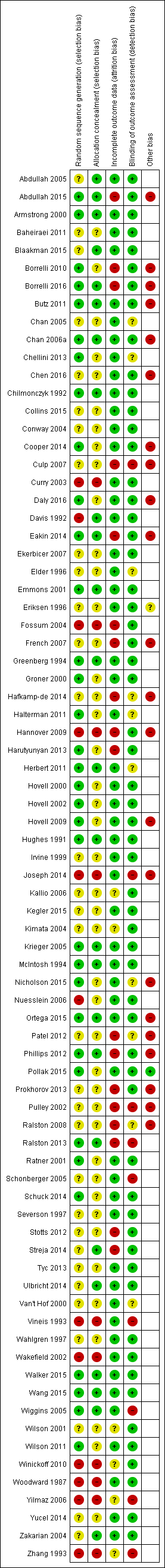
| Abdullah 2005 | Counselling strategies based on the stages of change component of Prochaska's transtheoretical model. Results as N (%), intervention N = 444, control N = 459. Biochemically validated quit rate: Intervention 47 (10.6) Control 21 (4.5)
Had not quit but had reduced intake: Intervention 145 (32.6) Control 83 (18.1)
Stopped smoking for at least 24 hours: Intervention 145 (32.7) Control 136 (29.7)
Complete restriction: Intervention 113 (24.6) Control 151 (34.1)
Partial restriction: Intervention 278 (62.7) Control 259 (56.4) No measure of children's exposure or absorption via cotinine. |
| Abdullah 2015 | ETS exposure: 6 month follow‐up: 1) higher proportion of the intervention (62%) than the comparison (45%) group households adopted complete smoking restrictions at home (P = 0.022); 2) higher proportion of the intervention (38%) than the comparison (17%) group households did not smoke at home at all (P = 0.002); 3) total exposure from household members inside home in the past 7 days (measured by mean number of cigarettes smoked per week in front of the child by household members) was lower in the intervention (3.29) than the comparison (7.41) group (P = 0.021); 4) total exposure from all smokers indoors and outdoors in the past 7 days (measured by mean number of cigarettes smoked per week in front of the child) was significantly lower among children in the intervention (15.2) than the comparison (25.7) group (P = 0.005); 5) Comparison group: mean cotinine levels increased from baseline to 2 months and maximum at 6 months, with no statistically significant difference in time effects. Intervention group: mean cotinine levels increased at 2 months from baseline level but decreased again at 6 months, with statistically significant difference in time effects only from 2 to 6 months (P < 0.05); 6) No significant difference in allowing others to smoke around the child (P = 0.908). Air quality: At 6 month follow‐up: 1) mean number of cigarettes smoked daily was significantly lower in the intervention (11.02) than the comparison (13.6) group (P = 0.021); 2) significantly more participants in the intervention (48%) than the comparison (28%) group reduced the number of cigarettes smoked at home daily (P = 0.006) Child health: Perceived overall respiratory health of the child improved significantly in the intervention (35%) than the comparison (20%) group (P = 0.024). There were no significant differences in the reports respiratory symptoms of the child (P = 0.258). |
| Armstrong 2000 | Targeted disadvantaged mothers. Smoking in house around infant (maternal self report verified by researcher observation during home visit)
Intervention 8.6% v Control 23.8% (P < 0.05). included education about smoking near infants as a Sudden Infant Death Syndrome (SIDS) prevention strategy in a post‐natal nurse home visiting programme aimed to improve the quality of maternal‐child attachment, maternal health and child health parameters. At four months the intervention group had significantly more completed immunizations than the controls, although both groups had high immunization rates. At 12 months there was no statistically significant difference between the groups for immunization status. There was also no significant difference at four or 12 months for rates of utilisation of community services. |
| Baheiraei 2011 | Motivational Interviewing used. In 3 months geometric mean urinary cotinine: intervention decreased from 48.72 ng/mg to 28.68 ng/mg, control decreased from 40.43 to 36.32 ng/mg, differences between two groups statistically significant using one tailed t‐test. Greater decrease in total daily cigarette consumption in the presence of child in the intervention group than the control group (statistically significant with one tailed t‐test). Intervention median cigarettes at 3 month 0 (IQR 1 to 2.71), control 1 (IQR 0 to 3.21). Home smoking bans: intervention 15% to 33.3% (statistically significant increase), control 11.5% to 19.5% (not statistically significant increase), differences between two groups statistically significant using a one tailed t‐test. Car smoking bans in the intervention group increased from 4% to 8%, and didn't change in the control group. This was not a statistically significant difference. |
| Blaakman 2015 | ETS exposure: 5 months after discharge from NICY, caregivers in treatment group were sig more likely to report a home smoking ban than the comparison group (96% vs 84%; P = 0.03), and less likely to report routine infant contact with a smoker (40% vs 58%, P = 0.03). Differences in reported home bans (92% vs 83%, P = 0.14) and routine infant contact with smokers (44% vs 53%, P = 0.33) were no longer significantly different at study end (8 months after NICU discharge). No difference in car smoking bans or total smoking bans at any time. 8 months after NICU discharge, infants in intervention group had lower salivary cotinine and a greater decrease in salivary cotinine since baseline than infants in the comparison group. Air quality: Overall, very few caregivers quit smoking, which didn't differ between groups after intervention or at study end. Of the 29 total caregivers who reported smoking 5 months after NICU discharge, caregivers in the intervention group reported significantly higher confidence to quit than smoking caregivers in the comparison group at the 5‐month survey, but not at study end. No significant difference between groups in caregiver motivation to quit. Child health: No significant differences between groups in respiratory symptoms or use of health care services. |
| Borrelli 2010 | Latino families targeted. Used two interventions with different theoretical frameworks: one intervention used motivational interviewing, whilst the other intervention used the social cognitive theory. At 3 months 61.7% home monitors were returned and 98.8% were in good condition, whilst 60.9% child monitors returned and 100% in good condition. Household air nicotine significantly decreased from pretreatment to the 3 month follow‐up in the BAM condition, (baseline M = 1.07, SE 0.19, and 3‐month M = 0.28, SE 0.11, P = 0.01), whereas the decrease observed in the PAM condition was not statistically significant. Changes in secondhand smoke concentrations as assessed by the child monitors were not statistically significant. Continuous abstinence at 3 months 12.3% BAM group and 19.1% PAM group (OR 1.68, 95% CI 0.64 to 4.37). The child's level of functional morbidity due to asthma decreased significantly (P < 0.001) in both groups over time. Secondhand smoke exposure as measured by monitors directly on the child did not show a significant decrease in either group. |
| Borrelli 2016 | ETS exposure: SELF‐REPORTED: 1) PAM had significant reductions over time on one SHS exp variable, while HC had reductions on 4 of the 5 SHS exp variables, with a significant group x time interaction. 2) Enhanced PAM showed sig within‐group decreases in SHS exp over time on all 5 variables and HC showed sig within group decreases in SHS exp over time on 4 of the 5. Sig group x time interaction, such that enhanced PAM showed greater decreases in SHS exp over time versus HC for 3 of the 5 SHS exp variables; 3) Comparing PAM with enhanced PAM, no significant group x time interaction. OBJECTIVE: 1) No significant differences in levels of SHS exp at baseline; 2) At follow‐up, there were significant differences in detectable levels of SHS exp in the HOME monitors (PAM 92.1% vs HC 97.2%, P = 0.04), but NOT the CHILD monitors (PAM 91.4% vs HC 95.6%); 3) At follow up, no significant between‐group differences in detectable levels of SHS exp in either the home or child monitors, when comparing PAM with enhanced PAM. Air quality: 1) PAM more than 2x as likely to achieve 7‐day and 30‐day point‐prevalence abstinence than HC (statistically significant); 2) Enhanced PAM more than 2x as likely to achieve 7‐day PPA, 3x as likely to achieve 30‐day PPA than HCs, and 5x as likely to be continuously abstinent than HCs (statistically significant); 3) At 4‐months, enhanced PAm were more than 2x as likely to achieve 30‐day PPA versus PAM (significant). Child health: 1) At 6‐months, enhanced PAM had significantly lower child asthma hospitalisations than PAM; 2) At 2, 4 and 6 month follow‐up, enhanced PAM had sig lower missed school days due to asthma than PAM; 3) Odds of at least 1 day with asthma symptoms was sig lower in enhanced PAM than PAM at 6‐months; 3) No sig diff between groups in changes in asthma functional morbidity. |
| Butz 2011 | Low income households targeted. No statistically significant differences in urinary cotinine between baseline and follow up by group After combining the air cleaner groups, children assigned to those groups had a significant increase in symptom‐free days (SFDs) during the past 2 weeks (1.36 SFDs) compared with 0.24 SFDs for control group children from baseline to follow‐up No statistically significant differences In air nicotine at baseline and follow‐up by group Comparison of the combined air cleaner groups and the control group indicated that the combined air cleaner groups had significant mean differences in PM2.5 and PM2.5‐10 levels from baseline to follow‐up (mean differences for PM2.5: control, 3.5 [SD, 20.0]; combined air cleaner groups, ‐18.0 [SD, 33.2; P 0.001]; and for PM2.5‐10: control, 2.4 [SD, 20.8]; combined air cleaner groups, ‐9.6 [SD, 16.0; P = 0.009]) |
| Chan 2005 | Motivational Interviewing used. No statistically significant evidence of effect.
Quit rate at 1 month post intervention: Intervention 7.5% [95%CI: 0 to 21] v 2.5% [95% CI: 0 to 7] control NS
Reduced smoking consumption by half (self report): Intervention: 15% Control: 10% NS
Reported quit attempts in last 30 days: Intervention 20% Control 7.5% NS
Moved up the stage of readiness to quit: Intervention 17.5% Control 10% NS |
| Chan 2006a | Fishbein's theory of reasoned action and Ajzen's theory of planned behaviour used in the development of the educational intervention. Three most frequently reported actions taken by the mother to protect the child from passive smoking at home: opening the windows (N = 641, 43.9%), asking the father not to smoke near the child (N = 608, 41.6%), and moving the child away from the smoke (N = 482, 33%).
Moved the children away when they were exposed to the fathers’ smoke at home at 3‐month follow up (78.4% vs. 71.1%; P = 0.01) NS at 6 and 12 months.
Number of smokers (excluding the father) living with the child at 12 month follow up (11% vs 13% P = 0.049)
Smokers who smoked at home (Excluding Child’s Father), at 12‐month follow up (92% vs 93% NS)
Child’s ETS exposure at home by any smoker 3 months Intervention 37% vs Control 42% (P = 0.02) 6mths 51% vs 53% P = 0.48 12 mths 52% vs 58% P = 0.03 |
| Chellini 2013 | Post‐intervention smoke free homes were not significantly different between groups (increased in both): percentage increase in intervention group 12.7% and control group 11.1% (OR 1.04, 95 CI 0.47 to 2.28) . For cars: intervention group 18.2%, and control group 12.0% (OR 1.47 95 CI 0.69 to 3.11. Of the N = 131 smokers there was no significant difference in change of smoking habits. between intervention and control group (7% total stopped smoking, 5% stopped smoking indoors and n = 9 stopped smoking in the car). |
| Chen 2016 | ETS exposure: After intervention, the percentage of children with a urine cotinine concentration higher than 6ng/ml (indicating exposure) in the intervention group was significantly lower than that in the control group at both 8 weeks (P < 0.0001) and 6 months (P = 0.007). Air quality: Significantly less smoking in presence of children in intervention group at both 8 weeks and 6 months. Child health: N/A |
| Chilmonczyk 1992 | No evidence of effect.
Intervention: 27/52 provided follow‐up urine. Control 29/51 provided follow‐up urine. Mean log urinary cotinine difference x100: Intervention group 2.05, control 2.17. P = 0.26 |
| Collins 2015 | ETS exposure: Associated with lower child urine cotinine compared with the control group. Air quality: Twenty (18.3%) of intervention group mothers and three (1.9%) of the control group mothers had bioverified quit status) P < 0.01). Child health: N/A |
| Conway 2004 | Participants (Latino families) for this study were recruited through advertising at community organisations and venues. Social learning model used. No significant effect.
Hair nicotine (log ng/mg) 3mth Intervention 0.28, Control 0.32;12 mth Intervention 0.23, Control0.23 NS
Hair cotinine (log ng/mg) 3mth Intervention 0.04, Control 0.04;12 mth Intervention 0.02, Control 0.04 NS
Parent report reduction: % confirmed reducers 3mth Intervention 52%, Control 46%; 12mth Intervention 61%, Control 56% NS |
| Cooper 2014 | ETS exposure: N/A Air quality: After delivery, there were no statistically significant differences in cessation; self‐reported abstinence at 2 years was 2.9% in the NRT group and 1.7% in the placebo group. However, few participants reported using a full 8‐week course of NRT; 7.2% in NRT group and 2.8% in placebo group used their trial medications for over 1 month. Child health: At birth, significantly more Caesarian births occurred in the NRT group (20.7% vs 15.3%); at 2 years, significantly more infants in the NRT group (72.6% vs 65.5%) survived with 'no impairment'; 3) However, no sig difference between groups in infants' reported respiratory problems. |
| Culp 2007 | At 12 months the intervention group smokers smoked mean 2.1 fewer than control, which was not statistically significant: intervention 7.28 (s.d. 6.79), control 9.41 (s.d. 7.09) (t(147) = 1.82, P = 0.071). There were no significant differences between groups on number of hospital admissions or emergency room visits. At 12 months, intervention mothers were more likely to make use of health department clinics for well child care as compared to control group (chi square P =0.04) Knowledge of secondhand smoke exposure on child development: at 12 months significantly more intervention (N = 90, 58.1%) than control (N = 51, 47.7%) knew about SHS and impaired brain development, and significantly more intervention (N = 126, 80.6%) than control (N = 77, 72.0%) knew it takes longer to get well. No other significant differences with questions. |
| Curry 2003 | Ethnically diverse low income women targeted. Motivational Interviewing used. Abstinence rates: 3 mth Intervention 7.7% vs Control 3.4%; 12mth Intervention 13.5% vs Control 6.9% ‐ 12 mth difference statistically significant.
Serious attempt to quit at 12 months Adjusted OR 1.53 (95% CI 0.96 to 2.44)
Ever quit for 24h at 12 months Adjusted OR 0.94 (95% CI 0.59 to 1.5)
Prevalent abstinence 3 months Adjusted OR 2.40 (95% CI 0.85 to 7.8) 12 months Adjusted OR 2.77 (95% CI 1.24 to 6.60)
Sustained abstinence (abstinent at 3 and 12 months) Adjusted OR 1.83 (95% CI 0.29 to 14.30) Validation of smoking cessation by carbon monoxide expiration was completed by only a small subsample (13/156 in the intervention group and 5/147 in the control group). |
| Daly 2016 | ETS exposure: At 12 month follow‐up, 13% of all infants were reported to be exposed to SHS; however with urine cotinine validation, 17% overall were exposed. No significant time by group difference detected from baseline to follow‐up for either of the 2 treatment arms when compared with the control group. Air quality: At follow‐up, 47% of all parent/carers reported they were smokers. No significant time by group differences detected comparing either treatment arm with the control group. Child health: N/A |
| Davis 1992 | This study recruited participants through an advertising campaign that invited them to call a telephone smoking cessation assistance counselling service run by the National Cancer Institute in the USA. No evidence of difference between self‐help guides.
Self‐reported quit attempts: Guide 1 121/198 (61%), Guide 2 122/204 (60%), Guide 3 147/229 (64%);
Self‐reported abstinence for last week:
Guide 1 28/198 (14%),
Guide 2 24/204 (12%),
Guide 3 27/229 (12%)
P > 0.05 |
| Eakin 2014 | ETS exposure: Differences in salivary cotinine were not significant. However, among all families who reported a home smoking ban, salivary cotinine and air nicotine levels declined in both groups (P < 0.05). Air quality: Participants in the MI and education group had significantly lower air nicotine levels (0.29 vs 0.40 mg), 17% increase in prevalence of caregiver‐reported home smoking bans, and a 13% decrease in caregiver smokers compared with education‐alone group (all P values < 0.05). Child health: N/A |
| Ekerbicer 2007 | This study from Turkey recruited ETS exposed children from a primary school. Parents of identified children received telephone counselling or a note regarding their child's urinary cotinine result. At 9 months follow‐up: Group one 74/93 students had urinary cotinine levels < 10 ng/ml; group two 69/93 had urinary cotinine < 10 ng/ml. "The proportion of children with urinary cotinine values < 10ng/ml were statistically similar (P > 0.05) in both groups". |
| Elder 1996 | Social learning model used. No evidence of effect on tobacco‐free school policy after 3 years:
Intervention 78% of 56 schools,
Control 75% of 40 schools |
| Emmons 2001 | Motivational Interviewing used. Quit rates: Intervention 7.5%, Control 10.1%, P > 0.05
CPD: no effect
Kitchen and TV room air nicotine measured by passive sampling diffusion monitors at 6 months (log transformed units): Intervention 3.7 & 3.1 fell to 2.6 & 2.3, Control 3.0 & 3.5 changed to 6.9 & 3.5. * P < 0.05, |
| Eriksen 1996 | No evidence of effect.
Quit smoking: Intervention 7/222 (3%) vs Control 1/221 (0.5%);
Stopped indoor smoking 4/222 vs 4/221;
Any positive change 32/222 (14%) vs 34/221 (15%) |
| Fossum 2004 | Social learning model used. Self‐reported smoking (number of cigarettes) 1 month before childbirth: Intervention 13.1 vs Control 10.8 NS; 3 months after childbirth Intervention 12.8 vs Control 8.2 (significant); Past 24 hrs Intervention 11.8 vs Control 7.8 (significant).
Salivary cotinine: Mean for Intervention reduced from 185 ng/ml to 165; mean for Control increased from 245 to 346 ng/ml.
Weak correlation between mother's reported rate of smoking and cotinine levels for both control and intervention groups. |
| French 2007 | Six month follow‐up data Saliva cotinine verified non smoker: intervention (N = 26, 22%), control (N = 9, 10%) ‐ P < 0.025 Self‐reported non‐smoker: intervention (N = 40, 33%), control (N = 21, 22%) ‐ P < 0.10 |
| Greenberg 1994 | Social learning model used. Targeted ETS exposure in infants less than six months of age, and aimed to reduce the incidence of lower respiratory tract illness and the prevalence of respiratory symptoms. For infants of smoking mothers it demonstrated a lower prevalence of persistent symptoms in the intervention group (17.8%) compared with control group (30.9%; risk difference 13.1%; 95% CI: 1.0 to 27.0%). There was no difference in the incidence of illness.
Parents report significant reduction in number of CPD: Intervention 12.5 CPD pre vs 7.7 CPD at 12month follow up, Control 12.3 CPD pre vs 13.3 at follow up P=0.01. Child urinary cotinine does not support this. Baseline mean urinary cotinine/ creatinine (nmol/mmol) Intervention 66 vs Control 51; at follow up Intervention 107 vs 98 Control. P = NS
Prevalence of persistent lower respiratory symptoms Intervention 17.8%, Control 30.9% [difference 13.1%, 95% CI ‐1.0 to 27.0] |
| Groner 2000 | No evidence of effect.
Self‐reported quit rates: Intervention Child Health Group 7/153, Mother's Health Group 4/164, Control 7/162. P = NS
Self‐reported CPD reduced in all groups;
Self‐reported not smoking indoors reduced: Intervention CHG 24, MHG 12, Control 13. P < 0.05 |
| Hafkamp‐de 2014 | ETS exposure: No significant difference in ETS exposure at home between intervention and control groups at age 6 years in the intention to treat analyses (OR 0.82, 95% CI: 0.66, 1.03); though this reached statistical significance in per‐protocol analysis with intervention group having less ETS exposure at age 6 years than the control group (OR 0.71, 95% CI: 0.59, 0.87). No effect modification by sociodemographic characteristics (data not shown). Air quality: N/A Child health: No significant differences between groups in asthma, wheezing frequency, airway inflammation (exhaled NO), or airway resistance (Rint). |
| Halterman 2011 | Motivational Interviewing used. Symptom‐free days/2 wk (difference) 0.96 (95% CI 0.39 to 1.52)
Symptom nights/2 wk (difference) −0.63 (95% CI −1.09 to −0.18)
Days with activity limitation/2 wk (difference) −0.44 (95% CI −0.87 to −0.02)
Days with rescue medication use/2 wk (difference) −1.04 (95% CI −1.51 to −0.56)
Days absent due to asthma/2 wk (difference) −0.22 (95% CI−0.36 to −0.07)
≥1 Visit for acute exacerbation of asthma (RR) 0.55 (95% CI 0.26 to 1.15) |
| Hannover 2009 | Motivational Interviewing used. At 24 months follow‐up Sustained abstinence: intervention (N = 36, 12%, 95% CI 8.8 to16.2), control (N = 39, 11%, 95% CI 8.4 to15.1), no statistically significant difference in proportions (0.7, 95% CI ‐4.2 to 5.8) Four week point prevalence: intervention (N = 72, 24% 95% CI 19.6 to29.2), control (N = 67, 19%, 95% CI 15.6 to23.9), no statically significant difference in proportions (4.7, 95 CI ‐1.7 to 11.1). |
| Harutyunyan 2013 | ETS exposure: Adjusting for baseline hair nicotine concentration, child's age and gender, the follow‐up geometric mean hair nicotine concentration in the intervention group was 17% lower than the control group (P = 0.239). The GM of hair nicotine in the intervention group significantly decreased from 0.30 ng/mg to 0.23 ng/mg (P = 0.024), but not in the control group. Adjusted odds of children's less than daily exposure to SHS at follow‐up was 1.87 times higher in the intervention group than in the control group (P = 0.077). Air quality: According to mothers, 4.5% intervention households and 5.4% control households completely banned indoor smoking at follow‐up. Also 4.5% smokers in the intervention group and 0.9% in the control group have reportedly stopped smoking at follow‐up. Child health: N/A |
| Herbert 2011 | Recruited families to participate in the study through five public health nursing offices, eight daycare centres, and kindergartens on Prince Edward Island. Used a family‐centred assessment and intervention model to empower families to reduce cigarettes smoked in the home. Those identified as having children exposed to ETS were then invited to participate in group counselling sessions. Intervention: decrease from median of 17 to 4.5 cigarettes/day and Control: decrease from 18.5 to 3.5 cigarettes/day. Both decreases statistically significant so did not detect a beneficial effect of the intervention. At 6 months follow‐up intervention participants smoked 0.65 (95% CI ‐5.68 to 6.98) more cigarettes per day compared to control participants |
| Hovell 2000 | Reduction in parent‐reported child exposure to cigarettes in the home and in total. At home reported exposure Intervention baseline 3.9 CPD, follow up 0.52 CPD vs Control 3.51 CPD baseline, 1.20 CPD follow up. The trend for parent‐reported total CPD exposure was similar.
Reports not supported by child urinary cotinine concentrations (ng/ml). Intervention baseline 10.93, follow up 10.47 vs Control baseline 9.43, follow up 17.47; 56% reduction (95% CI 48 to 63). Achieved a reduction in the number of parent‐reported cigarettes smoked in the presence of children per day at 12 months, following a three‐month intensive counselling intervention. There was, however, no change in cigarette smoke absorption as measured by children's urinary cotinine (ng/ml) for the intervention group over the 12 months (with measures collected at 3, 6 and 12 months). Cigarette smoke absorption for the control group increased from 9.4 ng/ml to 17.5 ng/ml over this time period, whereas there was almost no change in the intervention group (10.9 at baseline and 10.5 at 12 months). This increase in absorption observed for children in the control group appears to account for the apparent benefit of the intervention group. However the argument that this is solely due to reduced exposure in the home is uncertain, as the mothers in both the intervention and control groups reported falls in mothers' cigarettes smoked in the presence of the child from 3.9 to 0.5 (intervention) and 3.5 to 1.2 (control) cigarettes per day. In addition, they reported falls in total exposure to any source of cigarettes per day from 7.3 to 1.2 (intervention) and 7.2 to 2.8 (control). As the cotinine indicates a minimal fall for the intervention group and almost a doubling in urinary cotinine for the control group, either the cotinine measurement is unreliable or, more probably, that the parental report of cigarette exposure is not reliable. |
| Hovell 2002 | Latino families targeted. No significant effect.
Decline in reported ETS exposure from (Intervention) 97% to 52% vs (Control) 93% to 69% at end of intervention (month 4).
At follow up month 13, 9 months post‐intervention (Intervention) 52% to 45% and (Control) 69% to 54%.
Average parent‐reported exposure levels declined over the follow‐up period from 0.57 to 0.47 CPD (Intervention) and 1.11 to 0.71 CPD (Control). These results show a difference of mean 0.34 CPD reduction in exposure by report.
Biological verification of child exposure reveals a less successful outcome. Child cotinine levels fell in the intervention group immediately post‐intervention (month 4) 1.44 to 1.19 ng/mL, and rose in control group 1.17 to 1.35 ng/mL. Between end of intervention and follow up 9 months later levels fell 1.19 to 0.97 ng/mL (intervention) and 1.35 to 0.86 ng/mL (control). There was no significant difference in the mothers' rate of smoking cessation between groups. |
| Hovell 2009 | Low income households targeted. Behavioural ecological model used for development of the counselling intervention. Children's total SHSe showed a significant group by linear time interaction (P = 0.012) and a linear time effect (P < 0.001) from baseline to 6 months. Children's urinary cotinine showed no significant difference. Exposure from mothers in home (reported cigarettes/week) intervention 1.93 (95% CI 0.92 to3.48) control 6.16 (95% CI 3.61 to10.12); total reported exposure (cigarettes/week) intervention 5.15 (95% CI 2.71 to9.17) control 22.97 (95% CI 15.14 to34.58); mothers smoking reported cigarettes/week intervention 77.91 (95% CI 64.22 to91.60) control 92.88 (95% CI 80.59 to105.16); reported smoking by mothers indoors at home (cigarettes/week) intervention 3.94 (95% CI 2.06 to6.97) control 10.37 (95 CI 6.16 to17.06); reported smoking by all indoors at home (cigarettes/week) intervention 6.46 (95% CI 3.16 to12.40) control 19.18 (95% CI 11.15 to32.52). Children's urinary cotinine concentration and mother's reported smoking showed a significant group main effect, but did not show a significant difference in rates between intervention and control groups at 18 months. |
| Hughes 1991 | Intervention to reduce children's ETS exposure in a study of a comprehensive asthma education intervention. The outcome was improved asthma control but no change in exposure to ETS.
No evidence of effect on homes with smoker: Intervention baseline 60% of 47 homes, follow up 52% vs Control baseline 57% of 48 homes, follow up 51% P = NS |
| Irvine 1999 | No evidence of effect.
Mean decrease in child salivary cotinine (ng/ml): Intervention 0.70 vs Control 0.88. Difference= 0.19, 95% CI ‐0.86 to 0.48
Mean increase in mothers' salivary cotinine (ng/ml): Intervention 3.1 vs Control 1.8. Difference= 1.3, 95% CI ‐26.4 to 23.9
Self‐reported quit attempts: Intervention 101/213 vs Control 97/222, P = NS |
| Joseph 2014 | ETS exposure: Little change in household or car rules about smoking 8 weeks after index visit, but parents reported a high rate of total restriction at baseline. Air quality: 8 weeks after index visit, 11 of 38 (29%) parents in the intervention group reported 7‐day point‐prevalent abstinence. In contrast, only one parent in the comparison group reported abstinence from smoking (P = 0.001). There were fewer quit attempts and less readiness to quit in the comparison group. Child health: Not reported |
| Kallio 2006 | At child 8 years of age 10.1% (29/287) of mothers and 19.7% (43/218) fathers in the intervention group smoked regularly. The corresponding %s for the control group were 15.1% (45/298) mothers and 25.1% (60/239) fathers. Additionally 5.9% (17/287) of intervention group mothers and 8.3% (18/218) of intervention group fathers smoked occasionally compared with 5.7% (17/298) of control group mothers and 6.7% (16/239) of control group fathers (NS). |
| Kegler 2015 | ETS exposure: Significantly more intervention participants reported a full ban on smoking in the home than control participants at both 3 months (30.4% vs 14.9%, P < 0.001) and 6 months (40.0% vs 25.4%, P = 0.002) post‐baseline. The longitudinal intent‐to‐treat analysis showed that the difference in change was significant over time. When defining success more stringently by including only those reporting a full ban and no enforcement challenges, we found again that more intervention than control participants were successful in having and enforcing their smoke‐free home rule at 3 months (11.0% vs 5.6%; P = 0.03) and at 6 months post baseline (18.3% vs 8.7%; P = ).002). Air quality: Larger reduction in self‐reported exposure to SHS in the home among intervention participants at both follow‐up points, with a significantly larger decrease in the intervention group. In addition, significantly higher percentage of intervention participants (26.2% vs 18.0%) reported a full smoking ban in cars at 3 months (P = 0.02), although this difference was not observed 6 months post baseline.
Smokers in the intervention group reported fewer cigarettes smoked per day at both follow‐up points, and the longitudinal analysis
indicated that the intervention group had a significantly larger reduction over time. Although observed no difference in cessation
rates between intervention and control groups, smokers in the intervention group had a higher number of quit attempts at the first follow‐up point, but not at 6 months post baseline. Also found that smokers in the intervention group had higher confidence in being able to quit at 3 months, but not at 6 months. The longitudinal intent‐to‐treat analysis, however, showed a significant difference in self‐efficacy to quit.. Child health: Not reported |
| Kimata 2004 | After 1 month urinary cotinine levels reduced 285±43 ngmL‐1 to 2.2±0.85 ngmL‐1 in AEDS cessation group, 257±31 ngmL‐1 to 1.8±52 ngmL‐1 in normal child cessation group and 274±42 ngmL‐1 vs 298±52 ngmL‐1 in control group of children with AEDS. AEDS children showed significant reduction in SCORAD index skin wheal (mm) from 9.9 baseline to 7.5; Control group 9.6 baseline to 9.3. Also significant changes in response to house dust mite & cat dander & lower neutrophil levels. |
| Krieger 2005 | Intervention guided by the transtheoretical stages of change model, as well as by social cognitive theory. Report that 20% of the sample quit smoking and that among smokers who did not go outside to smoke prior to intervention, a quarter did so after education, but data are not provided and it is unclear whether intervention outcomes were different between groups.
Homes where smoking was reported as not allowed at baseline 80% (high intensity group) vs 76% (low intensity group) and at exit 77% (high) vs 80% (low) P = 0.33 NS. |
| McIntosh 1994 | Number of smokers who moved outside: Intervention 7/30, Control 4/30. Not statistically significant.
Urinary cotinine concentrations of children of subjects reportedly smoking outside are above 10.0 in 4/6 (range 6.7 to 54) in Intervention children tested, and in 3/3 (range 12.2 to 21.5) control children tested. These levels suggest significant ETS exposure. |
| Nicholson 2015 | ETS exposure: At the end of the follow‐up phase, 45.4% of families reported a home ban (intervention: 47.2%; control: 43.6%) and 20.4% employed a full ban (intervention: 24.5%; control: 16.4%). Group assignment (intervention or control) was not a significant predictor of adopting a home ban. There was a marginal difference between intervention and control groups for the adoption of full bans (OR = 1.81, P = .060). Air quality: Not reported Child health: Not reported |
| Nuesslein 2006 | Calculated nicotine consumption Intervention: 12 micrograms to 4.65 micrograms vs Control: 12 micrograms to 7.5 micrograms NS
Urinary cotinine levels Intervention 3520 ng/ml to 741 ng/ml vs Control 4572 ng/ml to 724 ng/ml P > 0.05 NS
Across the entire sample (both intervention and control groups) there was an overall reduction in self‐reported smoking with average number of cigarettes smoked reduced from 17 to 10 per day and significant reduction in calculated nicotine consumption using self report data 12 micrograms to 5.5 micrograms (P < 0.05), urinary cotinine 4101 ng/ml to 741 ng/ml (P < 0.05). |
| Ortega 2015 | ETS exposure: TSP‐avoidance strategies improved more in the intervention group than in the control: 35.4% and 26.9% (P = 0.006) at home, and 62.2% and 53.1% in cars (P = 0.008). Logistic regression showed adjusted ORs for appropriate measures in the intervention group vs control group of 1.59 (95% CI 1.21 to 2.09) at home and 1.30 (95% CI 0.97 to 1.75) in cars. Air quality: Not reported Child health: Not reported |
| Patel 2012 | No significant differences between intervention compared to control groups in:
Changed smoking policy: OR2.0 (95% CI 0.166 to 24.069)
Reduced no. of cigarettes: OR 4.88 (95% CI 0.785 to 30.286)
Quit smoking: OR 1.12 (95% CI 0.346 to 3.590) |
| Phillips 2012 | Where both saliva cotinine and self‐report were available, saliva cotinine was used. At eight weeks post‐partum, there was a significantly more smoke free mothers in the intervention (81%) compared with the control group (46%) ‐ P < 0.001. |
| Pollak 2015 | ETS exposure: Not reported Air quality: Found high rates of cessation but no arm differences in smoking rates at the end of pregnancy (0.31 vs. 0.30, materials only vs. counselling, respectively) and 12 months after randomisation (postpartum: 0.39 vs. 0.38). Found high quit rates among non daily smokers but no arm differences (0.43 vs. 0.46 in pregnancy and 0.52 vs. 0.48 postpartum). Among daily smokers, found lower quit rates with no arm differences but effects favouring the intervention arm (0.13 vs. 0.16 in pregnancy and 0.17 vs. 0.24 postpartum). Child health: Not reported |
| Prokhorov 2013 | Smoking status of smoker; 90% on baseline smokers in each group still using tobacco (N = 36 intervention, N = 35 control) Results for the environmental monitors: two monitors ‐ one in a "higher exposure" room than the other. In the high exposure room there was a significant main effect for time (P < 0.001) and time by condition effect (P < 0.05); for the intervention group the mean ambient nicotine level decreased from baseline at 12 months (1.14 μg/m3 to 0.20μg/m3, P < 0.01). There was a decrease in mean of control group but not significant (0.55 μg/m3 to 0.17μg/m3, P = .99), and a significant difference between average rate of change for intervention and control groups. In the low exposure there was a significant main effect for time but not time‐by‐condition and similar reductions in the intervention and control groups. Percentage of households banning smoking at 12 months: 73% of the intervention group and 56% of the control group. |
| Pulley 2002 | Follow‐up three weeks post‐intervention Cigarettes/day: intervention 16.17 (sd 9.10), control 11.33 (sd 4.69) ‐ P = 0.132 Mothers in the intervention group smoked more at enrolment compared with control group, an effect not present at the 2 week visit (baseline) but present again three weeks post intervention Respiratory illness: intervention N = 5 (42%), control N = 6 (66%) ‐ P = 0.666 |
| Ralston 2008 | Counselling strategies based on the stages of change component of Prochaska's transtheoretical model. N = 42, 33% (N = 14) lost to follow‐up. The quit rate: 14% intervention, 5% control group which did not reach statistical significance |
| Ralston 2013 | Differences between intervention and control groups were not significant (fisher's test): Self‐reported quit ‐ control 6/30 (20%, 95% CI 9 to 38%) and intervention 5/30 (17%, 95% CI 7 to 34%); any quit attempt during follow‐up ‐ control 11/30 (37%, 95 CI 22 to 55%) and intervention 16/30 (53%, 95% CI 36 to 70%); cut down ‐ control 11/30 (27%, 95% CI 22 to 55%) and intervention 15/30% (15%, 95 CI 33 to 67%); used quitline ‐ control 2/30 (7%, 95% CI 8 to 22%) and intervention 0/30 (0%, 95% CI 0 to 13%). |
| Ratner 2001 | 6 month Follow up: 36% abstinent, 26% occasional, 38% daily smoking. 76% homes smoke‐free.
12 month Follow up: 20% abstinent, 35% occasional, 46% daily. 76% homes smoke‐free
No difference between groups.
6 month Follow up abstinence was 41% vs 30% (intervention vs control) but at 12 months abstinence was sustained in 21% vs 18.5% (intervention vs control) NS.
Daily smoking at 6 months was 31% vs 45% (intervention vs control) but at 12 months was 41% vs 50% (intervention vs control). NS
Abstinence reported as 38% vs 27% (treatment vs control) NS. |
| Schonberger 2005 | At 6 month Follow up
Maternal post‐natal smoking Intervention 52% (14/27) vs. Control 28% (8/30) P = 0.04
Partner smoking Intervention 31% (14/44) vs Control 20% 9/45) NS
Smoking by others Intervention 47% vs Control 50% NS |
| Schuck 2014 | ETS exposure: Not reported Air quality: Parents who received quitline counselling were more likely to report 7‐day point‐prevalence abstinence at 12‐month assessment (34.0 versus 18.0%, odds ratio (OR) = 2.35, confidence interval (CI) = 1.56–3.54) than those who received a standard self‐help brochure. Parents who received quitline counselling were more likely to use nicotine replacement therapy (P < 0.001) than those who received a standard self‐help brochure. Among parents who did not achieve abstinence, those who received quitline counselling smoked fewer cigarettes at 3‐month (P < 0.001) and 12‐month assessment (P < 0.001), were more likely to make a quit attempt (P < 0.001), to achieve 24 hours’ abstinence (P < 0.001) and to implement a complete home smoking ban (P < 0.01). Child health: Not reported |
| Severson 1997 | Cessation at 6 & 12 months: Intervention 25/1073 (2.3%), Control 10/802 (1.2%), P < 0.05*, 1‐tailed test
Cessation at 12 months: Intervention 59/1073 (5.5%), Control 38/802 (4.7%) NS. Only 35 of the 97 12‐month quitters had quit by six months, with more early quitters in the intervention group (25/59) compared with the control group (10/38).
Relapse prevention at 6 & 12 months: Intervention 200/609 (33%). Control 109/417 (26%), P < 0.05*, 1‐tailed test
Relapse prevention at 12 months: Intervention 261/609 (43%), Control 163/417 (39%)
* when controlling for other variables this effect was lost.
Significant benefits of intervention on CPD, readiness to quit, likelihood of making a quit attempt, attitude towards smoking, knowledge of ETS effects on children. |
| Stotts 2012 | Lower rates of total smoking bans in the usual care‐reduced measurement group (P < 0.012 for total ban, P < 0.01 for car) but not significantly different for home alone. 63.6% receiving motivational interviewing had a ban by 1 month post‐discharged compared to 20% of the usual care group. No significant differences in environmental nicotine monitors measurements |
| Streja 2014 | ETS exposure: No significant difference between intervention and control groups in child urine cotinine levels. Air quality: No significant difference between intervention and control groups in any of the measures. Child health: Not reported |
| Tyc 2013 | Group difference for average cigarettes smoked and child SHSe was not significantly different as the 12‐month follow‐up (P > 0.05). Child SHSe was significantly lower at 12 months from baseline for each group (P < 0.05). Children's urinary cotinine showed no significant difference, and did not change significantly over time in either group. |
| Ulbricht 2014 | ETS exposure: The child urine cotinine level difference between follow‐up and baseline was smaller in the control than in the intervention group, but the effect was not significant. Air quality: Not reported Child health: Not reported |
| Van't Hof 2000 | There was no statistically significant difference in the smoking relapse rate between women in the intervention (41%) and control (37%) groups. |
| Vineis 1993 | Smoking cessation for mothers: Intervention 12/74 vs Control 10/84, OR 1.4, 95% CI 0.6 to 3.5
Smoking cessation for fathers: Intervention 18/173 vs Control 26/244 OR 1.0 showed a trend towards smoking cessation for mothers classified as white collar workers in the intervention arm (5/33) versus the control arm (2/36) (Odds Ratio [OR] 3.0; 95% confidence intervals [CI] 0.6 to 16.0). No difference was detected for the other participants, comprising 80 blue collar mothers and a total of 411 men defined as white or blue collar workers. |
| Wahlgren 1997 | Intensive intervention was able to demonstrate a statistically significant but very small reduction in cigarette exposure from parents' cigarettes reported by parents without biological verification. Mean number of parent cigarettes smoked in presence of child fell in Intervention group: 5.8CPD baseline, 3.4CPD at clinic pre‐intervention to 1.2 CPD at 6 months following completion of intervention. In control group, parent reported exposure fell from 8.0 baseline, 5.7 pre‐intervention to 4.6 CPD at 6 month follow up. P for trend < 0.01. The effect size was small, however, and curiously, the largest fall in this measure occurred in the period after recruitment but before the intervention. After the intervention, parents reported a reduction of 1.1 cigarettes per day smoked in the presence of the children for the control group, and 2.2 cigarettes per day for the intervention group. There was no validation by measurement of children's exposure or absorption via cotinine, or validation of the parental reports, and the clinical significance of such a fall is unclear
Environmental monitor (1 room with heaviest child exposure) measured air nicotine (mcg/ cubic metre). Intervention group baseline 1.7, follow up 1.9 vs Control baseline 2.3, follow up1.4. Measured child asthma symptoms but found no sustained difference between groups for this measure. |
| Wakefield 2002 | Home smoking ban:
Intervention 41% at baseline, 49% at Follow up vs Control 40% at baseline, 42% at Follwo up. Relative increase in bans not significant; P = 0.40
Car smoking bans: Intervention baseline 33%, Follow up = 52%, Control baseline 37%, Follow up 48%, NS;
Low rates of parental cessation, no difference between groups.
Urinary cotinine measured for 209 children: Mean cotinine/ creatinine Intervention B = 22.8 nmol/mmol Follow up 21.0, Control baseline 25.7, Follow up 21.0, NS, P = 0.40 |
| Walker 2015 | ETS exposure: No significant difference between group in urine cotinine level change over time, self‐reported SHS exposure, smoking ban, smoking cessation. Air quality: No significant change in smoking prevalence and intensity was seen by group. Child health: No significant difference in infant cough, acute respiratory illness or rate of hospitalisations between treatment groups. |
| Wang 2015 | ETS exposure: Children's urinary cotinine was significantly lower (Z = ‐3.136; P = 0.002) in the intervention group (1.29 ng/mL) than the control group (1.78 ng/mL). After 6months, reported mean ETS exposure from caregivers decreased 40.6% from baseline among the intervention group and 3.4% among controls. Air quality: Caregiver's 7‐day quit rate was significantly higher (34.4% versus 0%) (p < 0.001; adjusted OR = 1.13; 95% CI: 1.02‐1.26) in the intervention group. Child health: Not reported |
| Wiggins 2005 | Mothers living in disadvantaged inner city areas targeted. No significant effect of either intervention.
Support health visitor group vs control group, RR 0.86 (95% CI 0.86 to 1.19); Community support group RR 0.97 (95% CI 0.72 to 1.33). Reported no notable differences in child health outcomes
for children receiving either post‐natal support intervention. |
| Wilson 2001 | Of 51 children with complete urinary cotinine: creatinine ratio (CCR) data. Log CCR (ng/mg) Intervention baseline 1.82, Follow up 1.27 vs Control baseline 2.34, Follow up 1.93, adjusted Diff ‐0.38, adjusted P = 0.26.
Proportion with >1 acute asthma visit/year: Intervention baseline 50, Follow up 29.6, Control baseline 37.2, Follow up 46.5, OR 0.32, P = 0.03
No significant differences in hospitalisation, prohibition of smoking in home, or smoking. examined the effect of an intervention targeting smoking behaviour change and asthma education on health care utilisation and asthma hospitalisations, and explored other measures of asthma control. It demonstrated a reduction in the prevalence of children making more than one acute care asthma visit in the year following the intervention. Given that there was no apparent benefit of the smoking‐related counselling on smoking‐related outcomes, it is likely that it was the asthma education that achieved the improvement in asthma morbidity, rather than the smoking behaviour programme. |
| Wilson 2011 | Mean urinary cotinine creatinine ratio (CCR) decreased in both groups (not shown data for 6 and 12 month follow‐up). The natural log of the urinary CCR decreased more in the intervention arm but it did not reach statistical significance (B coefficient ‐0.307 95% CI ‐0.633 to 0.018, P = 0.64) Decrease in asthma symptoms at follow‐up visits in both groups. The decrease in the intervention group did not reach statistical significance (B coefficient 0.035, 95% CI ‐0.208 to 0.277, P = 0.78) At 12 months 84.0% of the intervention group (N = 142) and 77.1% of the control group (N = 131) had home smoking bans (P = 0.11). |
| Winickoff 2010 | Prevalence of self‐reported 7 day abstinence 38% at baseline and 30% at follow up in the control group vs 31% at baseline and 30% at follow up in the intervention group (Effect size = 13% P = NS) Cotinine‐confirmed 7 day abstinence for baseline current smokers NS.
For baseline current smokers 18% in the control and 64% in the intervention group reported making a 24hr quit attempt by follow up (P = 0.005). |
| Woodward 1987 | No evidence of effect.
Mother self‐reported quitting: Intervention 6%, Control 2.2%, P = 0.25.
Median infant urinary cotinine levels (mcg/litre): Intervention 11.0 (N = 48) vs Control 10.0 (N = 53), P = NS |
| Yilmaz 2006 | Quit smoking: Child intervention group 24.3%; Mother intervention group 13%; Control 0.8%. (χ2 = 29.5, P < 0.0001)
Smoking location change: Child intervention: 73%, Mother intervention: 46.6%, Control 11.6% (χ2 = 90.1, P < 0.0001)
Knowledge change (score on MCQ, possible score 0‐100): mean post‐intervention score in child intervention 63.51 (±7.35 ‐ not stated whether these ± is standard deviations, or 95% confidence intervals) mother intervention 57.69 (±10.46) control 56.68 (±7.67) (ANOVA showed that these scores differed) P < 0.0001
(Note: not an intention‐to‐treat analysis) |
| Yucel 2014 | ETS exposure: No significant difference between intensive and minimal intervention groups in change in child urine cotinine levels. Air quality: No significant difference in any outcome. Child health: Not reported |
| Zakarian 2004 | Low income ethnically diverse population. Both groups showed significant decline in reported exposure to mother's cigarette's/week (intervention group 18.89 at baseline to 5.41 at 12 months, control group 13.25 at baseline to 5.23 at 12 months) (P < 0.001). Total exposure to cigarettes/week (intervention group 53.2 at baseline to 21.99 at 12 months, control 54.48 at baseline to 18.22 at 12 months) (P < 0.001) however, no significant difference between groups.
Children's urinary cotinine concentration did not show a significant change over time in either group ‐ No significant difference between groups. |
| Zhang 1993 | This was a study designed to increase public knowledge of the health consequences of cigarette smoking and to promote healthier attitudes among elementary school students in China, and encouraged these students to help their fathers to quit smoking. Schools in one district used a tobacco control curriculum, and the control group were students in another district. The other school‐based study was a cardiovascular health promotion programme that included an intervention designed to limit children's ETS exposure and negative role modelling from staff and visitors smoking at school (Elder 1996). Conducted in the USA, this study used a cluster‐randomized design with schools as the unit of allocation.Number (proportion) of smoking fathers: Intervention baseline 6843/9953 (68.8%) & follow up 60.7% vs Control baseline 6274/9580 (65.5%), follow up "approximately the same" [numbers are not stated]
Proportion of fathers who quit smoking for at least 180 days:
Intervention 800/9953 (11.7%), Control 14/6274 (0.2%) |