical management, Outcome 15 Reflux (5 years or more).
| Laparoscopic fundoplication versus medical management for gastro‐oesophageal reflux disease (GORD) in adults | ||||||
| Patient or population: Patients with gastro‐oesophageal reflux disease (GORD) in adults Control: Medical management | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Medical management | Laparoscopic fundoplication | |||||
| Health‐related quality of life | ||||||
| (< 1 year) | The mean health‐related quality of life (< 1 year) in the intervention groups was | 605 | ⊕⊝⊝⊝ | SMD 0.14 (‐0.02 to 0.3) | ||
| (1 to 5 years) | The mean health‐related quality of life (1 to 5 years) in the intervention groups was | 323 | ⊕⊝⊝⊝ | SMD 0.03 (‐0.19 to 0.24) | ||
| GORD‐specific quality of life | ||||||
| (< 1 year) | The mean GORD‐specific quality of life (< 1 year) in the intervention groups was | 1160 | ⊕⊕⊝⊝ | SMD 0.58 (0.46 to 0.7) | ||
| (1 to 5 years) | The mean GORD‐specific quality of life (1 to 5 years) in the intervention groups was | 994 | ⊕⊝⊝⊝ | SMD 0.28 (‐0.27 to 0.84) | ||
| Adverse events | ||||||
| Serious adverse events | 124 per 1000 | 181 per 1000 | RR 1.46 | 637 | ⊕⊝⊝⊝ | |
| Adverse events | 10 per 1000 | 140 per 1000 | RR 13.98 | 83 | ⊕⊝⊝⊝ | |
| Dysphagia | ||||||
| (< 1 year) | 36 per 1000 | 129 per 1000 | RR 3.58 | 637 | ⊕⊝⊝⊝ | |
| (1 to 5 years) | 19 per 1000 | 101 per 1000 | RR 5.36 | 554 | ⊕⊝⊝⊝ | |
| (5 years or more) | 255 per 1000 | 229 per 1000 | RR 0.9 | 228 | ⊕⊝⊝⊝ | |
| Heartburn | ||||||
| (< 1 year) | 222 per 1000 | 100 per 1000 | RR 0.45 | 554 | ⊕⊝⊝⊝ | |
| (1 to 5 years) | 222 per 1000 | 42 per 1000 | RR 0.19 | 554 | ⊕⊝⊝⊝ | |
| (5 years or more) | 736 per 1000 | 412 per 1000 | RR 0.56 | 217 | ⊕⊝⊝⊝ | |
| Reflux | ||||||
| (< 1 year) | 199 per 1000 | 20 per 1000 | RR 0.1 | 554 | ⊕⊝⊝⊝ | |
| (1 to 5 years) | 139 per 1000 | 21 per 1000 | RR 0.15 | 554 | ⊕⊝⊝⊝ | |
| (5 years or more) | 357 per 1000 | 246 per 1000 | RR 0.69 | 233 | ⊕⊝⊝⊝ | |
| Long‐term overall health‐related quality of life and long‐term GORD‐specific quality of life were not reported in any of the trials. | ||||||
| *The basis for the assumed risk was the mean control group risk across studies for all outcomes other than adverse events. For control group risk, 1% was used as the control group risk since there were no adverse events in the control group in the only trial that reported this outcome (Anvari 2011). The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 The trial(s) was/were at high risk of bias. | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Health‐related quality of life (< 1 year) Show forest plot | 3 | 605 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.14 [‐0.02, 0.30] |
| 2 Health‐related quality of life (1 to 5 years) Show forest plot | 2 | 323 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.03 [‐0.19, 0.24] |
| 3 GORD‐specific quality of life (< 1 year) Show forest plot | 4 | 1160 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.58 [0.46, 0.70] |
| 4 GORD‐specific quality of life (1 to 5 years) Show forest plot | 3 | 994 | Std. Mean Difference (IV, Random, 95% CI) | 0.28 [‐0.27, 0.84] |
| 5 Serious adverse events Show forest plot | 2 | 637 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.46 [1.01, 2.11] |
| 6 Adverse events Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 7 Dysphagia (< 1 year) Show forest plot | 2 | 637 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.58 [1.91, 6.71] |
| 8 Dysphagia (1 to 5 years) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 9 Dysphagia (5 years or more) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 10 Heartburn (< 1 year) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 11 Heartburn (1 to 5 years) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 12 Heartburn (5 years or more) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 13 Reflux (< 1 year) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 14 Reflux (1 to 5 years) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 15 Reflux (5 years or more) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |